A new model for “accept or reject” strategies in off-line and on-line megavoltage treatment...
Transcript of A new model for “accept or reject” strategies in off-line and on-line megavoltage treatment...
Pergamon
Int. J. Radiation Oncology Biol. Phys., Vol. 31, No. 4, pp. 943-952, 1995 1995 Elsevier Science Ltd
Printed in the USA. All rights reserved 0360-3016/95 $9.50 + .00
0360-3016(94)00517-6
• Technical Innovations and Notes
A NEW MODEL FOR "ACCEPT OR REJECT" STRATEGIES IN OFF-LINE AND ON-LINE MEGAVOLTAGE TREATMENT EVALUATION
D I YAN, D . S c . , JOHN W . W O N G , P H . D . , G A R Y GUSTAFSON, M . D .
AND ALVARO MARTINEZ, M.D., F . A . C . R .
Department of Radiation Oncology, William Beaumont Hospital, Royal Oak, MI 48703
Purpose: With megavoltage on-line imaging, a temporal record of the treatment setup variation is made available during the course of radiotherapy. This work describes the theoretical framework where the imaging data is incorporated as feedback for deriving off-line and on-line "accept or reject" decisions to improve the quality of radiotherapy on an individual patient basis. Methods and Materials: A dynamic model of treatment setup variation is developed to describe: (a) the variations of multifraction treatment position and (b) the variation of measurement. Based on this model, a confidence region of subsequent treatment position is estimated from measurements of previous treatment position. The confidence region is compared with an allowance region of the treatment position, representing the acceptable margin of setup variation. The difference of the two regions are then evaluated to derive off-line and on-line "accept or reject" treatment decisions. Results: The model was simulated retrospectively using sequential daily images from different treatment sites. "Accept or reject" decisions were produced for on-line and off-line applications. The results also demonstrate the ability of the model to include the effects of setup variation that drifted during the course of treatment. Conclusion: The preliminary result demonstrates that "accept or reject" treatment decisions can be derived quantitatively from on-line imaging data. The model shows potential to guide the physician and therapist in implementing efficient and accurate treatment adjustments. Further work is required to test the model in the clinical setting.
Megavoltage on-line imaging, Treatment setup variation, Measurement variation, "Accept or reject" deci- sions.
I N T R O D U C T I O N
Substantial daily setup variation exists in conventional radiation therapy (5, 6, 11, 16) and can be detrimental to the treatment goals (5, 10, 15). The negative effect of setup variation is of even greater concern for conformal radiation therapy, where treatment margins are shrunk and dose to the target is escalated. A direct approach to reduce setup error is to increase the frequency of daily portal imaging ( 1 5 ) - - a task made practical with the ad- vent of electronic megavoltage on-line imaging systems. Unfortunately, except for a large catastrophic mistake (for example, the use of wrong shielding block), what consti- tutes an unacceptable error remains unclear. Conse- quently, when daily on-line images are evaluated, it is
difficult to decide when a correction should be made. Incorrect adjustments may be made that might not im- prove setup accuracy. To realize the potential of on-line imaging in improving treatment accuracy, it becomes im- portant to develop an efficient and quantitative model that allows the physician to make proper adjustment decisions.
There are many causes for treatment setup variation. These include inaccurate patient repositioning and beam placement, patient motion during treatment, and organ displacement between treatment fractions. At present, setup variations for an individual patient during the course of treatment have been divided in two types: systematic and random, and are defined by a single Gaussian distribu- tion (3, 7, 8, 14, 18). Systematic variation is considered
Presented at the 35th meeting of ASTRO, New Orleans, LA, October 11, 1993.
Reprint requests to: Di Yan, D.Sc., Department of Radiation Oncology, William Beaumont Hospital, 3601 W. Thirteen Mile Rd., Royal Oak, MI 48703-6769. Acknowledgements--The authors wish to acknowledge Dr. Joos Lebesque, Dr. Arjan Bel, Dr. Shlomo Shalev, and Dr. Jeff
M. Michalski for useful discussion and valuable data. Also we would like to thank Dr. Frank Vicini, Dr. Peter Chen, Dr. Don- ald Brabbins, Dr. Carla Cook, and Dr. Arthur Frazier for their useful input during the development of this concept. Special thanks to the therapists in our clinic for their support.
Accepted for publication 1 September 1994.
943
944 1. J. Radiation Oncology • Biology • Physics Volume 31, Number 4. 1995
Measurement Tool H
On-line Imaging | System [
Estimator ~ " E v a l u a t i o n ~
rreatment ~ , Set up
Fig. 1. Integrated online verification and evaluation system.
ring ]
as the mean of the Gaussian distribution, while the latter is characterized by the standard deviation. Based on the Gaussian model, variation data from patient population have been used to derive objective decisions for setup adjustment (2, 3) and for acquiring more port films (7, 18). However, it is conceivable that the nature of setup variation can be more complex and may drift with time. Apparent linear trend has been observed by Ali A. H. EI- Gayed et al.. for the variation study of pelvic treatment (9). The causes of the drift may be due to changes in patient shapes or degradation of immobilization devices, etc.
In this work, we present a new model for deriving "accept or reject" treatment decisions using on-line im- aging data. The setup variation of the individual patient is characterized to include the potential existence of a drift component, and the effects of measurement uncer- tainty. The history of setup variation is analyzed to esti- mate a confidence region for subsequent setup position. In turn, the confidence region is evaluated with respect to the treatment target and organs at risk to produce an objective value for making "accept or reject" decisions.
Dynamic model,fi~r treatment setup variation In this section, a linear discrete time model is developed
to describe the treatment setup variation for a multifrac- tion clinical treatment. Let the course of a patient treat- ment consists of N tractions. Let X(k), I ~ k <- N, be a positional vector that represents a systematic component and a possible drift component of the setup variation at the kth traction. X(k) is defined in the simulation central axis as the reference coordinate. In our model, the X(k)s from different treatment tractions are assumed to be re- lated such that X(k+l) is a combination of X(k) and a drift that occurs during the time between the treatment fraction k and k+l . For a single patient, X(1), therefore, represents the systematic error between simulation and treatment as defined by other workers (3, 18). For a popu- lation of patient, X(1) has been assumed to have a Gaussian distribution.
The mathematical relation of X(k) is given by,
X(k + 1) = X(k) + ~, (Eq. 1 a)
where ( denotes a possible drift component, and is similar to the concept of Brownian Motion. When equals 0, the X(k) = X(I) for all k and is constant for the entire course of treatment. In our present model, we as- sume that ~ has a Gaussian distribution N(0, ~), with mean 0 and covariance matrix ~. E is treatment site de- pendent.
Rigorously speaking, X(k) can only be inferred by a measurement where the portal image is aligned with a reference image. Let Y(k) be the measured position of the treatment setup in the same coordinate as X(k). The relationship between Y(k) and X(k) at the kth fraction is simply described by,
Y(k) = X(k) + O, (Eq. l b)
METHO DS AND MATERIALS
The following steps show the scheme for making an "accept or reject" decision using on-line imaging data: (a) daily portal images are acquired and the setup varia- tions are measured using an off-line measurement tool; (b) the random noise in the measurement is reduced with a "filter," while the systematic and drift components of the setup variation is estimated; (c) a confidence region for subsequent treatment positions is estimated based on previous measurements and is continuously updated dur- ing the course of treatment; (d) the updated confidence region is compared with a predefined allowance region of setup variation such that a decision can be made to accept or reject the current setup for subsequent treat- ments. In addition, the confidence region can also be used to define a tolerance region for making on-line rejection of a setup if on-line imaging is available. Figure 1 shows the schematic of steps (a) through (d).
where the random vector 0 is due to the combined effects of both the random variation of the treatment setup and the uncertainty, or noise, of the measurement. The random variation of treatment position is by definition an independent parameter. Unlike the drift component ~, the random variation 0 at current treatment fraction will not affect the setup variation of subsequent treatment fraction. In previous studies (2-4, 7), 0 has been assumed to have a Gaussian distribution N(0, O), with a mean of zero and a covariance (~). N(0, ®) is treatment site dependent.
Estimation procedure To make an unbiased estimation of setup variation X(k),
it is important to reduce the effects of random setup and measurement errors. Knowledge of the random vector and 0 becomes important. These probability distribution can be obtained from the goodness-of-fit techniques of a large data sample, or approximated with Gaussian distri- bution.
Accept or reject strategies treatment evaluation • D. YAN et al. 945
treatment position
position measurement I Measurement ~ Y(k)
Tool ~ _.0 Gain Factor ] ~ subsequent estimate
II(K) l ~] GF(k) ' /T 1"I0¢+1)
previous estimate
Fig. 2. Estimation procedure.
Considering the model of Eqs. l a and l b again, let l(k) = [Y(i) I i = I . . . . . k] indicate a set of previous measure- ments of setup variation from treatment fraction 1 to k. Let H ( k + l ) be an estimation of the variation X ( k + l ) after k fractions of setup measurements. Mathematically, H(k+ I ) can be given as an expectation, or mean, for the condition of k previous measurements, that is, Vl(k+ 1) = E(X(k+I ) I l(k)). In other words, FI (k+l ) is the optimal estimate of X(k+ 1) with a priori information l(k) based on the criterion of minimum mean square difference. In same scheme, the well-known Kalman filtering theory (1), can be applied to the model l a and i b to provide the optimal estimate by following recursive formulas,
Vl(k + 1)
= H(k) + S(k) - [S(k) + 6))] '[Y(k) - Fl(k)], (Eq. 2a)
S(k + 1) = S~k, - S~k~[S(k) + O]- 'S(k) + ~,, (Eq. 2b)
where the S(I) = Covar[X(l) , X(I)] , the covariance matrix of the X(1). Due to the lack of appropriate data for input, S(1) will be assumed to have value of ® for all treatment sites in our initial implementation. The initial estimate Vl(l) -- E[X(1)], and is set to be 0, since there is no reason to define a nonzero constant error before first treatment fraction.
Defining a gain factor as GF(k) = S(k) [S(k) + (")]-~, then Eq. 2a can be rewritten as,
Vl(k + l) = H(k) + GF(k)[Y(k) - l](k)], (Eq. 2c)
The recursive formula 2c shows that the optimal esti- mation of subsequent setup variation equals the previous estimate plus a weighted difference of the previous mea- surement and estimate. It implies that k+ 1 estimate will always be modified by the previous k measurements and k estimates as shown in the schematic o f Fig. 2. The gain factor GF plays an important role in the estimator of Eq. 2c, and can be adjusted to change the sensitivity of the estimator. In the case of no drift where ~ = 0, the estima- tion simply converges to the average of previous measure- ments. Here, S(k) = 6)/k, GF(k) = 1/(k+l) and Vl(k+l) = V[(k) + l / ( k+ l ) [Y(k) - H(k)], or H ( k + l ) = I / ( k+ l ) Zi_~ ..... kYu~- The k + l factor is due to the assumption of
zero estimate value as initial condition. On the other hand, in the case of 0 = 0, then GF(k) = I and H(k+ 1) = Y(k). This means that the subsequent estimation will be equal to the most recent measurement if no random setup varia- tion and no measurement noise exist. The above two cases represent two extremes, one assigning equal weight to all previous measurements and the other assigning all weight to the last measurement. In general, the estimation is a kind of running average in which the combination of the covariance matrices, E, ®, and Covar[X(l) , X(I)], plays a role in adjusting the estimator sensitivity.
Finally, H(k+ 1) can be used as the center of a confi- dence region for the estimated k + l setup position after k tractions. The standard residual deviation R(k+ l ), based on the difference between previous measurements and estimations, defines the radius of the region at certain confidence level. The confidence region can then be com- pared to a preset tolerance and plays a key role in the derivation of a treatment decision. Strictly speaking, the confidence region needs to be estimated from at least two portal measurements and updated after each subsequent fraction. In our case, the standard deviation of random variation from the patient population is used to construct the initial confidence region.
Derivation o f off-line "accept or re jec t" decisions The estimated setup position and its corresponding con-
fidence region can be used to derive an "accept or reject" decision. Our first application is to make an off-line deci- sion to reject the setup of subsequent treatment.
Clinical "accept or reject" decisions are based on the deviation of anatomic structures and predefined treatment margins. In this section, a decision model is developed that incorporates (a) each individual patient and each indi- vidual field, (b) predefined target, surrounding critical tis- sues and the corresponding prescribed dose, (c) the con- fidence region of subsequent treatment positions, and (d) clinical knowledge on tumor control and normal tissue tolerance. Figure 3 shows the knowledge-based decision- making scheme.
Allowance region The Allowance Region of treatment setup variation is
defined as a region within which the treatment isocenter
Estimation lMeasurement [ Clinical \ Knowledge
[ Confidence Region [ A CcP;ar~aC e Accept, ....
Allowance Region $
Prescription
Fig. 3. Treatment evaluation decision-making scheme.
Reject >
946 1. J. Radiation Oncology • Biology • Physics Volume 31, Number 4, 1995
is allowed to move, while preserving the predefined mar- gins/'or both target and surrounding tissue, in the presence of setup variations. In this work, the description of mar- gins is based on the definitions of "Clinical Target Vol- ume," "Treated Volume," "Irradiated Volume," and "Organs at Risk" proposed by the Working Group for ICRU Report 50 (12). These volumes are chosen instead of those defined in ICRU Report 29 (13) because the latter does not separate between oncological margin and planning safety margin. Accordingly, the Clinical Target Volume is defined as the Gross Tumor Volume plus vol- ume(s) of suspected clinical disease; the Treated Volume is defined as the volume enclosed by a prescribed isodose surface for tumor eradication; the Irradiated Volume, on the other hand, is a volume that receives a dose considered significant in relation to normal tissue tolerance; the Or- gans at Risk are normal tissues whose presence influence prescribed dose. For treatment evaluation purposes, these volumes are interpreted as either projected two-dimen- sional beam's eye view areas or three-dimensional vol- umes, depending on the methods with which they are measured.
The Allowance Region is a geometric area (or volume) with a radius in any direction from the treatment isocenter, defined by a function of the distance between the bound- aries of the Clinical Target Volume and the Treated Vol- ume, and the distance between the boundaries of the Irra- diated Volume and all Organs at Risk. In the two-dimen- sional case, the mathematical representation of this region is given by,
Allowance Region (AR)
= {r(qS)lr(&) -< Min(llr~(~b + 70 - r2(~6 + 7r)ll,
I[r3(4') - r4(4')11), 0 -< ~b -< 27r, with r,(&) C CTB,
rz(qb) E TVB, r3(qS) • IVB, r4(~b) (E ORB}, (Eq. 3)
C T B - - t h e boundary of clinical target volume; T V B - - t h e boundary of treated volume; I V B - - t h e boundary of irradiated volume; O R B - - t h e boundaries of the organs at risk,
where r denotes the radius and & the polar angle with respect to the reference position coordinate. The set rela- tionship Eq. 3 describes the allowed movement of the treatment isocenter confined by the difference of the Clin- ical Target Volume and the Treated Volume, and the difference of the Irradiated Volume and the Organs at Risk for all directions. The angle ~b+Tr is used for the target boundary because as a field moves in the ~b direc- tion, the target in the opposite direction will have in- creased risk of mistreatment.
Confidence region for deriving treatment decision The Confidence Region to derive treatment decision
incorporates the translational components of setup varia- tion, while the rotational components from the estimator
fi'action k- 1 k k+ 1
• : Mematrement of I.~-eenter Position. 0 : Center of Confidence Region.
t : Allowenee Region. 0 : Confidence Region.
Fig. 4. FOD indication
is used to define the angle of the Confidence Region with respect to the Allowance Region. A geometric region is, thus, defined that contains the subsequent treatment posi- tion at a certain confidence level.
Mathematically, the Confidence Region of treatment position for k+ Ith treatment is defined by,
Confidence Region (CRk+~)
= {xlx = Fl,(k + 1) + Cn, v; v E Vk+ffp)}; (Eq. 4a)
v~+,(p)
= { v l II~ - n , ( k + 1)11 -< ~R,(k + l ) } , (Eq. 4b )
where the estimate Fl(k+ 1 ) and standard residual devia- tion R(k+ 1 ) have been defined previously. The subscripts, t and r, indicate the translational and rotational compo- nents, respectively. Cn, represents the rotational operation matrix, c~ is a constant that defines a confidence level p. The Vk+ 1 (p) defines a set of the possible random varia- tion, v, within a range bounded by -~Rt(k+l) to +~Rt(k+l). Thus, the position and shape of the Confi- dence Region indicate the range of setup variation for subsequent treatment at a confidence level p.
Figure of demerit In our decision model, a Figure of Demerit (FOD) is
used to evaluate the potential risk of mistreatment due to a setup variation. FOD is defined by the ratio between the partial area of the Confidence Region outside the Al- lowance Region, and the entire Confidence Region.
FOD = [(CRk+~ - (AR A CRk+~))/CRk+~]
× p, wi th0_< FOD_< 1, (Eq. 5)
where CRk+I is given by (4a), and AR by (3). p is the confidence level for the Confidence Region after k fractions of treatment. Figure 4 demonstrates the intercept of the Allowance Region and the Confidence Region that is used to calculate a FOD.
According to Eq. 5, if the Confidence Region estimated from k previous treatments is contained by the Allowance
Accept or reject strategies treatment evaluation • D. YAN et al. 947
Region, then FOD equals 0, indicating a good treatment. In this case, the probability of the subsequent treatment position to lie within the acceptable treatment margin will be at least p (a typical value will be > 95%). If the Confidence Region is not entirely inside the Allowance Region, then the FOD will have a value proportional to the probability of the subsequent treatment position to lie outside the acceptable treatment margin, indicating a level of potential risk.
Deriwlt ion o f on-line "accept or re j ec t " decision The estimated treatment position and the confidence
region after k treatments can also be applied to a template of anatomical structures for display on the portal image at the k+ 1 treatment. Initially, a template of anatomical structures of interest is defined, similar to the one used in the Cumulative Verification Image Analysis (CVIA) software tool (1 l, 14) for aligning portal images with the reference prescription image. As the treatment progress, the confidence region of the anatomical template for sub- sequent treatment can be estimated and displayed on the monitor of an on-line imaging system prior to the capture of the portal image and, thus, provides guidelines for the observer to make an on-line accept or reject decision of the setup.
Implementat ion Daily port films were obtained for several head and
neck, lung, and pelvic cancer patients. The prescription on the simulation film was used as reference. The two- dimensional treatment setup variations from the refer- ences were measured using the CVIA software tool. The feasibility of using the estimation procedure to provide decision criteria for off-line and on-line accept or reject decisions was simulated retrospectively by comparing the estimated results with measured data.
The estimation procedure requires the covariance ma- trices, O and ~, as input. In practice, the covariance of random setup variation and measurement noise, ®, would be derived from the setup variation of a large patient population and from the data of a large group of clinicians aligning phantom images of known setup variation. The covariance of actual drift, ~, has to be estimated in our present work but can be adjusted during the clinical use of the tool. For our feasibility study, the main diagonal components of covariance matrix (9 was estimated from the random setup deviations published in previous studies as shown in Table 1. Our translational variances of the O in x and y directions were assumed to be equal to the variances listed in Table 1, as the latter did not contain directional information. Rotational variance was taken to be 1.5 ° from the data of Michalski et al. (14). The re- maining components of O were assumed to be 0. The value of ~ was simply taken as half of the O. More reasonable value of ~ can be obtained from further clini- cal study.
In the implementation of our off-line decision model,
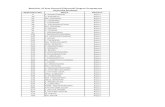
Table I. or, and a,, are standard deviation of random variation for treatment position and measurement random error
Treatment Measurement Treatment site o, (mm)* c% (mm) t
Head and neck 1.2 1.5 Pelvis 3.0 1.0 Mantle/thorax 3.5 1.5
* c~, derived from the data of several institutes that has been summarized by Dr. Shalev, Shlomo (personal communication, May, 1993).
t ~,~ derived from Dr. Jeff M. Miichalski's article [16].
we used the 50% is®dose line with an added uniform margin of 6 mm to approximate the two-dimensional Irra- diated Volume boundary and an subtracted uniform mar- gin of 6 mm to approximate Treated Volume boundary. The implementation consisted of the toll®wing steps:
1. The physicians outlined the clinical target and sur- rounding critical normal tissues. In addition, they pre- scribed the dose levels. The physicians also defined the anatomical structures for on-line decision.
2. The Allowance Region of the treatment is®center was created using ideally the first approved portal image, otherwise, the simulation film. The former was pre- ferred to include the possible effect of block cutting error.
3. The daily portal images were aligned and setup varia- tion were measured using the CVIA tool.
4. The estimator produced the estimation of subsequent treatment position and the corresponding confidence region.
5. The FOD was evaluated before a subsequent treatment, and was translated as clinical criteria for accept, atten- tion, or reject action. In this study, the assignment of FOD to these action is listed in Table 2. As the study progresses, the FOD would be matched to the actual decision made by the physicians.
RESULTS
The data obtained from three patients is depicted in Fig. 5. It shows plots of measured x and y translational and rotational variations of the daily treatment fields from the reference central axis for a (a) lung, (b) head and neck, and (c) pelvic case. The dotted lines show the esti- mations that would appear ahead of the measurements as indicated by the solid lines. The plots show the ability of
Table 2. Initial acceptance criteria
Decision FOD
Accept ~ 0.l 5 Attention 0.15 -- 0.4 Reject > 0.4
I. J. R a d i a t i o n O n c o l o g y • B i o l o g y • Phys i c s 948 V o l u m e 31, N u m b e r 4, 1995
12.5
7.5
2.5
-2.5
-7,5
-12.5
12.5
73
2.5
X sh i f t ( r a m )
- - .
1' - ' ' ~ ' ~ l~l ' • • • 1 ~
Y sh i f t ( m m )
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . : :zo:_-_-~ . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . -2.5 - - - _. - .
-7,5
~2"5
6.0
3.6
1,2
-1.2
-3.6
-6.0
f 8 t l 1 ~
R o t a t i o n ( d e g r e e )
12.5
7.5
2.5
-2"5
-7"5
-12~ =
12.5
7.5
2.5
-23
-73
-123 _
6.0
3.6
1.2
1.2
-3.6
X sh i f t ( m m )
Y sh i f t ( r a m )
. . . . . . . . . . . . . ;:~;ii2_-? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . ;- - - O- ---~ . . . . . . . . • . . . . . . . . • . . . . . . . . . . . . . . . . •
1 r • , T " , ~ - - . l~l '
R o t a t i o n ( d e g r e e )
-6.0
F i g . 5 . ( a ) H o r i z o n t a l , v e r t i c a l , a n d a n g l e v a r i a t i o n f o r a l u n g t r e a t m e n t . ( b ) H o r i z o n t a l , v e r t i c a l , a n d a n g l e v a r i a t i o n
f o r a h e a d a n d n e c k t r e a t m e n t . ( c ) H o r i z o n t a l , v e r t i c a l , a n d a n g l e v a r i a t i o n f o r a p e l v i s t r e a t m e n t .
Accept or reject strategies treatment evaluation • D. YAN et al. 949
12.5
7.5
2.5
2,5
7 3
-12.5
12.5
7.5
2.5
2.5
-12.5
6,0
3.6
1.2
-1.2
3.6
6.0
X shi f t ( m m ) - " ~ " ~ l ~ _ . - o
1' II fl 1~
Y shift ( m m )
1 II fl I~
Rota t ion (degree)
.o-. . . . . . -0-.
f {i fl i~
Fig. 5. (Con t ' d )
the model to estimate the trend of the drift. The example for the head and neck patient (Fig. 5b) was chosen to demonstrate the tracking ability of the estimator during the case of no drift or small drift case.
Figure 6 show the Allowance Region (the black area), the estimated Confidence Region (the gray area), mea- sured setup variation (the black dot), and the resultant accept or reject decisions for the (a) lung, (b) head and neck, and (c) pelvis case of Fig. 5 throughout the course of treatment. An 8 mm uniform margin was used to define the Allowance Region for the lung and the pelvis cases and a 5 mm margin for the head and neck. The Confidence Region was updated after each treatment. For the lung case, a drift occurred in the superior and inferior direction (the y axis), as shown in Fig. 5a, which caused the deci- sion model to warn the observer after the 13th treatment due to a trend of the treatment isocenter drifting out of the allowance region, as shown in Fig. 6a. For the head and neck case in Fig. 5b, a larger random variation oc- curred in the x direction that formed the major axis of the elliptical shape of the confidence region, as indicated by Fig. 6b. Interestingly, the results suggest that despite the existence of a large systematic error in the y direction, the decision to accept or reject was more influenced by the effects of the random variation along the x direction. Such a decision process would not likely be made in conventional clinical verification using weekly portal films. Figure 5c shows a large drift of the pelvic treatment,
which leads to a rejection decision after the 9th fractions shown in Fig. 6c.
Figure 7 shows a template of bony landmarks with a 95% confidence region superimposed on a portal image of the head and neck patient prior to image alignment with CVIA. As mentioned earlier, the confidence region of anatomical template can be adapted for display on the monitor of an on-line imaging system. This type of on- line application is more suitable for rejecting unexpected large setup errors.
DISCUSSION
Conventional treatment evaluation using weekly portal films is based on criteria established from patient popula- tion averages. Values such as 5 mm to 10 mm have been used widely for adjusting a treatment setup based on a post-treatment port film. Since daily portal images are not available in most clinics, methods have not been devel- oped to distinguish systematic variation, drift variation, and random variation for the individual patient. Indeed, setup adjustment requested by physicians are based on a few port films that inherently assumes systematic setup error. With the advent of on-line imaging providing a wealth of verification data, it is becoming apparent to the clinicians that the so called "conventional treatment margin" may be modified for some treatment sites. Also, a higher dose could be delivered for some patients in dose
95O
L Attention 40.18)
1. J. R a d i a t i o n O n c o l o g y • B i o l o g y • P h y s i c s
2. Attention (020) 3 Accept (0.05) 4. Accept 40.00)
q
V o l u m e 31 , N u m b e r 4 , 1995
1. Accep t (0.[1{)) 2, Accep t (0 .00) 3. Accept (0.00) 4. Accept (0.13)
5. Accept (0.02) 6. Accept (0 10) 7. Accept (0.08) 8 Accept (0.10) 5 Accept (D.I[I) 6. Attention (0.15) 7 Accept (0.05) 8. Attention (11.19)
, q , q
k
9 Accept (0.03) 10Accept (0.02) llAcc*pt (0.10) 12Accept(0.13) 9. Attention((I.21) lOAttention(0 18) llAccept(0.10) 12Attention (0.20)
" 1 . ,q
k I
q
, J
13AtmnUon (0.15) 14. 13Attention (0.29) 14.
r
k
a
1 .,\ec~apt (0.11 ) 2 Attent ion ((3.32)
J
.'1. Attention (0.29)
ft. Attention (0.17) 6. Attention (0.19) 7 Attention (0.29) 8. &ttention (0.36)
9. Reject (0.47) 10Attention ({) 40) I ll~eject (0.65) 121k-~ject (0 73)
13ge j ec t ([) 86) 14.
C
Fig. 6. (a) Clinical decision plotting for a lung treatment. (b) Clinical decision plotting for a head and neck treatment. (c) Clinical decision plotting for a pelvis treatment.
escalat ing studies, provided that an efficient and accurate method is avai lable to evaluate and adjust inevi table treat- ment variation in a t imely fashion.
In this article, a quanti tat ive approach to der ive on- line and off-l ine "accep t or r e jec t " t reatment decis ion is proposed. The "accep t or re jec t" decis ion is based on the history of treatment setup variat ion for an individual patient. It is also heavi ly influenced by the physic ians prior knowledge of outcome fol lowing standard treat-
ment. The concept of F O D provides a quanti tat ive esti- mate of t reatment decis ion that, up to now, have been made on a subject ive basis.
Addi t ional research is needed before our proposed deci- s ion-making concept can be real ized for standard cl inical use. For those patients where the treatment setup variat ion is roughly equal to the treatment margin, the decision to accept or reject a t reatment setup is not clear and most l ikely will be physician dependent . There may not exist
Accept or reject strategies treatment evaluation • D. YAN et al. 951
Fig. 7. Template of tolerance region for a head and neck treatment.
a definitive rule to follow, such that an exact mathematical criterion may not exist. It appears more reasonable that the objective decision criteria, such as the calculated FOD in our proposal, be matched with the actual clinical deci- sions. Artificial intelligence or knowledge-based methods need 1o be created to train both the physicians and the decision making algorithm on the matching of clinical decisions with objective functions. Other important devel- opments include the issue of automatic image alignment algorithms to speed up the process and the improvement of image quality from on-line imaging systems to reduce the magnitude of measurement noise. Clinically, the tem- plate of estimated anatomical positions needs to be incor- porated in the display of on-line imaging system to assist the therapist in making on-line treatment decision. Later on, the new data can be reentered into the treatment plan-
ning system for isodose calculation, updating the physi- cian with the dosimetric consequences of treatment setup variation.
The concepts presented in this article represent initial steps of integrating information from on-line imaging with a treatment evaluation system. With the recent em- phasis on three-dimensional conformal megavoltage ther- apy, for which higher doses of radiation are expected to be delivered to tumors, the development and implementa- tion of "Accept or Reject" strategies goes hand in hand. However, a difficult problem remains. Despite the ability of the clinician to declare a treatment setup unacceptable, the decision model does not identify the source of treat- ment error. Research eflbrt must be directed towards the derivation of the proper corrective action that forms the final crucial step to help improve treatment accuracy.
REFERENCES
1. Anderson, B. O.; Moore, J. B. In: Kailath, R., ed. Optimal filtering, a information and system science series. Engle- wood Cliffs, NJ: Prentice Hall; 1979.
2. Bel, A.; van Herk, M.; Bartelink, H.; Lebesque, J. V. A verification procedure to improve patient set-up accuracy using portal image. Radiother. Oncol. 29:253-260; 1993.
3. Bijhold, J.; Lebesque, J. V.; Hart, A. A. M.; Vijlbrirf, R. E. Maximizing setup accuracy using portal images as applied
to a conformal boost technique for prostatic cancer. Ra- diother. Oncol. 24:261-271; 1992.
4. Bissett, R.; Ryder, S.; Leszczynski, K.; Cosby, S.; Duns- combe, P.; Lightfoot, N. Efficiency and decision making in on-line portal verification. 34th ASTRO, San Diego; 1992.
5. Brahme, A. Dosimetric precision requirements in radiation therapy. Acta Radiol. 23:379-391; 1984.
6. De Neve, W.; Van den Heuvel, F.; De Beukeleer, M.;
952 I.J. Radiation Oncology Q Biology Q Physics Volume 31, Number 4, 1995
Coghe, M.; Thon, L.; De Roover, P.; Van Lancker, M.; Storme, G. Routine clinical on-line portal imaging followed by immediate field adjustment using a tele-controlled pa- tient couch. Radiother. Oncol. 24:45-54; 1992.
7. Denham, J. W.; Dally, M. J.; Hunter, K.; Wheat, J.; Leslie, G.; Fahey, P. P.; Hamilton, C. S. Objective decision-making following a portal film: The results of a pilot study. Int. J. Radiat. Oncol. Biol. Phys. 26:869-876; 1993.
8. Dutreix, A.; van der Schueren, E.; Leunens, L. Quality control at the patient level: Action or retrospective intro- spection. Radiother. Oncol. 25:146-147; 1992.
9. E1-Gayed, A. A. H.; Bel, A.; Vijlbrief, R.; Bartelink, H.; Lebesque, J. V. Time trend of patient setup deviations dur- ing pelvic irradiation using electronic portal imaging. Ra- diother. Oncol. 26:162-171; 1993.
10. Goitein, M.; Busse, J. Immobilization error: Some theoreti- cal considerations. Radiology 117:407-412; 1976.
l l. Halverson, K. J.; Leung, T. C.; Pellet, J. B.; Weinhous, M. S.; Wong, J. W. Study of treatment variation in the radiotherapy of head and neck tumors using a fiber-optic on-line radiotherapy imaging system. Int. J. Radiat. Oncol. Biol. Phys. 21:1327-1336; 1991.
12. ICRU Report 50, International commission of radiation units and measurements, prescribing, recording and re- porting photon beam therapy; 1993.
13. 1CRU Report 29, International commission of radia- tion units and measurements, dose specification for report- ing external beam therapy with photons and electrons; 1978.
14. Lebesque, J. V.; Bel, A.; Bijhold, J.; Hart, A. A. M. Detec- tion of systematic patient setup errors by portal film analy- sis. Radiother. Oncol. 23:198; 1992.
15. Marks, J. E.; Haus, A. G.; Sutton, H. G.; Griem, M. L. The value of frequent treatment verification films in reducing localization error in the irradiation of complex fields. Can- cer 37:2755-2761 ; 1976.
16. Michalski, J. M.; Wong, J. W.; Gerber, R. L.; Yan, D.; Cheng, A.; Graham, M. V.; Renna, M. A.; Sawyer, P. J.; Perez, C. A. The use of on-line image verification to esti- mate the variation in radiation therapy dose delivery. Int. J. Radiat. Oncol. Biol. Phys. 27:707-716; 1993.
17. Michalski, J. M.; Wong, J. W.; Bosch, W. R.; Yan, D.; Cheng, A.; Gerber, R. L. An evaluation of two methods of anatomical alignment of radiotherapy portal images. Int. J. Radiat. Oncol. Biol. Phys. 27:1199 1206; 1993.
18. Mitine, C.; Leunens, G.; Verstrate, J.; Blanckaert, N.; Van Dam, J.; Dutreix, A.; van der Schueren, E. Is it necessary to repeat quality control procedures for head and neck pa- tients'? Radiother. Oncol. 21:201-210; 1991.