WAPEBB - Guide to Your Benefits and Services · Your first annual wellness visit can't take place...
Transcript of WAPEBB - Guide to Your Benefits and Services · Your first annual wellness visit can't take place...
-
GUIDE TOYOUR BENEFITSAND SERVICES
kp.org
-
1
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
Medical Benefits Chart: Senior Advantage without Part D
Medicare-Eligible Washington PEBB Employees 1983 - 301-307 For group benefits effective January 1, 2020, through December 31, 2020
You will see this apple next to the preventive services in this Medical Benefits Chart.
Services that are covered for you What you must pay when you get these services
Maximum out-of-pocket amount $1,500 per person per year.
Abdominal aortic aneurysm screening A one-time screening ultrasound for people at risk. Our plan only covers this screening if you have certain risk factors and if you get a referral for it from your physician, physician assistant, nurse practitioner, or clinical nurse specialist.
There is no coinsurance, copayment, or deductible for members eligible for this preventive screening.
Alternative care therapies (self-referred) $30 per chiropractic visit up to 12 visits per calendar year. Additional visits provided if treatment extension is approved by a network provider.
See the "Chiropractic services" section in this Medical Benefits Chart for physician-referred chiropractic services.
(See the Chiropractic Services Rider in the EOC for additional information about self-referred chiropractic services.)
Ambulance services • Covered ambulance services include fixed wing, rotary
wing, and ground ambulance services to the nearest appropriate facility that can provide care if they are furnished to a member whose medical condition is such that other means of transportation could endanger the person's health or if authorized by our plan.
$50 per one-way trip.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
2
Services that are covered for you What you must pay when you get these services
• We also cover the services of a licensed ambulance anywhere in the world without prior authorization (including transportation through the 911 emergency response system where available) if you reasonably believe that you have an emergency medical condition and you reasonably believe that your condition requires the clinical support of ambulance transport services.
• You may need to file a claim for reimbursement unless the provider agrees to bill us (see Chapter 5).
• †Nonemergency transportation by ambulance is appropriate if it is documented that the member's condition is such that other means of transportation could endanger the person's health and that transportation by ambulance is medically required.
Annual routine physical exams Routine physical exams are covered if the exam is medically appropriate preventive care in accord with generally accepted professional standards of practice. This exam is covered once every 12 months.
There is no coinsurance, copayment, or deductible for this preventive care.
Annual wellness visit If you've had Part B for longer than 12 months, you can get an annual wellness visit to develop or update a personalized prevention plan based on your current health and risk factors. This is covered once every 12 months.
Note: Your first annual wellness visit can't take place within 12 months of your "Welcome to Medicare" preventive visit. However, you don't need to have had a "Welcome to Medicare" visit to be covered for annual wellness visits after you've had Part B for 12 months.
There is no coinsurance, copayment, or deductible for the annual wellness visit.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
3
Services that are covered for you What you must pay when you get these services
Bone mass measurement For qualified individuals (generally, this means people at risk of losing bone mass or at risk of osteoporosis), the following services are covered every 24 months or more frequently if medically necessary: procedures to identify bone mass, detect bone loss, or determine bone quality, including a physician's interpretation of the results.
There is no coinsurance, copayment, or deductible for Medicare-covered bone mass measurement.
Breast cancer screening (mammograms) Covered services include:
• One baseline mammogram between the ages of 35 and 39.
• One screening mammogram every 12 months for women age 40 and older.
• Clinical breast exams once every 24 months.
There is no coinsurance, copayment, or deductible for covered screening mammograms.
Cardiac rehabilitation services† Comprehensive programs for cardiac rehabilitation services that include exercise, education, and counseling are covered for members who meet certain conditions with a doctor's order. Our plan also covers intensive cardiac rehabilitation programs that are typically more rigorous or more intense than cardiac rehabilitation programs.
$30 per visit.
Cardiovascular disease risk reduction visit (therapy for cardiovascular disease) We cover one visit per year with your primary care doctor to help lower your risk for cardiovascular disease. During this visit, your doctor may discuss aspirin use (if appropriate), check your blood pressure, and give you tips to make sure you're eating healthy.
There is no coinsurance, copayment, or deductible for the intensive behavioral therapy cardiovascular disease preventive benefit.
Cardiovascular disease testing Blood tests for the detection of cardiovascular disease (or abnormalities associated with an elevated risk of cardiovascular disease) once every five years (60 months).
There is no coinsurance, copayment, or deductible for cardiovascular disease testing that is covered once every five years.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
4
Services that are covered for you What you must pay when you get these services
Cervical and vaginal cancer screening Covered services include:
• For all women: Pap tests and pelvic exams are covered once every 24 months.
• If you are at high risk of cervical or vaginal cancer or you are of childbearing age and have had an abnormal Pap test within the past three years: one Pap test every 12 months.
There is no coinsurance, copayment, or deductible for Medicare-covered preventive Pap and pelvic exams.
Chiropractic services† Covered services include:
• We cover only manual manipulation of the spine to correct subluxation. These Medicare-covered services are provided by a participating chiropractor of the CHP Group and listed in the Provider Directory.
$20 per office visit.
Colorectal cancer screening • For people 50 and older, the following are covered:
♦ Flexible sigmoidoscopy (or screening barium enema as an alternative) every 48 months.
• One of the following every 12 months: ♦ Guaiac-based fecal occult blood test (gFOBT). ♦ Fecal immunochemical test (FIT).
• DNA-based colorectal screening every 3 years. • For people at high risk of colorectal cancer, we cover a
screening colonoscopy (or screening barium enema as an alternative) every 24 months.
• For people not at high risk of colorectal cancer, we cover a screening colonoscopy every 10 years (120 months), but not within 48 months of a screening sigmoidoscopy.
There is no coinsurance, copayment, or deductible for a Medicare-covered colorectal cancer screening exam.
Depression screening We cover one screening for depression per year. The screening must be done in a primary care setting that can provide follow-up treatment and/or referrals.
There is no coinsurance, copayment, or deductible for an annual depression screening visit.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
5
Services that are covered for you What you must pay when you get these services
Diabetes screening We cover this screening (includes fasting glucose tests) if you have any of the following risk factors: high blood pressure (hypertension), history of abnormal cholesterol and triglyceride levels (dyslipidemia), obesity, or a history of high blood sugar (glucose). Tests may also be covered if you meet other requirements, like being overweight and having a family history of diabetes.
Based on the results of these tests, you may be eligible for up to two diabetes screenings every 12 months.
There is no coinsurance, copayment, or deductible for the Medicare-covered diabetes screening tests.
Diabetes self-management training and diabetic services and supplies For all people who have diabetes (insulin and noninsulin users), covered services include:
• †Supplies to monitor your blood glucose: Blood glucose monitor, blood glucose test strips, lancet devices, lancets, and glucose-control solutions for checking the accuracy of test strips and monitors.
No charge.
• †For people with diabetes who have severe diabetic foot disease: One pair per calendar year of therapeutic custom-molded shoes (including inserts provided with such shoes) and two additional pairs of inserts, or one pair of depth shoes and three pairs of inserts (not including the noncustomized removable inserts provided with such shoes). Coverage includes fitting.
No charge.
• Diabetes self-management training is covered under certain conditions.
There is no coinsurance, copayment, or deductible for members eligible for the diabetes self-management training preventive benefit.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
6
Services that are covered for you What you must pay when you get these services
Durable medical equipment (DME) and related supplies† (For a definition of "durable medical equipment," see Chapter 10 of this booklet.)
Covered items include, but are not limited to: wheelchairs, crutches, powered mattress systems, diabetic supplies, hospital beds ordered by a provider for use in the home, IV infusion pumps, speech-generating devices, oxygen equipment, nebulizers, and walkers.
We cover all medically necessary DME covered by Original Medicare. If our supplier in your area does not carry a particular brand or manufacturer, you may ask them if they can special order it for you. The most recent list of suppliers is available on our website at kp.org/directory.
No charge for durable medical equipment.
No charge for certain items such as CADD pumps, bone and spine stimulators, ventilators and enteral pumps and supplies.
Emergency care Emergency care refers to services that are:
• Furnished by a provider qualified to furnish emergency services, and
• Needed to evaluate or stabilize an emergency medical condition.
A medical emergency is when you, or any other prudent layperson with an average knowledge of health and medicine, believe that you have medical symptoms that require immediate medical attention to prevent loss of life, loss of a limb, or loss of function of a limb. The medical symptoms may be an illness, injury, severe pain, or a medical condition that is quickly getting worse.
Cost-sharing for necessary emergency services furnished out-of-network is the same as for such services furnished in-network.
You have worldwide emergency care coverage.
$50 per Emergency Department visit. This copayment does not apply if you are immediately admitted directly to the hospital as an inpatient (it does apply if you are admitted to the hospital as an outpatient; for example, if you are admitted for observation).
†If you receive emergency care at an out-of-network hospital and need inpatient care after your emergency condition is stabilized, you must return to a network hospital in order for your care to continue to be covered or you must have your inpatient care at the out-of-network hospital authorized by our plan and your cost is the cost-sharing you would pay at a network hospital.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
7
Services that are covered for you What you must pay when you get these services
Fitness benefit (Silver&Fit® Exercise and Healthy Aging Program) With the Silver&Fit program, you can choose membership in a participating fitness center or the Silver&Fit Home Fitness Program.
• You can join a participating Silver&Fit fitness center in our service area and take advantage of all of the services and amenities that are part of your basic fitness center membership. Amenities offered by fitness centers vary by center. Any nonstandard fitness center service that typically requires an additional fee is not included in your basic fitness membership (for example, court fees or personal trainer services). You can switch from one participating Silver&Fit fitness center once a month and your change will be effective the first of the following month. (You may need to complete a new membership agreement at the center.)
• In lieu of a fitness facility membership, if you prefer to work out at home, you may want to sign up for the Silver&Fit Home Fitness Program and receive up to two fitness kits each calendar year for use at home.
• Also, you have access to healthy aging educational materials by visiting kp.org/SilverandFit. Or you can request a selection of healthy educational materials be mailed to you every quarter once you have enrolled into a program.
If you have questions or want to enroll or get a list of participating fitness center locations, visit kp.org/SilverandFit or call Silver&Fit Customer Service at 1-877-750-2746 (TTY/TDD users should call 711), Monday–Friday, between 5 a.m. and 6 p.m. (PST).
Note: The Silver&Fit Program is provided by American Specialty Health Fitness, Inc., a subsidiary of American Specialty Health Incorporated (ASH). All programs and services are not available in all areas. Silver&Fit® is a federally registered trademark of American Specialty Health, Inc.
No charge.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
8
Services that are covered for you What you must pay when you get these services
Health and wellness education programs Health and wellness programs include weight management, quitting tobacco, diabetes management, life care planning, prediabetes, and more. Registered dietitians, health coaches, certified diabetes educators, and other health professionals facilitate our classes. We offer in-person, online, and phone options to fit your learning style. Please see our health and wellness classes and resources catalog at kp.org/healthylivingcatalog/nw. Contact Member Services for more details or to request a copy of our catalog.
No charge.
Hearing services • Diagnostic hearing and balance evaluations performed by
your provider to determine if you need medical treatment are covered as outpatient care when furnished by a physician, audiologist, or other qualified provider.
• Routine hearing exams.
$30 per office visit.
• Evaluation and fitting for hearing aids. No charge.
• *Hearing aids. Balance after $800 allowance is applied every three years.
(See the Hearing Aid Rider in the EOC for additional information.)
HIV screening • For people who ask for an HIV screening test or who are at
increased risk for HIV infection, we cover one screening exam every 12 months.
• For women who are pregnant, we cover up to three screening exams during a pregnancy.
There is no coinsurance, copayment, or deductible for members eligible for Medicare-covered preventive HIV screening.
• HIV screening test after each exposure. No charge.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
9
Services that are covered for you What you must pay when you get these services
Home-based palliative care† Services not covered by Medicare in the home are provided in the form of palliative care to diminish symptoms of terminally ill members with a life expectancy of 7–12 months. Services include non-Medicare covered palliative nursing and social work services in the home. Contact Member Services for more details.
No charge.
Home health agency care† Prior to receiving home health services, a doctor must certify that you need home health services and will order home health services to be provided by a home health agency. You must be homebound, which means leaving home is a major effort.
Covered services include, but are not limited to:
• Part-time or intermittent skilled nursing and home health aide services. To be covered under the home health care benefit, your skilled nursing and home health aide services combined must total fewer than 8 hours per day and 35 hours per week.
• Physical therapy, occupational therapy, and speech therapy.
• Medical and social services.
• Medical equipment and supplies.
No charge. Note: There is no cost-sharing for home health care services and items provided in accord with Medicare guidelines. However, the applicable cost-sharing listed elsewhere in this Medical Benefits Chart will apply if the item is covered under a different benefit; for example, durable medical equipment not provided by a home health agency.
Home infusion therapy† We cover home infusion supplies and drugs if all of the following are true:
• Your prescription drug is on our standard formulary (or you have a formulary exception).
• We approved your prescription drug for home infusion therapy.
• Your prescription is written by a network provider and filled at a network home-infusion pharmacy.
No charge.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
10
Services that are covered for you What you must pay when you get these services
Hospice care You may receive care from any Medicare-certified hospice program. You are eligible for the hospice benefit when your doctor and the hospice medical director have given you a terminal prognosis certifying that you're terminally ill and have six months or less to live if your illness runs its normal course. Your hospice doctor can be a network provider or an out-of-network provider.
Covered services include:
• Drugs for symptom control and pain relief.
• Short-term respite care.
• Home care. *For hospice services and services that are covered by Medicare Part A or B and are related to your terminal prognosis: Original Medicare (rather than our plan) will pay for your hospice services and any Part A and Part B services related to your terminal prognosis. While you are in the hospice program, your hospice provider will bill Original Medicare for the services that Original Medicare pays for.
For services that are covered by Medicare Part A or B and are not related to your terminal prognosis: If you need nonemergency, non–urgently needed services that are covered under Medicare Part A or B and that are not related to your terminal prognosis, your cost for these services depends on whether you use a provider in our plan's network:
• If you obtain the covered services from a network provider, you only pay the plan cost-sharing amount for in-network services.
• *If you obtain the covered services from an out-of-network provider, you pay the cost-sharing under Fee-for-Service Medicare (Original Medicare).
For services that are covered by our plan but are not covered by Medicare Part A or B: We will continue to cover plan-covered services that are not covered under Part A or B whether or not they are related to your terminal prognosis. You pay your plan cost-sharing amount for these services.
When you enroll in a Medicare-certified hospice program, your hospice services and your Part A and Part B services related to your terminal prognosis are paid for by Original Medicare, not our plan.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
11
Services that are covered for you What you must pay when you get these services
Note: If you need nonhospice care (care that is not related to your terminal prognosis), you should contact us to arrange the services.
We cover hospice consultation services (one time only) for a terminally ill person who hasn't elected the hospice benefit.
No charge.
Immunizations Covered Medicare Part B services include:
• Pneumonia vaccine.
• Flu shots, once each flu season in the fall and winter, with additional flu shots if medically necessary.
• Hepatitis B vaccine if you are at high or intermediate risk of getting Hepatitis B.
• Other vaccines if you are at risk and they meet Medicare Part B coverage rules.
There is no coinsurance, copayment, or deductible for the pneumonia, influenza, and Hepatitis B vaccines.
Inpatient hospital care† Includes inpatient acute, inpatient rehabilitation, long-term care hospitals, and other types of inpatient hospital services. Inpatient hospital care starts the day you are formally admitted to the hospital with a doctor's order. The day before you are discharged is your last inpatient day.
There is no limit to the number of medically necessary hospital days or services that are generally and customarily provided by acute care general hospitals. Covered services include, but are not limited to:
• Semiprivate room (or a private room if medically necessary).
• Meals, including special diets.
• Regular nursing services.
• Costs of special care units (such as intensive care or coronary care units).
• Drugs and medications.
$500 per admission. Cost-sharing is charged for each inpatient stay.
If you get authorized inpatient care at an out-of-network hospital after your emergency condition is stabilized, your cost is the cost-sharing you would pay at a network hospital.
Note: If you are admitted to the hospital in 2019 and are not discharged until sometime in 2020, the 2019 cost-sharing will apply to that admission until you are discharged from the hospital or transferred to a skilled nursing facility.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
12
Services that are covered for you What you must pay when you get these services
• Lab tests.
• X-rays and other radiology services.
• Necessary surgical and medical supplies.
• Use of appliances, such as wheelchairs.
• Operating and recovery room costs.
• Physical, occupational, and speech language therapy.
• Inpatient substance abuse services for medical management of withdrawal symptoms associated with substance abuse (detoxification).
• Under certain conditions, the following types of transplants are covered: corneal, kidney, kidney-pancreatic, heart, liver, lung, heart/lung, bone marrow, stem cell, and intestinal/ multivisceral. If you need a transplant, we will arrange to have your case reviewed by a Medicare-approved transplant center that will decide whether you are a candidate for a transplant. Transplant providers may be local or outside of the service area. If our in-network transplant services are outside the community pattern of care, you may choose to go locally as long as the local transplant providers are willing to accept the Original Medicare rate. If we provide transplant services at a location outside the pattern of care for transplants in your community and you choose to obtain transplants at this distant location, we will arrange or pay for appropriate lodging and transportation costs for you and a companion.
• Blood—including storage and administration.
• Physician services.
Note: To be an "inpatient," your provider must write an order to admit you formally as an inpatient of the hospital. Even if you stay in the hospital overnight, you might still be considered an "outpatient." If you are not sure if you are an inpatient or an outpatient, you should ask the hospital staff. You can also find more information in a Medicare fact sheet called "Are You a Hospital Inpatient or Outpatient? If You Have Medicare – Ask!" This fact sheet is available on the Web at https://www.medicare.gov/sites/default/files/2018-09/11435-Are-You-an-Inpatient-or-Outpatient.pdf or by calling 1-800-MEDICARE (1-800-633-4227). TTY users call 1-877-486-2048. You can call these numbers for free, 24 hours a day, 7 days a week.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
13
Services that are covered for you What you must pay when you get these services
Inpatient mental health care† Covered services include mental health care services that require a hospital stay.
• We cover up to 190-days per lifetime for inpatient stays in a Medicare-certified psychiatric hospital. The number of covered lifetime hospitalization days is reduced by the number of inpatient days for mental health treatment previously covered by Medicare in a psychiatric hospital.
• The 190-day limit does not apply to mental health stays in a psychiatric unit of a general hospital.
$500 per admission. Cost-sharing is charged for each inpatient stay.
Note: If you are admitted to the hospital in 2019 and are not discharged until sometime in 2020, the 2019 cost-sharing will apply to that admission until you are discharged from the hospital or transferred to a skilled nursing facility.
Inpatient stay: Covered services received in a hospital or SNF during a noncovered inpatient stay† If you have exhausted your inpatient mental health or skilled nursing facility (SNF) benefits or if the inpatient stay is not reasonable and necessary, we will not cover your inpatient or SNF stay. However, in some cases, we will cover certain services you receive while you are in the hospital or SNF. Covered services include, but are not limited to:
You pay the following for covered outpatient services and other items covered under Medicare Part B when provided by network providers:
• Physician services. $30 per primary care visit. $30 per specialty care visit.
• Diagnostic tests (like lab tests). No charge for lab tests.
• X-rays.
• Radium and isotope therapy including technician materials and services.
No charge per visit, per department, for X-rays.
No charge per visit for radium and isotope therapy.
No charge per visit, per department, for specialty scans such as MRI, CT, PET scans.
• Surgical dressings. No charge for surgical dressings. No charge for take-home dressings and supplies.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
14
Services that are covered for you What you must pay when you get these services
• Splints, casts, and other devices used to reduce fractures and dislocations.
No charge for casts. No charge for splints and other devices to reduce fractures and dislocations.
• Prosthetics and orthotics devices (other than dental) that replace all or part of an internal body organ (including contiguous tissue), or all or part of the function of a permanently inoperative or malfunctioning internal body organ, including replacement or repairs of such devices.
• Leg, arm, back, and neck braces; trusses; and artificial legs, arms, and eyes (including adjustments, repairs, and replacements required because of breakage, wear, loss, or a change in the patient's physical condition).
No charge.
• Physical therapy, speech therapy, and occupational therapy. $30 per visit.
Medical nutrition therapy This benefit is for people with diabetes, renal (kidney) disease (but not on dialysis), or after a kidney transplant when ordered by your doctor.
We cover three hours of one-on-one counseling services during your first year that you receive medical nutrition therapy services under Medicare (this includes our plan, any other Medicare Advantage plan, or Original Medicare), and two hours each year after that. If your condition, treatment, or diagnosis changes, you may be able to receive more hours of treatment with a physician's order. A physician must prescribe these services and renew his or her order yearly if your treatment is needed into the next calendar year.
There is no coinsurance, copayment, or deductible for members eligible for Medicare-covered medical nutrition therapy services.
Medicare Diabetes Prevention Program (MDPP) MDPP services will be covered for eligible Medicare beneficiaries under all Medicare health plans.
MDPP is a structured health behavior change intervention that provides practical training in long-term dietary change, increased physical activity, and problem-solving strategies for overcoming challenges to sustaining weight loss and a healthy lifestyle.
There is no coinsurance, copayment, or deductible for the MDPP benefit.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
15
Services that are covered for you What you must pay when you get these services
Medicare Part B prescription drugs† These drugs are covered under Part B of Original Medicare. Members of our plan receive coverage for these drugs through our plan. Covered drugs include:
• Antigens. No charge.
• Certain drugs for home dialysis, including heparin, the antidote for heparin when medically necessary, topical anesthetics, and erythropoiesis-stimulating agents (such as Epogen, Procrit, Epoetin Alfa, Aranesp, or Darbepoetin Alfa).
No charge.
• Drugs that usually aren't self-administered by the patient and are injected or infused while you are getting physician, hospital outpatient, or ambulatory surgical center services.
No charge.
• Injectable osteoporosis drugs, if you are homebound, have a bone fracture that a doctor certifies was related to post-menopausal osteoporosis, and cannot self-administer the drug.
No charge.
• Clotting factors you give yourself by injection if you have hemophilia.
Your applicable prescription drug copayment or coinsurance.
• Immunosuppressive drugs, if you were enrolled in Medicare Part A at the time of the organ transplant.
Your applicable prescription drug copayment or coinsurance.
• Drugs you take using durable medical equipment (such as nebulizers) that were authorized by our plan.
Your applicable prescription drug copayment or coinsurance.
• Certain oral anti-cancer drugs and anti-nausea drugs. Your applicable prescription drug copayment or coinsurance.
• Intravenous Immune Globulin for the home treatment of primary immune deficiency diseases.
Your applicable prescription drug copayment or coinsurance.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
16
Services that are covered for you What you must pay when you get these services
Obesity screening and therapy to promote sustained weight loss If you have a body mass index of 30 or more, we cover intensive counseling to help you lose weight. This counseling is covered if you get it in a primary care setting, where it can be coordinated with your comprehensive prevention plan. Talk to your primary care doctor or practitioner to find out more.
There is no coinsurance, copayment, or deductible for preventive obesity screening and therapy.
Opioid treatment program services† Opioid use disorder treatment services are covered under Part B of Original Medicare. Members of our plan receive coverage for these services through our plan. Covered services include:
• FDA-approved opioid agonist and antagonist treatment medications and the dispensing and administration of such medications, if applicable.
No charge.
• Substance use counseling. • Individual and group therapy. • Toxicology testing.
$30 per visit.
Outpatient diagnostic tests and therapeutic services and supplies† Covered services include, but are not limited to:
• X-rays.
• Ultrasounds.
• Special diagnostic tests, such as electrocardiograms (EKGs) and Holter monitoring.
No charge per visit, per department.
• Radiation (radium and isotope) therapy, including technician materials and supplies.
No charge per visit.
• Surgical supplies, such as dressings.
• Splints, casts, and other devices used to reduce fractures and dislocations.
No charge for surgical supplies or casts. No charge for take-home dressings and supplies, splints, and other devices to reduce fractures and dislocations.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
17
Services that are covered for you What you must pay when you get these services
• Laboratory tests. No charge.
• Blood—including storage and administration. No charge.
• Other outpatient diagnostic tests: ♦ Special imaging procedures, for example, MRI, CT, and
PET scans.
No charge per visit, per department.
Outpatient hospital observation† Observation services are hospital outpatient services given to determine if you need to be admitted as an inpatient or can be discharged.
For outpatient hospital observation services to be covered, they must meet the Medicare criteria and be considered reasonable and necessary. Observation services are covered only when provided by the order of a physician or another individual authorized by state licensure law and hospital staff bylaws to admit patients to the hospital or order outpatient tests.
Note: Unless the provider has written an order to admit you as an inpatient to the hospital, you are an outpatient and pay the cost-sharing amounts for outpatient hospital services. Even if you stay in the hospital overnight, you might still be considered an "outpatient." If you are not sure if you are an outpatient, you should ask the hospital staff.
You can also find more information in a Medicare fact sheet called "Are You a Hospital Inpatient or Outpatient? If You Have Medicare – Ask!" This fact sheet is available on the Web at https://www.medicare.gov/sites/default/files/2018-09/11435-Are-You-an-Inpatient-or-Outpatient.pdf or by calling 1-800-MEDICARE (1-800-633-4227). TTY users call 1-877-486-2048. You can call these numbers for free, 24 hours a day, 7 days a week.
$50 per stay when admitted directly to the hospital for observation as an outpatient.
Note: There's no additional charge for outpatient observation stays when transferred from an Emergency Department or outpatient surgery.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
18
Services that are covered for you What you must pay when you get these services
Outpatient hospital services† We cover medically necessary services you get in the outpatient department of a hospital for diagnosis or treatment of an illness or injury.
Covered services include, but are not limited to:
• Services in an Emergency Department or outpatient clinic, such as observation services or outpatient surgery. Note: Refer to the "Outpatient hospital observation" section of this Medical Benefits Chart for the cost-sharing applicable to observation services.
$50 per Emergency Department visit. $50 per outpatient surgery visit or outpatient procedure.
• Laboratory and diagnostic tests billed by the hospital. No charge for lab tests. No charge for diagnostic tests such as electrocardiograms.
• Mental health care, including care in a partial-hospitalization program, if a doctor certifies that inpatient treatment would be required without it.
$30 per day in partial hospitalization program.
• X-rays and other radiology services billed by the hospital. No charge per visit, per department for X-rays and ultrasounds.
No charge for radiation therapy. No charge per visit, per department for specialty scans, such as MRI, CT, PET scans.
• Medical supplies such as splints and casts. No charge for splints and casts. No charge for take home dressings and supplies.
• Certain drugs and biologicals that you can't give yourself. No charge.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
19
Services that are covered for you What you must pay when you get these services
Note: Unless the provider has written an order to admit you as an inpatient to the hospital, you are an outpatient and pay the cost-sharing amounts for outpatient hospital services. Even if you stay in the hospital overnight, you might still be considered an "outpatient." If you are not sure if you are an outpatient, you should ask the hospital staff. You can also find more information in a Medicare fact sheet called "Are You a Hospital Inpatient or Outpatient? If You Have Medicare – Ask!" This fact sheet is available on the Web at https://www.medicare.gov/sites/default/files/2018-09/11435-Are-You-an-Inpatient-or-Outpatient.pdf or by calling 1-800-MEDICARE (1-800-633-4227). TTY users call 1-877-486-2048. You can call these numbers for free, 24 hours a day, 7 days a week.
Outpatient mental health care† Covered services include:
• Mental health services provided by a state-licensed psychiatrist or doctor, clinical psychologist, clinical social worker, clinical nurse specialist, nurse practitioner, physician assistant, or other Medicare-qualified mental health care professional as allowed under applicable state laws.
$30 per individual therapy visit. $15 per group therapy visit.
• Mental health day treatment. $30 per day.
Outpatient rehabilitation services† • Covered services include: physical therapy, occupational
therapy, and speech language therapy. Outpatient rehabilitation services are provided in various outpatient settings, such as hospital outpatient departments, independent therapist offices, and Comprehensive Outpatient Rehabilitation Facilities (CORFs).
$30 per visit (or per day at a comprehensive outpatient rehabilitation facility.
Outpatient substance abuse services† Covered services include:
• Intensive outpatient treatment program.
$30 per individual visit. $15 per group visit.
• Substance abuse day treatment services. $30 per day.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
20
Services that are covered for you What you must pay when you get these services
Outpatient surgery, including services provided at hospital outpatient facilities and ambulatory surgical centers† Note: If you are having surgery in a hospital facility, you should check with your provider about whether you will be an inpatient or outpatient. Unless the provider writes an order to admit you as an inpatient to the hospital, you are an outpatient and pay the cost-sharing amounts for outpatient surgery. Even if you stay in the hospital overnight, you might still be considered an outpatient.
$50 per visit.
Outside service area benefit If you travel outside our service area, but inside the United States or its territories, we cover preventive, routine, follow-up, or continuing care office visits obtained from out-of-network Medicare providers not to exceed $1,000 in covered plan charges per calendar year.
We will pay up to 80% of the Medicare allowable charge, if the provider accepts assignment. Otherwise, we will pay 80% of the Medicare limiting charge, if the provider does not accept assignment.
20% of the Medicare allowable or the limiting charges. Up to $1,000 maximum benefit per calendar year.
Partial hospitalization services† "Partial hospitalization" is a structured program of active psychiatric treatment, provided as a hospital outpatient service or by a community mental health center that is more intense than the care received in your doctor's or therapist's office and is an alternative to inpatient hospitalization. Note: Because there are no community mental health centers in our network, we cover partial hospitalization only as a hospital outpatient service.
$30 per day.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
21
Services that are covered for you What you must pay when you get these services
Physician/practitioner services, including doctor's office visits Covered services include:
• †Medically necessary medical care or surgery services furnished in a physician's office, certified ambulatory surgical center, hospital outpatient department, or any other location.
• †Consultation, diagnosis, and treatment by a specialist.
• †Second opinion by another network provider prior to surgery.
• Basic hearing and balance exams performed by a network provider, if your doctor orders it to see if you need medical treatment.
$30 per primary care visit. $30 per specialty care visit. $50 per visit for an outpatient surgery or procedure at an ambulatory surgery center or hospital outpatient department.
• †Nonroutine dental care (covered services are limited to surgery of the jaw or related structures, setting fractures of the jaw or facial bones, extraction of teeth to prepare the jaw for radiation treatments of neoplastic cancer disease, or services that would be covered when provided by a physician).
$30 per specialty care visit. $50 per visit for an outpatient surgery or procedure at an ambulatory surgery center or hospital outpatient department.
• †Pain management office visits. $30 per individual visit. $15 per group visit.
• Chemotherapy visits. No charge per visit.
• †Ultraviolet light treatments. $5 per visit.
• †Visits for injections administered in outpatient settings. No charge per injection.
• Certain telehealth services, including for: primary and specialty care, which includes cardiac and pulmonary rehabilitation, mental health care, substance abuse treatment, physical therapy, kidney disease, diabetes self-management, preparation for a hospital stay, and follow up visits after a hospital stay or Emergency Department visit. Services will only be provided via telehealth when deemed clinically
No charge.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
22
Services that are covered for you What you must pay when you get these services
appropriate by the network provider rendering the service. You have the option of receiving these services either through an in-person visit or via telehealth. If you choose to receive one of these services via telehealth, then you must use a network provider that currently offers the service via telehealth. We offer the following means of telehealth:
♦ Interactive video visits for professional services when care can be provided in this format as determined by a network provider.
♦ Scheduled telephone appointment visits for professional services when care can be provided in this format as determined by a network provider.
• Telehealth services for monthly ESRD-related visits for home dialysis members in a hospital-based or critical access hospital-based renal dialysis center, renal dialysis facility, or the member's home.
• Telehealth services for diagnosis, evaluation, or treatment of symptoms of an acute stroke.
• Brief virtual (for example, via telephone or video chat) 5- to 10-minute check-ins with your doctor, if you are an established patient and the virtual check-in is not related to an office visit within the previous 7 days, nor leads to an office visit within the next 24 hours or soonest available appointment.
• Remote evaluation of prerecorded video and/or images you send to your doctor, including your doctor's interpretation and follow-up within 24 hours (except weekends and holidays)—if you are an established patient and the remote evaluation is not related to an office visit within the previous 7 days, nor leads to an office visit within the next 24 hours or soonest available appointment.
• Consultation your doctor has with other physicians via telephone, internet, or electronic health record assessment—if you are an established patient.
Note: Cost-sharing is charged based on the medical department where the service is provided, not the type of provider. In addition, multiple copayments may apply, depending on services provided and/or whether a consultation occurs.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
23
Services that are covered for you What you must pay when you get these services
Podiatry services† Covered services include:
• Diagnosis and the medical or surgical treatment of injuries and diseases of the feet (such as hammer toe or heel spurs).
• Routine foot care for members with certain medical conditions affecting the lower limbs.
$30 per visit. $50 per outpatient surgery visit.
*Prescription drugs† (Not covered by Medicare, but covered by your group plan.)
$20 generic/$40 brand, for up to a 30-day supply, per prescription.
$40 generic/$80 brand for a 31- to 90- day supply from our Mail-Order Pharmacy.
No charge for formulary contraceptives.
(See the Outpatient Prescription Drug Rider in the EOC for additional information.)
Prostate cancer screening exams For men age 50 and older, covered services include the following once every 12 months:
• Digital rectal exam.
• Prostate Specific Antigen (PSA) test.
There is no coinsurance, copayment, or deductible for an annual digital rectal exam or PSA test.
Prosthetic devices and related supplies† Devices (other than dental) that replace all or part of a body part or function.
Covered items include, but are not limited to:
• Colostomy bags and supplies directly related to colostomy care, pacemakers, braces, prosthetic shoes, artificial limbs, and breast prostheses (including a surgical brassiere after a mastectomy).
• Certain supplies related to prosthetic devices, and repair and/or replacement of prosthetic devices.
No charge for external prosthetic or orthotic devices and supplies, including wound care supplies.
No charge for surgically implanted internal devices and enteral and parenteral nutrition therapy.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
24
Services that are covered for you What you must pay when you get these services
• Wigs following chemotherapy or radiation therapy (up to $100 benefit maximum per lifetime).
• Some coverage following cataract removal or cataract surgery (see "Vision care" later in this section for more detail).
Pulmonary rehabilitation services† Comprehensive programs for pulmonary rehabilitation are covered for members who have moderate to very severe chronic obstructive pulmonary disease (COPD) and an order for pulmonary rehabilitation from the doctor treating the chronic respiratory disease.
$30 per day.
Residential treatment for mental health and substance abuse† There is no limit to the number of medically necessary days in our residential treatment program to treat mental health conditions and substance abuse when prescribed by a network provider. Covered services include the following:
• Nursing care. • Room and meals. • Services by counselors and licensed therapists, such as
assessments, care plans, and therapy. • Group, family, and individual counseling. • Occupational therapy. • Discharge planning.
$250 per admission. Cost-sharing is charged per admission to a residential treatment program.
Screening and counseling to reduce alcohol misuse We cover one alcohol misuse screening for adults with Medicare (including pregnant women) who misuse alcohol, but aren't alcohol dependent.
If you screen positive for alcohol misuse, you can get up to four brief face-to-face counseling sessions per year (if you're competent and alert during counseling) provided by a qualified primary care doctor or practitioner in a primary care setting.
There is no coinsurance, copayment, or deductible for the Medicare-covered screening and counseling to reduce alcohol misuse preventive benefit.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
25
Services that are covered for you What you must pay when you get these services
Screening for lung cancer with low-dose computed tomography (LDCT)† For qualified individuals, a LDCT is covered every 12 months. • Eligible members are people aged 55–77 years who have no
signs or symptoms of lung cancer, but who have a history of tobacco smoking of at least 30 pack-years and who currently smoke or have quit smoking within the last 15 years, who receive a written order for LDCT during a lung cancer screening counseling and shared decision-making visit that meets the Medicare criteria for such visits and be furnished by a physician or qualified non-physician practitioner.
• For LDCT lung cancer screenings after the initial LDCT screening, the member must receive a written order for LDCT lung cancer screening, which may be furnished during any appropriate visit with a physician or qualified non-physician practitioner. If a physician or qualified non-physician practitioner elects to provide a lung cancer screening counseling and shared decision-making visit for subsequent lung cancer screenings with LDCT, the visit must meet the Medicare criteria for such visits.
There is no coinsurance, copayment, or deductible for the Medicare-covered counseling and shared decision-making visit or for the LDCT.
Screening for sexually transmitted infections (STIs) and counseling to prevent STIs We cover sexually transmitted infection (STI) screenings for chlamydia, gonorrhea, syphilis, and Hepatitis B. These screenings are covered for pregnant women and for certain people who are at increased risk for an STI when the tests are ordered by a primary care provider. We cover these tests once every 12 months or at certain times during pregnancy.
We also cover up to two individual 20- to 30-minute, face-to-face high-intensity behavioral counseling sessions each year for sexually active adults at increased risk for STIs. We will only cover these counseling sessions as a preventive service if they are provided by a primary care provider and take place in a primary care setting, such as a doctor's office.
There is no coinsurance, copayment, or deductible for the Medicare-covered screening for STIs and counseling for STIs preventive benefit.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
26
Services that are covered for you What you must pay when you get these services
Services to treat kidney disease Covered services include:
• Kidney disease education services to teach kidney care and help members make informed decisions about their care.
No charge.
• †Outpatient dialysis treatments (including dialysis treatments when temporarily out of the service area, as explained in Chapter 3).
• †Self-dialysis training (includes training for you and anyone helping you with your home dialysis treatments).
• †Home dialysis equipment and supplies.
• †Certain home support services (such as, when necessary, visits by trained dialysis workers to check on your home dialysis, to help in emergencies, and to check your dialysis equipment and water supply).
No charge.
• †Inpatient dialysis treatments (if you are admitted as an inpatient to a hospital for special care).
No additional charge for services received during a hospital stay. Refer to the "Inpatient hospital care" section of this Medical Benefits Chart for the cost-sharing applicable to inpatient stays.
Certain drugs for dialysis are covered under your Medicare Part B drug benefit. For information about coverage for Part B drugs, please go to the section called "Medicare Part B prescription drugs."
Skilled nursing facility (SNF) care† (For a definition of "skilled nursing facility care," see Chapter 10 of this booklet. Skilled nursing facilities are sometimes called "SNFs.")
We cover up to 150 days per benefit period of skilled inpatient services in a skilled nursing facility in accord with Medicare guidelines (a prior hospital stay is not required). Covered services include, but are not limited to:
• Semiprivate room (or a private room if medically necessary).
• Meals, including special diets.
No charge.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
27
Services that are covered for you What you must pay when you get these services
• Skilled nursing services.
• Physical therapy, occupational therapy, and speech therapy.
• Drugs administered to you as part of your plan of care (this includes substances that are naturally present in the body, such as blood clotting factors).
• Blood—including storage and administration.
• Medical and surgical supplies ordinarily provided by SNFs.
• Laboratory tests ordinarily provided by SNFs.
• X-rays and other radiology services ordinarily provided by SNFs.
• Use of appliances such as wheelchairs ordinarily provided by SNFs.
• Physician/practitioner services. Generally, you will get your SNF care from network facilities. However, under certain conditions listed below, you may be able to pay in-network cost-sharing for a facility that isn't a network provider, if the facility accepts our plan's amounts for payment.
• A nursing home or continuing care retirement community where you were living right before you went to the hospital (as long as it provides skilled nursing facility care).
• A SNF where your spouse is living at the time you leave the hospital.
Smoking and tobacco use cessation (counseling to stop smoking or tobacco use) If you use tobacco, but do not have signs or symptoms of tobacco-related disease: We cover two counseling quit attempts within a 12-month period as a preventive service with no cost to you. Each counseling attempt includes up to four face-to-face visits.
If you use tobacco and have been diagnosed with a tobacco-related disease or are taking medicine that may be affected by tobacco: We cover cessation counseling services. We cover two counseling quit
There is no coinsurance, copayment, or deductible for the Medicare-covered smoking and tobacco use cessation preventive benefits.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
28
Services that are covered for you What you must pay when you get these services
attempts within a 12-month period; however, you will pay the applicable cost-sharing. Each counseling attempt includes up to four face-to-face visits.
Supervised Exercise Therapy (SET) SET is covered for members who have symptomatic peripheral artery disease (PAD) and a referral for PAD from the physician responsible for PAD treatment.
Up to 36 sessions over a 12-week period are covered if the SET program requirements are met.
The SET program must: • Consist of sessions lasting 30–60 minutes, comprising a
therapeutic exercise-training program for PAD in patients with claudication.
• Be conducted in a hospital outpatient setting or a physician's office.
• Be delivered by qualified auxiliary personnel necessary to ensure benefits exceed harms, and who are trained in exercise therapy for PAD.
• Be under the direct supervision of a physician, physician assistant, or nurse practitioner/clinical nurse specialist who must be trained in both basic and advanced life support techniques.
Note: SET may be covered beyond 36 sessions over 12 weeks for an additional 36 sessions over an extended period of time, if deemed medically necessary by a health care provider.
$30 per visit.
Urgently needed services Urgently needed services are provided to treat a nonemergency, unforeseen medical illness, injury, or condition that requires immediate medical care. Urgently needed services may be furnished by network providers or by out-of-network providers when network providers are temporarily unavailable or inaccessible.
• Inside our service area: You must obtain urgent care from network providers, unless our provider network is temporarily unavailable or inaccessible due to an unusual
$35 per provider office visit. $50 per Emergency Department visit.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
29
Services that are covered for you What you must pay when you get these services
and extraordinary circumstance (for example, major disaster).
• Outside our service area: You have worldwide urgent care coverage when you travel if you need medical attention right away for an unforeseen illness or injury and you reasonably believed that your health would seriously deteriorate if you delayed treatment until you returned to our service area.
Cost-sharing for necessary urgently needed services furnished out-of-network is the same as for such services furnished in-network.
See Chapter 3, Section 3, for more information.
Vision care Covered services include:
• Outpatient physician services for the diagnosis and treatment of diseases and injuries of the eye, including treatment for age-related macular degeneration.
$30 per visit.
• Original Medicare doesn't cover routine eye exams (eye refractions) for eyeglasses/contacts. However, our plan does cover the following exams: ♦ Routine eye exams (eye refraction exams) to determine
the need for vision correction and to provide a prescription for eyeglass lenses.
• Visual field tests.
$30 per visit.
• For people who are at high risk of glaucoma, we will cover one glaucoma screening each year. People at high risk of glaucoma include: people with a family history of glaucoma, people with diabetes, African-Americans who are age 50 and older, and Hispanic Americans who are 65 or older.
• For people with diabetes, screening for diabetic retinopathy is covered once per year.
No charge.
-
† Your provider must obtain prior authorization from our plan. * Your cost-sharing for these services or items doesn't apply toward the maximum out-of-pocket amount.
30
Services that are covered for you What you must pay when you get these services
• One pair of eyeglasses or one conventional contact lens or up to a 6-month supply of disposable contact lenses after each cataract surgery that includes insertion of an intraocular lens. (If you have two separate cataract operations, you can reserve the benefit after the first surgery and purchase two eyeglasses after the second surgery.)
• Corrective lenses/frames (and replacements) needed after a cataract removal without a lens implant.
No charge for eyewear in accord with Medicare guidelines.
Note: If the eyewear you purchase costs more than what Medicare covers, you pay the difference.
• *Prescription eyewear (eyeglass lenses, eyeglass frames, and contact lenses).
Balance after $150 eyewear allowance to use toward the purchase price of eyewear once within a two-calendar-year period.
(See the Prescription Eyewear Rider in the EOC for additional information.)
"Welcome to Medicare" preventive visit We cover the one-time "Welcome to Medicare" preventive visit. The visit includes a review of your health, as well as education and counseling about the preventive services you need (including certain screenings and shots), and referrals for other care if needed.
Important: We cover the "Welcome to Medicare" preventive visit only within the first 12 months you have Medicare Part B. When you make your appointment, let your doctor's office know you would like to schedule your "Welcome to Medicare" preventive visit.
There is no coinsurance, copayment, or deductible for the "Welcome to Medicare" preventive visit.
Note: Refer to Chapter 1 (Section 7) and Chapter 9 (Section 10) for information about coordination of benefits that applies to all covered services described in this Medical Benefits Chart.
-
WAPEBBEC0120
January 1 – December 31, 2020
Evidence of Coverage Your Medicare H ealth Benefits and Services a s a Member of K aiser Permanente Senior Advantage Group Plan (HMO) for Medicare Eligible Washington PEBB Employees
This booklet gives you the details about your Medicare health care coverage from January 1 to December 31, 2020. It explains how to get coverage for the health care services you need. This is an important legal document. Please keep it in a safe place.
This plan, Kaiser Permanente Senior Advantage, is offered by Kaiser Foundation Health Plan of the Northwest (Health Plan). When this Evidence of Coverage says "we," "us," or "our," it means Health Plan. When it says "plan" or "our plan," it means Kaiser Permanente Senior Advantage (Senior Advantage).
This document is available in large print if you need it by calling Member Services (phone numbers are printed on the back cover of this booklet).
Benefits, premium, deductible, and/or copayments/coinsurance may change on January 1, 2021. The provider network may change at any time. You will receive notice when necessary.
-
1-877-221-8221 (TTY 711), 7 days a week, 8 a.m. to 8 p.m.
2020 Evidence of Coverage for WA PEBB Senior Advantage Table of Contents
2020 Evidence of Coverage
Table of Contents
This list of chapters and page numbers is your starting point. For more help in finding information you need, go to the first page of a chapter. You will find a detailed list of topics at the beginning of each chapter.
CHAPTER 1. Getting started as a member................................................................. 1
Explains what it means to be in a Medicare health plan and how to use this booklet. Tells about materials we will send you, your plan premium, your plan membership card, and keeping your membership record up-todate.
CHAPTER 2. Important phone numbers and resources ......................................... 24
Tells you how to get in touch with our plan (Senior Advantage) and with other organizations including Medicare, the State Health Insurance Assistance Program (SHIP), the Quality Improvement Organization, Social Security, Medicaid (the state health insurance program for people with low incomes), and the Railroad Retirement Board.
CHAPTER 3. Using our plan's coverage for your medical services ...................... 34
Explains important things you need to know about getting your medical care as a member of our plan. Topics include using the providers in our plan's network and how to get care when you have an emergency.
CHAPTER 4. Medical Benefits Chart (what is covered and what you pay) ........... 49
Gives the details about which types of medical care are covered and not covered for you as a member of our plan. Explains how much you will pay as your share of the cost for your covered medical care.
CHAPTER 5. Asking us to pay our share of a bill you have received for covered medical services.................................................................... 62
Explains when and how to send a bill to us when you want to ask us to pay you back for our share of the cost for your covered services.
CHAPTER 6. Your rights and responsibilities ......................................................... 67
Explains the rights and responsibilities you have as a member of our plan. Tells what you can do if you think your rights are not being respected.
-
kp.org
2020 Evidence of Coverage for WA PEBB Senior Advantage Table of Contents
CHAPTER 7. What to do if you have a problem or complaint (coverage decisions, appeals, and complaints) .................................................. 76
Tells you step-by-step what to do if you are having problems or concerns as a member of our plan.
• Explains how to ask for coverage decisions and make appeals if you are having trouble getting the medical care you think is covered by our plan. This includes asking us to keep covering hospital care and certain types of medical services if you think your coverage is ending too soon.
• Explains how to make complaints about quality of care, waiting times, customer service, and other concerns.
CHAPTER 8. Ending your membership in our plan................................................ 112
Explains when and how you can end your membership in our plan. Explains situations in which our plan is required to end your membership.
CHAPTER 9. Legal notices ....................................................................................... 117
Includes notices about governing law and about nondiscrimination.
CHAPTER 10. Definitions of important words ........................................................ 123
Explains key terms used in this booklet.
-
1
2020 Evidence of Coverage for WA PEBB Senior Advantage Chapter 1: Getting started as a member
1-877-221-8221 (TTY 711), 7 days a week, 8 a.m. to 8 p.m.
CHAPTER 1. Getting started as a member
SECTION 1. Introduction ............................................................................................. 2
Section 1.1 You are enrolled in Senior Advantage, which is a Medicare HMO........................ 2
Section 1.2 What is the Evidence of Coverage booklet about? ................................................. 2
Section 1.3 Term of the Evidence of Coverage ......................................................................... 2
SECTION 2. What makes you eligible to be a plan member? ................................... 3
Section 2.1 Your Senior Advantage eligibility requirements .................................................... 3
Section 2.2 What are Medicare Part A and Medicare Part B? ................................................... 3
Section 2.3 Here is our plan service area for Senior Advantage ................................................ 4
Section 2.4 Group eligibility requirements ................................................................................ 4
Section 2.5 When you can enroll and when coverage begins .................................................... 7
Section 2.6 U.S. citizen or lawful presence .............................................................................. 18
SECTION 3. What other materials will you get from us? ........................................ 18
Section 3.1 Your plan membership card—use it to get all covered care ................................. 18
Section 3.2 The Provider Directory: Your guide to all providers in our network .................... 19
SECTION 4. Premiums ............................................................................................... 20
Section 4.1 Plan and Medicare premiums ................................................................................ 20
SECTION 5. Please keep your plan membership record up-to-date ...................... 21
Section 5.1 How to help make sure that we have accurate information about you.................. 21
SECTION 6. We protect the privacy of your personal health information ............. 22
Section 6.1 We make sure that your health information is protected ...................................... 22
SECTION 7. How other insurance works with our plan .......................................... 22
Section 7.1 Which plan pays first when you have other insurance? ........................................ 22
-
kp.org
2 2020 Evidence of Coverage for WA PEBB Senior Advantage
Chapter 1: Getting started as a member
SECTION 1. Introduction
Section 1.1 You are enrolled in Senior Advantage, which is a Medicare HMO
You are covered by Medicare, and you have chosen to get your Medicare health care coverage through our plan, Kaiser Permanente Senior Advantage.
There are different types of Medicare health plans. Senior Advantage is a Medicare Advantage HMO Plan (HMO stands for Health Maintenance Organization) approved by Medicare and run by a private company.
Coverage under this plan qualifies as Qualifying Health Coverage (QHC) and satisfies the Patient Protection and Affordable Care Act's (ACA) individual shared responsibility requirement. Please visit the Internal Revenue Service (IRS) website at https://www.irs.gov/Affordable-Care-Act/Individuals-and-Families for more information.
Section 1.2 What is the Evidence of Coverage booklet about?
This Evidence of Coverage (EOC) booklet tells you how to get your Medicare medical care covered through our plan. This booklet explains your rights and responsibilities, what is covered, and what you pay as a member of our plan.
If you are not certain which plan you are enrolled in, please call Member Services or your group's benefits administrator.
The words "coverage" and "covered services" refer to the medical care and services available to you as a member of our plan.
It's important for you to learn what our plan's rules are and what services are available to you. We encourage you to set aside some time to look through this Evidence of Coverage booklet. If you are confused or concerned or just have a question, please contact Member Services (phone numbers are printed on the back cover of this booklet).
Section 1.3 Term of the Evidence of Coverage
This Evidence of Coverage explains what our plan covers, in addition to your enrollment form, and any notices you receive from us about changes to your coverage or conditions that affect your coverage. These notices are sometimes called "riders" or "amendments."
If your group renews on January 1, the Evidence of Coverage is in effect for the months in which you are enrolled in Senior Advantage between January 1, 2020, and December 31, 2020, unless amended.
If your group's Agreement renews at a later date in 2020, the term of this Evidence of Coverage is during that contract period, unless amended.
https://www.irs.gov/Affordable-Care-Act/Individuals-and-Families
-
1-877-221-8221 (TTY 711), 7 days a week, 8 a.m. to 8 p.m.
3 2020 Evidence of Coverage for WA PEBB Senior Advantage Chapter 1: Getting started as a member
Your group can tell you the term of this Evidence of Coverage and whether this Evidence of Coverage is still in effect, and give you a current one if this Evidence of Coverage has been amended.
Medicare must approve our plan each year Medicare (the Centers for Medicare & Medicaid Services) must approve our plan each year. You can continue to get Medicare coverage as a member of our plan only as long as your group continues to offer this plan, we choose to continue to offer our plan, and Medicare renews its approval of our plan.
SECTION 2. What makes you eligible to be a plan member?
Section 2.1 Your Senior Advantage eligibility requirements
You are eligible for membership in our plan as long as:
• You have both Medicare Part A and Medicare Part B (Section 2.2 below tells you about Medicare Part A and Medicare Part B).
• – and – you live in our geographic service area (Section 2.3 below describes our service area). If you have been a member of our plan continuously since before January 1999 and you were living outside of our service area before January 1999, you are still eligible as long as you have not moved since before January 1999.
• – and – you are a United States citizen or are lawfully present in the United States. • – and – you do not have End-Stage Renal Disease (ESRD), with limited exceptions, such as if
you develop ESRD when you are already a member of a plan that we offer, or you were a member of a different plan that was terminated.
Note: If you are enrolled in a Medicare plan and lose Medicare eligibility, you may be able to enroll under your group's non-Medicare plan if that is permitted by your group (please ask your group for details).
Section 2.2 What are Medicare Part A and Medicare Part B?
When you first signed up for Medicare, you received information about what services are covered under Medicare Part A and Medicare Part B. Remember:
• Medicare Part A generally helps cover services provided by hospitals (for inpatient services), skilled nursing facilities, or home health agencies.
• Medicare Part B is for most other medical services (such as physician's services and other outpatient services) and certain items (such as durable medical equipment (DME) and supplies).
-
kp.org
4 2020 Evidence of Coverage for WA PEBB Senior Advantage
Chapter 1: Getting started as a member
Section 2.3 Here is our plan service area for Senior Advantage
Although Medicare is a federal program, our plan is available only to individuals who live in our plan service area. To remain a member of our plan, you must continue to reside in the plan service area. The service area is described below.
• Our service area includes these counties in Oregon: Clackamas, Columbia, Hood River, Marion, Multnomah, Polk, Washington, and Yamhill. Also, our service area includes these parts of counties in Oregon, in the following ZIP codes only: ♦ Benton: 97330, 97331, 97333, 97339, 97370. ♦ Linn: 97321, 97322, 97335, 97355, 97358, 97360, 97374, 97389.
• Our service area includes Clark, Cowlitz, and Skamania counties in Washington. Also, our service area includes parts of Wahkiakum County in Washington, in the following ZIP codes only: 98612, 98647.
If you plan to move out of the service area, please contact Member Services (phone numbers are printed on the back cover of this booklet). Active employees also need to contact their personnel, payroll, or benefits office. Retirees, COBRA, and LWOP members also need to contact the PEBB Program.
It is also important that you call Social Security if you move or change your mailing address. You can find phone numbers and contact information for Social Security in Chapter 2, Section 5.
Section 2.4 Group eligibility requirements
Medical plan eligibility and enrollment for a retiree or survivor In these sections, we use the term "subscriber" to refer to a retiree or survivor. The term "enrollee" refers to a subscriber and their dependents. The term "retiree" or "retiring employee" includes an elected or full-time appointed official of the legislative and executive branch of state government eligible to continue enrollment in Public Employees Benefits Board (PEBB) retiree insurance coverage. The term "retiree" or "retiring school employee" includes a retiring non-represented employee of an educational service district (ESD) or retiring school employee from a School Employees Benefits Board (SEBB) organization. Additionally, "health plan" is used to refer to a plan offering medical or dental, or both, developed by PEBB and provided by a contracted vendor or self-insured plans administered by the Health Care Authority (HCA).
Eligibility The PEBB Program determines if a retiring employee or retiring school employee is eligible to enroll in PEBB retiree insurance coverage upon receipt of a completed PEBB Retiree Coverage Election Form. If the retiring employee or retiring school employee does not have substantive eligibility or does not meet the procedural requirements for enrollment in PEBB retiree insurance coverage, the PEBB Program will notify them of their right to an appeal. Information about appealing a PEBB Program decision can be found in Section 2.5 of this chapter under "Appeal rights." For information on how to enroll, see "Enrollment" in Section 2.5.
-
1-877-221-8221 (TTY 711), 7 days a week, 8 a.m. to 8 p.m.
5 2020 Evidence of Coverage for WA PEBB Senior Advantage Chapter 1: Getting started as a member
The PEBB Program determines if a dependent is eligible to enroll or continue enrollment in PEBB retiree insurance coverage as a survivor upon receipt of a completed PEBB Retiree Coverage Election Form. If the survivor does not meet the eligibility and procedural requirements for enrollment in PEBB retiree insurance coverage, the PEBB Program will notify them of their right to an appeal. Information about appealing a PEBB Program decision can be found in Section 2.5 of this chapter under "Appeal rights." For information on how to enroll, see "Enrollment" in Section 2.5.
A retiree, a survivor, and their enrolled dependents are required to enroll in Medicare Part A and Part B if they are entitled. Any enrollee who is entitled to Medicare must enroll and stay enrolled in Medicare Part A and Part B to enroll or continue enrollment in a PEBB retiree health plan. A subscriber must provide a copy of their or their dependent’s Medicare card or entitlement letter from the Social Security Administration with Medicare Part A and Part B effective dates to the PEBB Program as proof of Medicare enrollment. If a subscriber or their dependent is not entitled to either Medicare Part A or Part B on their 65th birthday, a copy of the denial letter from the Social Security Administration must be provided to the PEBB Program. The only exception to this rule is for an employee or school employee who retired on or before July 1, 1991.
To enroll an eligible dependent the subscriber must follow the procedural requirements described in Section 2.5 of this chapter under "Enrollment." The PEBB Program verifies the eligibility of all dependents and requires the subscriber to provide documents that prove a dependent’s eligibility.
The following are eligible as dependents: 1. Legal spouse.
2. State-registered domestic partner as defined in state statute and substantially equivalent legal unions from other jurisdictions as defined in Washington state statute.
3. Children. Children are eligible through the last day of the month in which their 26th birthday occurs except as described in subsection (g) of this section. Children are defined as the subscriber's:
a. Children as defined in state statutes that establish a parent-child relationship, except when parental rights have been terminated;
b. Children of the subscriber’s spouse, based on the spouse’s establishment of a parent-child relationship, except when parental rights have been terminated. The stepchild’s relationship to the subscriber (and eligibility as a dependent) ends on the same date the marriage with the spouse ends through divorce, annulment, dissolution, termination, or death;
c. Children for whom the subscriber has assumed a legal obligation for total or partial support in anticipation of adoption of the child;
d. Children of the subscriber’s state-registered domestic partner, based on the state-registered domestic partner’s establishment of a parent-child relationship, except when parental rights have been terminated. The child’s relationship to the subscriber (and eligibility as a dependent) ends on the same date the subscriber’s legal relationship with
-
kp.org
6 2020 Evidence of Coverage for WA PEBB Senior Advantage
Chapter 1: Getting started as a member
the state-registered domestic partner ends through divorce, annulment, dissolution, termination, or death;
e. Children specified in a court order or divorce decree for whom the subscriber has a legal obligation to provide support or health care coverage;
f. Extended dependent in the legal custody or legal guardianship of the subscriber, the subscriber’s spouse, or subscriber’s state-registered domestic partner. The legal responsibility is demonstrated by a valid court order and the child’s official residence with the custodian or guardian. Extended dependent child does not include a foster child unless the subscriber, the subscriber’s spouse, or the subscriber’s state-registered domestic partner has assumed a legal obligation for total or partial support in anticipation of adoption; and
g. Children of any age with a developmental or physical disability that renders the child incapable of self-sustaining employment and chiefly dependent upon the subscriber for support and maintenance provided such condition occurs before the age of 26. The following requirements apply to a dependent child with a disability:
• The subscriber must provide proof of the disability and dependency within 60 days of the child’s attainment of age 26;
• The subscriber must notify the PEBB Program, in writing, within 60 days of the last day of the month the child is no longer eligible under this subsection;
• A child with a developmental or physical disability who becomes self-supporting is not eligible as of the last day of the month in which they become capable of self-support;
• A child with a developmental or physical disability age 26 and older who becomes capable of self-support does not regain eligibility under this subsection if they later become incapable of self-support; and
• The PEBB Program with input from the medical plan will periodically verify the eligibility of a dependent child with a disability, but no more frequently than annually after the two-year period following the child’s 26th birthday, which may require renewed proof from the subscriber.
4. Parents of the subscriber.
a. Parents covered under PEBB medical before July 1, 1990, may continue enrollment on a self-pay basis as long as:
• The parent maintains continuous enrollment in PEBB medical;
• The parent qualifies under the Internal Revenue Code as a dependent of the subscriber;
• The subscriber continues enrollment in PEBB insurance coverage; and
• The parent is not covered by any other group medical plan.
b. Parents eligible under this subsection may be enrolled with a different medical plan than that selected by the subscriber. Parents may not enroll additional dependents to their PEBB insurance coverage.
-
1-877-221-8221 (TTY 711), 7 days a week, 8 a.m. to 8 p.m.
7 2020 Evidence of Coverage for WA PEBB Senior Advantage Chapter 1: Getting started as a member
Section 2.5 When you can enroll and when coverage begins
Enrollment Deferring enrollment in a PEBB retiree health plan A retiring employee, a retiring school employee, and a dependent becoming eligible as a survivor who want to defer enrollment in a PEBB retiree health plan must submit a PEBB Retiree Coverage Election Form to the PEBB Program within the PEBB Program’s enrollment timelines. Deferring enrollment will also defer enrollment for all eligible dependents, except as described below. A retiring employee, a retiring school employee, and a dependent becoming eligible as a survivor who do not enroll in a PEBB retiree health plan are only eligible to enroll later if they have deferred enrollment as identified below:
• Beginning January 1, 2001, enrollment in a PEBB health plan may be deferred when the subscriber is enrolled in employer-based group medical insurance as an employee or the dependent of an employee, or such medical insurance continued under Consolidated Omnibus Budget Reconciliation Act (COBRA) coverage or continuation coverage.
• Beginning January 1, 2001, enrollment in a PEBB health plan may be deferred when the subscriber is enrolled as a retiree or the dependent of a retiree in a federal retiree medical plan.
• Beginning January 1, 2006, enrollment in a PEBB health plan may be deferred when the subscriber is enrolled in Medicare Parts A and B and a Medicaid program that includes payment of medical and hospital benefits. Eligible dependents who are not enrolled in Medicaid coverage that includes payment of medical and hospital benefits may be enrolled.
• Beginning January 1, 2014, subscribers who are not eligible for Part A and Part B of Medicare may defer enrollment in a PEBB health plan when the subscriber is enrolled in coverage through a health care exchange developed under the Affordable Care Act.
• Beginning July 17, 2018, enrollment in a PEBB health p






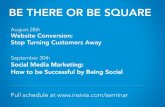







![Four Questions Your Prospects Can't Help-But Answer [+ Cheat Sheet]](https://static.fdocuments.us/doc/165x107/546dfec2b4af9f612c8b5523/four-questions-your-prospects-cant-help-but-answer-cheat-sheet.jpg)


