Bleeding Diathesis Inherited & Acquired Causes of Bleeding Disorders Harry Kopolovich.
62
Bleeding Diathesis Inherited & Acquired Causes of Bleeding Disorders Harry Kopolovich
-
Upload
giles-flynn -
Category
Documents
-
view
217 -
download
5
Transcript of Bleeding Diathesis Inherited & Acquired Causes of Bleeding Disorders Harry Kopolovich.
- Slide 1
- Slide 2
- Bleeding Diathesis Inherited & Acquired Causes of Bleeding Disorders Harry Kopolovich
- Slide 3
- Clinical Vignette #1 24 y/o male with a history of Hemophilia A is playing baseball, when a line drive strikes him in the head He is immediately brought to your ER, where he has a GCS of 15, and a normal neuro exam He complains of a slight headache and pain from a bruise that is developing on his temple Imaging? Management?
- Slide 4
- Clinical Vignette #2 65 y/o woman is brought to your emergency room because of epistaxis Medical history reveals that she is taking Coumadin for a DVT/PE INR is 7.9 Treatment?
- Slide 5
- Clinical Vignette #3 55 y/o man is brought to your hospital after sustaining a frontal crash on I- 95. The patients abdomen struck the steering wheel He is complaining of abdominal pain Medical history reveals that he is taking Pradaxa (Dabigatran) for non- valvular atrial fibrillation Ct-imaging demonstrates a retroperitoneal hematoma with a blush Management?
- Slide 6
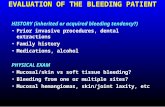
- Disorder of Hemostasis Inherited Genetic Mutations Familial De Novo Mutations Iatrogenic Purposeful Huge Pharmaceutical Market
- Slide 7
- Normal Hemostasis Balance between pro-coagulant and anti- coagulant factors Competing interest between smooth laminar blood flow and maintenance of structural integrity of vasculature Healthy individuals have this occurring constantly Diseased states lead to hemorrhage or thromboembolism
- Slide 8
- Arterial V.S. Venous Arterial High flow and high pressure Small amounts of damage leads to catastrophic losses Primarily relies on platelets Venous Slower flow and lower pressure Coagulation cascade with thrombin generation primary means of hemostasis Thus, ASA to prevent coronary artery thrombus and heparin/lovenox/coumadin to prevent DVT
- Slide 9
- Disorders Of Hemostasis Following should be considered: 1)Thrombocytopenia or Platelet Dysfunction 2)Low levels of multiple coagulation factors resulting from Vitamin K deficiency of hepatic dysfunction 3)Single factor deficiency Inherited or Acquired 4)Consumptive coagulopathies Eg. DIC 5)Circulating inhibitors to coagulation factors
- Slide 10
- Vascular Wall Physiology Endothelial Cells Functions as a barrier to contain blood Prevents contact with thrombogenic sub-endothelial contents Intact cells posses strong anti- coagulant functions Prostacyclin, NO, ADPase, plasminogen activator
- Slide 11
- Endothelial Cell Damage Procoagulant state Activated endothelial cells Selectins, -integrins, vWF Exposed sub endothelial matrix Tissue Factor End Result Combination of activated proteins and exposed surfaces result in: Platelet Activation Leukocyte Migration Initiation of Coagulation Cascade Initiation of Anti-coagulant systems Thrombin-thrombomodulin cascade, protein C, S, t-PA
- Slide 12
- Coagulation Cascade Critical for understanding normal hemostasis Huge target for Pharmaceutical Companies Potential for remediating deficiencies created by acquired or iatrogenic means Liver is the primary site for synthesis of coagulation factors
- Slide 13
- Slide 14
- Extrinsic Pathway Vascular injury leads to exposed sub endothelial matrix Results in exposure of highly thrombogenic Tissue Factor Combines with Factor VII--> VIIa Results in conversion X-->Xa Monitored using PT/INR Deficiencies in Vitamin K analogues leads to elevations
- Slide 15
- Intrinsic Pathway Contact Activation Pathway Initiated by collagen contacting HMWK Monitored by aPTT
- Slide 16
- Common Pathway Both pathways converge ultimately result in activated thrombin Abnormalities of X, V, II result in elevation of PT & PTT
- Slide 17
- Platelet Physiology Platelet functions as cellular based platform for hemostasis Adhesion results in transmembrane signaling Translocation of receptors to membrane surface Receptor transformational changes Degranulation Pro-coagulant surface of platelet Serves as assembly point for coagulation cascade Amplifies overall procoagulant response Produces fibrin-->Leading to clot stabilization
- Slide 18
- Platelet Physiology Platelets derived from bone marrow Survival time 7-10 days ~7,100 platelets required/day even with no challenge to vascular integrity Normal count is 150,000-450,000 Qualitative function measure through bleeding time
- Injury leads to tumbling of platelets--> Conformational change leads to transmembrane signaling Exposure of GPIIb/IIIa receptor Higher affinity bond Secures platelet firmly to sub endothelium
- Slide 21
- Bleeding Caused by Platelet Disorder Can be broadly separated by Quantitative versus Qualitative Disorders
- Slide 22
- Quantitative Disorder of Platelets 1)Decreased Platelet Production B12/Folate Deficiency Congenital Causes Alport's Syndrome, Fanconi's anemia, Wiskott-Aldrich Syndrome Marrow damage Aplastic anemia, Chemotherapy, Drug Induced, Malignancy 2)Increased Platelet Destruction Immune Mediated: ITP, Drug Induced, HIV, SLE, Heparin Non-Immune Mediated DIC, TTP, HELLP 3)Increased Platelet Sequestration Splenomegaly, Liver Disease, Malignancy, Myelofibrosis
- Slide 23
- Qualitative Platelet Defects 1 Drug Induced Aspirin Normal platelet function requires release of Thromboxane A2 Vasoconstrictor & Platelet Agonist Generated in cytostol of platelet by cleavage of Arachidonic acid by COX ASA irreversibly binds COX for the lifetime of the platelet Aggrenox Blocks GPIIb/IIIa Receptor Plavix ADP receptor blocker
- Slide 24
- Qualitative Defects 2 Uremic Dysfunction Caused by protein accumulation in renal failure GSA (Guanidinosuccinic acid): Induces high levels of NO Both compounds inhibit platelet function Can be treated by treating underlying cause DDAVP, Cryoprecipitate Platelet transfusion usually futile Newly transfused platelets rapidly acquire uremic effect
- Slide 25
- Congentital Platelet Dysfunction Inherited platelet disorders can be classified: 1)Disorders of Platelet Receptors Bernard-Soulier Disorder Decreased Surface Expression of GPIb Can manifest even in adulthood Mild-to-Moderate bleeding disorder Glanzmann's Thrombasthemia Absent platelet aggregation in response to Ristocetin Caused by decreased number/function of GPIIb/IIIa receptors
- Slide 26
- 2)Disorder of Platelet Granules: Hermansky-Pudlak Syndrome Lack of secondary wave of platelet aggregation due to deficient cytostolic proteins Congentital Platelet Dysfunction
- Slide 27
- Von Willenbrand Disease Disorder of plasma proteins that serve as ligands for platelet adhesion Phenotypically identical to platelet dysunction vWF is synthesized in vascular endothelial cells Mediates platelet rolling along damaged vascular wall with subsequent platelet adhesion vWF serves as the carrier protein for Factor VIII Decreased vWF-VIII binding leads to elevation of aPTT
- Slide 28
- Three type of VWD 1)Type I -Mild to moderate quantitative decrease Dominant patter of inheritance Mild bleeding in relation to dental procedures or surgery Treated with DDAVP 0.3mcg/kg SC Increases amount of vWF synthesized in EC 2)Type II -Qualitative defect in vWF Dominant/Recessive Treatment is with vWF concentrate 3)Type III -Complete Deficiency of vWF Inherited two bad copies of genes Severe bleeding vWF concentrate
- Slide 29
- Bleeding Caused by Coagulation Factor Disorders With normal platelet function, primary hemostasis initiates plugging of vascular lesions and maintains mucosal integrity However, if coagulation factors are not present, then the initial platelet plug is not solidified by secondary hemostasis, leading to clot breakdown and bleeding
- Slide 30
- Coagulation cascade deficiency bleeding differs from platelet dysfunction/absence bleeding Etiology Platelet Abnormality Coagulation Factor Deficiency Phenotype 1)Mucosal bleeding 2)Petechiae 1)Bleeding in deep tissues & joints 2)Delayed bleeding
- Slide 31
- Hemophilia X linked deficiencies of Hemophilia A & B are the most common inherited bleeding disorder after VWD Hemophilia A is six time more common the B Both are characterized by their factor levels Mild: >5% activity Moderate: 1-5% Severe:
- Patients on Coumadin frequently become excessively over anti-coagulated, even those who have been stable for months In 2001 Penning-Van Beest et al., looked at risks for becoming over anticoagulated when using coumadin Sample size: 17,000 outpatients INR >6.0 noted on 22.5 per 10,000 treatment day Diarrhea: RR 12.8 Worsened Heart Failure: RR 3.0 Fever: RR 2.9 Impaired Liver Function: RR 2.8
- Slide 43
- Coumadin Mechanism of Action -Blocks gamma-carboxylation of Vitamin K dependent coagulation factors -Impairs synthesis of coagulant factors II, VII, IX, X and anti-coagulant factors protein C & S -Factor VII has the shortest half life (6 hours) Absorption -Rapidly and completely absorbed from stomach, with peak concentration occurring within 4 hours
- Slide 44
- Metabolism -Coumadin undergoes metabolism via Cytochrome P450 system in the liver -92% of metabolites excreted in Urine Accidental/Intentional Ingestion -Absorption with activated charcoal
- Slide 45
- Reversal Need for reversal depends on: Height of elevation of INR Seriousness of injury Need for rapidity of normalization of INR 2008, Journal Chest Published Pharmacology and management of the Vitamin K antagonist
- Slide 46
- Recommended Management of A Supratherapeutic INR INRBleeding PresentRecommended Action >Ther5.0NoLower Warfarin Dose or Omit a Dose and Resume Warfarin At A Lower Dose When INR Is In Therapeutic Range >59.0NoOmit A Dose And Give Vit K 1 to 2.5mg PO >9.0NoHold Warfarin And 2.5 to 5mg Vit K AnySerious or life threateningHold Warfarin, Give 10mg Vit K via Slow IV, Supplement With FFP or rfVIIa
- Slide 47
- How to Give Vit K? Meta Analysis of 10 randomized and 11 prospective trials to determine effectiveness of various routes of Vit K supplementation in patients with pretreatment INR 4.010 without signs of bleeding Reported as percentages of INR 1.84.0 24 hours after stopping Warfarin and administration of Vitamin K by various routes -Placebo: 20% -Subcutaneous: 31% -IV: 77% -PO: 82% 10mg of Vit K temporarily renders pt resistant to Warfarin for days to weeks
- Slide 48
- Significant Or Life Threatening Bleeding Rapid reversal must be undertaken at any INR -Slow IV infusion of Vit K -FFP: ~2 to 3 Units Dose of FFP = (target INR level [%] - present INR level [%] x kg Eg. 60Kg woman with AVR who has UGIB and INR 7.5 (5% of normal), target INR 1.5 (40% normal) (40-5) x 60 = 2100ml FFP -Recombinant Factor VIIa -Prothrombin Complex Concentrate (10-80mcg/kg)
- Slide 49
- ICH on Warfarin Mortality rates associated with anticoagulant associated ICH at 30 days Unconscious on Admission 96% Unconscious before start of active treatment 80% Treatment with Warfarin antagonist while still conscious 28% Factors associated with positive outcome are inversely proportional to delays in therapy -Simply put, the longer the delay, the worse off the patient
- Slide 50
- FFP - Avg 8Units of FFP ~ 2L -Disadvantage: Large volume load -Median time to normalization of INR: 30 hours -Cost: $200-400 PCC - US Has three factor PCC (II, IX, X) -Disadvantage: Thrombotic events -Median time to normalization of INR: 30 min -Cost: $1,000-2,000 Recombinant factor VIIa - Initial Dose 62mcg/kg -Disadvantage: Has to be re-dosed (t1/2 = 2.3 hours) -Median time to normalization of INR: Immediate -Cost: $5,000-15,000
- Slide 51
- Clinical Vignette #2 65 y/o woman is brought to your emergency room because of epistaxis Medical history reveals that she is taking Coumadin for a DVT/PE INR is 7.9 Treatment? Depends If you can achieve hemostasis, treat at INR 5.0 9.0 with Vit K 2.5 or 5mg If unable to achieve hemostasis and/or bleeding significant, will need FFP or whatever your facility has
- Slide 52
- Pradaxa (Dabigtran) In 2010, US FDA gave Pradaxa, the first new oral anti-coagulant in 50 years Currently, its approved only for the prevention of embolic stroke for non-valvular atrial fibrillation Reversible, potent, competitive direct thrombin inhibitor. Capable of binding both free and already bound thrombin Ultimately prevents conversion of fibrinogen to fibrin -Inhibits platelet aggregation (2 o effect of thrombin)
- Slide 53
- Background RE-LY (Randomized Evaluation of Long Term Anti-Coagulation Therapy) -Phase 3 Prospective trial -Head to Head evaluation of Pradaxa vs Coumadin -Studied 110mg BID, 150mg BID vs. Coumadin -150mg BID had similar rates of bleeding, but superior efficacy
- Slide 54
- Pharmacokinetics Dabigatran etexilate is a pro-drug After ingestion, it is metabolized to dabigatran, which produces immediate anti-coagulation Time to peak is 2 hours Within 4-6 hours post ingestion, 70% drug is metabolized 80% Eliminated in urine ~12-17 hours -Dosing Schema Crcl >30ml/min: 150mg/BID CrCl 15-30ml/min 75mg/BID CrCl
- Slide 55
- Monitoring of Anticoagulation Currently, there is no simple way of measuring the degree of anti- coagulation Furthermore, the manufacture does not advocate for routine monitoring as there are no known drug-drug, drug-food interactions* -Pradaxa-Amiodarone has been implicated in a case report implicating supratherapeutic dabigatran levels as contributing to fatal GI hemorrhage Legrand et al., The use of dabigatran in elderly patients
- Slide 56
- Monitoring of Anticoagulation Typical Measures of clotting time aPTT/PT/INR have limited clinical utility in assessing the anti-coagulant effect aPTT does not respond linearly to the dose or intensity of dabigatran aPTT reaches a plateau and peaks 2-3x control value in the presence of dabigatran aPTT is a qualitative measure to the presence of dabigatran If aPTT is normal, excludes presence of dabigatran PT/INR also demonstrates linear response -INR expected to rise no more then 1.2-2.0 in the presence of dabigatran
- Slide 57
- Monitoring of anti-coagulation Thrombin time - Not routinely available -Asses activity of thrombin by measuring rate of conversion of fibrinogen fibrin Ec arin Clotting Time (ECT) - Ecarin is a snake venom -Converts prothrombin meizothrombin -Metabolite inhibited by direct thrombin inhibitors Hemoclot Thrombin Inhibitor Kit - Awaiting FDA approval
- Slide 58
- Management of Bleeding Complications Current recommendation are based on anecdotal reports No evidence based recommendations 2011 AHA/ACC Guidelines recommend dabigatran-associated hemorrhage be treated with FFP and/or pRBC's -Theoretical benefit -FFP contains thrombin, thus potentially competitively inhibiting dabigatran's effect -Likely limited effect in cases of supratherapeutic dabigatran levels in cases of acute renal failure
- Slide 59
- Reversal? rfVIIa -Rat studies demonstrate reduced bleeding time -Even in absence of TF, rfVIIa generates thrombin -Human experience is limited aPCC -Improved clotting times in animals and humans -Demonstrated in vitro -Unfortunately, thrombogenic Leads to ischemic events
- Slide 60
- Dabigatran is renally excreted -Hemodialysis -Removes 62 % of dabigatran at 2h and 68% at 4h -Human experience is lacking Activated Charcoal -Intentional/Accidental overdose -2-3x serum increase in the setting of normal renal function well tolerated -Admission for prolonged monitoring if ingestion more then that amount
- Slide 61
- Retrospective Within 12 weeks of initial marketing approval for the United States in October 2010, the Institute for Safe Medication Practices reported that dabigatran was responsible for more serious adverse events then 98.7% of all medications Moore et al., Signals for two newly approved drugs and 2010 annual summary. Closed space bleeding is a large concern for ED physicians -Pericardial, ICH, Intraspinal -Medical, Surgical management? All prior modalities of reversal are theoretical/anecdotal
- Slide 62
- Monitoring 75 y/o male with dm, htn, a-fib on Pradaxa. How often should his renal function be monitored? a)Always b)Sometimes c)Never d)Some combination of the above No consensus Significant implications for lack of monitoring in this age group, that is likely to have higher likelihood of bleeding as well as less reserve
- Slide 63
- Clinical Vignette #3 55 y/o man is brought to your hospital after sustaining a frontal crash on I-95. The patient abdomen struck the steering wheel He is complaining of abdominal pain Medical history reveals that he is taking Pradaxa (Dabigatran) for non- valvular atrial fibrillation Ct-imaging demonstrates a retroperitoneal hematoma with a blush Management? A, B, C's PRBC's as needed, IVF IR FFP? PCC? Hemodialysis? Prayer?