2016 - Endo Bridge · 2020. 11. 18. · 2016 2 20 - 23 October, 2016 Antalya - Turkey SCIENTIFIC...
Transcript of 2016 - Endo Bridge · 2020. 11. 18. · 2016 2 20 - 23 October, 2016 Antalya - Turkey SCIENTIFIC...
-
w w w . e n d o b r i d g e . o r g
Bridging the World of Endocrinology
SELECTED CASES
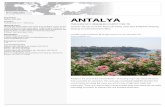
201620 - 23 October 2016
Cornelia Diamond Hotel, Antalya - Turkey
-
2016
220 - 23 October, 2016 Antalya - Turkey
SCIENTIFIC PROGRAM
Friday, 21 October 2016
08.40-09.00 Welcome and Introduction to EndoBridge 2016
MAIN HALL09.00-09.3009.30-10.00
10.00-10.3010.30-11.00
Chairs: Jens Bollerslev, Refik TanakolRecent advances in clinical and molecular understanding of metabolic bone disease - Nilgün Güvener Demirağ Approach to “drug holidays” “treatment failures” and possible combination therapy for postmenopausal osteoporosis Hasan AydınMedical therapy in primary hyperparathyroidism - Peter SchwarzUpdate on Vitamin D - Skeletal and nonskeletal effects - Ghada El-Hajj Fuleihan
11.00-11.20 COFFEE BREAK
11.20-12.50 HALL AHALL BHALL CHALL D
Interactive Case Discussion Sessions see page 5 for detailsBone / Calcium - Jens Bollerslev, Alper GürlekThyroid - Ralf Paschke, Seda SancakObesity / Lipids - Marc Cornier, Oğuzhan DeyneliMale Reproductive Endocrinology - Joshua Safer, Andrea Isidori
12.50-14.00 LUNCH
14.00-15.30 HALL AHALL BHALL CHALL D
Interactive Case Discussion Sessions see page 5 for detailsBone / Calcium - Peter Schwarz, Ghada El-Hajj FuleihanThyroid - Michael McDermott , Georg BrabantObesity / Lipids - Marc Cornier, Sinem Küçüksaraç Kıyıcı Female Reproductive Endocrinology - Duarte Pignatelli, Füsun Saygılı
15.30-15.50 COFFEE BREAK
MAIN HALL15.50-16.2016.20-16.5016.50-17.2017.20-17.50
Chairs: Georg Brabant, M. Sait GönenPerplexing thyroid function tests - Michael McDermott Management of subclinical thyroid dysfunction including pregnancy - Georg Brabant Molecular diagnostic testing in evaluation of thyroid nodules - Ralf PaschkeDifferentiated thyroid cancer: Which type of surgery? How much RAI? How much suppression? - Ayşe Kubat Üzüm
-
2016
320 - 23 October, 2016 Antalya - Turkey
SCIENTIFIC PROGRAMSaturday, 22 October 2016
MAIN HALL09.00-09.3009.30-10.0010.00-10.3010.30-11.00
Chairs: Camilla Schalin-Jäntti, Bülent Yıldız Management of hyperglycemia and cardiovascular disease in type 2 diabetes - Rita Kalyani What is new in insulin therapy of diabetes? - Richard HoltDiabetes technologies: Current use and future perspectives Hans De VriesBariatric-metabolic surgery in type 2 diabetes - Kåre Birkeland
11.00-11.20 COFFEE BREAK
11.20-12.50 HALL AHALL BHALL CHALL D
Interactive Case Discussion Sessions see page 6 for detailsDiabetes - Kåre Birkeland, Rita Kalyani Adrenal - Massimo Terzolo, Özlem ÇelikPituitary - AJ Van Der Lely, Nurperi GazioğluNeuroendocrine Tumors - Camilla Schalin-Jäntti, Eva Tiensuu Janson
12.50-14.00 LUNCH
14.00-15.30 HALL AHALL BHALL CHALL D
Interactive Case Discussion Sessions see page6 for detailsDiabetes - Hans De Vries, Mohamed Hassanein Adrenal - Jerome Bertherat, Tevfik Demir Pituitary - Vera Popovic, John WassNeuroendocrine Tumors - Camilla Schalin-Jäntti, Eva Tiensuu Janson
15.30-15.50 COFFEE BREAK
MAIN HALL15.50-16.2016.20-16.5016.50-17.2017.20-17.50
Chairs: George Mastorakos, Fahri BayramThe “omics” of adrenocortical cancer - Jerome Bertherat Approach to adrenal incidentaloma: 2016 guidelines -Massimo TerzoloMale hypogonadism - Andrea IsidoriCare of transgender patients - Joshua Safer
-
2016
420 - 23 October, 2016 Antalya - Turkey
SCIENTIFIC PROGRAMSunday, 23 October 2016
MAIN HALL09.00-09.3009.30-10.0010.00-10.3010.30-11.00
Chairs: AJ Van der Lely, Melek Eda ErtörerEvaluation and management of sellar masses - Vera Popovic Can we really cure Cushing’s disease? - Susan Webb Medically refractory prolactinoma - John WassChallenges and controversies in diagnosis and management of acromegaly - Pınar Kadıoğlu
11.00-11.20 COFFEE BREAK
MAIN HALL11.20-11.50
11.50-12.20
12.20-12.5012.50-13.20
Chairs: Marja-Riitta Taskinen, İlhan YetkinAbdominal obesity, type 2 diabetes and cardiometabolic health - Amika Singh* Supported by International Chair on Cardiometabolic Risk
Ectopic fat: A new target for CVD risk management - Marja-Riitta Taskinen* Supported by International Chair on Cardiometabolic Risk
Food addiction: Does it really exist? - AJ Van der Lely The evolving science of nutrition and nutritional quality- Reyhan Nergiz Ünal
13.20-13.30 Closing comments and adjourn
-
2016
520 - 23 October, 2016 Antalya - Turkey
SELECTED CASESDATE TIME HALL SESSION TITLE
21.10 11.20-12.50 A Bone/Calcium O-01 / Postoperative Hypoparathyroidism: Treatment With Teriparatide
21.10 11.20-12.50 A Bone/Calcium O-02 / A case of primary hyperparathyroidism diagnosed during pregnancy
21.10 11.20-12.50 A Bone/CalciumO-03 / A striking finding during intraoperative jugular sampling in a case of parathyroid adenoma with low-normal serum intact parathyroid hormone levels
21.10 11.20-12.50 B Thyroid O-04 / A case of hypothyroidism requiring parenteral levothyroxine treatment
21.10 11.20-12.50 B Thyroid O-05 / Primary thyroid lymphoma presenting with subacute thyroiditis
21.10 11.20-12.50 B Thyroid O-06 / A rare case of thyrotoxic periodic paralysis with accompanying transient hyperglycemia
21.10 11.20-12.50 B Thyroid O-07 / A case with MEN-2b who has neurinoma of the tongue and eyes
21.10 11.20-12.50 B ThyroidO-08 / A case of papillary thyroid carcinoma in toxic adenoma: Are hyperfunctioning nodules truly innocent all the times?
21.10 11.20-12.50 B Thyroid O-09 / Medically refractory amiodarone-induced thyrotoxicosis: Two case reports
21.10 11.20-12.50 C Lipids/ObesityO-10 / Metabolic abnormalities associated with insulin resistance in a young patient with acquired partial lipodystrophy
21.10 14.00-15.30 A Bone/Calcium O-12 / Effect of zolendranate treatment on hearing loss in a patient with the Paget’s disease who has skull involvement
21.10 14.00-15.30 A Bone/Calcium O-13 / Thyroid nodule or parathyroid adenoma: a case report
21.10 14.00-15.30 B Thyroid O-14 / A case of thrombotic thrombocytopenic purpura in a toxic multinodular goiter patient on antithyroid medication
21.10 14.00-15.30 B ThyroidO-15 / Agressive follicular variant of papillary microcarcinoma presenting with extensive bone metastases and associated with weird thyroid function tests
21.10 14.00-15.30 B Thyroid O-16 / Thyrotoxic Periodic Paralysis
21.10 14.00-15.30 B Thyroid O-17 / Thyrotoxicosis with pleural effusion and hypoalbuminemia
21.10 14.00-15.30 B ThyroidO-18 / Plasmapheresis as a temporary management option in a patient with Graves’ disease and primary sclerosing cholangitis
21.10 14.00-15.30 B Thyroid O-19 / A lump on the scalp: An unusual presentation of papillary thyroid carcinoma
21.10 14.00-15.30 C Lipids/Obesity O-20 / Wernicke encephalopathy in a case who had gastric bypass surgery due to morbid obesity
-
2016
620 - 23 October, 2016 Antalya - Turkey
DATE TIME HALL SESSION TITLE
22.10 11.20-12.50 A Diabetes O-21 / The investigation for celiac disease in a newly diagnosed patient with diabetes is necessary in any case
22.10 11.20-12.50 A Diabetes O-22 / Mauriac syndrome still exists; a rare complication of type 1 diabetes mellitus
22.10 11.20-12.50 B AdrenalO-23 / Unilateral adrenalectomy improves cushing syndrome in a patient with primary bilateral macronodular adrenal hyperplasia
22.10 11.20-12.50 B Adrenal O-24 / CAH presenting as premature puberty with associated testicular adrenal rest tumors (TART)
22.10 11.20-12.50 B Adrenal O-25 / Different clinical presentations in three patients with adrenocortical cancer
22.10 11.20-12.50 B Adrenal O-26 / Bilateral cystic hemorrhagic adrenal incidentalomas
22.10 11.20-12.50 B AdrenalO-27 / Adrenocortical carcinoma presenting with Cushing’s syndrome in a patient with 8 years history of adrenal insufficiency and adrenomyolipomas
22.10 11.20-12.50 C Pituitary O-28 / Idiopathic granulomatous hypophysitis mimicking pituitary adenoma
22.10 11.20-12.50 C Pituitary O-29 / Case of giant prolactinoma in young man
22.10 11.20-12.50 C Pituitary O-30 / Pituitary stalk interruption syndrome: a rare cause of panhypopituitarism
22.10 11.20-12.50 D Neuroendocrine tumorsO-31 / How multifocal insulinomas can be diagnosed and treated in a case with MEN-1 disease?
22.10 11.20-12.50 D Neuroendocrine tumorsO-32 / Catastrophic Cushing’s Syndrome: Report of a mortal case
22.10 14.00-15.30 A Diabetes O-33 / Effect of Imatinib on insulin therapy in a patient with Type 2 DM
22.10 14.00-15.30 B AdrenalO-35 / A Case Of Von Hippel-Lindau Disease with bilateral pheochromocytoma, abdominal paraganglioma and pancreatic neuroendocrine tumor
22.10 14.00-15.30 B Adrenal O-36 / Silent Pheochromocytoma in von Hippel-Lindau Disease: Report of a Case
22.10 14.00-15.30 B Adrenal O-37 / Adrenocortical carcinoma in pregnancy
22.10 14.00-15.30 B Adrenal O-38 / A case with adrenal cyst hydatid mimicking malignant tumour in MRI and PET-CT
22.10 14.00-15.30 C Pituitary O-39 / Hamartoma of hypothalmus presented as precocious puberty and epilepsy in 10-years old girl
22.10 14.00-15.30 C Pituitary O-40 / A rare cause of Diabetes Insipidus: Rosai Dorfman Disease
22.10 14.00-15.30 D Neuroendocrine tumors
O-41 / Localization of an insulinoma by selective intraarterial calcium stimulation with hepatic venous sampling
22.10 14.00-15.30 D Neuroendocrine tumors O-42 / Known syndrome, a new case
-
2016
720 - 23 October, 2016 Antalya - Turkey
ORAL PRESENTATIONS
-
2016
820 - 23 October, 2016 Antalya - Turkey
O - 01 Bone/Calcium
POstOPerative HyPOParatHyrOidism: treatment WitH teriParatide
DENiz CAN GüVEN1, ÖMER ALPER GüRLEK2, SEDA OğUz2, NAfiyE HELVACI2
1Deparment of Internal meDIcIne, Hacettepe UnIversIty meDIcal facUlty, ankara, tUrkey 2Deparment of enDocrInology, Hacettepe UnIversIty meDIcal facUlty, ankara, tUrkey
Postoperative hypoparathyroidism is a common problem, follow-ing both thyroid and parathyroid surgeries. Conventionally vita-min D and elementary calcium have been the mainstay of therapy. Herein, we present our experience with teriparatide (recombinant parathormone) in a postoperative hypoparathyroidism patient. A 28-year-old female patient was referred to our clinic due to euthy-roid autoimmune thyroiditis with thyroid nodules. The patient was followed without treatment. Three years later, the patient applied to our clinic with inflammatory low back pain and morning stiffness. An MRI of sacroiliac joint showed bilateral grade III sacroileitis. Af-ter the patient’s evaluation with these findings, the diagnosis was made as ankylosing spondylitis. Before starting the steroid treat-ment, a bone mineral density measurement was performed and showed a lumbar spine z score of -6.6 and femur z score of -4. To-tal calcium and phosphate levels were 10.5 mg/dL and 2.5 mg/dL, respectively. Serum PTH test was ordered and it was 1619 pg/ml. Parathyroid ultrasonography revealed two lesions located inferior of each thyroid lobe which were compatible with parathyroid gland pathology. Total thyroidectomy and parathyroid gland excision and servical lymph node dissection were performed with the prelimi-nary diagnosis of parathyroid carcinoma. Histopathological exam-ination of surgical specimen showed chronic lymphocytic thyroiditis and parathyroid adenoma. In the postoperative period, the patient’s total calcium levels was around 5.5-6 mg/dL. IV calcium replace-
ment with oral calcitriol and calcium carbonate was required for three weeks postoperatively. After discharge with a maintenance regimen of calcitriol 12 mcg/day, calcium carbonate 15 grams/day and cholecalciferol 3600 IU/day, the patient’s hypocalcemia persist-ed and hyperphosphatemia developed. At this point we decided to start subcutaneous recombinant parathyroid hormone. Teriparati-de (20 μg/12 h s.c.) was started. This therapy enabled dose reduc-tion of calcitriol down to 4.5 mcg/day and calcium carbonate to 9 grams/day. Hyperphosphatemia was resolved. After seven months of therapy teriparatide dose was tapered to a daily single dose which was ceased completely after another month. Hypocalcemia did not recur after the cessation of teriparatide. During 5 years of follow up, the patient has been normocalcemic under the reg-imen of calcitriol 1.5 mcg/day and calcium carbonate 3 grams/day. Short term use of teriparatide is reported in multiple case reports especially in patients with thyroidectomy and neck dissection. A prospective study with four years follow up provided data for the safety and efficacy of long term teriparatide treatment in postop-erative hypoparathyroidism. Although further studies are required for long term effects, teriparatide seems to be a good choice with a favorable safety profile for refractory postoperative hypoparathy-roidism.
Keywords: refractory postoperative hypoparathyroidism, teri-paratide, parathyroid adenoma
-
2016
920 - 23 October, 2016 Antalya - Turkey
Primary hyperparathyroidism (PHPT) is a rare disorder. Incidence is 8/100000.This incidence is same among child bearing age wom-en and pregnants. PHPT during pregnancy is associated with sev-eral risks to the mother and fetus especially when maternal total serum calcium is >11 mg/dL. In gestational PHPT cause is a single adenoma in %80-85 patients, hyperplasia in %10-12 patients, mul-tiple adenoma in %2 patients and carcinoma %1 patients as gen-eral population. We present a case of PHPT diagnosed during third trimester of pregnancy.
A 43 years old woman, was under follow up of obstetric clinic be-cause of her fourth pregnancy. She was admitted to the hospital with abdominal pain, nausea and constipation at 27th week of ges-tational age. Complete blood count and biochemical tests were to-tally normal except hypercalcemia [Ca:11,4 mg/dl (8,7-10,4)]. She was referred to our clinic because of hypercalcemia. There were no pathological findings on her physical examination. Hyperpara-thyroidism was detected with initial tests for differential diagno-sis; creatinine:0,62 mg/dl (0,5-11), Ca: 11,4 mg /dl (8,7-10,4),P: 2,67 mg/dl(2,4-5,5), PTH: 140 pg/ml (14-72),25-OH D3:18,2 ng/ml (30-100), 24 hour urine Ca:310 mg/24h (
-
2016
1020 - 23 October, 2016 Antalya - Turkey
Aim: Primary hyperparathyroidism (PHP) is the most common cause of hypercalcemia based on outpatient clinic. The diagnosis of PHP is generally straightforward with high intact PTH (iPTH) and hypercalcemia. But, PHP does not always exhibit those biochemi-cal features. Less known phenotype of PHP is the hypercalcemia with normal level of iPTH. We report a case of parathyroid adenoma with low normal peripheral iPTH and high jugular PTH levels pre-senting as hypercalcemia.
Case: A thirty-six year old woman who have type 2 diabetes melli-tus was admitted to the hospital with the diagnosis of acute pancre-atitis. She had no cholelithiasis. Serum amylase and lipase levels were high. Acute edematous pancreatitis was shown on comput-ed tomography. She had hypertriglyceridemia in her past medical history. Serum of the patient was observed as lipemic. Hypertri-glyceridemia could be a reason for the pancreatitis. On laboratory examination at admission to the hospital; calcium level was 8.0 mg/dL (8.8-10.2), intact PTH (iPTH) level was 28.8 pg/mL (12-88) and 25-hydroxy vitamin D level was 6.5 ng/mL. Cholecalciferol was giv-en intramuscularly as 300.000 IU. In her past medical history, hypo-thyrodism was present. Thyroid ultrasonography was performed. There was a hypoechoic solid nodule on right thyroid lobe sized as 7x3mm. There was also 17x6 mm sized lesion at the lower part of right thyroid lobe that revealed as possible parathyroid adenoma. On Tc 99m MIBI scintigraphy, a lesion was seen at the lower part of
right thyroid lobe (figure 1). This lesion was thought as parathyroid adenoma. There was no osteoporosis according to bone mineral densitometry. After replacement of vitamin D and acute pancreati-tis subsided, serum Ca and iPTH levels were as follows: 10.6, 10.7, 10.9 mg/dL and 28.8, 33.3, 31.7 pg/mL, respectively. Twenty-four hour calcium excretion was 403 mg/day, serum phosphorus was 2.3 mg/dL. iPTH measurement was repeated in another accredited laboratory and was found as 27 pg/mL. iPTH was measured also by using dilution technique and obtained as 38 pg/mL. Hydration and furosemide treatment were performed, but Ca level was still high, which was 11.4 mg/dL. Besides hypertriglyceridemia, we thought that hypercalcemia could precipitate the episodes of pancreatitis. Based on the findings of hypercalcemia, hypercalciuria, positive so-nographic and scintigraphic images, operation was performed with the possible diagnosis of PHP. PTH measurement was taken from the right jugular vein. Intraoperative PTH was 634 pg/mL. Histo-pathological examination revealed as parathyroid adenoma. Post-operative hypocalcemia didn’t occur and postoperative calcium and iPTH levels were normal.
Conclusion: Clinicians should be aware of the presence of low-nor-mal iPTH in PHP. If the clinical suspicion of PHP is high as in our case, surgery should be performed after exclusion of other causes of hypercalcemia.
Keywords: Hypercalcemia, low-normal PTH, parathyroid adenoma
O - 03 Bone/Calcium
a striking finding during intraOPerative jugular samPling in a Case Of ParatHyrOid
adenOma WitH lOW-nOrmal serum intaCt ParatHyrOid HOrmOne levels
ILGIN yILDIRIM şiMşiR1, BANU şARER yüREKLi1, HATiCE ÖzIşIK1, MURAT ÖzDEMiR2, yEşiM ERTAN3, ÖzER MALAy2, GÖKHAN ÖzGEN1
1 ege UnIversIty facUlty of meDIcIne, Department of enDocrInology, IzmIr, tUrkey 2 ege UnIversIty facUlty of meDIcIne, Department of general sUrgery, IzmIr, tUrkey
3 ege UnIversIty facUlty of meDIcIne, Department of patHology, IzmIr, tUrkey
-
2016
1120 - 23 October, 2016 Antalya - Turkey
Introduction: Some hypothyroid patients need high doses of oral levothyroxine (LT4) due to poor adherence to treatment, not taking the drug on an empty stomach, malabsorption, and co-administration of drugs interfering with absorption. We present a case of isolated mal-absorption of LT4 responding to intramuscular (IM) therapy.
Clinical Case: A 32 year old female patient was admitted to hospital due to hair loss and massive weight gain in 2008. She had thyroidec-tomy and radioactive iodine therapy in 2004. She was on 400 μg/d LT4 therapy. Physical examination revealed dry skin, non-pitting oedema, and diminished deep tendon reflexes. History of systemic diseases, diarrhea, and co-administration of any other drugs or herbal products interfering with LT4 absorption were absent. Thyroid function tests (TfT) did not improve despite medication under supervision.
Gastrointestinal endoscopy and stool analysis was normal. Antipari-etal, endomysium, and transglutaminase antibodies were negative. Triiodothyronine added to high-dose LT4 therapy was ineffective.
To evaluate LT4 malabsorption, 1000 µg LT4 was administered orally and TfT were measured with 2 hour intervals for 6 hours. fT4 level did not change. During the test she developed aphasia, loss of vision, and hemiparesis. Cranial imaging was normal and transient ischemic attack (TIA) was diagnosed. The neurologic symptoms regressed with anti-oedema and acetylsalicylic acid (ASA) therapy. She was discharged with daily 450 µg LT4 and 75 µg triiodothyronine therapy.
She was lost to follow-up until 2012. During this period she had another TIA during intravenous (IV) therapy in another center. fur-thermore rectal route could not be tolerated and vaginal route was unsuccessful.
Her treatment schedule was planned as weekly increased doses of 200, 500, 1000, and 1200 µg IM LT4. TfT were measured at weekly in-tervals. She developed left sided loss of strength during 1200 µg dose. Cranial imaging was again normal. The symptoms regressed within a week with ASA therapy. Detailed tests for coagulopathy were normal.
TfT quickly normalized with IM 500 µg LT4 twice a week. No other TIAs occurred.
After euthyroidism was achieved, parenteral route was switched to oral route according to the assumption that malabsorption due to oedema in the gastrointestinal tract secondary to hypothyroidism might have improved. However hypothyroidism ensued soon. Pre-vious regime was started again. She was euthyroid at the last time she was seen.
Conclusion: Impaired LT4 absorption may continue despite vigorous acts against factors interfering with absorption. Due to its limited mar-keting and its high cost, LT4 is administered for short term via slow IV infusion. The only risk for TIA and atherosclerosis was prolonged hypothyroidism. She did not experience acute variations in serum T4 during high dose LT4 therapy to explain to TIAs. An adverse effect of high dose LT4 therapy seems to be the best explanation for TIAs.
Keywords: hypothyroidism, malabsorption, parenteral levothyrox-ine, transient ischemic attack
Table 1. The changes in the levels of free throxine and thyroid stimu-lating hormone after administration of intramuscular 500 µg LT4 twice a week (fT4: free thyroxine, TSH:Thyroid stimulating hormone)
O - 04 thyroid
a Case Of HyPOtHyrOidism requiring Parenteral levOtHyrOxine treatment
HANDE PEyNiRCi1, BENGüR TAşKIRAN2, ERDiNç ERTüRK3, PINAR şişMAN3, CANAN ERSOy3
1 kastamonU state HospItal, kastamonU, tUrkey 2 yUnUs emre state HospItal , eskIşeHIr, tUrkey
3 UlUDag UnIversIty , bUrsa, tUrkey
-
2016
1220 - 23 October, 2016 Antalya - Turkey
Table 2. The changes in the levels of free T4 and TSH after administration of oral 1000 mcg LT4 at the end of a 6-hour monitoring
TFT baseline 2nd hour 4th hour 6 th hour
fT4 (ng/dL) 0.40 0.40 0.40 0.40
TSH (μIU/mL) 100 81.81 84.74 93.48
-
2016
1320 - 23 October, 2016 Antalya - Turkey
Background: Primary thyroid lymphoma (PTL) is defined as a lympho-ma involving only the thyroid gland or the thyroid gland and adjacent (regional) neck lymph nodes. Thyroid lymphoma represents 4% of all malignancies that is a relatively rare disease often posing a diagnostic challenge (1). Reaching the final diagnosis can be delayed if insufficient biopsy material is obtained. fNA diagnosis of thyroid lymphoma, par-ticularly due to the histological similarities with thyroiditis and the high coincidence of these pathologies within the same gland, which results in increased false-negative rates from sampling error (2). The present study describes the case of a patient who was treated as subacute thy-roiditis and diagnosed as having diffuse large B-cell lymphoma.
Clinical Case: A 61-year-old female presented with anterior neck pain, hoarseness and rapidly expanding mass of the neck diagnosed as subacute thyroiditis and she had recieved NSAi at least 2 months for her pain 4 months earlier. fine needle aspiration cytodiagnosis was benign. The patient was admitted to our hospital because of in-creasing dyspnea. Laboratory studies revealed an euthyroid state; antithyroglobulin and thyroid peroxidase antibodies were both pos-itive. In PA chest X-ray trachea was narrowed and shifted to the left side. A neck ultrasound showed a significantly enlarged, diffuse pa-renchymal inhomogeneity and ill defined border over right lobe and isthmus of the thyroid gland. Also, the trachea was narrowed and pressed to the right. Tru-cut biopsy was performed and histological diagnosis was Diffuse large B-cell lymphoma of the thyroid gland. A computed tomography scan demonstrated that the trachea was markedly compressed and displaced by the mass. His respiratory status was so urgent that the patient was given corticosteroids and saved her from receiving a tracheostomy. After she recieved che-motherapy she was in a good physical condition.
Conclusion: The most common presentation of subacute thyroid-itis is an anterior neck pain radiating up to the jaw and ear. Other causes of pain in the thyroid gland should be taken into consider-ation during differential diagnosis, especially when a patient pres-ents with misleading symptoms like progressive dyspnea, dyspha-gia or dysphonia. Such a presentation should be acknowledged and this leads to early diagnosis, treatment and prevention of unneces-sary surgery.
Keywords: Primary thyroid lymphoma, subacute thyroiditis, neck mass
figure 1: A computed tomography
figure 1. A computed tomography the trachea was markedly compressed and displaced by the mass.
figure 2: PA chest X-ray
figure 2. PA chest X-ray yazılacak narrowing and shifting of trachea
O - 05 thyroid
Primary tHyrOid lymPHOma Presenting WitH suBaCute tHyrOiditis
SEVGüL fAKI1, NESLiHAN çUHACI1, OyA TOPALOğLU1, CüNEyT BiLGiNER1, BERNA ÖğMEN1, HAKAN KORKMAz2, üNSAL HAN3, REyHAN ERSOy1, BEKiR çAKIR1
1 Department of enDocrInology anD metabolIsm, ankara yIlDIrIm beyazIt UnIversIty, scHool of meDIcIne, ankara, tUrkey
2 Department of otorHInolaryngology, ankara yIlDIrIm beyazIt UnIversIty, scHool of meDIcIne, ankara, tUrkey 3 Department of patHology, ankara yIlDIrIm beyazIt eDUcatIon anD researcH HospItal, ankara, tUrkey
-
2016
1420 - 23 October, 2016 Antalya - Turkey
Introduction:Thyrotoxic periodic paralysis (TPP) is an uncommon complication of thyrotoxicosis which is associated with paralysis and hypokalemia. Treatment of TPP consists of adequate potassi-um replacement, beta-adrenergic blockage and control of hyper-thyroidism.
Clinical Case: A-51-year-old male patient was admitted to emer-gency department with complaint of muscle weakness which start-ed 2 weeks ago but was aggravated a high carbohydrate intake. He was admitted to department of cardiology in another hospital 3 months ago because of dyspnea and his coronary angiography showed normal coronaries. He had no history of diabetes or hyper-tension. One week after coronary angiography he was applied to endocrinology and metabolism unit with complaint of sweating and subclinical hyperthyroidism was diagnosed. Non-iodized salt was recommended. In his admission to emergency department in our hospital; his physical examination revealed proximal muscle weak-ness in both upper extremities (4-/5) and lower extremities (2/5). His electrocardiogram showed u waves with 90 beats per minute. Other physical examination findings were unremarkable. His bio-chemical analysis results were as follows: random plasma glucose: 363mg/dl, serum creatinine: 0.53mg/dL, sodium: 138mmol/L, potassium: 1.9mmol/L, total calcium: 9.13mg/dL, phosphorus: 1.17mg/dL, albumin 4.22g/dL, Hb: 13.0g/dL. His white blood cell count and thrombocyte levels as well as liver function tests were normal. Despite high glucose levels, he had neither acidosis nor
ketosis. He had overt hyperthyroidism with TSH: 140/90 mmHg during his stay and 10mg amlodipine was prescribed. After normalization of potassium levels he didn’t have any complaints of muscle weakness. His insulin requirement decreased during his stay and he was discharged with 10 units of insulin glargine and 10mg amlodipine as well as 20mg propronolol and 30mg methi-mazole. He was invited to consultation 1 week after his discharge and his free T4 level was 1.27ng/dL and he did not have any need of insulin, amlodipine and propronolol.
Conclusion: TPP is an uncommon but potentially fatal complica-tion of hyperthyroidism. Despite being an easily treatable condition, it could have life-threatening consequences if it is overlooked.
Keywords: Thyrotoxicosis, Transient hypokalemic paralysis, Graves’ disease
0 - 06 thyroid
a rare Case Of tHyrOtOxiC PeriOdiC Paralysis WitH aCCOmPanying transient HyPerglyCemia
BAşAK ÖzGEN SAyDAM, üMiT çAVDAR, BARIş AKINCI, TEVfiK DEMiRDepartment of enDocrInology anD metabolIsm, DokUz eylUl UnIversIty facUlty of meDIcIne, IzmIr, tUrkey
-
2016
1520 - 23 October, 2016 Antalya - Turkey
Introduction: Multiple endocrine neoplasia type 2b (MEN 2b) is a rare and dominantly inherited syndrome characterized by medul-lary thyroid cancer, pheochromocytoma and mucosal neuromas. The most characteristic feature of MEN2b is multiple mucosal neuromas seen in almost all cases. As it is rarely seen, we have decided to present this case.
Case: A male patient aged 41 underwent bilateral total thyroidecto-my operation due to multinodular goiter in 2004 and the patholog-ical examination showed that the patient developed medullary thy-roid carcinoma. In surveillance, upon the detection of pathological lymph nodes in the neck, left neck dissection was applied.
In 2005, adjuvant radiotherapy was applied to the neck. In 2006, in genetical analysis, M918T heterozygous mutation was detected in RET gene. In 2008, as a mass was identified in the left adrenal gland, laparoscopic left adrenalectomy was applied. The pathology was determined as pheochromocytoma. Calcitonin value had not been checked in the preoperative period. Calcitonin value was 120 pg/mL in the post-operative period.
In the family history of the patient, his elder brother had had an operation due to pheochromocytoma.
In his physical examination, there were neuromas on the tongue and eye lids (Picture 1). He had hyperpigmented areas on his left shoulder (Picture 2)
The latest value for calcitonin was 88.6 pg/mL and CEA was 6,78 ng/mL. 24 hour urine metanephrine and normetanephrine levels were normal.
In laboratory examination, TSH was 2.26µIU/ mL and fT4 was 1.37 ng/dL. He was euthyroid with 150 mcg/day L-thyroxine treatment. The patient has been surveilled through the ultrasonography of neck (USG) and 24 hour urine metanephrine and normetanephrine.
Conclusion: The medullary thyroid carcinoma can progress most agressively in MEN2b. In this syndrome metastasis were defined even in the first year of life.
Mutations at codon 883 and 918 mutations with MEN 2b are at in-creased risk of agressiveness. In our case,codon 918 mutation was also detected.
It is recommended that the family members of these cases are screened for medullary thyroid carcinoma and if there is any carry-ing these mutations, they should be treated with prophylactic total thyroidectomy. for these cases, lifelong surveillance is required.
Keywords: Multiple endocrine neoplasia type 2b, medullary thy-roid cancer, mucosal neuromas
Picture 1
Picture 1. Neuromas on the tongue
Picture 2. hyperpigmented areas on the left shoulder
O - 07 thyroid
a Case WitH men-2B WHO Has neurinOma Of tHe tOngue and eyes
HATiCE ÖzIşIK1, BANU şARER yüREKLi1, NiLüfER ÖzDEMiR KUTBAy1, MAHiR AKyILDIz2, GÖKHAN ÖzGEN1
1 Department of enDocrInology, ege UnIversIty, İzmIr, tUrkey 2 Department of general sUrgery, ege UnIversIty, İzmIr, tUrkey
-
2016
1620 - 23 October, 2016 Antalya - Turkey
Introduction: Thyroid scintigraphy should be performed for the evaluation of thyroid nodules in case of suppressed Thyroid Stim-ulating Hormone (TSH) level. While the malignancy probability of hypofunctioning nodules is 15%, this ratio is generally lower than 1% in hyperfunctioning nodules. So we would like to present a case of toxic adenoma with the diagnosis of papillary thyroid carcinoma.
Case: forty-four-year-old woman patient had presented with the diagnosis of thyroid nodule. Thyroid fine needle aspiration biopsy (TfNAB) was performed for the evaluation of thyroid nodule mea-sured as 47x12 mm. This nodule was in mixed solid form bear-ing cystic components. TfNAB revealed that the thyroid nodule was benign. Propylthiouracil had been started before admission to our clinic according to laboratory values of TSH and free thy-roxin (fT4) which were 0.005 µIU/ mL and 1.75 ng/dL, respective-ly. On admission to our endocrinology clinic we performed thyroid scintigraphy showing hyperfunctioning thyroid nodule with scene of suppressed rest of thyroid region. Thyroid auto-antibodies were negative. Radioactive iodine therapy was recommended as a mo-dality of treatment. However, the patient preferred surgery for her
treatment with the concern of her father’s death due to leukemia. Our ultrasonographic evaluation was consistent with a thyroid nodule located at right lobe with a diameter of 43x18x28 mm. The nodule was mixed type solid nodule with regular borders and thin hypoechoic peripheral halo. Central chaotic hypervascularity and microcalcification were not detected. The patient underwent right thyroid lobectomy. Pathology report revealed macrofollicular vari-ant of papillary thyroid carcinoma. The tumor was 3.5 cm in diam-eter with regular border and 0.2 cm away from the surgical border. The tumor didn’t spread out of the thyroid capsule. Second thyroid surgery was performed due to remaining thyroid tissue. After that ablative radioactive iodine therapy was applied.
Conclusion: Although malignant potential of hyperfunctioning thyroid nodules is low, possibility of thyroid carcinoma cannot be excluded in those thyroid nodules. So, hyperfunctioning thyroid nodules warrants careful evaluation and appropriate therapy. We wanted to draw attention of the clinicians for this rare issue.
Keywords: toxic adenoma, papillary thyroid carcinoma, surgery
O – 08 thyroid
a Case Of PaPillary tHyrOid CarCinOma in tOxiC adenOma: are HyPerfunCtiOning nOdules truly innOCent all tHe times?
BANU şARER yüREKLi1, HATiCE ÖzIşIK1, NiLüfER ÖzDEMiR KUTBAy1, ÖzER MAKAy2, GÖKHAN ÖzGEN1, AyşEGUL AKGüN3
1 ege UnIversIty facUlty of meDIcIne, enDocrInology Department, IzmIr, tUrkey 2 ege UnIversIty facUlty of meDIcIne, general sUrgery Department , IzmIr, tUrkey 3 ege UnIversIty facUlty of meDIcIne, nUclear meDIcIne Department , IzmIr, tUrkey
-
2016
1720 - 23 October, 2016 Antalya - Turkey
Background: Amiodarone is the most commonly prescribed an-tiarrhythmic drug that is used mainly for the treatment of atrial fibrillation. Amiodarone-induced thyrotoxicosis (AIT) is a therapeu-tic challenge and it may be due to iodine-induced excessive syn-thesis of thyroid hormone (Type 1) or a destructive thyroiditis (Type 2). Herein we present two cases of medically refractory AIT treated with a surgical approach.
Case 1: A 24-year-old female with recurrent ventricular fibrillation attacks due to cardiomyopathy was referred to our clinic because of thyrotoxicosis. She had an intracardiac defibrillator (ICD), ejection fraction (Ef) was 35%, and had been using amiodarone orally for three months. Thyroid function test (TfT) results revealed thyro-toxicosis. Thyroid gland size was normal but mildly parenchymal heterogeneity and decreased vascularization were detected. Car-diology department discontinued the amiodarone therapy. Due to diagnosis of type 2 AIT, steroid therapy was started. In addition to increased steroid dosage, 3 weeks later methimazole and lithium therapies were initiated because of the progression in clinical and laboratory findings. Despite current medical therapies, no improve-ment was detected. Patient was diagnosed as non-responsive type 2 AIT and surgical approach was decided. In order to regulate the TfT levels, 12 sessions of plasmapheresis were performed. Thyroid function tests returned to normal. Subsequently, total thyroidecto-my was performed without perioperative complication. Patient was discharged from hospital by the third day.
Case 2: A 39-year-old male with history of hypertrophic cardiomy-opathy due to ventricular arrhythmia, heart failure (Ef 20%) and ICD was hospitalized to the coronary intensive care unit. Amiodarone infusion therapy was started. While amiodarone therapy continued thyrotoxicosis was detected and patient was consulted to endocri-nology clinic. The thyroid gland was normal but the vascularization was reduced. Thyroid scintigraphy showed active involvement on thyroid gland. Due to diagnosis of Type 1 AIT, antithyroid therapy was initiated while streoid therapy was added a week later. The therapy was continued in high doses but no response was seen and arrhythmias continued. Because of high-risk for thyroid surgery firstly 30 mCi radioiodine was administered but thyrotoxicosis con-tinued. Therefore, total thyroidectomy was performed under strict cardiology consultation. No perioperative complications were seen. Levothyroxine replacement started and tapering of steroid therapy was planned. Patient was discharged from hospital by the fourth day.
Discussion: Amiodarone-induced thyrotoxicosis is a diagnos-tic challenge due to its complicated pathogenesis and unreliable response to therapy. After the classification of AIT, the appropri-ate treatment must be started immediately. Persistent treatment choices such as surgery should be considered in uncontrolled pa-
tients or patients that are refractory to medical treatment.
Keywords: Amiodarone, thyrotoxicosis, resistant
O – 09 thyroid
mediCally refraCtOry amiOdarOne-induCed tHyrOtOxiCOsis: tWO Case rePOrts
NARiN NASIROğLU iMGA1, zEyNEP çETiN1, ALPER çAğRI KARCI1, DiLEK BERKER1, SERDAR GüLER2
1 Department of enDocrInology, ankara nUmUne eDUcatIon anD researcH HospItal, ankara, tUrkey 2 Department of enDocrInology, HItIt UnIversIty facUlty of meDIcIne, corUm, tUrkey
-
2016
1820 - 23 October, 2016 Antalya - Turkey
Introduction: About 250 patients with acquired partial lipodystro-phy (APL) have been reported so far. It is characterized by the loss of adipose tissue from the face, arms and upper part of the body. The disease usually starts during childhood or adolescence. fat loss often come into view in months or years. females are more fre-quently affected. Although the etiology of APL is unclear, increased complement activity has been reported in some APL patients.
Case: A 23-year-old female reported fat loss on her face that she first noticed when she was 12. She was diagnosed with diabetes when she was 21 which was treated with metformin. On physical examination, fat loss was remarkable on her face, arms and up-per trunk (fig.1a). Acanthosis nigricans was noticed on her arm-pits and around her neck (fig.1b). Her laboratory results were as follows: fasting blood glucose: 111 mg/dl, HbA1c: 6.1%, fasting in-sulin: 34.3 ulU/ml, AST: 40 U/L, ALT: 65 U/L, triglyceride: 393 mg/dl, HDL-cholesterol: 32 mg/dl, C3: 1.02 g/L (0.9-1.8), C4:0.29 g/L (0.1-0.4), and microalbumin in spot urine: 26.5 mg/L. Abdominal ultrasonography showed grade 1 hepatosteatosis. Echocardiogra-phy was normal. No Drusen-like lesion was detected in eye exam-ination.
Conclusion: Although previous studies reported that metabolic ab-normalities were rarely observed in APL, our recent study showed that metabolic abnormalities associated with insulin resistance are more common than previously thought. Our observation on this newly diagnosed APL patient also supports the idea that a regular screening for metabolic abnormalities should be carried out in pa-tients with APL even at young age.
Keywords: Acquired partial lipodystrophy, metabolic abnormali-ties,Drusen-like lesion
figure 1a, 1b: A case of acquired partial lipodsyttrophy (APL)
O – 10 lipids/Obesity
metaBOliC aBnOrmalities assOCiated WitH insulin resistanCe in a yOung Patient WitH
aCquired Partial liPOdystrOPHyNiLüfER ÖzDEMiR KUTBAy1, BANU SARER yüREKLi2, HALiT DiRi1, HATiCE ÖzIşIK2, zEKi yAşAR3,
füSUN SAyGILI2, BARIş AKINCI4
1 gazI yasargIl traInIng anD researcH HospItal, DIvIsIon of enDocrInology, DIyarbakIr, tUrkey 2 ege UnIversIty, DIvIsIon of enDocrInology, IzmIr, tUrkey
3 selaHaDDIn eyyUbI state HospItal, DIvIsIon of plastIc sUrgery, DIyarbakIr, tUrkey 4 DokUz eylUl UnIversIty, DIvIsIon of enDocrInology, IzmIr, tUrkey
-
2016
1920 - 23 October, 2016 Antalya - Turkey
Background: Paget’s disease is a localised disorder of bone re-modelling characterized by the excessive resorption and new bone formation. Clinical features of Paget’s disease are pain, fractures, deformity, and manifestations of the neurologic, rheumatologic, or metabolic complication of the disease. However, at least two-thirds of patients are asymptomatic.
Case: We reported a 50 years old woman attend neurosurgery outpa-tient clinic complaining of headache for about a year. The patient was reffered to endocrinology outpatient clinic because the cranial mag-netic resonance imaging (MRI) of the patient raised suspicion of Pag-et’s disease of bone. from the anamnesis of the patient we learned that she also has progressive hearing loss. On physical examination, she has enlargement of the skull with left frontal bossing.
Laboratory findings; serum calcium, phosphorus, urea, creatinine, liver enzyme levels were normal. Serum alkaline phosphatase (ALP) activity and parathyroid hormone (PTH) levels were increased and serum vitamin D level was deficient.
Imaging studies; Cranial MRI of the head show marked thickening of the diplopic space, diffuse calvarial thickening. Left side is more thick than the right side. There are heterogenous signal differences in all sequences. Bone scan releaved intense uptake of the radionuclide in the calvarium that is generally diffuse but heterogenous only in some parts and more marked in the left fronto-parietal bone. There is also intense uptake of the radionuclide on the left femur.
The patient was sent to ear specialist for evaulation of her hearing loss. Physical examination of her ears were normal. In her audio-metric assesment there was bilateral asymmetric sensorineural hearing loss in pure tone audiometry of patient. Pure tone averages of air/bone conduction were 25 dB/25 dB on the right side and 35 dB/27 dB on left side.
After vitamin D deficiency was corrected serum PTH level became normal but serum ALP level was still high. A single 5 mg dose iv zolendronate was given for the treatment of her Paget’s disease. Six months following this treatment serum ALP activity, calcium, phosphorous, PTH levels are in normal limits. At the audiometric reassesment pure tone audiometry averages of air/bone conduc-tion are 22 dB/17 dB on the right side and 37 dB/32 dB on the left side. Her hearing loss has not changed significantly. The differenc-es between pure tone averages of two periods are minimal and can be audiometrist dependent.
Conclusion: Hearing loss due to Paget’s disease may not be re-versible but early diagnosis and treatment may prevent further deterioration of hearing. Randomized, double-blind, placebo con-trolled clinical trials in which the effect of antipagetic therapy is assessed on hearing loss in patients with Paget’s disease of the temporal bone, are needed.
Keywords: hearing loss, paget’s disease, bisphosphonate
O - 12 Bone/Calcium
effeCt Of zOlendranate treatment On Hearing lOss in a Patient WitH tHe Paget’s
disease WHO Has skull invOlvementiLKAy KARTAL1, ARzU TATLIPINAR2
1 Department of Internal meDIcIne, DIvIsIon of enDocrInology anD metabolIsm, meDenIyet UnIversIty, goztepe traInIng anD researcH HospItal, IstanbUl, tUrkey
2 Department of otolaryngology- HeaD anD neck sUrgery, fatIH sUltan meHmet traInIng anD researcH HospItal, IstanbUl, tUrkey
-
2016
2020 - 23 October, 2016 Antalya - Turkey
Introduction: Primary hyperparathyroidism is a disorder caused by enlargement of one or more parathyroid glands. About 6-16% of parathyroid adenomas can be in an ectopic location, therefore, localization of parathyroid lesions can be challenging.
Case Report: A 74-year-old female patient was admitted to our hospital with weakness, fatigue and constipation. Her medical history included type 2 diabetes mellitus, hypertension and coro-nary heart disease. Laboratory studies revealed normal iPTH con-centration (56.9 pg/mL normal: 12-88 pg/mL) and normal serum biochemistry except elevated calcium level (13.15 mg/dL). Urinary calcium excretion was to be high (549.15mg/day). Based on clinical and laboratory findings, a final clinical diagnosis of primary hyper-parathyroidism was made.
Neck ultrasonography exam was planned and performed with the intention to localize the adenoma. A 14x10 mm, hyopoechoic solid lesion was located in the inferior pole of the right thyroid parenchy-ma. In addition to this nodule there were also several other sub-centimeter solid nodules scattered throughout both thyroid lobes. The hypoechoic solid nodules described in the inferior pole of the right thyroid lobe was biopsied with fine needle aspiration (fNA) under US guidance. The cytological exam revealed atypia of un-
determined significance. The following 99mTc-MIBI scintigraphy, SPECT–CT, neck MRI and 4-D neck CT did not depict any findings suggestive of a parathyroid adenoma. Under the light of these find-ings we considered that an intrathyroidal parathyroid adenoma was clinically possible and a second fNA biopsy with PTH washout was performed. PTH washout concentration was found to be conclusive for a parathyroid adenoma with the level of 2612 pg/mL.
Based on these findings surgical removal of the right thyroid lobe was planned. Intraoperative frozen exam revealed this nodule to represent a papillary thyroid carcinoma and a total thyroidectomy was performed after this result. Post-surgical definitive patholog-ical exam confirmed that this nodule was consistent with a para-thyroid adenoma instead of PTC. Post-operative serum PTH and calcium levels returned to normal values.
Discussion: Intrathyroidal parathyroid adenomas may cytologically mimic primary papillary thyroid carcinomas. In this case report, we aimed to underline the diagnostic value of PTH washout after fNA for suspicious intrathyroidal nodules.
Keywords: parathyroid adenoma, hypercalcemia, fine needle aspi-ration, parathyroid hormone
O – 13 Bone/Calcium
tHyrOid nOdule Or ParatHyrOid adenOma: a Case rePOrt
EDA çALIşKAN yILDIRIM, UğUR üNLüTüRK, NAfiyE HELVACI, MiyASE BAyRAKTARDIvIsIon of enDocrInology anD metabolIsm, Department of Internal meDIcIne, Hacettepe UnIversIty, ankara,
tUrkey
-
2016
2120 - 23 October, 2016 Antalya - Turkey
Introduction: Thrombotic thrombocytopenic purpura (TTP) is a rare disease characterized by thromboses, resulting in thrombo-cytopenia. It consists of the pentad of microangiopathic hemolytic anemia, thrombocytopenic purpura, neurologic abnormalities, fe-ver, and renal disease. It’s unclear what triggers TTP, but some factors may play a role such as: pregnancy, malignancies, infec-tions, surgery, blood and marrow stem cell transplant, chemother-apeutics, ticlopidine, clopidogrel, cyclosporine A, estrogens and quinine. The association between hyperthyroidism or antithyroid drugs with TTP is nonexistent in the literature; this case is the first in the literature to discuss possible hyperthyroidism or antithyroid medication triggered TTP.
Case: A fifty four years old female patient was diagnosed with toxic multinodular goiter and treated with propylthiouracil for two weeks and methimazole for a week before admission. Patient was admit-ted to emergency room with disseminated purpura, acute renal failure and lethargy. Her routine blood work revealed elevated cre-atinine [4.8 mg/dL (0.5-1.1 mg/dL)] and thrombocytopenia [13.000/mm3 (150.000-450.000/mm3)]. Coagulation tests were normal. Pe-ripheral blood smear revealed shistocytes; patient was diagnosed as TTP and was hospitalized by Hematology. TSH levels were low [
-
2016
2220 - 23 October, 2016 Antalya - Turkey
Introduction: Papillary microcarcinomas can rarely manifest as aggressive bone metastatic lesions with unexpected laboratory and clinical findings. We herein present an elderly patient diagnosed with multiple bone metastasis during investigations for acute kid-ney injury.
Clinical Case: In february 2015, a 72-year-old woman experienced a car accident, which lead to right humerus fracture and acute kid-ney injury. Her previous history was remarkable for tuberculosis, hydatid cyst, type 2 diabetes and hypertension, and she donated her kidney to her daughter. She also suffered from widespread bone pain for 1 year, and abdominal CT revealed multiple bone lesions involving lumbar spine and ischial bone. Pelvic MRI and bone scan showed extensive lytic bone lesions involving mandible, humerus, femur, multiple ribs, manubrium sterni, scapula, clav-icle, lumbar and sacral spine and pelvic bones. Bone biopsy was compatible with thyroid cancer. Thyroid ultrasound revealed mul-tiple nodules, and biopsy was suspicious for follicular neoplasm. The patient underwent total thyroidectomy and neck dissection, and histopathological investigations showed two foci of follicular variant of papillary microcarcinoma in the right lobe. External ra-diotheraphy was also performed for some of the metastatic bone lesions. Postoperatively, she was treated with 200 mCi 131I-ther-apy combined with temporary high dose dexamethasone. Whole body scan after treatment showed uptakes in the neck and bones. Levothyroxine was begun and the dose was increased to 150 mcg/day, but the patient began to experience dyspnea and pretibial ede-
ma due to diastolic congestive heart failure. Thyroid function tests showed a very low fT4, high fT3 and supressed serum TSH. During follow-up L-thyroxine dose was tapered to 50 mcg/day. Her weird thyroid function tests were possibly due to tumor tissue expressing excessive type 2 deiodinase activity converting circulating T4 to T3. She did not have functioning thyroid cancer metastases, since the patient’s thyroid hormone levels fell when levothyroxine supple-mentation was held, and her TSH levels were increased. After the first radioactive iodine therapy she experienced progressive tumor burden, and another 200 mCi radioactive iodine was administered, which resulted in tumor lysis syndrome, DIC, bone marrow failure, and she needed hemodialysis. She rejected further treatment and died of extensive metastatic disease at home.
Conclusion: Although papillary microcarcinomas are known to be tumors with good prognosis, they can also present with extensive refractory and fatal bone metastasis. Some of the weird thyroid function tests such as low free T4 and normal to high free T3 levels and comparably low levothyroxine need to supress TSH may be as-sociated with type 2 deiodinase activity in the tumor. In these condi-tions, increasing levothyroxine dosage for normalising free T4 level is useless and may even lead to very high T3 levels and associated adverse affects.
Keywords: follicular variant of papillary microcarcinoma, bone metastasis, thyroid function tests
O - 15 thyroid
agressive fOlliCular variant Of PaPillary miCrOCarCinOma Presenting WitH extensive BOne metastases and assOCiated WitH Weird
tHyrOid funCtiOn testsNURDAN GüL1, HüLyA HACIşAHiNOğULLARI1, METBAN MESTANzADE1, AyşE KUBAT üzüM1,
ÖzLEM SOyLUK SELçUKBiRiCiK1, SEVGi KALAyOğLU BEşIşIK2, REfiK TANAKOL1
1 IstanbUl facUlty of meDIcIne, Department of Internal meDIcIne, DIvIsIon of enDocrInology anD metabolIsm , IstanbUl, tUrkey
2 IstanbUl facUlty of meDIcIne, Department of Internal meDIcIne, DIvIsIon of Hematology , IstanbUl, tUrkey
-
2016
2320 - 23 October, 2016 Antalya - Turkey
Introduction: Thyrotoxic periodic paralysis (TPP) is characterized by sudden onset of hypokalemia and paralysis under the condition of thyrotoxicosis. TPP is more prevalent in Asians than in non-Asians and also in males more than in females. In Chinese and Japanese patients with hyperthyroidism, 1.8–1.9% experience TPP. The typical age of onset is 20–40. Hypokalemia in TPP results from an intracellular shift of potassium under conditions of high thyroid hormone levels.
Clinical Case: A 29-year-old man with a history of recurrent mus-cle weakness presented to our emergency department with diffi-culty in walking. The patient’s symptoms started one day before, and he was unable to walk to the hospital. He had had similar epi-sodes before. He stated palpitations, tremor and excessive sweat-ing. He had no family history of periodic paralysis.
On physical examination, he had an enlarged thyroid gland and tachycardia. He had tremor in his hands and decreased mus-cle strength in both lower extremities. His initial potassium lev-el was 2.6 mEq/L (3.5–5.1 mEq/L), phosphorus level was 3.7 mg/dL (2.5–4.5 mg/dL), and magnesium level was 1.9 mg/dL (1.7–2.6 mg/dL). Electrocardiogram showed sinus tachycardia with a rate of 124 beats per minute. He was given intravenous potassium chloride with saline infusion. He was also given oral potassium replacement, which resulted in resolution of his lower-extremity paralysis. On the second day of admission, his serum potassium level increased to 4.8 mEq/L. His renin and aldosterone levels were
within normal limits. The thyroid-stimulating hormone (TSH) level was 0.01 mU/L (0.4–3.9 µIU/mL), the free thyroxine (fT4) level was 3.8 ng/dL (0.8–2.7 ng/dL) and the free triiodothyronine (fT3) level was 13.8 ng/dL (2.3–4.4 pg/mL). Thyrotoxicosis was diagnosed, and the patient was given propranolol 40 mg twice a day. The anti-TSH receptor antibody level was 19.6 IU/L (1.22-1.75 IU/L), His thyroid scintigraphy and uptake scan was consistent with Graves’ disease. He was started on methimazole 20 mg per day. Serial measure-ments of his serum potassium level remained within normal limits without potassium replacement. The patient was diagnosed as TPP secondary to Graves’ disease.
CONCLUSION: The diagnosis of TPP is made when a patient pres-ents with a paralytic attack that is associated with hypokalemia and hyperthyroidism. The most common underlying form of thyroid dis-ease associated with TPP is Graves’ disease but any other cause of hyperthyroidism can be associated with TPP. The condition may be life-threatening if weakness of the breathing muscles leads to respiratory failure, or if the low potassium levels lead to cardiac arrhythmias. Patients should be on cardiac monitoring, and potas-sium levels should be monitored for potential rebound hyperkale-mia. Treatment of TPP includes replacing potassium, prevention of this shift of potassium by using nonselective beta-blockade and treatment of underlying thyrotoxicosis.
Keywords: thyrotoxicosis, hypokalemia, paralysis
O - 16 thyroid
tHyrOtOxiC PeriOdiC ParalysisETHEM TURGAy CERiT1, MEHMET TUNCAy2, MEHMET MUHiTTiN yALçIN1
1 Department of enDocrInology & metabolIsm, Dr. ersIn arslan traInIng anD researcH HospItal, gazIantep, tUrkey
2 Department of nepHrology, Dr. ersIn arslan traInIng anD researcH HospItal, gazIantep, tUrkey
-
2016
2420 - 23 October, 2016 Antalya - Turkey
Introduction: Hypothyroidism and pleural effusion (PE) are well-defined to accompany, however thyrotoxicosis and PE collab-oration is not so frequent. We described a patient with no history of heart or liver failure; suffering from PE, peripheral edema, and hypoalbuminemia who was diagnosed with thyroxicosis. PE and peripheral edema resolved immediately after initiation of antithy-roid medication.
Case- A 50-year old man arrived at our clinic with fatique, short-ness of breath, palpitations and edema in lower extremity. He had a pulse rate of 130/min with a respiratory rate of 28/min, while pulmonary examination defined decreased sounds in right inferi-or and mid lobe and there was grade 3 pretibial edema. His blood test results were: Creatinine: 0,32 mg/dl, Albumin(alb): 2.8 g/dl, Alanine Aminotransferase (ALT): 21 U/l, Gamma Glutamyl Trans-ferase (GGT): 48 U/l, Thyroid Stimulating Hormone (TSH): 0.00 µIU/ml, free T4 (fT4): 3. 6 (0.89-1.79) ng/dl, free T3 (fT3): 8.7 (2.3-4.2) pg/ml. His chest graph revealed right pleural effusion and chest computed tomography (CT) showed 27 mm pleural effusion in right hemithorax. Echocardiography (echo) demonstrated grade 2 mitral regurgitation (MR), tricuspid regurgitation (TR) and normal ejection fraction. Hepatobiliary ultrasonography (USG) showed no pathology. Spironolactone 25 mg/d, hydrochlorthiazide 25 mg/d and furosemide 40 mg/d was started. Thyroid USG revealed mul-tinodular goiter, the biggest nodule 18x22x34mm on right lobe and thyroid 99m Technetium-pertecnatate scintigraphy showed diffuse
increased uptake and a hypoactive nodule in right lobe. After toxic diffuse multinodular goitre (TDMNG) was diagnosed, MMI 30 mg/day was attempted to start. Since unavailability of MMI, PTU 300 mg/day was started. After one week, fT4: 2.55 ng/dl, fT3: 8.37 pg/ml were found along with increase of alb to 3.5 g/dl. Meanwhile pulmonary sounds reversed to normal and chest graph revealed normal examination with peripheral edema resolved in lower ex-tremity. Echo showed trace amount of TR and MR. After one month TSH:0.00 µIU/ml, fT4: 2.24 ng/dl, fT3: 7.95 pg/ml and 3.8 g/dl alb level were seen. A month later, alb level rised to 4.6 g/dl.
Conclusion: PE is rare, while hypoalbuminemia is again unex-plained in thyrotoxic patients. Thyrotoxic state establishes inflam-mation that would cause alb to decrease. In our case hypoalbu-minemia evolved to be noteworthy since it would describe PE and peripheral edema accompanying thyrotoxicosis. After antithyroid treatment, volume excess resolved with alb rise. Nevertheless, multiple diuretic medications may also improve the patients’ ail-ments. Diuretics may have decreased the volume overload and me-diate alb level rise by increasing alb concentration. However abrupt disappearance of such volume load would not be depended only on low dose oral diuretic treatment. PE may be seen in patients with thyrotoxicosis and responds well to antithyroid therapy and low dose diuretic therapy.
Keywords: Thyrotoxicosis, pleural effusion, hypoalbuminemia
O - 17 thyroid
tHyrOtOxiCOsis WitH Pleural effusiOn and HyPOalBuminemia
iffET DAğDELEN DURAN1, NEşE ERSÖz GüLçELiK2
1 Department of enDocrInology anD metabolIc DIseases, kIrIkkale yüksek İHtIsas HospItal, kIrIkkale, tUrkey 2 Department of enDocrInology anD metabolIc DIseases, ankara eDUcatIon anD researcH HospItal,
ankara,tUrkey
-
2016
2520 - 23 October, 2016 Antalya - Turkey
Introduction: Graves’ disease is an autoimmune disorder which can be accompanied with other autoimmune diseases affecting various organ systems. In such cases, treatment of hyperthyroid-ism may be troublesome due to organ dysfunction caused by con-comitant disease. Herein, we present a patient with liver failure due to primary sclerosing cholangitis complicated with Graves’ disease.
Case Presentation: A 35-year-old man, who was diagnosed with friedreich Ataxia at the age of 12 and primary sclerosing cholangi-tis two months ago, presented to our gastroenterology clinic with the complaints of pruritus, diarrhea, palpitations and weight loss. He was currently taking ursodeoxycholic acid and proton pump inhibitor ther-apy. On physical examination, he had jaundice, ataxic gait, choreiform movements. Laboratory workup yielded elevated ammonia levels indicating hepatic encephalopathy in addition to very high bilirubin, transaminase and prothrombin time levels. Thyroid function tests suggested primary hyperthyroidism. TSH receptor antibody (TRAb) was positive (6.27 IU/L). Thyroid ultrasonography showed parenchy-mal heterogeneity in a normal sized gland, which was diffusely hyper-
active in technetium 99m pertechnetate scintigraphy. The patient was diagnosed as Graves’ disease. Antithyroid druq therapy was not suit-able for the patient because of liver failure. Therefore, the patient un-derwent plasmapheresis as a temporary management option before definitive treatment for thyrotoxicosis. After two sessions of plasma-pheresis, TRAb became negative, fT4 and fT3 levels decreased, clinical findings of hepatic encephalopathy improved due to decreasing biliru-bin levels and the need for urgent liver transplantation disappeared. After discharge, total thyroidectomy was performed. Pathological ex-amination revealed diffuse hyperplasia and multifocal thyroid micro-papillary carcinoma.
Conclusion: Plasmapheresis is a viable option for patients with Graves’ disease and impaired liver function. In our case, only two sessions of plasmapheresis enabled the patient to have thyroid surgery and resolved the need for urgent liver transplantation.
Keywords: Plasmapheresis, Graves’ disease, primary sclerosing cholangitis
O - 18 thyroid
PlasmaPHeresis as a temPOrary management OPtiOn in a Patient WitH graves’ disease and
Primary sClerOsing CHOlangitisBATUHAN BAşPINAR1, SEDA HANifE OğUz2, TAyLAN KAV3, BüLENT OKAN yILDIz2
1 Department of Internal meDIcIne, Hacettepe UnIversIty scHool of meDIcIne, ankara, tUrkey 2 DIvIsIon of enDocrInology anD metabolIsm, Department of Internal meDIcIne, Hacettepe UnIversIty scHool of
meDIcIne, ankara, tUrkey 3 DIvIsIon of gastroenterology, Department of Internal meDIcIne, Hacettepe UnIversIty scHool of meDIcIne,
ankara, tUrkey
-
2016
2620 - 23 October, 2016 Antalya - Turkey
Introduction: Papillary thyroid carcinoma (PTC) is the most com-mon malignancy of the thyroid gland. Metastasis to the regional lymph nodes is relatively high, and the most common distant me-tastasis sites are the lung and bone. Skin metastasis of PTC is very rare, whereas scalp is the most frequent cutaneous area involved.
Case Presentation: 80-year-old female with history of hyperten-sion and diabetes was referred to neurosurgery clinic due to a pro-gressively enlarging lump at the frontal head region for 4 years. CT scan revealed a heterogeneously enhancing semisolid lesion measuring 115x84x69 mm. The lesion was found to be causing ex-tensive frontal bone destruction with associated superior sagittal sinus invasion. Incisional biopsy of the lesion came back as well- differentiated thyroid carcinoma metastasis with positive staining for TTf-1 and thyroglobulin. Her TSH level was suppressed with a value of 0.18 mIU/ml and with normal fT4 and fT3 levels (10.56 pmol/L, fT3: 5.94 pmol/L, respectively). Thyroid ultrasonography exam revealed a left lobe located hypoechoic solid nodule with pe-ripheral coarse eggshell calcifications measuring 30x20 mm. This nodule was found to be cold on thyroid scintigraphy. US guided fine needle aspiration biopsy of the nodule was reported to be highly
suspicious for follicular thyroid carcinoma. Genomic studies re-vealed negative Pax8-PPARg gene rearrangement. PET-CT study performed after the biopsy did not detect any additional metastatic foci. The patient underwent total thyroidectomy and final patholog-ic examination revealed a 4 cm diameter and encapsulated type papillary thyroid carcinoma of follicular variant. The serum fT4 and fT3 levels remained elevated after total thyroidectomy (with the lev-els of 37.78 pmol/L and 12.04 pmol/L, respectively) a finding which we ascribed to continued, and uncontrolled, thyroid hormone pro-duction by the metastatic head lesion.
Based on these clinical and laboratory findings, we started oral methimazole therapy. After consultation with neurosurgery de-partment the lesion was planned for cytoreductive surgery as the patient was not a candidate for complete resection.
Discussion: Cutaneous thyroid carcinoma metastasis is highly unusual and it generally occurs in the setting of disseminated ad-vanced stage disease.
Keywords: papillary thyroid carcinoma, skin metastasis,scalp
O – 19 thyroid
a lumP On tHe sCalP: an unusual PresentatiOn Of PaPillary tHyrOid CarCinOma
DAMLA EyüPOğLU1, UğUR üNLüTüRK2
1 Department of Internal meDIcIne, Hacettepe UnIversIty, ankara, tUrkey 2 Department of enDocrInology anD metabolIsm, Hacettepe UnIversIty, ankara, tUrkey
-
2016
2720 - 23 October, 2016 Antalya - Turkey
Introduction: Wernicke encephalopathy (WE) is an acute neurologic disorder and results from deficiency of thiamine (vitamin B1). Tradi-tional clinical triad is occulomotor abnormalities, confusion and gait ataxia. It has a high chance of recovery through thiamine treatment. However, since there is a serious mortality risk, conditions other than alcoholism which may lead to malabsorption should be included in the differential diagnosis. In this report, a WE case which developed after Roux-en-y gastric bypass surgery due to morbid obesity is presented.
Case Report: A female patient, aged 47 and known to have had dia-betes mellitus for 17 years and getting insulin treatment, underwent a gastric bypass operation in November 2014 since BMI was 51.4 kg/m2. After two months from the operation, the patient was hospitalized due to dizziness, fatique, nausea and vomiting. After 6 months from the operation, the patient was observed to have lost 53 kg.
In the physical examination, the general condition of the patient was good; and there were pearlescent striae and surgical scars on the abdomen. In the neurological examination, the patient was con-scious, cooperative, oriented and had end-point nystagmus. Deep tendon reflexes were symmetrical and normal, romberg test was negative but ataxia was present.
In biochemical examination, Hba1c was %7.6, Hb was 9.7 g/dl, cre-atinine was 1.12 mg/dL, and iron parameters, B12 and folic acid were normal. In cranial MRI, multiplane monitoring was carried out at TSE (turbo spin echo) and fLAIR (fluid-attenuated inversion recovery) sequences. In supratentorial sections, on T2-weighted and fLAIR images hyperintensity was detected in mamillary body and periaqueaductal area. In diffusion weighted MRI, acute isch-emia or diffusional restriction were not detected. With reference to the MRI findings, WE was thought to be present in the patient who had rapid weight loss after gastric bypass surgery. Intravenous thiamine treatment 500 mg/day was started. It was given for two days and then the treatment continued with oral administration of vitamine B. The symptoms were regressed significantly in a week.
Conclusion: Roux-en-y gastric bypass is a bariatric surgery which gives good results in the long term. However, in the post-operative pe-riod nausea and vomiting occur frequently. Wernicke Encephalopathy
is a disorder resulting from a combination of ataxia, ophthalmople-gia, nystagmus, mental confusion and lack of vitamin B1. Thiamine deficiency can be seen in alcoholism, prolonged fasting, hyperemesis gravidarum, prolonged parenteral nutrition, dialysis and AIDS. If Wer-nicke Encephalopathy is not treated, it can cause catastrophic amne-sia, Korsakoff’s psychosis and death. In conclusion, like in this case, it should be kept in mind that Wernicke Encephalopathy may be seen in patients who have complaints of dizziness after gastric bypass.
Keywords: Wernicke encephalopaty, thiamine, gastric bypass
figure 1. Periaquaductal involvement in axial T2
figure 2
figure 2. Mamillary body in T2 fLAIR(marked with pink arrow) and periaquaductal hyperintense areas(marked with yellow arrow)
O – 20 lipids/Obesity
WerniCke enCePHalOPatHy in a Case WHO Had gastriC ByPass surgery due tO mOrBid OBesityHATiCE ÖzIşIK1, BANU şARER yüREKLi1, NiLüfER ÖzDEMiR KUTBAy1, ILGIN yILDIRIM şiMşiR1,
CAN EMRE ERDOğAN2, füSUN SAyGILI1
1 Department of enDocrInology, ege UnIversIty, İzmIr, tUrkey 2 Department of general neUrology, ege UnIversIty, İzmIr, tUrkey
-
2016
2820 - 23 October, 2016 Antalya - Turkey
Background: Celiac disease (CD) is a malabsorption syndrome. Its coexistence with type 1 diabetes mellitus (t1DM) has been proven. Growth retardation is the most common cause that leads to the diagnosis in childhood and adolescence.
Clinical Case: A 7.5-year-old girl presented with hematuria and poly-uria. She was born at term after an uneventful pregnancy with normal vaginal delivery (birth weight: 3720gr). Her height followed the 97th percentile (her target height was at 75th percentile). Since then, her weight increased inappropriately due to unhealthy diet and exercise absence. At the admission her BMI was 24.4 (>97th centile). She devel-oped body odor and pubic hair at the age of 7 years. Both her parents had constitutional delay of growth and puberty. Regarding her family history, her mother and maternal grandmother had nephrolithiasis, her maternal grandfather had t2DM and her father had hypertension. Her mother also reported a history of gestational diabetes during her second pregnancy. On physical examination, she was prepubertal (Tanner stage: Breast 1, Pubic Hair 2, Axillary Hair 1) and acanthosis nigricans was noticed. Her initial investigation tests revealed cystitis and severe hypeglycemia. Her HbA1c level was 9.1% and she was put on insulin treatment and antibiotics. Due to obesity and family history of diabetes, it was ordered further laboratory workup that supported
the diagnosis of t1DM by revealing very high Anti-GAD and Anti-insu-lin antibodies levels. Moreover, she was checked for Hashimoto thy-roiditis and CD and was found very high Antigliadin IgG, Anti-tTG IgA and Anti-endomysial antibodies levels. HLA class II typing revealed the presence of DQA1*05 and DQB1*02 alleles that encode HLA-DQ2 heterodimer found in approximately 95% of patients with CD. Subse-quently, gastroscopy led to the diagnosis of CD. Her bone age was 2.5 years ahead of chronological age. She was prescribed a specific diet and exercise program that led to weight loss while two months later, following the CD diagnosis, she was put on gluten free diet. As soon as she left hospital, her insulin requirements decreased and 20 days after the onset of therapy she stopped insulin due to repeated hypogly-cemic episodes. Her HbA1c level was within normal range 4 months later and she was off insulin treatment for 8 months. After that period hyperglycemic episodes were noticed, HbA1c level increased and she was put on insulin treatment again.
Conclusion: Even though obesity is very uncommon between pa-tients with CD, it is necessary for every patient with t1DM to be evaluated for CD at the time of t1DM diagnosis and on regular basis thereafter.
Keywords: diabetes, celiac disease, obesity
O - 21 diabetes
tHe investigatiOn fOr CeliaC disease in a neWly diagnOsed Patient WitH diaBetes is
neCessary in any CaseMARIA PAPAGIANNI1, GEORGE PALTOGLOU2, GEORGE MASTORAKOS3
1 enDocrIne UnIt, tHIrD Department of peDIatrIcs, arIstotle UnIversIty of tHessalonIkI, HIppokrateIon general HospItal of tHessalonIkI, tHessalonIkI, greece
2 fIrst Department of peDIatrIcs, “agHIa sofIa” cHIlDren’s HospItal, atHens UnIversIty meDIcal scHool, atHens, greece
3 enDocrIne UnIt, seconD Department of obstetrIcs anD gynecology, areteIon HospItal, atHens UnIversIty meDIcal scHool, atHens, greece
-
2016
2920 - 23 October, 2016 Antalya - Turkey
Mauriac syndrome (MS) is an underrecognized complication, char-acterized by short stature, delayed puberty mostly in adolescents with poor control of type 1 diabetes metllitus (T1DM). It presents with cushingoid features and hepatomegaly due to hepatic glucog-enosis with altered liver enzymes.
A 20-year-old female with a-17 year history of T1DM was admit-ted with diabetic ketoacidosis and for further evaluation of her lat-est poor glycemic control and abdominal distension, she had for a long time. The patient was on intensive insulin treatment since her disease onset. Her first diabetic ketoacidosis was documented in 2014. Her present admission was due to her third diabetic ketoac-idosis. Her ever lowest HbA1c was 8%, but last several years her A1c levels have been measured between 9.2-11%.
Anthropometric data revealed height 146 cm (
-
2016
3020 - 23 October, 2016 Antalya - Turkey
Primary bilateral macronodular adrenal hyperplasia (BMAH) is a rare condition, characterized by enlarged adrenal glands and se-cretion of cortisol independent of pituitary adrenocorticotropic hormone (ACTH) which results in subclinical or overt Cushing syn-drome (CS). Bilateral adrenalectomy is the standard of care in overt CS but it imposes primary adrenal insufficieny and requires life long glucocorticoid replacement. We describe a patient with BMAH who underwent unilateral adrenalectomy of the enlarged adrenal gland and subsequently displayed remission of CS.
57 year old woman with a history of type 2 diabetes mellitus (DM) and hypertension for 5 years, atrial fibrillation and ischemic stroke for 3 years admitted to our clinic because of bilateral adrenal en-largement on MRI that’s seen due to abdominal pain. On physical examination, patient was found to have centripedal obesity with BMI 34 kg/m², plethora and buffalo hump. Her blood pressure was 140/80 mmHg under ramipril 5 mg and carvedilol 12,5 mg treat-ment. With metformin 2000 mg, insulin aspart 3x10 ü and insu-lin detemir 1x16 ü the patient’s HbA1C level was %6,7. Contrast enhanced CT revealed multinodular enlargement of both adrenal glands with left side predominance and the largest nodules were 40x40 mm on left side and 22x20 mm on right side.
Endocrine assesment showed 3-4 fold increased urinary cortisol lev-els, loss of diurnal rhythm with elevated late night serum and salivary cortisol levels. Plasma cortisol was not suppressed in a 2 mg dexa-metasone suppression test (DST). Plasma ACTH level was < 5 pg/
ml showing the etiology of CS as adrenal gland. 24 hour urinary ca-thecholamines, 17-OH progesterone and DHEA-S levels were normal. Tests for aberrant receptor expression was normal. With the diagnosis of CS due to BMAH we decided on unilateral adrenalectomy of the pre-dominantly enlarged gland and the patient underwent laparoscopic left adrenalectomy. On macroscopic examination adrenal gland size was 9,5x5x4,5 cm consisting of multipl yellow nodules. Microscopic examination revealed multiple nodules composed of lipid rich clear cells and Ki-67 proliferation index was %2.
Serum cortisol was 4,3 µg/dl on post operative day 1 and hydrocor-tisone 25 mg was started. Two months after surgery ACTH stimula-tion test was normal and hydrocortisone was stopped. One month later urinary cortisol, late night salivary cortisol were normal and cortisol was suppressed in response to 2 mg DST and CS was in remission. At the last visit 8 months after surgery the patient was in remission, lost 12 kg weight and DM was treated with metformin alone without insülin requirement and HbA1C level was %5.8. We follow-up patient with six months intervals.
Unilateral adrenalectomy of the larger gland appears to be an ef-fective treatment for BMAH. It may result in remission of CS and improves obesity and diabetes. But follow-up of the patient is re-quired for recurrence of the disease.
Keywords: Cushing syndrome, primary bilateral macronodular adrenal hyperplasia, unilateral adrenalectomy
O – 23 adrenal
unilateral adrenaleCtOmy imPrOves CusHing syndrOme in a Patient WitH Primary Bilateral
maCrOnOdular adrenal HyPerPlasiaALPER çAğRI KARCI, zEyNEP çETiN, NARiN NASIROğLU iMGA, DiLEK BERKER, SERDAR GüLERDepartment of enDocrInology anD metabolIsm, ankara nUmUne eDUcatIonal anD researcH HospItal, ankara,
tUrkey
Table 1. Laboratuary tests for Cushing syndrome evaluation
AT DIAGNOSIS POST-OP 3 MONTHS POST-OP 8 MONTHS
ACTH (pg/ml)
-
2016
3120 - 23 October, 2016 Antalya - Turkey
Background: Congenital adrenal hyperplasia (CAH) is one of auto-somal recessive disorders resulting from CyP 21(21-hydroxylase) deficiency. Testicular adrenal rest tumors (TARTs) are common in CAH, due to hyper-secretion of ACTH. These lesions inside the tes-tis are bilateral and multiple. TARTs may lead to structural damage and their tumors may be mistaken for Leydig cell tumor. Because of their locations; TART may cause seminiferous obstruction and infertility.
History: 6-year old boy presented with early growth of pubic hair, the condition started at age of four years when his parents noticed that their child has developed pubic hair. They also noticed that he is taller than his siblings with abnormal behavior and deepening of voice. There is history of sudden death of his brother when he was 22 days old. Testicular examination was normal. Physical ex-amination revealed develpoment of pubic hair (stage 4) and adult scrotum.
Diagnosis and Treatment: His random 17OH progesterone was 60.80 mg/ml (increased by more than 60 folds, repeated result for 17OH progesterone showed increase by more than 20 folds). U/S and MRI showed testicular tumors keeping with TARTs. We started patient on HC tabs with consultation of urologist . Continuous fol-low up of these tumors were done.
Conclusion: Giving the clinical presentation, biochemical profile and MRI findings, the diagnosis is keeping with CAH complicated with TARTs. Multidisciplinary approach with the involvement of en-docrinologist, pathologist and urologist is of great importance for the correct diagnosis and treatment. The aim is to draw the atten-tion of the clinicians to the presence of the TARTs and to evaluate critically every patient with testicular tumors concomitantly with CAH. It’s very important to consider treatment of CAH to prevent short stature in future.
Keywords: CAH, TART, precocious pubery
O – 24 adrenal
CaH Presenting as Premature PuBerty WitH assOCiated testiCular adrenal rest tumOrs
(tart)BAyAR AHMED QASIM
Dpartment of meDIcIne, UnIversIty of DUHok, Iraq
-
2016
3220 - 23 October, 2016 Antalya - Turkey
Introduction: Adrenocortical carcinoma (ACC) is a rare disease with poor prognosis. About 42% to 57% of patients with ACC pres-ent with symptoms of hormonal excess such as Cushing syndrome or virilization. Non-functional tumors usually present with abdom-inal or flank pain, varicocele and renal vein thrombosis. In addition, a growing proportion of these patients (>15%) is initially diagnosed incidentally. Here we report 3 ACC cases with different clinical pre-sentations.
Case 1: A 38-year-old female patient admitted to our clinic with low back and abdominal pain, weight loss, and hirsutism. On phys-ical examination, her body mass index was 17.3 kg/m2 and ferri-man-Gallwey score (fGS) was 10. She had a history of vena cava inferior (VCI) thrombosis and a filter was put in another center 6 months ago. Abdominal ultrasonography (US) revealed invasion and thrombosis in VCI and multiple metastatic lesions with the big-gest diameter of 58 mm in the liver. In computerized tomography (CT), a 200x95 mm lesion in the left adrenal gland was observed. Basal cortisol and ACTH levels were 11.4 mcg/dL and 4.6 mcg/dL, respectively. Overnight 1 mg and 2 days 2 mg dexamethasone sup-pression tests (DSTs) showed no suppression in the morning fast-ing cortisols. DHEAS was 907 mcg/dl (normal limits: 0-340 mcg/dl) (Table 1). The percutaneous biopsy of metastatic mass in the liver revealed ACC and the patient was evaluated as inoperable.
Case 2: A 57-year-old female patient admitted to internal medicine clinic with fatigue, abdominal pain and high blood pressure. She was referred to our clinic due to low potassium (3.1mEq/L) concen-tration. In further laboratory examination, basal cortisol was 11.8 mcg/dL, ACTH was 2.6 mcg/dL, DHEAS was very high (1000 mcg/dl) and plasma aldosteron/renin ratio was normal. Abdominal CT revealed a 110x88 mm mass in the right adrenal gland. There was no suppression in overnight 1 mg and 2 days 2 mg DSTs (Table 1). Patient underwent right adrenalectomy and pathology was consis-tent with ACC.
Case 3: A 52-year-old female patient admitted to our clinic with hirsutism in the last 6 months. On physical examination, her body mass index was 31 kg/m2 and plethora, moon face, abdominal obe-sity, abdominal blue-purple striae, and buffalo hump were present. Basal cortisol and ACTH were 23.0 mcg/dl and 1.0 pg/ml, respec-tively. DHEAS was 884 mcg/dl. Overnight single dose of 1 mg and 2 days 2 mg DSTs showed no suppression (Table 1). Adrenal Cush-ing’s syndrome was diagnosed. A 80x60 mm mass in the left adre-nal gland was observed in abdominal CT. Right adrenalectomy was performed and the histopathological diagnosis was ACC.
Conclusion: ACC is seen more commonly, diagnosed at a young-er age and more often functional in females compared to males. The clinical presentation varies in a wide spectrum ranging from asymptomatic/mild disease as in case 3 to symptoms related with hormone overproduction as in case 2 and to severe life threating metastasis as in case 1.
Keywords: adrenocortical cancer, cushing syndrome, inferior vena cava trombosis, hypokalemia
Figure 1
Adrenal masses in patients Case 1: 200x95 mm heterogeneous ne-crotic hypodense solid lesion in the left adrenal gland (CT) Case 2: 110x88 mm heterogeneous necrotic solid lesion in the right adre-nal gland (CT) Case 3: 80x60 mm heterogeneous solid lesion in the left adrenal gland (CT)
O – 25 adrenal
different CliniCal PresentatiOns in tHree Patients WitH adrenOCOrtiCal CanCerNAGiHAN BEşTEPE1, DiDEM ÖzDEMiR1, şEfiKA BURçAK POLAT1, MEHMET KILIç2,
AyDAN KILIçARSLAN3, MELiKE RUşEN METiN4, REyHAN ERSOy1, BEKiR çAKIR1
1 yIlDIrIm beyazIt UnIversIty facUlty of meDIcIne, Department of enDocrInology anD metabolIsm ankara, tUrkey 2 yIlDIrIm beyazIt UnIversIty facUlty of meDIcIne, Department of general sUrgery, ankara, tUrkey
3 yIlDIrIm beyazIt UnIversIty facUlty of meDIcIne, Department of patHology, ankara, tUrkey 4 atatürk eDUcatIon anD researcH HospItal, Department of raDIology, ankara, tUrkey
-
2016
3320 - 23 October, 2016 Antalya - Turkey
Table 1: Clinical, laboratory and radiological findings of patients
Case 1 Case 2 Case 3
Age /sex 38/female 57/female 52/female
Presentation Abdominal pain, weight loss, hirsutism, inferior vena cava thrombosis
fatigue, abdominal pain high blood pressure, hypokalemia
Hirsutism, moon face, blue-purple striae, buffalo hump
Basal cortisol (mcg/dl) 11.4 11.8 23
ACTH (pg/ml) 4.6 2.6 1
Overnight DST (mcg/dl) 10.2 12.4 24
Low dose DST (Liddle) (mcg/dl) 13.1 12.9 25.8
8 mg DST (mcg/dl) 12.6 13.2 23.2
24 hour urinary catecholamines Normal Normal Normal
Aldosterone/renin ratio Normal Normal Normal
DHEAS04 (0-340mcg/dl) 907 1000 884
17-OH progesterone (0.27-1.99) (ng/ml) 6.2 2.5 0.8
Adrenal imaging 200x95 mm heterogeneous necrotic hypodense solid lesion in the left adrenal gland, metastatic lesions (max 58 mm) in the liver
110x88 mm heterogeneous necrotic solid lesion in the right adrenal gland
80x60 mm heterogeneous solid lesion in the left adrenal gland
-
2016
3420 - 23 October, 2016 Antalya - Turkey
Case Presentation: A 60 years old Caucasian heavy smoker man presented with cough and backache for four months as well as gradually worsening weakness, intermittent abdominal pain and slight hyperpigmentation. Because of the above, the primary care physician from a Greek island where the patient lived ordered a CT, which incidentally revealed bilateral lesions in adrenal glands (8 cm R and 7 cm L) (fig. 1). He was then referred to our hospital for further investigation and treatment. On admission, the patient presented with dehydration, hyperpigmentation, cachexia and or-thostatic hypotension. Laboratory evaluation revealed: Glu=115mg/dl, Creat=1.9mg/dl, K=5.7mEq/l, Na=121mEq/l, f=5 μg/dl, ACTH=831pg/ml, DHEAS=13mg/dl and Renin=217 pg/ml. Abdom-inal MRI confirmed bilateral cystic hemorrhagic adrenal lesions, while a mass of similar imaging characteristics (5 x 4 cm) at the lower pole of the left kidney was visible. The diagnosis was acute adrenal insufficiency due to secondary metastases. After hydration and replacement therapy with hydrocortisone and fludrocortisone symptoms gradually improved. A brain and neck CT as well as a bone scan did not reveal any other pathological findings consistent with malignancy. Biochemical cancer markers were negative too. A biopsy of the lesion at the lower pole of the left kidney under CT guidance was performed and resulted in findings consistent with sarcomatoid renal cell carcinoma. Thus, the patient underwent left radical nephrectomy-adrenalectomy. The histopathology examina-tion confirmed the diagnosis of sarcomatoid renal cell carcinoma.
Discussion: Adrenal incidentalomas are most commonly unilater-al. Nevertheless, bilateral adrenal incidentalomas are reported in 7.8-15% of cases. Most of them represent single discrete bilateral lesions, while in a small percentage appear as diffuse adrenal hy-perplasia or enlargement. The majority of lesions are benign and non-functional. However, the possibility of congenital adrenal hy-perplasia, metastases, hemorrhage, pheochromocytoma, lympho-
ma, infectious or metabolic storage diseases is higher compared to unilateral lesions. Acute adrenal insufficiency due to adrenal metastases is uncommon, despite the fact that adrenal glands rep-resent a common metastasis site for several solid tumors. This is likely due to the sufficient functional compensation by the adrenal glands and the fact that the signs and symptoms of deficiency are non-specific and often masked by the symptoms of neoplastic dis-ease. Renal cell carcinomas can metastasize to the adrenal glands via both the lymphatic and the venous system, but bilateral presen-tation of adrenal metastases is extremely rare. The optimal strate-gy for the detection of adrenal metastases including the possibility of biopsy as well the best treatment option are not clear in the lit-erature and should be individualized. The diagnosis and treatment approach needs multidisciplinary team collaboration with active participation of endocrinologists.
Keywords: adrenal, incidentalomas, bilateral, metastases
Figure 1: Chest VT: arrows indicate bilateral adrenal
lesions revealed incidentally
figure 1. Chest VT: arrows indicate bilateral adrenal lesions re-vealed incidentally
O – 26 adrenal
Bilateral CystiC HemOrrHagiC adrenal inCidentalOmas
STAVROULA A. PASCHOU1, KONSTANTINOS TzIORAS1, CHRISTINA NIKA1, ATHANASIOS PAPATHEODOROU2, VASSILIS SAMARAS3, ANDROMACHI VRyONIDOU1
1 Department of enDocrInology anD DIabetes, HellenIc reD cross HospItal, atHens, greece 2 Department of raDIology, HellenIc reD cross HospItal, atHens, greece 3 Department of patHology, HellenIc reD cross HospItal, atHens, greece
-
2016
3520 - 23 October, 2016 Antalya - Turkey
Introduction: Primary adrenal cortical carcinoma is a high-grade tumor associated with poor prognosis. Sixty percent of adrenal car-cinomas are functional. Thirty percent of these patients may exhibit Cushing’s syndrome. This is the first case report in the literature of an adrenal carcinoma presenting with Cushing’s syndrome devel-oping on 8 year history of adrenomyolipomas and adrenal insuffi-ciency.
Case: A fifty years old male patient was admitted with fatigue and hyperpigmentation to another instution in 2008, when he was diag-nosed with