522 Routine second trimester ultrasound reduces the risk of Down Syndrome following a positive...
-
Upload
kenneth-lim -
Category
Documents
-
view
212 -
download
0
Transcript of 522 Routine second trimester ultrasound reduces the risk of Down Syndrome following a positive...
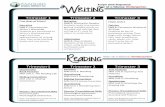
Volume 185, Number 6 A m J Obstet Gynecol
520 THE RELATIONSHIP OF STILLBIRTH TO MATERNAL SERUM ALPHA FETOPROTEIN AND HUMAN CHORIONIC GONADOTROPIN ROSA WON 1, BOB CURRIER 2, FRED LOREY 2, DENA TOWNER~; ~University of California, Davis, Obstetrics and Gynecology, Sacramento, CA; 2Genetetic Disease Branch, DHS, Berkeley, CA; 3University of California, Davis, Obstetrics & Gynecology, Sacramento, CA
OBJECTIVE: To determine whether elevations in maternal serum alpha fetoprotein (MSAFP) and maternal serum human chorionic gonadotropin (MShCG) have an impact on the timing of stillbirths.
STUDY DESIGN: There were 44,525 women with known outcomes identified from the California State Expanded AFP program. All had normal ultrasounds and all with amniocentesis had normal karyotypes. Pregnancies ended in stillbirth after 24 weeks in 272 cases. MSAFP, MShCG and gestational age (GA) in days at time of stillbirth were available for 242. Student t test and multiple regression were used for analysis.
RESULTS: Elevated MSAFP and MShCG were found in 53 cases, MSAFP >2.5 MOM in 130 and MShCG >2.0 in 104. The incidence of stillbirth was 6.1/1000 overall. GA at time of stillbirth fi~r MSAFP >2.5 was 217.7 +_ 3.1 days SE vs. 238.6 _+ 3.7 tbr MSAFP <2.5 (P< .0001). MShCG had no correlation with GA at stillbirth (MShCG >2.0, 226.9 _+ 3.7 vs. MShCG <2.0, 227.6 _+ 3.5, P = .89). Those with MShCG >4.0 were further subdivided and lhere was no difference in GA at time of stillbirth (P= .51 ). In the figure, cumulative stillbirths over GA can be seen with respect to elevated MSAFE
CONCLUSION: It appears that the incidence of stillbirth (6.1/1000) in this highly selected and at risk population is not increased fi'om the baseline incidence in Calitornia (5.6/1000). Stillbirths occur earlier in women with an elevated MSAFP, but an elevated MShCG does not seern to correlate with the timing of stillbirths.
Figure Cumulative stillbirths
CumuI~live Stil b i ' th
y 521 "FLUSH AFTER YOU ARE FINISHED"--THERE ARE RESIDUAL VII J.l I N
THE CATHETER, SYRINGE, AND NEEDLE AFTER CVS SPECIMEN HAS BEEN TRANSFERRED TO THE COLLECTION TUBE LAURA GORSKI 1, STUART WEINER 1, MARK HAYNES'-', BRUCE SMITH 2, VINCENZO BERGHELLA1; 1Thomas Jeffi~rson University, Obstetrics and Gynecology', Philadelphia, PA; 2Thomas Jefferson University, Rheumatology, Philadelphia, PA
OBJECTIVE: To determine if there are residual villi in the syringe, catheter, or needle after the chorionic villus sampling (CVS) specimen has been transterred to the collection tube.
STUDY DESIGN; Women presenting for CVS for genetic testing between 10 0 /7 and 12 6 /7 weeks' gestation were offered participation in the stud),. The study was approved by the IRB and the patients were consented. Trans- ahdontinal (TA) and transcervical (TC) CVS were collected t?om the catheter and syringe (TC) or needle (TA) as per routine. After collection, the syringe, catheter or needle fi'om the participants were flushed with media. The new specimen was then transferred to the lab within 2 hours. Chorionic villi were identified and separated with microscopy, washed with a PBS solution, and frozen for later analysis, mRNA was isolated fi-om the specimens using oligo-dT cellulose. Isolated mRNA was then assayed by RT-PCR using primers specific for GADPH and 1L-4.
RESULTS: 16 patients agreed to participate in this study. Of 12 syringes, catheters, and needles flushed aider routine transfer to the collection tube, 5 (42%) of the specimens contained GADPH and 3 (25%) of the specimens were weakly positive Ior GADPH. Of 16 syringes, catheters, and needles flushed at~.er routine transfer to the collection tube, 6 (38%) of the specimens contained 1L4. Both TA and TC CVS techniques demonstrated mRNA.
CONCLUSION: There are residual villi and available mRNA in the cathetel, syringe, and needle after the CVS specimen has been transterred to the collection tube. Without interfering with the genetic specimen, this residual mRNA can be used tor both clinical genetic or research purposes.
522
SMFM Abstracts S223
ROUTINE SECOND TRIMESTER ULTRASOUND REDUCES THE RISK OF DOWN SYNDROME FOLLOWING A POSITIVE MATERNAL SERUM SCREEN KENNETH LIM 1, LAURA ARBOUR 2, R WILSON 1, DAWN SICIL- IANO, MS 2, LEEANNE DAHLGREN DR 3, LAURIE AINSWORTH2: ] University of British Colmnbia, Obstetrics & Gynaecology, Vanconver, British Columbia; 2University of British Columbia, Medical Genetics, Vancouver, British Colum- bia; 3University of British Columbia, Obstetrics and Gynecology, Vancouver, British Columbia
OBJECTIVE: To determine the sensitivity, specificity, positive and negative likelihood ratios of a routine, detailed, mid-trimester anatomical scan for Trisomy 21 (T21), tollowing a positive maternal serum screen (+MSS) test.
STUDY DESIGN: Retrospective case-control. The provincial cytogenetic and medical genetics databases were cross reterenced to identify referred cases of +MSS (>1:385), with 1) cytogenetic confirmation of T21 and 2) complete mid-trimester anatomical scan prior to knowledge of ka~otype. The Control group consisted of the next four +MSS cases (N karyotype with detailed scan) following each identified case ofT21. A detailed scan was considered abnormal if a major fetal abnormality/condition was noted by the reporting sonologist. Soft markers were not considered in this analysis. Only cases with US performed in our center were considered for this analysis.
RESULTS: There were 45 cases ofT21 and 180 euploid cases identified. Of these, 35 T21 and 135 Control cases had a detailed ultrasound at BC Women's Hospital. An abnormal routine anatomical scan had a sensitivity for T21 of 60.0% (95% CI: 42.2%, 75.6%) and a specificity of 95.6% (95% CI: 90.2%, 98.2%). The positive and negative likelihood ratios were 13.5 (95% CI: 5.9, 30.9) and 0.42 (95% CI: 0.28, 0.63) respectively. If the MSS risks were modified (retrospectively) according to the results of the detailed ultrasound (ie. cases with a MSS risk of <1:240 and a normal scan are not offered amniocentesis), 33/35 cases ofT21 (94.3%, [95% CI: 79.5%, 99.0%) would have been offered amniocentesis whereas 57/135 euploid cases (42%) would not.
CONCLUSION: A routine mid-trimester anatomical scan can significantly modify the risk of T21 tollowing a +MSS. This could result in a reduction of amniocentesis pertormed by 42%, while detecting 94.3% of T21 fetuses that would have been identified by the provincial MSS program.
523 IS INHERITED THROMBOPHII JA EVALUATION WARRANTED IN CAU- CASIAN WOMEN WITH POOR OBSTETRIC HISTORY?. TULIN OZCAN 1, HENRY M RINDER 2, ANITA KARNEA :3, JOSHUA COPEL 4, URANIA MA- GR1PLES4; tYale University, Obstetrics and Gynecology', New Haven, CT; 2yale University, Laboratory Medicine, New Haven, CT; ~Yale University, Obstetrics and Gynecology, New Haven, CT; 4yale University, Obstetrics and Gynecology, New Haven, CT
OBJECTIVE: To assess whether the prevalances of inherited thrombo- philia is increased in Caucasian women with poor obstetric histol T.
STUDY DESIGN: A retrospective study of patients ot Caucasian ethnicity ref;erred for pregnancy complications who had a thrombophilia evaluation. The prevalances of Factor V Leiden AI691G (FVL), methylene tetrahydroxy- folate reductase C677T (MTHFR) and prothrombin G20210A (ProG) nmta- tions were compared with the prevalances of a historical control popula- tion.Only homozygosity for MTHFR was included for statistical analysis.
RESULTS: There were 130 Caucasian women who were tested fc, r inherited thrombophilia. The indications were equal to or more than 3 miscarriages at 1st TM (22), second and third TM losses (28), preeclampsia (26), growth restriction (9), thrombotic events (16), abruption (10) and combinations (19).
CONCLUSION: Caucasian women with poor obstetric history have an increased prevalence of FVL and MTHFR nmtations. Prothrombin gene mutation prevalence appears to be similar in the study population compared to the control group.
Table
EXPECTED PREVALAN CE PREVALANCE P
FVL (Heterozygosity and 18.3% 3.5% .001 homozygosity)
ProG (Hetero~,gosity, and 5.3% 2.6% >.05 homozygosity)
MTHFR (Homozygosity) 17.8% 7.1% .027











![Elevated Serum Creatine Kinase BB Levels in Patients with ... · serum CK-BB (>10 ng/ml) [range, 11 to 522 ng/ml; median, 40.0 ng/ml; mean, 76.0 ±19.2 (S.E.)]. Only 1 of 42 patients](https://static.fdocuments.us/doc/165x107/601acf0e09c473280b7133e1/elevated-serum-creatine-kinase-bb-levels-in-patients-with-serum-ck-bb-10.jpg)




