ACQUIRED HEMOSTATIC DISORDERS
description
Transcript of ACQUIRED HEMOSTATIC DISORDERS

ACQUIRED HEMOSTATIC DISORDERS
Lugyanti SukrismanDiv. of Hematology & Medical Oncology
Dept. of Internal Medicine University of Indonesia/
Cipto Mangunkusumo Hospital

ACQUIRED HEMOSTASTIC DISORDERSBLEEDINGLiver diseasesITPAcquired qualitative
platelet defectsDef of vit K-
dependent factorsExcessive
fibrinolysis
THROMBOSISDisseminated
intravascular coagulation
Antiphospholipid syndrome
• Pathologic anticoagulant (immune coagulopathies)

Classification of disorders of hemostasisMajor types
Disorders Examples
Acquired Thrombocytopenia Auto- and alloimune, drug-induced, hypersplenism, hypoplastic (primary, suppressive), DIC
Liver disease Cirrhosis, acute liver failure, liver transplantation
Renal failureVitamin K deficiency Malabsorption syndrome, hemorrhagic
disease of the newborn, prolonged antibiotic therapy, malnutrition, prolonged billiary obstruction
Hematologic disorders
Acute leukemias (particulary promyelocytic), myelodysplasias, monoclonal gammopathies, essential thrombocytemia

Classification of disorders of hemostasisMajor types
disorders Examples
Acquired Acquired antibodies against coagulation factors
Neutralizing antibodies against F.V, VIII & XIII; accelerated clearance of antibody-factor complexes, e.g. acquired von Willebrand disease, hypoprothrombinemia associated with APS
Disseminated intravascular coagulation
Acute (sepsis, malignancies, trauma, obstetric complications) and chronic (malignancies, giant hemangiomas, missed abortion)
Drugs Antiplatelet agents, anticoagulants, antithrombins, and thrombolytic, myelosuppressive, hepatotoxic, and nephrotoxic agents
Vascular Nonpalpable purpura (“senile”, solar, factitious purpura), use of corticosteroids, vitamin C deficiency, purpura fulminans; palpable purpura (Henoch-Schönlein, vasculitis, dysproteinemias)

A. Coagulation abnormalities of liver diseases (1)Liver’s central role in hemostasis:
◦The major site of synthesis of all coagulation factors (except vWF), regulatory proteins of coagulation system (antithrombin, protein C & S),
component of fibrinolytic system◦Clearance of activated clotting factors from circulation
Colman RW. Hemostasis & thrombosis. Basic principles & clinical practice 2006

A. Coagulation abnormalities of liver diseases (2)
1. Thrombocytopenia2. Platelet dysfunction3. Coagulation abnormalities4. Disseminated intravascular coagulation
& hyperfibrinolysis
Colman RW. Hemostasis & thrombosis. Basic principles & clinical practice 2006

1. ThrombocytopeniaPathogenesis: Splenic sequestration due to portal
hypertension Impaired platelet production Thrombin-mediated platelet consumption HCV infection:
◦ Viral infection of megakaryocytes◦ Platelet destruction due to autoimmune
mechanisms

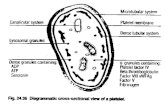
2. Platelet dysfunction Reduced platelet adhesion Impaired platelet aggregation
Colman RW. Hemostasis & thrombosis. Basic principles & clinical practice 2006

3. Coagulation abnormalities Reduced of vit-K-dependent coagulation
factors (II, VII, IX, X) & F. V Fibrinogen: normal/increased decreased:
◦ Impaired synthesis◦ Increased catabolism◦ Loss into extra vascular space◦ Massive hemorrhage
Diminished antithrombin, protein C & S, heparin cofactor II, α-2 macroglobulin
Colman RW. Hemostasis & thrombosis. Basic principles & clinical practice 2006

Diagnosis (1)History of jaundice/acute hepatitis, risk of
infection (iv drug user, liver disease in family, etc)(History of) bleeding: hematemesis &/melenaClinical sign of liver disease & complication:
◦Jaundice◦Other signs: pale, ascites, splenomegaly, palmar
erythema, edema, etc◦Bleeding signs: petechiae, hematoma,
hematemesis/melena, etc

Diagnosis (2)Laboratory results:
◦CBC: thrombocytopenia ± anemia/leukopenia◦Liver function tests: low albumin level, increased
transaminase/bilirubin (variably)◦Coagulation tests: PT, aPTT, fibrinogen, D-dimer◦Hepatitis markers (hepatitis B/C)
Abdominal US: liver disease & others (bile stone, etc)
Others: endoscopy of upper GI

TreatmentActive bleeding/plan of invasive procedure:
Vit K, FFP/cryoprecipitate, platelet concentrate, packed red cells
Stop the bleeding: ligation/sclerosing therapy & pharmacology treatment
Treatment of liver disease & complication, non pharmacologic treatment & nutritional support

B. Disseminated intravascular coagulation
Consumptive coagulation Defibrin(ogen)ation syndromeThrombohemorrhagic syndrome



Activation of coagulation
Circulating thrombi
Thrombotic occlusion of microcirculation of all organs
Fibrinolysis inmicrocirculation
Circulating fibrin degradation products
Consumption of platelets and coagulation proteins
+
Events leading to thrombosis
Signs of microvascular thrombosis•Neurologic : multifocal, delirium, coma•Skin : focal ischemia, superficial gangrene•Renal : oliguria, azotemia, cortical necrosis•Pulmonary: acute respiratory distress syndrome•GI: acute ulceration•Fragmentation hemolytic anemia
Events leading to bleeding
Signs of hemorrhagic diathesis•Neurologic : intracerebral bleeding•Skin : petechiae, ecchymoses, venipuncture oozing•Renal : hematuria•Mucous membranes: epistaxis, gingival oozing•GI: massive bleeding
Marder VJ. Hemost and Thromb. 5edt. 2006.1571-1600
Marder VJ. Hemost and Thromb.. 2006.1571-1600

Underlying disorder
Systemic activation of coagulation
Widespread intravascular fibrin deposition
Consumption of platelets and clotting factors
Thrombosis and organ failure
(severe) Bleeding

Clinical manifestationComplexity and variability depends on:Triggering event(s)Host ResponseComorbid conditions

Diagnostic approachClinical featuresBleeding: mucosal
oozing, ecchymoses, petechiae, massive GI blood loss
Renal/cerebral/ hepatic dysfunction, ARDS
LaboratoryIncreased D-Dimer level Increased FDP level Decreased AT levelDecreased platelet levelBload smear:
schistocytesDecreased fibrinogen
levelProlonged thrombin
time/aPTT/PT

Differential Diagnosis Severe liver failure/liver disease Vitamin K deficiency HELLP syndrome Thrombotic thrombocytopenic purpura Congenital abnormalities of fibrinogen

TREATMENT OF DIC Treat the underlying disease Restore the circulation Replacement therapy
FFP/cryoprecipitate, platelet concentrate, packed red cells
Other pharmacologic therapy:Heparin, antithrombin, activated Protein C, others

C. Deficiency of vitamin K-dependent factors vitamin K: essential for the final postribosomal
carboxylation of coagulation factors II, VII, IX, X and protein C and protein S
laboratory features: prolonged PT & decreased factors II, VII, IX, X level
in severe, protracted vitamin K deficiency: prolonged aPTT

Vitamin K deficiencyI. Inadequate supply: 1. Dietary deficiency 2. Destroying the gut flora by administration
of broad-spectrum antibiotics II. Impaired absorption of vitamin K: 1. Biliary obstruction (gallstone, tumor) 2. Malabsorption of vitamin K 3. Drugs (cholestyramine)III. Pharmacologic antagonists of vitamin K (coumarins, warfarin)

D. Excessive fibrinolysis Primary fibrinolysis (excessive release of tissue
Plasminogen Activator): rare Acquired:
◦ Thrombolytic therapy◦ Secondary disease-related:
surgical/ trauma neoplasms (prostate, pancreas, leukemia) systemic lupus erythemathosus severe liver disease (defective clearance of activator)
◦ Fibrinolysis secondary to intravascular coagulation
Ratnoff OD, Forbes CD. Disorders of hemostasis 1996, 296-322


Diagnosis Bleeding signs Thrombolytic therapy/other condition
related to acquired excessive fibrinolysis Laboratory:
◦ FDP: increased◦ Plasma fibrinogen level: reduced◦ Euglobulin clot lysis time: rapid◦ TT, PT, aPTT: prolonged
Ratnoff OD, Forbes CD. Disorders of hemostasis 1996, 296-322

Treatment of excessive fibrinolysis Fibrinolytic inhibitors:
◦ Tranexamic acid◦ -Aminocaproic acid (EACA)
Fibrinolytic inhibitor: contraindicated for fibrinolysis secondary to/associated with intravascular clotting
Ratnoff OD, Forbes CD. Disorders of hemostasis 1996, 296-322


E. Pathologic anticoagulants (immune coagulopathies) (1)
• Appear spontaneously in subjects with previously normal hemostatic function.
• Antibodies to factor VIII, “idiopathic” inhibitor• Autoimmune disorders (SLE, rheumatoid arthritis,
multiple sclerosis, pemphigus, etc)• Hematologic malignancies: chronic lymphocytic
leukemia, non-Hodgkin lymphoma, multiple myeloma, etc
Drug reactions: allergies to penicillin, sulfonamides, chloramphenicol, methyldopa, etc

E. Pathologic anticoagulants (immune coagulopathies) – (2)
• Prolonged aPTT• Reduced F. VIII levels• Inhibitor F. VIII • Spontaneous, often severe/life-
threatening bleeding
Colman RW. Hemostasis & thrombosis. Basic principles & clinical practice 2006