WALES BOWEL CANCER AUDIT REPORT FOR PATIENTS … Bowel... · Cancer National Specialist Advisory...
Transcript of WALES BOWEL CANCER AUDIT REPORT FOR PATIENTS … Bowel... · Cancer National Specialist Advisory...

Cancer National Specialist Advisory Group WALES BOWEL CANCER AUDIT REPORT FOR PATIENTS DIAGNOSED APRIL 2009-MARCH 2010 and AUGUST 2010-JULY 2011 Published 2013

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
2
FOREWORD
I am delighted to introduce the 2009-2011 Wales Bowel Cancer Audit Report. This document
includes data on over 4000 patients treated by the 13 Multidisciplinary teams (MDTs) in
Wales. It is gratifying that the quality of data captured has continued to improve, making the
exercise useful and meaningful. As the Cancer National Specialist Advisory Group (NSAG)
colorectal quality indicators have been met by MDTs in all but a few cases, we will look at
introducing new indicators in time for the next audit that will focus in on the clinical priorities
for colorectal cancer services in NHS Wales and complement the findings of the UK National
Bowel Cancer Audit.
The 30 day mortality rate after surgery has continued to fall. However, emergency surgery is
still required in 20% of operated patients in Wales and is associated with a far higher risk of
post-operative death. Over 20% of patients presented with metastatic disease. It is hoped
that the Bowel Cancer Screening Programme will alter these figures in the next few years.
There has been a general increase in the use of laparoscopic surgery, whilst there is still
room for improvement in the uptake rates in some units, the figures are encouraging and are
testament to the formalised laparoscopic training and mentorship that has been supported
by the Welsh Government (WG) and provided at the Welsh Institute for Minimal Access
Therapy in recent years.
The audit shows variation in the management of rectal cancer across Wales. Specifically,
there are differences in the use of radiotherapy, the rates of permanent colostomy and
complete surgical removal. The Colorectal Cancer (NSAG) will be considering these issues
with a view to supporting a multidisciplinary training programme similar to the Department of
Health’s Low Rectal Cancer National Development Programme (LOREC).
I am extremely grateful to the MDT co-ordinators and their clinical teams for the quality of
their data returns and also Linda Roberts, Rebecca Thomas, Julie Howe for expert data
analysis that has been guided by our clinical audit leads, Martyn Evans and Gethin Williams.
Finally, I must thank Louise Carrington and Jane Hanson of the Cancer NSAG Core Team
for their efforts in coordinating and editing the final report.
Mark Davies (Chair Cancer NSAG Colorectal Group)

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
3
Acknowledgments
This audit report was prepared on behalf of the Cancer National Specialist Advisory Group
(NSAG) Colorectal subgroup by:
• Martyn Evans, Consultant Colorectal Surgeon, Singleton and Morriston Hospital,
Swansea, Abertawe Bro Morgannwg University Health Board (ABMUHB)
• Gethin Williams, Consultant Colorectal Surgeon, Royal Gwent Hospital, Newport,
Aneurin Bevan Health Board (ABHB)
• Rebecca Thomas, Senior Statistician, Welsh Cancer Intelligence and Surveillance Unit
(WCISU)
• Julie Howe, Statistical Analyst, WCISU
• Linda Roberts, Canisc Information Specialist for Colorectal Cancer, Cancer Information
Framework (CIF)
• Louise Carrington, Programme Coordinator, Cancer NSAG Core Team.
Advice and comments were gratefully received from:
• Hayley Heard, Head of Bowel Cancer Screening Programme, Public Health
Wales
• Andrew Maw, Consultant Colorectal Surgeon, Betsi Cadwaladr University
Health Board (BCUHB), Lead for Colorectal Cancer North Wales
• Jane Hanson, Head of the Cancer NSAG Core Team
• Mark Davies, Consultant Surgeon, ABMUHB, Chair of the Colorectal subgroup
of the Cancer NSAG
• Jared Torkington, Consultant Colorectal Surgeon, Cardiff and Vale LHB
(C&VUHB), and Lead of Welsh Laparoscopic Colorectal Training Scheme
• Jeff Stamatakis, Retired consultant General Surgeon, former clinical audit lead
for colorectal cancer (Wales) and former chair of the National Bowel Cancer
Audit Project (NBOCAP).
Thanks should also go to all MDTs, including data and administration staff, without whose
work this report would not have been possible.
Contacts Queries concerning this report should be directed in the first instance to the Cancer NSAG
Core team at [email protected]

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
4
Contents FOREWORD ........................................................................................................................ 2
Acknowledgments ............................................................................................................. 3
Contacts................................................................................................................................ 3
Executive summary ............................................................................................................... 5
Recommendations............................................................................................................. 7
Introduction ......................................................................................................................... 10
Data collection .................................................................................................................... 10
Data presentation ................................................................................................................ 11
Risk adjusted mortality – logistic regression .................................................................... 12
Funnel plots ..................................................................................................................... 13
Data quality ......................................................................................................................... 13
Case ascertainment ......................................................................................................... 14
Completeness of key fields .............................................................................................. 15
Number and distribution of newly diagnosed bowel cancers ............................................... 17
Procedures used in the surgical treatment of bowel cancer................................................. 18
Operation and resection rates ............................................................................................. 20
Stage of disease at presentation ......................................................................................... 23
Surgical urgency of operated patients ................................................................................. 26
Co-morbidity ....................................................................................................................... 29
30-day mortality following surgery for bowel cancer ............................................................ 30
Use of laparoscopic surgery in Wales ................................................................................. 32
Length of stay ..................................................................................................................... 35
Rectal cancer ...................................................................................................................... 38
Use of radiotherapy ......................................................................................................... 38
Circumferential margin involvement ................................................................................. 39
APER rates ..................................................................................................................... 42
Clinical outcomes ................................................................................................................ 43
Lymph node harvest ........................................................................................................ 43
Extra-mural vascular invasion .......................................................................................... 44
National Specialist Advisory Group Clinical Indicators......................................................... 46
Bowel screening .................................................................................................................. 48
Screening demographics ................................................................................................. 48
Surgical treatment ........................................................................................................... 50
Stage at presentation of screen detected cancers ........................................................... 51
Laparoscopic surgery for screen-detected cancers.......................................................... 53
Post operative mortality for screen detected cancers ....................................................... 55
APPENDIX 1: Data set used in NBOCAP/WBCA ................................................................ 56

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
5
APPENDIX 2: NCEPOD operative urgency classification .................................................... 56
APPENDIX 3: American Society of Anesthesiology Grading System .................................. 57
APPENDIX 4: Odds ratios for 30 day mortality following surgery calculated from the WBCA
risk adjustment model. ........................................................................................................ 58
APPENDIX 5: DATA ........................................................................................................... 59
APPENDIX 6: REFERENCES ............................................................................................. 72
Executive summary
This is the 6th audit report of colorectal cancer in Wales. It is based on clinical information
from patients diagnosed during 2 periods: 1st April 2009 – 31st March 2010 and 1st August
2010 - 31st July 2011. Only those treated by MDTs in Welsh Health Boards are included.
Audit data on this cohort of patients is also submitted to the NHS Information Centre for
inclusion in the National Bowel Cancer Audit Program (NBOCAP). Where possible we have
benchmarked against the NBOCAP report (published December 2012).
Data quality link to section The data quality has improved dramatically since the first Welsh audit in 2005. Case
ascertainment is currently 100%. Data completeness of the five variables used in the
calculation of risk adjusted postoperative mortality is at 100% for age, urgency of surgery,
operation type; 81% for Dukes’ stage and 96% for ASA grade. Central validation of data
revealed errors with stage and postoperative death reports. These were corrected prior to
carrying out statistical analysis.
Clinical profile of colorectal cancer in Wales link to section
• Just over 2000 people were diagnosed with colorectal cancer in each audit year.
• In 2009/10, 77% of colon cancer patients and 67% of rectal cancer patients
underwent a resection. In 2010/11 the figures were 75% for colonic resections and
56% for rectal cancer resections.
• Over 20% of patients present with metastatic disease.
• Emergency surgery represented one-fifth of all operations for colorectal cancer.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
6
Mortality rate link to section The overall 30 day mortality rate following surgery has fallen to its lowest level since the first
report ten years ago. Non-adjusted 30 day mortality following elective colorectal surgery in
both audit years was 3%. For emergency surgery the mortality rates were higher (16% in
2009/10 and 11% in 2010/11). For the first time this report provides a calculation for risk-
adjusted mortality results for individual hospitals based on 3 years of consecutive data.
Lymph nodes link to section Lymph node yield is held as a quality indicator for surgery and pathological assessment. The
number of lymph nodes examined in patients having major resection surgery has remained
static over the last three years. Over 60% of patient specimens achieve the national
standard agreed for accurate staging by reporting on 12 or more lymph nodes.
Laparoscopic surgery & length of stay link to section The proportion of elective/scheduled laparoscopic operations performed has increased to
46% in the audit period 2010/11. There is wide inter-unit variation, with implication that some
suitable patients in Wales are not being considered for laparoscopic surgery, contrary to best
practice guidelines (NICE TA1051). The all Wales median length of stay for all elective
colorectal surgery was 8 days in 2009/10 and 7 days in 2010/11. Many surgical teams in
Wales have adopted enhanced recovery protocols for their patients. In 2010/11 patients
having laparoscopic surgery had a median length of stay of 6 days.
Bowel screening link to section
• The audit results clearly confirm the benefits of bowel screening with a significant
increase in early curative stage diagnosis.
• The uptake has been 55% of the invited population over the audit period.
• There were 203 screen detected cancers in 2009/10 (10.1% of total cancers
diagnosed).
• There were 241 screen detected cancers in 2010/11 (11.9% of total cancers
diagnosed).

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
7
• In 2010/11, 7% of screen detected cancers were stage Dukes’ D, as opposed to 24%
in patients presenting with symptoms.
• 66% of screen detected cancers in 2010/11 were stage Dukes’ A or B against 27% in
symptomatic patients.
Rectal cancer link to section
• Nearly 600 cases of rectal cancer were diagnosed in 2010/11 representing 29% of all
bowel cancers diagnosed in Wales.
• There is a wide variation in the use of preoperative short and long course
radiotherapy.
• Overall circumferential margin involvement for the 2 audit periods for
elective/scheduled rectal cancer cases was 5.8% with a rate of 3% for anterior
resections and 11% for Abdomino-Perineal Excision of Rectum (APER). For the first
time, this audit publishes Circumferential Margin Involvement (CMI) results for
individual hospitals based on 3 consecutive years’ data.
• APER rate for elective resected rectal cases was 34% in 2009/10 and 28% in
2010/11.
Recommendations
It is recommended that LHBs consider the following actions:
1. Maintain the continual improvement on data collection through:
a. The lead clinician and other MDT members ensuring accurate and complete
data recording for their patients.
b. Appropriate provision for coding and administration staff to support the clinical
MDT staff.
2. MDTs use this audit report as a basis for an annual review of their practice and
performance as benchmarked against other Welsh MDTs, and the UK-wide
NBOCAP, with each MDT holding an annual meeting to review their performance.
3. Prompted by the high postoperative mortality of emergency patients, MDTs to review
their practice to optimise their management of emergency patients (e.g. prompt

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
8
access to emergency theatres and critical care services, availability of colonic
stenting).
4. In line with current NICE guidelines, MDTs ensure that suitable patients are either
offered the choice of laparoscopic surgery or referred to surgeons/units that can offer
this if necessary. MDTs audit their laparoscopic results.
5. MDTs benchmark their performance with respect to other MDTs using three year
data on both postoperative mortality and circumferential margin involvement. Outliers
should perform in-house audit of their service to examine the reasons for their
results.
6. Move towards a national consensus on the role and application of radiotherapy for
rectal cancer, where currently a wide variation in use is reported. There is no
centrally funded MDT training in low rectal cancer management Welsh MDTs
currently; all Wales training and education should be considered.
The Cancer NSAG will:
7. Identify new clinical indicators for future audits in recognition of the audit results that
most of the NSAG clinical indicators of best practice in the management of bowel
cancer, agreed in 2008, are being exceeded by most MDTs.
8. Broaden the scope of the audit to cover more multidisciplinary data, to include:
a. Analysis of the outcomes of patients with rectal cancer who appear to have a
complete response and therefore do not initially undergo surgical resection
(“wait and watch”).
b. Analysis of stoma reversals and CMI rates for rectal cancers operated on as
emergencies.
c. Permanent stoma rates and complications
d. Dukes A polyp cancers
e. Complications from operations including the need to return to theatre for
further surgery
9. Support LHBs by providing feedback via PowerPoint to individual MDTs.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
9
10. Work with WG and NBOCAP to explore sharing of analysis of Welsh data
submissions to allow the WCBA to focus on unique analysis pertinent to Welsh
outcomes and patients.
11. Annually update the colorectal cancer section of the Cancer Delivery Plan’s
Technical report with key information to support improving outcomes.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
10
Introduction This document reports a two year audit of patients diagnosed and treated by the 13
colorectal MDTs between 1st April 2009 and 31st March 2010 and between 1st August 2010
and 31st July 2011. There has been an adjustment in the start month of the audit year
between the two years reported within this report to allow the WBCA to align itself with
NBOCAP which previously altered the start date of its audit to August in 2009. The Cancer
NSAG supported a report encompassing two years to bring the WBCA in alignment with the
NBOCAP report2 (published December 2012).
Data collection The information source for the WBCA report is Canisc (Cancer Network Information System
Cymru) which is the Wales clinical cancer record/database. The collection of data in Canisc
by cancer MDTs has been mandated by WG since 20083.
The audit was limited to those patients diagnosed with a colorectal cancer (see appendix 1)
during the dates specified above. A file consisting of the data items in NBOCAP (appendix 1)
was extracted from Canisc in July 2012. A validation process identified duplicate entries and
incompatible and out of range values (described in the relevant sections of the report). In
addition, the data file was cross-linked with data held by the Bowel Screening Wales (BSW)
Programme to identify all patients diagnosed by the Screening Programme.
Those patients who either died within 30 days of surgery or before discharge from hospital
should be recorded in Canisc and therefore reported to the audit. However, experience from
previous WBCA4, 5 and NBOCAP audits6 have shown that there can be under-reporting of
this extremely important outcome by individual MDTs. As in the previous two WBCA reports,
the Canisc data file has been cross-linked with a copy of the Office for National Statistics
(ONS) death file held by WCISU to ensure all patients dying within 30 days of surgery were
identified.
The audit methodology at this stage is unable to differentiate between patients who are
being primarily managed for their diagnosis of colorectal cancer and those who are being
primarily managed for another diagnosis but also have colorectal cancer e.g. a patient with

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
11
primary lung cancer who also has a colorectal primary. The audit group considers that this
would relate to a very minor number of cases within the audit as a whole, but on a patient
level treatment may incorrectly appear sub-optimal. In terms of the outcome measures
presented here, this would largely be limited to the percentage of patients surgically treated.
Throughout the report there are defined rules that govern the way that results are reported.
• the term operation is used for all procedures excluding stent insertion and
endoscopic polypectomy.
• a resection involves removal of the primary disease, either endoscopically or
surgically, therefore from the data items procedure list (appendix 1) the following
procedures are not recorded as resections:
o Examination under Anaesthesia only (EUA)
o Stoma – ileostomy and colostomy only
o Laparotomy only
o Laparoscopy only
o Stent procedures
o Some “other procedures” in which there are no histopathology results
recorded to suggest a resection has taken place.
The final cleaned file was analysed using two software packages, IBM SPSS™i and
STATA™ii and the results were compared to ensure accuracy.
Data presentation Results are attributed to the MDT responsible for providing patient care. In a small number
of cases a patient will have been diagnosed in one MDT and had surgery performed in
another MDT, in these cases the results have been attributed to the MDT that performed the
surgery. Results have been reported by MDT, rather than LHB, because some LHBs have
more than one colorectal MDT. Analysis in this way allows more relevant interpretation of the
audit results and facilitates local review of outcomes and process of care.
i IBM SPSS StatisticsMac v20, is the registered trademark of IBM Corporation, USA ii STATA is the registered trademark of STATACORP, L.P. Texas, USA,

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
12
In some figures the abbreviations in table 1 have been used for MDTs due to space
constraints. Table 1: Abbreviations used for MDTs
MDT Abbreviation Bronglais General Hospital Bronglais/BR Cardiff & Vale Cardiff/CAR Nevill Hall Hospital NHH Prince Charles Hospital PCH Princess of Wales and Neath Port Talbot Hospitals POW & NPT Royal Glamorgan Hospital RGLH Royal Gwent Hospital RGH Swansea Hospitals (Moriston/Singleton) Swansea/SWA West Wales General and Prince Philip Hospitals WGH & PPH Withybush General Hospital Withybush/WB Ysbyty Glan Clwyd YGC Ysbyty Gwynedd YG Ysbyty Maelor Wrexham YMH
The report has been prepared in two principal sections. The first reports on the care of all
patients in Wales with a new diagnosis of colorectal cancer (CRC) in the audit periods. The
second focuses on only the care of patients diagnosed through the BSW Programme. This
report is the first to include data from a whole audit year that includes screen-detected
patients.
The results are presented either as tables with numerical values or bar charts (some with
error bars representing the 95% confidence interval).
Risk adjusted mortality – logistic regression
Risk adjusted mortality rates were calculated using logistic regression. Logistic regression
analysis is a method used for predicting an outcome (usually a binary variable yes(1)/no(0))
based on one or more predictor variables. It is possible to test whether a predictor variable is
statistically significant in affecting the outcome of interest when other predictor variables are
taken into account. The probabilities describing the possible outcome as a function of
explanatory variables are modelled using a logistic function.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
13
For this analysis, the outcome was whether a patient had died within 30 days (inclusive) of
surgery. The predictor variables analysed were sex, age, cancer site, ASA, Dukes stage,
surgical urgency, surgical access and whether the surgery was a resection.
The analysis was performed by the statistics unit at WCISU, using similar methods to those
used to produce the Association of Coloproctology of Great Britain and Ireland (ACPGBI)
Colorectal Cancer Risk adjusted mortality model 7, 8 (see appendix 4).
The predictor variables found to be significant were age, ASA, Dukes’ stage, surgical
urgency and surgical access.
The analysis was repeated using only complete data (i.e. no missing values for any of the
predictor variables) and results were similar to those using all data.
Funnel plots
The funnel plots in this report are designed to give an indication whether the outcome for a
particular hospital is substantially different from the mean. The x axis shows the number of
cases for that hospital, and the y axis the outcome under consideration.
The dotted lines (see figure 10) show 95% (two standard deviations) confidence intervals
and dashed lines show 99.7% (three standard deviations) confidence intervals. If a hospital
were to lie outside the confidence limits then its outcome under study would be statistically
significantly different from the mean and considered to be an outlier, with higher rates if
above the upper dotted line and with lower rates if below the lower dotted line.
Data quality
This section addresses case ascertainment and completeness of key data fields, whether
the audit has captured all patients with colorectal cancer who presented to secondary care in
the relevant years and how complete was data for each of these patients, particularly for the
key variables used to calculate risk for post-operative mortality.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
14
Case ascertainment
Case ascertainment was calculated by comparison with registrations held at WCISU. The
WBCA and NBOCAP reports are based on cases diagnosed in the period, April to March, or
August to July. Cancer Registries report by calendar year. The WCISU data in table 2 refers
to cases registered 1st January – 31st December 2009 and 1st January – 31st December
2010. Case ascertainment is therefore indicative only, which explains the apparent
contradiction of a case ascertainment of >100%.
Table 2 demonstrates that the vast majority of patients expected to be treated for CRC in
Wales have been reported to the WBCA.
Table 2: Case ascertainment
2009/10 data 2010/11 data
WBCA count
WCISU count
% WBCA count
WCISU count
%
YG 178 151 118% 172 145 119%
YGC 154 163 94% 178 190 94%
YMH 143 144 99% 178 155 115%
POW & NPT 174 179 97% 171 191 90%
SWANSEA 208 217 96% 186 203 92%
WWG & PPH 165 170 97% 149 169 88%
WITHYBUSH 93 104 89% 95 98 97%
BRONGLAIS 45 46 98% 57 58 98%
NHH 108 108 100% 118 112 105%
RGH 231 215 107% 280 190 147%
CARDIFF 261 268 97% 234 264 89%
RGLH 116 118 98% 106 134 79%
PCH 143 140 102% 107 123 87%
ALL WALES 2019 2023 100% 2031 2032 100%
OTHER WELSH HOSPITAL 170 - 160 -
ENGLISH HOSPITAL 107 - 121 -
NULL HOSPITAL 56 - 42 -

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
15
Null hospital diagnoses, recorded at WCISU, are mainly Death Certificate Only (DCO)
cases, where no other information is available for that case other than a death certificate
stating a bowel cancer.
WCISU records the diagnosing hospital, whether or not it has an MDT and as a result
captures a number of cases diagnosed at smaller cottage hospitals (Other Welsh Hospitals
in the table).
Measured against WCISU records, case ascertainment for Wales as a whole (100%) and
individual hospitals is excellent.
Completeness of key fields
Table 3 reports the completeness of the variables by MDT that are used to risk adjust for
post-operative mortality following surgery. The results show an impressive increase in the
quality of data submitted to the audits compared to previous years. It will never be possible
to achieve 100% completeness for the field Dukes’ stage because it is impossible to assign
a Dukes’ stage to patients who do not have a surgical resection and do not have radiological
evidence of metastatic disease. This situation may arise in patients with surgically
resectable disease who are too unfit for surgery and those patients treated by endoscopic
excision alone.
Table 3: Data quality by MDT for the variables used in the calculation of risk adjusted mortality
a) 2009/10
MDT Age Stage ASA* Surgical urgency
YG 100% 95% 79% 100%
YGC 100% 100% 99% 100%
YMH 100% 88% 93% 99%
POW & NPT 100% 94% 99% 100%
SWANSEA 100% 89% 93% 89%
WWG & PPH 100% 85% 100% 100%
WITHYBUSH 100% 88% 96% 100%
BRONGLAIS 100% 100% 100% 100%
NHH 100% 74% 89% 100%
RGH 100% 88% 94% 100%
CARDIFF 100% 96% 87% 98%
RGLH 100% 96% 99% 99%
PCH 100% 84% 100% 100%

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
16
ALL WALES 100% 90% 94% 98%
b) 2010/11
MDT Age Stage ASA* Surgical urgency
YG 100% 93% 85% 100%
YGC 100% 93% 98% 100%
YMH 100% 73% 98% 100%
POW & NPT 100% 92% 100% 100%
SWANSEA 100% 92% 99% 100%
WWG & PPH 100% 90% 96% 99%
WITHYBUSH 100% 99% 99% 100%
BRONGLAIS 100% 96% 100% 100%
NHH 100% 91% 95% 100%
RGH 100% 90% 95% 100%
CARDIFF 100% 96% 90% 100%
RGLH 100% 96% 99% 100%
PCH 100% 86% 100% 100%
ALL WALES 100% 91% 96% 100%
*ASA includes only patients having surgical procedures other than polypectomy or stent

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
17
Number and distribution of newly diagnosed bowel cancers During the audit period the thirteen MDTs treated 2019 patients with a new diagnosis of
bowel cancer in 2009/10 and 2031 patients in 2010/11. The 2009/10 figure was an increase
of 126 cases compared to the audit of 2008/9. The increase may be due to the introduction
of population screening for colorectal cancer by Bowel Screening Wales (BSW). The age of
patients diagnosed with bowel cancer in Wales in the audit periods is reported in table 4
below. Seventy three percent of patients with bowel cancer in Wales were over 65 years of
age at diagnosis, a figure that is very similar to the 72% of patients over the age of 65
reported in NBOCAP2 for 2012.
Table 4: Age of patients diagnosed with bowel cancer in Wales
Age group
2009/10 data 2010/11 data 2 yrs of data
Colon
no.
Rectum
no.
Total
no.
Colon
no.
Rectum
no.
Total
no.
Colon
%
Rectum
%
Total
%
<35 4 2 6 11 3 14 1% 0% 0%
35-44 13 10 23 23 10 33 1% 2% 1%
45-54 60 52 112 82 41 123 5% 8% 6%
55-64 272 118 390 251 137 388 18% 22% 19%
65-74 451 190 641 449 197 646 31% 33% 32%
75-84 463 134 597 462 133 595 32% 23% 29%
85+ 184 66 250 159 73 232 12% 12% 12%
All ages 1447 572 2019 1437 594 2031 100% 100% 100%
Whilst there is little change in the proportion of colon to rectal cancer since 2007/08, when
compared with the Wales-Trent Audit of 1993 a proximal shift in disease presentation has
occurred, with the proportion of cases that are rectal decreasing from 41.3% to less than
30%4, 5, 9, 10, 11 (see table 5).
The reasons for this are not fully understood but the phenomenon of a proximal shift in CRC
incidence has previously been noted by others12.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
18
Table 5: Tumour site by MDT
MDT 2009/2010 data 2010/2011 data
Colon
no.
Rectum
no.
Total
no.
Colon
no.
Rectum
no.
Total
no.
YG 139 39 178 123 49 172
YGC 112 42 154 120 58 178
YMH 97 46 143 120 58 178
POW & NPT 137 37 174 123 48 171
SWANSEA 140 68 208 119 67 186
WWG & PPH 134 31 165 116 33 149
WITHYBUSH 67 26 93 70 25 95
BRONGLAIS 34 11 45 43 14 57
NHH 76 32 108 88 30 118
RGH 158 73 231 198 82 280
CARDIFF 190 71 261 169 65 234
RGLH 75 41 116 76 30 106
PCH 88 55 143 72 35 107
ALL WALES 1447 572 2019 1437 594 2031
Procedures used in the surgical treatment of bowel cancer Table 6 details the procedures performed to treat patients in the audit period. The names of
the procedures are fixed by the NBOCAP data set definitions (appendix 1). The Office of
Population Censuses and Surveys Classification of Surgical Operations (OPCS) codes
reported in Canisc were mapped to the data set for the WBCA/NBOCAP. In a small number
of cases the OPCS code did not easily fit the data set definitions, and the clinical audit leads
agreed the best-fit by consensus. Cases that could not be mapped were recorded as
“other”.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
19
A particular difficulty with multi-visceral resection was encountered and these procedures
were therefore recorded as “other” but included in analyses that examined outcomes in
patients having their disease resected.
The definitions of “operation” and “resection” used here have been described previously (see
data presentation section). In table 6 procedures in which the primary tumour has been
excised/resected have been shaded.
Table 6: Primary procedure performed to treat patients with bowel cancer in Wales
All Surgical Procedures 2009/10 data 2010/11 data
Right hemicolectomy 432 410 Extended right hemicolectomy 97 91 Tranverse colectomy 5 3 Left hemicolectomy 89 63 Sigmoid colectomy 130 121 Total colectomy and ileorectal anastomosis 30 50 Total excision of colon and rectum 36 13 Total excision of colon and rectum and anastomosis of ileum to anus and creation of a pouch
1 8
Hartmann's procedure 94 96 Anterior resection 390 375 APER 130 94 Transanal Resection of Tumour (TART) 14 9 Transanal Endoscopic Microsurgery (TEMS) 0 1 Polypectomy 51 74 EUA only 2 1 Laparoscopy only 2 2 Laparotomy only 7 7 Stoma - colostomy only 65 67 Stoma - ileostomy only 17 17 Stent 22 18 Other 44 29 Total 1658 1549
The number of anterior resections performed (390 for patients diagnosed in 2009/10 and
375 for those in 2010/11) appears high compared to the number of rectal cancers resected:
383 patients from the 2009/10 cohort and 332 from 2010/11. However, historically
operations where any part of the rectum is removed, even a small, proximal section, are
often recorded as anterior resection. A proportion of the anterior resections included in the

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
20
audit data will therefore relate to tumours with a primary site in the terminal portion of the
colon (sigmoid or rectosigmoid), where a portion of the rectum was removed. Another
prominent feature of table 6 is the small number of cases treated by Transanal Endoscopic
Microsurgery (TEMS): only one procedure across the audit cohort. In the future, population
screening may identify more patients suitable for local excision with this technique as part of
their tailored treatment.
Operation and resection rates
The following charts (figure 1 and figure 2) report the proportion of patients diagnosed with
either colon or rectal cancer that had an operation for their disease (this excludes patients
treated by stent and endoscopic polypectomy). The charts show considerable inter-MDT
variation in the use of surgery, with one or two MDTs operating on approximately 90% of all
patients whilst in others this figure is around 65%. Previous WBCA reports have recorded
similar variation. Whilst there is likely to be year on year variation, the data presented
suggests that there are management differences between MDTs.
Figure 1: Proportion of colon cancers being operated on by MDT and year
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
YG
YGC
YMH
POW & NPT
SWANSEA
WWG & PPH
WITHYBUSH
BRONGLAIS
NHH
RGH
CARDIFF
RGLH
PCH
ALL WALES
MD
T
09/10 colon data 10/11 colon data 95% CI

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
21
Figure 2: Proportion of rectal cancers operated on by MDT and year
Figure 3 and figure 4 show the proportion of patients diagnosed with colon and rectal cancer
respectively that had their primary tumour resected, by either surgical or endoscopic
methods. It is extremely unlikely that a patient will be cured of CRC without surgical or
endoscopic removal of their primary disease, except for a small proportion of rectal cancers
that may have a complete clinicopathological response to radiotherapy. It is therefore
concerning to note that only 56% of patients diagnosed with rectal cancer in Wales in
2010/11 had their primary tumour resected. The implication being that fewer than 6 out of 10
patients in Wales have potentially curative disease at diagnosis. These data have clear
implications when comparing survival with other nations.
The figure in Wales is similar to the 57% of patients with rectal cancer who had their disease
resected in the 2012 NBOCAP report, which included patients treated UK wide over the
same time period. The reasons why so many patients with rectal cancer do not have their
disease resected is not fully understood. In the previous WBCA report4 the rectal resection
rate at the Royal Gwent Hospital was found to be less than 50%. This prompted an in-house
study which found that the reasons for non-resection were multi-factorial but included
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
YG
YGC
YMH
POW & NPT
SWANSEA
WWG & PPH
WITHYBUSH
BRONGLAIS
NHH
RGH
CARDIFF
RGLH
PCH
ALL WALES
MD
T
09/10 rectal data 10/11 rectal data 95% CI

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
22
metastatic disease in half of patients, locally advanced disease in 15% of patients and
patient age / morbidity in a quarter of patients13.
Figure 3: Proportion of colon cancer cases being resected by MDT and year
Figure 4: Proportion of rectal cancer cases being resected by MDT and year
0% 20% 40% 60% 80% 100%
YG
YGC
YMH
POW & NPT
SWANSEA
WWG & PPH
WITHYBUSH
BRONGLAIS
NHH
RGH
CARDIFF
RGLH
PCH
ALL WALES
MD
T
09/10 colon data 10/11 colon data 95% CI
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
YG
YGC
YMH
POW & NPT
SWANSEA
WWG & PPH
WITHYBUSH
BRONGLAIS
NHH
RGH
CARDIFF
RGLH
PCH
ALL WALES
MD
T
09/10 rectal data 10/11 rectal data 95% CI

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
23
Stage of disease at presentation The Dukes’ system remains in common use for staging bowel cancer and the audit
continues to use this. Although there is also the facility in Canisc to record Tumour Node
Metastasis (TNM) stage, as developed by the International Union Against Cancer (UICC).
The continued use of Dukes’ stage allows year on year comparison of stage. It is anticipated
that future audit reports will present data on TNM and Dukes’ stage in parallel.
The relevant data item in Canisc is modified Dukes’ staging. This is the final
clinicopathological (CP) stage and takes into account clinical, radiological and histopathology
information. The CP Dukes’ stage of operated patients by MDT is recorded in figure 5. It
must be remembered that unless a patient has metastatic disease identified on radiological
investigation, a patient can only be assigned a Dukes’ stage by removal of their cancer and
histopathological analysis. Therefore, the small number of patients who are unfit or have
locally advanced disease that precludes resection are unable to be assigned a Dukes’ stage
and it is therefore expected that this data item will be missing from a small number of cases
in figure 5.
Accurate reporting of Dukes’ stage is essential as it is used to calculate the risk adjusted
mortality of a unit. As with other variables used for the calculation of risk adjusted mortality,
the reporting of Dukes’ stage has improved greatly compared to previous WBCA4, 5 and
current NBOCAP reports. Precise comparison with this year’s NBOCAP data has not been
possible because the NBOCAP report2 has moved to reporting pathological stage using the
UICC system, rather than Dukes’ stage. However, using the UICC system, pathological data
is missing from between 35 and 50% of patients included in the NBOCAP audit this year,
which results in uncertainty when interpreting results.
Experience in previous years has identified that patients with CP Dukes’ stage D are
frequently under reported. This is believed to be due to the pathologist’s report on a
resected specimen not taking into account the results of preoperative imaging. In this
situation a patient with liver metastases may be assigned a Dukes’ stage of A to C by a
pathologist not aware of the results of preoperative imaging. This stage may then
erroneously be recorded in the CP Dukes’ stage. As in previous reports validation of the CP
Dukes’ stage has been performed and any patient who has been recorded as having
metastatic disease in the Liver CT result or the distant metastases data fields in whom the
CP Dukes’ stage was not recorded as stage D has had the record amended.

Figure 5: Clinicopathological Dukes’ Stage of Operated Patients
a) 2009/10
b) 2010/11
YG YGC YMH POW & NPT SWANSEA WWG &
PPH WITHYBUSH BRONGLAIS NHH RGH CARDIFF RGLH PCH ALL WALES
(blank) 7 0 13 8 21 19 9 0 21 21 8 4 20 151
D 25 15 11 17 28 22 11 9 5 22 40 13 17 235
C 40 37 29 37 59 25 19 14 20 55 53 26 39 453
B 50 30 30 48 47 51 21 12 26 60 59 30 29 493
A 22 19 24 21 31 14 18 3 8 23 31 17 22 253
0%
20%
40%
60%
80%
100% Pr
opor
tion
of c
ases
YG YGC YMH POW & NPT SWANSEA WWG &
PPH WITHYBUSH BRONGLAIS NHH RGH CARDIFF RGLH PCH ALL WALES
(blank) 8 8 28 10 13 10 1 2 8 20 6 3 12 129
D 20 14 12 14 24 10 10 13 11 26 25 19 7 205
C 22 36 19 44 44 24 12 10 28 55 40 30 29 393
B 42 34 31 48 55 42 33 20 42 61 48 15 26 497
A 31 23 15 13 23 15 11 4 3 37 33 11 14 233
0%
20%
40%
60%
80%
100%
Prop
orti
on o
f cas
es

Figure 6 below details the proportion of patients by MDT who have metastatic disease
(Dukes’ stage D) at presentation. These patients are presenting with a stage of disease
which is unlikely to be curable and increases the risk of postoperative death. There is year
on year variation between MDTs but the all Wales figure has been around 20% in the
previous WBCA reports, unchanged since the Wales-Trent Bowel Cancer Audit of 1993 and
similar to the results reported in the NBOCAP report in 20122. It is hoped that the
introduction of population screening for bowel cancer in Wales will reduce this figure in future
audits.
Figure 6: Proportion of Dukes’ D stage by MDT and year for all colorectal cases
0% 10% 20% 30% 40% 50%
YG
YGC
YMH
POW & NPT
SWANSEA
WWG & PPH
WITHYBUSH
BRONGLAIS
NHH
RGH
CARDIFF
RGLH
PCH
ALL WALES
MD
T
2008/09 data 2009/10 data 2010/11 data

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
26
Surgical urgency of operated patients
The National Confidential Enquiry into Patient Outcome and Death (NCEPOD)
categorisation is used to classify surgical urgency (see appendix 2). The completeness of
surgical urgency reporting has seen year on year improvement since the start of the audit.
In the audit year 2009/10 surgical urgency was complete in over 98% of patients operated
upon (see appendix 5). This figure rose further in 2010/11 with only one case out of 1457
patients operated upon missing surgical urgency data. Table 7 below reports surgical
urgency of patients operated on an urgent or emergency basis by MDT. Table 7: Number of urgent and emergency operations by MDT performed in the audit
09/10 data 10/11 data
Immediate (Emergency) Urgent Immediate (Emergency) Urgent
YG 16 17 10 4
YGC 19 6 27 15
YMH 10 4 8 12
POW & NPT 5 12 1 7
SWANSEA 23 19 35 7
WWG & PPH 16 4 20 6
WITHYBUSH 13 0 15 1
BRONGLAIS 10 4 5 1
NHH 27 2 16 7
RGH 28 11 26 18
CARDIFF 17 22 35 2
RGLH 9 16 8 11
PCH 17 1 8 1
ALL WALES 210 118 214 92

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
27
Figure 7: Proportion of operated cases that were classed as emergency/urgent in the management of colorectal cancer in Wales
The rate of urgent/ emergency surgery has remained static at around 20% over recent audits
periods (figure 7) and is similar to that reported in the Wales-Trent audit of 1993 and the
21% figure reported in the most recently published NBOCAP report2. Urgent/emergency
surgery to treat bowel cancer is associated with a far higher risk of peri-operative mortality
than elective surgery. The crude mortality rate for urgent/emergency surgery was 16% in
2009/10 and 11% in 2010/11. The rates compare unfavourably with a rate of 3% for elective
surgery in both 2009/10 and 2010/11. The rates of urgent/emergency surgery by MDT are
presented in figure 8. It is concerning that the need for emergency surgery has not
decreased. The reasons for this are poorly understood, and it is a challenging area in which
to improve the results of bowel cancer care. It is hoped that as the BSW programme matures
this figure will reduce.
It is possible that NCEPOD categorisation is not being accurately recorded; two thirds of all
unplanned operations were recorded as immediate (emergency), which according to
NCEPOD classification would suggest that these patients would have gone to theatre within
minutes of a decision to operate. In the surgical management of CRC it would be unusual for
a patient to require such immediate surgery. To avoid confusion a simpler separation is to
present surgery performed on either an elective/scheduled or emergency/urgent basis
(figure 8).
0% 10% 20% 30% 40% 50%
2010/11
2009/10
2008/09
Proportion of operated on cases

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
28
Figure 8: Surgical urgency by MDT and year
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
YG
YGC
YMH
PO
W &
N
PT
SWA
NSE
A
WW
G &
PP
H
WIT
HYB
USH
BR
ON
GL
AIS
N
HH
RG
H
CARD
IFF
RGLH
PC
H
ALL
W
ALE
S
MD
T
Elective/scheduled Emergency/urgent
MDT
Cardiff
YG
YGC
YMH
Swansea
POW & NPT
NHH
WWG & PPH
PCH
RGH
RGLH
Bronglais
Withybush
All Wales

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
29
Co-morbidity Co-morbidity is recorded using American Society of Anaesthesiologists (ASA) grading
(appendix 3). Whilst this is a subjective measure, it has previously been demonstrated to
correlate well with the risk of post-operative death8. Over the past few years there has been
a steady improvement in the recording of ASA status, rising to 94% complete in 2009-10 and
96% complete on 2010-11 (table 3). Figure 9 reports the ASA score of operated patients.
As in previous audits there are variations between MDTs.
It is generally accepted that ASA scoring has a subjective component, as it relies on the
anaesthetist’s opinion about a patient’s general health. Inter-unit differences may be a
combination of different co-morbidity levels in the patients that a unit is treating and
differences in ASA grading by anaesthetists between units.
Figure 9: ASA score by MDT in operated colorectal cancer patients for the years 2009/10 and 2010/11
a) 2009/10
YG YGC YMH POW
& NPT
SWANSEA
WWG &
PPH
WITHYBUS
H
BRONGLAIS
NHH RGH CARD
IFF RGLH PCH
ALL WALE
S
Unknown 30 1 7 1 13 0 3 0 9 10 24 1 0 99
4 & 5 8 6 5 7 9 8 4 5 2 5 9 4 5 77
3 32 32 28 40 43 23 29 19 26 58 47 16 50 443
2 57 50 50 65 99 80 35 12 39 88 86 46 66 773
1 17 12 17 18 22 20 7 2 4 20 25 23 6 193
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Prop
orti
on o
f cas
es
SWA WB CAR BR All Wales

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
30
b) 2010/11
30-day mortality following surgery for bowel cancer
Non-adjusted 30 day mortality following elective colorectal surgery in both audit years across
Wales was 3% (data not shown). Figure 10 represents the risk-adjusted 30 day mortality rate
for both elective and emergency surgery throughout Welsh hospitals over the last three audit
periods. The variables analysed on each patient were sex, age, cancer site, ASA, Dukes’
stage, surgical urgency, surgical access and whether the surgery was a resection. The
impact that each factor made to the model is reported in appendix 4. Robust comparison of
post-operative mortality needs to be ‘risk-adjusted’ to ensure that the impact of differences
between patients can be taken into account (e.g. age, comorbidity, stage of presentation,
emergency surgery etc.). The results have been averaged from 3 continuous years’ data,
which avoids drawing conclusions based on the variations that are recognised to occur year-
on-year or anomalous periods.
YG YGC YMH POW
& NPT
SWANSEA
WWG &
PPH
WITHYBUS
H
BRONGLAIS
NHH RGH CARD
IFF RGLH PCH
ALL WALE
S
Unknown 18 2 2 0 2 4 1 0 5 10 15 1 0 60
4 & 5 5 12 4 7 5 6 0 3 5 6 4 5 4 66
3 30 43 26 34 50 7 18 18 38 63 53 18 36 434
2 55 53 59 65 85 73 37 25 33 102 73 40 37 737
1 15 5 14 23 17 11 11 3 11 18 7 14 11 160
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Prop
orti
on o
f cas
es
SWA WB BR CAR All Wales

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
31
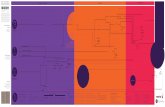
The average 30 day risk-adjusted mortality from the last three years of data is 5.1%, ranging
from 2.5% to 8.6% between hospitals. For comparison, the figure for England using Hospital
Episode Statistics (HES) data from 2003-2006 was 6.2%14 and the unadjusted figure for
Denmark 2001-2004 was 9.9%15.
It is worth noting that in previous years NBOCAP has reported Wales as having a higher
average observed post-operative mortality than England. However they have also
demonstrated that lower case ascertainment leads to a decreased postoperative mortality
estimate with the conclusion that observed rates in Wales better reflected the true mortality
rate compared to English rates as a whole.
Hospitals should use their own data to audit their results in comparison with others. Much of
the variation in 30 day mortality is probably due to the timely diagnosis and management of
emergency patients. Those with a high ASA score deserve particular attention from the
surgical and critical care teams as a patient is over 12 times more likely to suffer from a post-
operative death within 30 days of surgery with an ASA score of IV or V compared to a
patient with an ASA score of 1. Social deprivation and lifestyle factors are not included in
the risk adjustment model used by the WBCA. However, differences in deprivation have
been shown to contribute to an excess risk of peri-operative mortality in more deprived
patients undergoing surgery for CRC16 and may be a contributory factor to the observed
differences.
Figure 10: Risk adjusted postoperative mortality (within 30 days) for patients having surgery
(combined 3 years’ data for patients diagnosed April 2008-March 2010 and August 2010 to July 2011)
BRONGLAIS
CARDIFF
NHH
PCH
POW & NPT
RGLH
RGH
SWANSEA
WWG & PPH
WITHYBUSH YGC
YG
YMH
0
1
2
3
4
5
6
7
8
0 50 100 150 200
Ris
k ad
just
ed m
orta
lity
rate
(%)
Cases
Data Average 2SD limits 3SD limits

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
32
Use of laparoscopic surgery in Wales NICE have recommended laparoscopic surgery as an alternative to open surgery for the
treatment of bowel cancer1, providing that the patient and their disease are suitable for this
approach and that appropriately trained surgeons are able to undertake the surgery. The
benefit of a laparoscopic approach is that patients receive an equally effective cancer
operation but have a more rapid recovery, with a shorter hospital stay. The current audit has
found that a laparoscopic approach was associated with a reduction in hospital stay of three
days.
Recent consecutive audit periods show a progressive increase in the use of laparoscopic
surgery for the treatment of bowel cancer across Wales, with the figure for elective surgery
in 2010/11 standing at 46% (figure 11, excludes data on polyps, stents, EUA, TART and
TEMS). This figure is higher than that reported in England, where for the similar 2010/11
period 34% of elective operations were performed laparoscopically. The increased uptake in
Wales is testament to the Welsh laparoscopic colorectal training scheme that was introduced
by WG in response to the NICE recommendation. There is debate amongst experts as to the
appropriate percentage of patients that are able to have a laparoscopic approach but the
wide inter-MDT variability in Wales suggests that there is scope for increased use. The
uptake for elective bowel resection by MDT is shown in figure 11, which highlights this
variation. The trend in most MDTs is for an increased use in the most recent audit period.
This report does not include conversion rates for laparoscopic to open surgery, due to this
data not having been routinely collected during the current audit periods. It is however,
recognised that conversion rates are important to record in laparoscopic colorectal surgery.
Therefore, the routinely collected data has been amended to include this and it will be
reported in future audits.

Figure 11: Percentage of elective/scheduled cases performed laparoscopically by MDT (excludes polyps, stents, EUA, TART and TEMS)
YG YGC YMH POW & NPT SWANSEAWWG &
PPHWITHYBUSH BRONGLAIS NHH RGH CARDIFF RGLH PCH ALL WALES
2009/10 data 43% 47% 1% 24% 46% 4% 43% 0% 10% 41% 63% 14% 77% 36%
2010/11 data 81% 72% 16% 35% 40% 3% 72% 2% 22% 47% 68% 7% 91% 46%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Prop
orti
on o
f ca
ses

Figure 12: Variation in known surgical access for elective major colon resections by year and
resection type
Figure 12 reports the use of laparoscopic surgery for the most frequently performed elective
operations for bowel cancer (excludes polyps, stents, EUA, TART and TEMS). Over 50% of
anterior resections and right hemicolectomies were performed laparoscopically in the
2010/11 audit period. Of the elective operations performed for tumours located in the rectum
(figure 13), 35% were performed laparoscopically in 2009/10 and 40% in 2010/11.
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
2009/10
2010/11
AR
APE
R Ex
t R
Hem
i H
artm
ann'
s
Lapa
roto
my
/Lap
aros
copy
on
ly
L H
emi
Oth
er
R H
emi
Sigm
oid
cole
cto
my
Colo
stom
y on
ly
Ileos
tom
y on
ly
TC &
IR
A
Proc
toco
lect
om
y
Rest
orat
ive
Proc
toco
lect
om
y
Tran
s co
lect
om
y To
tal
Laparoscopic Open
APER
AR
TC & IRA
Left Hemi
Other
Trans colectomy
Hartmann's
TOTAL
Right Hemi
Procto colectomy
laparotomy/ laparoscopy only
SIgmoid colectomy
Colostomy only
Ileostomy only
restorative proto- colectomy
Ext R Hemi

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
35
Figure 13: Variation in known surgical access for elective major rectal resections by year and resection type
Length of stay Length of stay (LOS) is an outcome measure that is of interest to the patient, the surgeon
and healthcare managers. It is calculated by measuring the interval in days between the
date of operation and the date of death or discharge. The Wales median LOS is eight days,
a reduction of one day compared to the WBCA audit of 2008/9. The median LOS in the
current audit is the same as that reported in the UK wide NBOCAP report2. An ongoing
finding of the WBCA is that the LOS after surgery has reduced in each successive year and
is now almost half the fifteen day median LOS reported in the Wales-Trent audit of 1993.
The median LOS by MDT is reported in figure 14. Organisations may wish to examine the
local reasons for the failure of LOS to fall further.
Anterior resection
APER Hartmann's procedure
Other Anterior resection
APER Hartmann's procedure
Other
2009/10 data 2010/11 data
Open 102 88 17 11 92 53 17 12
Laparoscopic 73 35 8 1 69 39 7 2
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Prop
orti
on o
f cas
es

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
36
Figure 14: Overall median length of stay after surgery reported by MDT performing surgery (in
days), surgical access and year
The overall reduction in LOS after surgery has been achieved through reductions in the LOS
after elective surgery. LOS after urgent/emergency surgery has been 12 days in each of the
three audits between 2008 and 2011. In the audit year 2010/11 (table 8) the median LOS
after elective surgery has fallen to seven days. The widening difference between median
LOS after elective and emergency surgery is likely to be due to both the increased use of
laparoscopic surgery and the introduction of enhanced recovery after surgery programmes.
0 2 4 6 8 10 12 14 16
YG
YGC
YMH
POW & NPT
SWANSEA
WWG & PPH
WITHYBUSH
BRONGLAIS
NHH
RGH
CARDIFF
RGLH
PCH
ALL WALES
Median LOS (days)
MD
T
Open 2009/10 Laparoscopic 2009/10 Open 2010/11 Laparoscopic 2010/11

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
37
Table 8: Median LOS after surgery reported by MDT and surgical urgency
2009/10 data 2010/11 data
Elective/
Scheduled
Urgent/
Emergency
Elective/
Scheduled
Urgent/
Emergency
YG 11 19 7 16
YGC 7 10 7 11
YMH 8 11 7 10.5
POW & NPT 7 10.5 7 15
SWANSEA 6 7.5 6 8.5
WWG & PPH 10 10.5 6.5 14
WITHYBUSH 8 26 5 12.5
BRONGLAIS 12 13.5 11 16
NHH 8 10.5 8.5 10
RGH 8 12 8 12
CARDIFF 7 14 7 9
RGLH 8 11.5 8 13
PCH 5 16 6 8.5
ALL WALES 8 11.5 7 12
Table 8 reports the median LOS after surgery according to surgical access. In the units
performing higher volumes of laparoscopic surgery there is a marked decrease in LOS
associated with the use of minimally invasive surgery.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
38
Rectal cancer
Use of radiotherapy
Figure 15 reports the use of radiotherapy in patients having elective resectional surgery for
rectal cancer by MDT. These figures show that there are wide variations in the use of
radiotherapy between MDTs. Of the higher volume MDTs (treating >20 cases of rectal
cancer per year) the use of radiotherapy in patients treated for rectal cancer varies between
30% and 86% (Swansea and Ysbyty Glan Clwyd MDTs respectively).
There are no standardised UK wide protocols for decision making with regards to
radiotherapy and the variation in the use of radiotherapy by Welsh MDTs reflects this.
Figure 15. Use of radiotherapy by MDT in patients having elective resective surgery for rectal
cancer
a) 2009/10
YG YGC YMH POW
& NPT SWAN
SEA WWG & PPH
WITHYBUS
H
BRONGLAIS
NHH RGH CARDI
FF RGLH PCH
ALL WALE
S
Pre-op short course 3 4 6 0 0 0 0 0 0 3 6 1 2 25
Pre-op long course 12 15 21 13 17 4 9 1 5 23 22 4 6 152
Post-op 1 0 1 0 1 0 0 1 0 2 0 1 3 10
None 8 3 5 14 23 14 7 3 12 19 20 17 28 173
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Prop
orti
on o
f cas
es
SWA WB BR CAR ALL
WALES

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
39
b) 2010/11
Circumferential margin involvement
Involvement of the non-peritonealised resection margin in the surgical removal of rectal
cancer is known to confer a far worse outcome for the patient with both increased rates of
local recurrence of their disease and poorer overall survival. Involvement is defined as
there being a distance of <1mm between the tumour and the mesorectal fascial plane, and
reported as Circumferential Marginal Involvement (CMI).
In previous WBCA reports CMI has been poorly recorded in Canisc. This is no longer the
case, with only 7% of cases not having CMI recorded in 2009/10 and 8% in 2010/11. This
compares favourably with the 26% missing in the Welsh 2008/9 report and the 40.4%
missing in the latest NBOCAP report2.
The overall CMI for all patients operated on electively with rectal cancer in Wales was 7.0%
(excluding the patients in whom CMI was not reported to the audit). NBOCAP 2012 reported
a CMI rate of 7.9% over the same period2. There is no national guidance on the
YG YGC YMH POW
& NPT
SWANSEA
WWG &
PPH
WITHYBUS
H
BRONGLAIS
NHH RGH CARDI
FF RGLH PCH
ALL WALE
S
Pre-op short course 4 1 8 2 0 0 0 0 3 3 5 0 0 26
Pre-op long course 9 17 11 17 8 1 4 0 6 20 14 5 4 116
Post-op 1 2 2 0 2 1 0 2 0 1 0 0 2 13
None 14 5 6 14 34 12 8 6 6 17 13 15 16 166
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Prop
orti
on o
f cas
es
SWA WB BR CAR ALL
WALES

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
40
recommended standard for this value but the large UK multi-centre CR07 trial had a rate of
12%17.
The rates of CMI are higher in patients undergoing Hartmann’s procedures and APER than
those treated by anterior resection (AR, table 9). Hartmann’s procedure may be used as a
palliative procedure when the operating surgeon has anticipated an involved CMI, which
may explain higher rates for this procedure compared to others. APER operations are most
frequently used with curative intent in the treatment of low rectal cancers. The finding that
APER in Wales is associated with a higher CMI (11% in the two most recent audits) is in
keeping with the results from previous NBOCAP audits and published series. The reason for
higher CMI rates following APER is believed to be due to the increased technical difficulty of
adequately removing tumours that are located lower in the rectum and anal canal. Whilst
margin involvement is often perceived to be a surgical failing it is also a reflection of whole
MDT performance, including interpretation of pre-operative radiological imaging and
decisions about the use of pre-operative radiotherapy as these are also important
determinants of this outcome measure.
In England, concern about high CMI rates in the treatment of low rectal cancer have led to
the development of the centrally funded LOREC, which is training programme for all
members of the colorectal MDT, with the aim of improving patient outcomes.
Table 9: CMI in patients having elective surgery for rectal cancer according to operation
performed
Audit year
Operation performed 2009/10 2010/11
Anterior resection 2% 3%
APER 11% 11%
Hartmann’s procedure 15% 13%
Figure 16 reports the circumferential margin involvement (CMI) for elective, major resection
surgeries for rectal cancer by MDT over a three year period. Three-year data has been
presented because the case volume of each MDT in Wales is relatively small and the
outcome being studied (CMI) is an uncommon occurrence.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
41
Figure 16: Proportion of elective major resected rectal cases seen by an MDT, with CMI in a 3
year period (where CMI status is recorded)
The dotted lines represent deviations in results away from the mean by two and three
standard deviations respectively.
It is interesting to compare these data with the rates of radiotherapy reported in the previous
section of this report. Two units are shown to have a significantly lower rate (based on 95%
confidence limits) of CMI than the national average (figure 16), both are relatively high
volume units, yet their use of pre-operative radiotherapy is markedly different: 26% in the
Swansea MDT compared to 82% in the YGC MDT.
YG
YGC
YMH
POW & NPT
SWANSEA
WWG & PPH
WITHYBUSH
BRONGLAIS
NHH
RGH
CARDIFF
RGLH PCH
0
5
10
15
20
25
30
0 20 40 60 80 100 120
prop
ortio
n of
cas
es
Population of eligible rectal cases Data Average 2SD limits 3SD limits

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
42
APER rates
The all Wales APER rate for elective resected rectal cases was 34% in 2009/10 and
28% in 2010/11.
This has been calculated from major elective resections as shown in figure 17.
Figure 17: Major resection procedure rates for elective rectal cases (2009/10 and 2010/11
combined)
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
YG
YGC
YMH
POW & NPT
SWANSEA
WWG & PPH
WITHYBUSH
BRONGLAIS
NHH
RGH
CARDIFF
RGLH
PCH
ALL WALES
MD
T
APER Anterior resection Hartmann's procedure Other

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
43
Clinical outcomes
Lymph node harvest
NICE, the Royal College of Pathologists (RCP) and the ACPGBI have all recommended that
12 nodes should be examined following the surgical resection of colorectal cancer with an
associated mesenteric lymphadenectomy18. This is to ensure accurate staging and inform
decisions about adjuvant therapy. Patients staged as node negative after examination of
less than 12 nodes have a significantly reduced survival19, 20.
The year on year improvement in both the median lymph node harvest and proportion of
patients having the threshold of 12 nodes examined has now reached a plateau (figure 18).
These results match those reported UK wide in the NBOCAP audits.
There were two MDTs that did not achieve the 12 node guidance in 2009/10 and three in
2010/11 (figure 19, black line indicates the minimum median number of lymph nodes to be
harvested). As per NICE guidance, it is recommended that MDTs who consistently examine
fewer than 12 nodes (Bronglais) or have dropped below the recommended median (YG,
WWG & PPH, and RGLH) during the audit period should have a discussion between
surgeons and pathologists about their techniques to optimise nodal yield.
Figure 18: Proportion of major surgical resections achieving the 12 node median harvest guidance
0% 20% 40% 60% 80% 100%
2008/09
2009/10
2010/11

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
44
Figure 19: Median lymph node harvest by MDT for colorectal major resections
Extra-mural vascular invasion
Extra-mural vascular invasion (EMVI) is defined as the presence of tumour within the extra-
mural endothelium lined space21. The presence of EMVI confers a worse prognosis,
consequently it is recommended that patients with EMVI should be considered for adjuvant
chemotherapy, even in the absence of lymph node metastases. The Royal College of
Pathologists (RCPath), “Standards and Datasets for reporting Colorectal Cancer (2nd
edition)”21 recommends that EMVI should be identified in 25% of colorectal cancer resection
specimens in order to confirm adequate pathological examination. EMVI is reported for the
first time in the WBCA audit in figure 20 below. Overall, four out of thirteen of the MDTs did
not meet the RCPath guidance in either 2009/10 or 2010/11 (indicated by the black line in
figure 20). The charts also show that there is variance in EMVI reporting across Wales, with
the Ysbyty Gwynedd MDT identifying EMVI in 14% of reported cases in 2010/11 and the
West Wales General MDT identifying EMVI in 47% of cases in 2009/10, although the figure
for this MDT dropped to 25% in the audit year 2010/11. The NBOCAP report in 20122 found
that EMVI was present in 35% of colon cancer patients and 25% of rectal cancer patients,
although only 70% of patients had data relating to EMVI recorded in that audit.
0 2 4 6 8 10 12 14 16 18 20
YG
YGC
YMH
POW & NPT
SWANSEA
WWG & PPH
WITHYBUSH
BRONGLAIS
NHH
RGH
CARDIFF
RGLH
PCH
ALL WALES
MD
T
2009/10 data 2010/11 data ---------- median of 12 lymph nodes

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
45
Figure 20: EMVI rates for all major surgical resections by MDT
a) 2009/10
b) 2010/11
YG YGC YMH POW
& NPT
SWANSEA
WWG &
PPH
WITHYBUS
H
BRONGLAIS
NHH RGH CARDI
FF RGLH PCH
ALL WALE
S
Blank 4 1 2 5 15 7 0 0 5 3 3 1 1 47
No 101 64 70 76 107 51 61 30 54 109 106 56 82 967
Yes 28 29 32 45 43 51 12 8 16 51 52 25 28 420
0% 10% 20% 30% 40% 50% 60% 70% 80% 90%
100%
Prop
orti
on o
f cas
es
SWA WB BR CAR ALL
WALES
RCPath recommended level (25%)
YG YGC YMH POW
& NPT
SWANSEA
WWG &
PPH
WITHYBUS
H
BRONGLAIS
NHH RGH CARDI
FF RGLH PCH
ALL WALE
S
Blank 2 0 3 2 4 7 0 0 3 8 0 0 1 30
No 96 72 77 75 90 63 39 36 59 115 102 41 50 915
Yes 16 33 18 47 45 23 26 11 22 53 30 34 21 379
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Prop
orti
on o
f cas
es
SWA WB BR CAR ALL
WALES
RCPath recommended level (25%)

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
46
National Specialist Advisory Group Clinical Indicators In 2008 the Cancer Services Co-ordinating Group (CSCG), the precursor to the cancer
NSAG, established six clinical indicators of best practice in the management of bowel cancer
(1-6 below).
1. All elective cases seen by specialist nurse before surgery.
2. Review by MDT of all cases.
3. Abdominal CT scan before surgery in all cases (elective and emergency) excluding
polypectomies and stents.
4. Pelvic MRI scan (or EUS) carried out before all elective rectal cancer resections.
5. Report the presence or absence of non-peritonealised (circumferential) margin
involvement in all rectal cancer resections (except local resections).
6. The median number of lymph nodes examined in resection specimens for colorectal
cancer should be at least 12 (except local resections).
The indicators are derived from the data in Canisc. As in previous audit reports for the
indicators between 1 and 5, attainment of at least 80% (the minimum threshold) is indicated
by green shading (see table 10). For indicator 6 teams achieving a median harvest of 12 or
greater are shaded green. Poor quality data returns, rather than not meeting the standard,
may be an issue in some MDTs.
Compliance with the clinical indicators in 2010/11 is very good across all MDTs in Wales.
In 2009/10 eight of the fourteen MDTs were not compliant with the indicator measuring MRI
before all elective rectal cancer resections. This had improved by 2010/11 although
Swansea should review adherence to protocols and data input.
Bronglais has persistently reported a median number of lymph nodes examined of less than
12 and should review practice. All MDTs non-compliant with any indicator should review their
data and practice.
Since the clinical indicators were introduced in 2008 there have been annual year on year
improvements in attainment of the indicators across Wales. Whilst it is important that MDTs
maintain compliance with the current clinical indicators the NSAG have been asked to
identify new indicators for future WBCA reports.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
47
Table 10: Compliance with Cancer NSAG Clinical Indicators a) 2009/10
09/10 data CNS (elective
cases)
MDT (all)
CT (all op excl stents & polyps)
MRI (all rectal elective
resections)
CMI recorded (major rectal resections)
Median no. nodes (major
resections)
YG 98% 100% 95% 96% 100% 12
YGC 97% 99% 94% 83% 96% 15
YMH 100% 97% 90% 76% 84% 13
POW & NPT 95% 99% 95% 81% 96% 17
SWANSEA 96% 97% 82% 71% 98% 16
WWG & PPH 94% 100% 93% 74% 89% 9
WITHYBUSH 100% 98% 91% 94% 94% 16
BRONGLAIS 56% 96% 92% 60% 100% 9
NHH 9% 93% 64% 41% 93% 15
RGH 99% 99% 96% 77% 100% 12
CARDIFF 88% 93% 90% 92% 90% 15
RGLH 86% 100% 91% 74% 95% 13
PCH 99% 98% 89% 80% 82% 12
ALL WALES 91% 98% 90% 79% 93% 13
b) 2010/11
10/11 data CNS (elective
cases)
MDT (all)
CT (all op excl stents & polyps)
MRI (all rectal elective
resections)
CMI recorded (major rectal resections)
Median no. nodes (major
resections)
YG 91% 100% 98% 89% 87% 10
YGC 99% 100% 96% 84% 100% 17
YMH 100% 99% 79% 85% 96% 19
POW & NPT 93% 98% 98% 88% 100% 15.5
SWANSEA 91% 98% 92% 66% 86% 17
WWG & PPH 92% 100% 86% 86% 54% 12
WITHYBUSH 83% 96% 94% 92% 91% 12
BRONGLAIS 93% 98% 94% 100% 100% 10
NHH 96% 98% 95% 93% 100% 16
RGH 98% 99% 96% 80% 100% 12.5
CARDIFF 93% 98% 96% 91% 94% 15
RGLH 73% 99% 83% 95% 100% 11
PCH 98% 95% 75% 86% 81% 12
ALL WALES 93% 99% 92% 85% 92% 14

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
48
Bowel screening
Faecal Occult Blood (FOB) test based bowel cancer screening was introduced nationally in
Wales at the end of October 2008. Following a two month period testing systems and
processes, the first positive results were passed to Local Screening Centres in January
2009. FOB testing was offered to all individuals aged between 60 and 69 using an initial 6
window guaiac FOB card. Participants receiving an equivocal result were asked to undergo
a secondary test, the faecal immuno-chemical test (FIT). This differs from the English
Programme where a repeat guaiac test is offered to people with equivocal results. The
Programme is co-ordinated from the central hub at Llantrisant and there are 11 Local
Screening Centres (LCS) throughout Wales. From October 2011 the age range was
extended up to 74 years. After the first round, the uptake of screening was 55.2% of the
invited population. The FOB positivity rate for the first round of screening was 2.8%; the
detection of pathology at colonoscopy was over 70%.
Screening demographics From April 2009-March 2010 there were 203 screen detected colorectal cancers. These
represent 10.1% of all colorectal cancers in Wales. Of the screen detected cancers, 162
were colonic and 41 were rectal cancers. From August 2010–July 2011 there were 241
screen-detected colorectal cancers, representing 11.9% of all colorectal cancers detected.
Of these, 186 were colonic and 55 were rectal cancers (see table 11).

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
49
Table 11: Number and proportion of screen and symptomatic colon and rectum cancers by
MDT
a) 2009/10
Colon Rectum
2009/10 data Screen detected Symptomatic Screen detected Symptomatic
YG 11 (8%) 128 (92%) 2 (5%) 37 (95%)
YGC 7 (6%) 105 (94%) 5 (12%) 37 (88%)
YMH 14 (14%) 83 (86%) 4 (9%) 42 (91%)
POW & NPT 20 (15%) 117 (85%) 5 (14%) 32 (86%)
SWANSEA 20 (14%) 120 (86%) 5 (7%) 63 (93%)
WWG & PPH 22 (16%) 112 (84%) 1 (3%) 30 (97%)
WITHYBUSH 8 (12%) 59 (88%) 1 (4%) 25 (96%)
BRONGLAIS 3 (9%) 31 (91%) 0 (0%) 11 (100%)
NHH 8 (11%) 68 (89%) 1 (3%) 31 (97%)
RGH 16 (10%) 142 (90%) 8 (11%) 65 (89%)
CARDIFF 11 (6%) 179 (94%) 6 (8%) 65 (92%)
RGLH 7 (9%) 68 (91%) 1 (2%) 40 (98%)
PCH 15 (17%) 73 (83%) 2 (4%) 53 (96%)
ALL WALES 162 (11%) 1285 (89%) 41 (7%) 531 (93%)
b) 2010/11
Colon Rectum
2010/11 data Screen detected Symptomatic Screen detected Symptomatic
YG 18 (15%) 105 (85%) 2 (4%) 47 (96%)
YGC 16 (13%) 104 (87%) 7 (12%) 51 (88%)
YMH 18 (15%) 102 (85%) 5 (9%) 53 (91%)
POW & NPT 7 (6%) 116 (94%) 4 (8%) 44 (92%)
SWANSEA 18 (15%) 101 (85%) 8 (12%) 59 (88%)
WWG & PPH 15 (13%) 101 (87%) 2 (6%) 31 (94%)
WITHYBUSH 9 (13%) 61 (87%) 5 (20%) 20 (80%)
BRONGLAIS 5 (12%) 38 (88%) 2 (14%) 12 (86%)
NHH 9 (10%) 79 (90%) 5 (17%) 25 (83%)
RGH 41 (21%) 157 (79%) 8 (10%) 74 (90%)
CARDIFF 16 (9%) 153 (91%) 1 (2%) 64 (98%)
RGLH 3 (4%) 73 (96%) 3 (10%) 27 (90%)
PCH 11 (15%) 61 (85%) 3 (9%) 32 (91%)
ALL WALES 186 (13%) 1251 (87%) 55 (9%) 539 (91%)

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
50
Surgical treatment On diagnosis of cancer, the management of the patient is referred to the patient’s local
colorectal MDT for treatment. With regards to malignant polyps, surgical activity varies
between teams with some advocating resection for all such lesions and others treating with
polypectomy in appropriately selected cases. Table 12 demonstrates the outcome of screen
detected cancers managed by each MDT.
Table 12: Surgical management of screen detected cancers by MDT
a) 2009/10
2009/10 data Operated on Polypectomy Not operated on Total
YG 12 1 0 13
YGC 9 0 3 12
YMH 15 1 2 18
POW & NPT 15 9 1 25
SWANSEA 25 0 0 25
WWG & PPH 19 3 1 23
WITHYBUSH 9 0 0 9
BRONGLAIS 3 0 0 3
NHH 6 1 2 9
RGH 17 4 3 24
CARDIFF 14 3 0 17
RGLH 7 0 1 8
PCH 15 1 1 17
ALL WALES 166 23 14 203
b) 2010/11
2010/11 data Operated on Polypectomy Not operated on Total
YG 17 2 1 20
YGC 13 2 8 23
YMH 15 6 2 23
POW & NPT 7 3 1 11
SWANSEA 24 0 2 26
WWG & PPH 12 2 3 17
WITHYBUSH 11 2 1 14
BRONGLAIS 7 0 0 7
NHH 12 0 2 14
RGH 32 10 7 49
CARDIFF 13 2 2 17
RGLH 6 0 0 6
PCH 11 2 1 14
ALL WALES 180 31 30 241

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
51
Stage at presentation of screen detected cancers
During the first (prevalent) round of the English bowel cancer screening programme there
was a marked improvement in cancer stage at diagnosis, with more cancers presenting at
an earlier stage (10% polyp cancer, 32% Dukes’ A, 30% Dukes’ B). There was a decrease in
advanced cancers at diagnosis (25% Dukes’ C and 3% Dukes’ D). Staging data was missing
on 11% of cancers22. Table 13 demonstrates the Dukes’ staging of the screen detected
cancers in Wales.
Table 13: Clinicopathological Dukes stage at presentation of screen detected cancers
a) 2009/10
2009/10 data A B C1 C2 D Blank Total
YG 2 6 1 2 2 0 13
YGC 4 3 4 0 1 0 12
YMH 5 3 2 0 2 6 18
POW & NPT 7 6 2 0 1 9 25
SWANSEA 10 4 6 1 1 3 25
WWG & PPH 3 9 6 0 1 4 23
WITHYBUSH 2 1 2 1 0 3 9
BRONGLAIS 1 1 1 0 0 0 3
NHH 1 3 0 0 2 3 9
RGH 6 4 5 1 1 7 24
CARDIFF 7 3 3 0 3 1 17
RGLH 1 3 1 1 1 1 8
PCH 4 5 3 0 2 3 17
ALL WALES 53 51 36 6 17 40 203

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
52
b) 2010/11
2010/11 data A B C C1 C2 D Blank Total
YG 14 2 0 2 1 0 1 20
YGC 11 2 0 6 0 2 2 23
YMH 8 4 1 4 1 0 5 23
POW & NPT 5 2 0 3 0 1 0 11
SWANSEA 8 13 0 3 1 1 0 26
WWG & PPH 11 1 0 2 0 2 1 17
WITHYBUSH 7 4 0 3 0 0 0 14
BRONGLAIS 0 4 0 2 0 1 0 7
NHH 2 6 0 3 0 2 1 14
RGH 20 9 0 11 0 6 3 49
CARDIFF 11 4 0 2 0 0 0 17
RGLH 2 1 0 2 1 0 0 6
PCH 4 3 0 5 1 1 0 14
ALL WALES 103 55 1 48 5 16 13 241
Tumours diagnosed within the screening programme were more likely to be of an earlier
stage than the symptomatic group. In 2009-10 the screening group consisted of 51% of
tumours being Dukes’ A or B. In 2010-11 this rose to 66% of all screened cancers against
only 27% for patients not diagnosed through screening (x2, p<0.001). In both years the rate
of Dukes’ D cancers was a lowly 8% and 7% respectively. This compares with a Dukes’ D
rate of 24% in the non-screened population. Table 14 shows the different Dukes’ staging
between screen-detected cancers and non-screen detected (symptomatic) cancers.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
53
Table 14: Comparison of Dukes’ staging by referral type (screening and symptomatic)
a) 2009/10
Screened Symptomatic X2 p value
N % n %
Dukes’ A 53 26% 224 12% p<0.001
Dukes’ B 51 25% 457 25% p=0.002 Dukes’ C 42 21% 423 23% p=0.725 Dukes’ D 17 8% 429 24% p<0.001
Missing data 40 20% 283 16% p=0.186
b) 2010/11
Screened Symptomatic X2 p value
N % n %
Dukes’ A 103 43% 182 10% p<0.001 Dukes’ B 55 23% 463 26% p=0.048 Dukes’ C 54 22% 346 19% p=0.298 Dukes’ D 16 7% 424 24% p<0.001
Missing data 13 5% 375 21% p<0.001
Laparoscopic surgery for screen-detected cancers
It has been hoped that the earlier stage of diagnosis in screen detected cancers might make
these patients more amenable to laparoscopic resection. These two tables once again
reflect the wide variation of laparoscopic practice across Wales with many suitable screened
patients not being offered this type of surgery. Some centres offer no laparoscopic surgery,
whilst others are able to offer laparoscopic surgery to the majority of their screen-detected
patients. Screen-detected cancers are more likely to be amenable to laparoscopic resection
than symptomatic tumour and therefore feasibility of laparoscopic resection should be
considered as part of the MDT discussion.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
54
Table 15: Mode of surgical access of operations in screen detected cancers
a) 2009/10
2009/10 data Laparoscopic Open Total
YG 6 (50%) 6 (50%) 12
YGC 7 (88%) 1 (12%) 8
YMH 1 (7%) 14 (83%) 15
POW & NPT 5 (33%) 10 (67%) 15
SWANSEA 19 (76%) 6 (24%) 25
WWG & PPH 1 (5%) 18 (95%) 19
WITHYBUSH 4 (44%) 5 (56%) 9
BRONGLAIS 0 (0%) 3 (100%) 3
NHH 1 (17%) 5 (83%) 6
RGH 10 (59%) 7 (41%) 17
CARDIFF 11 (92%) 1 (2%) 12
RGLH 2 (29%) 5 (71%) 7
PCH 13 (87%) 2 (13%) 15
ALL WALES 80 (49%) 83 (51%) 163
b) 2010/11
2010/11 data Laparoscopic Open Total
YG 16 (94%) 1 (6%) 17
YGC 9 (75%) 3 (25%) 12
YMH 4 (27%) 11 (73%) 15
POW & NPT 1 (14%) 6 (84%) 7
SWANSEA 11 (46%) 13 (54%) 24
WWG & PPH 0 (0%) 12 (100%) 12
WITHYBUSH 9 (82%) 2 (18%) 11
BRONGLAIS 0 (0%) 7 (100%) 7
NHH 4 (33%) 8 (67%) 12
RGH 22 (69%) 10 (31%) 32
CARDIFF 10 (77%) 3 (23%) 13
RGLH 0 (0%) 6 (100%) 6
PCH 11 (100%) 0 (0%) 11
ALL WALES 97 (54%) 82 (46%) 179

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
55
Post operative mortality for screen detected cancers
Mortality is unfortunately perhaps inevitable after surgery for colorectal cancer. It is hoped
that screening will present younger patients with earlier stage disease to the MDTs; mortality
rates should hopefully be kept to a minimum in this group. There were only two operative
mortalities (overall 0.006%) in screen detected patients, one in each year of the audit.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
56
APPENDIX 1: Data set used in NBOCAP/WBCA
Available at the following link: http://www.hscic.gov.uk/bowel
ICD-10 diagnosis codes used in NBOCAP/WCBA
C18.0 – Caecum
C18.1 – Appendix
C18.2 – Ascending colon
C18.3 – Hepatic flexure
C18.4 – Transverse colon
C18.5 – Splenic flexure
C18.6 – Descending colon
C18.7 – Sigmoid colon
C19.X – Recto-sigmoid
C20.X – Rectum
APPENDIX 2: NCEPOD operative urgency classification
National Confidential Enquiry into Patient Outcome and Death (NCEPOD) Classification of
Interventions, December 2004. Reproduced with kind permission. Original available at the
following link: http://www.ncepod.org.uk/
Value Timing of surgery Notes
Immediate (previously termed emergency)
Immediate (Life, limb or
organ saving intervention)
Resuscitation
simultaneous with surgical
treatment. The target time
to theatre is within minutes
of decision taken to
operate
Urgent Intervention within 24
hours
The target time to theatre
is within 24 hours of
decision to operate and
normally once
resuscitation is complete.

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
57
Expedited (previously termed scheduled)
Expedited (Stable patient
requiring early intervention
for a condition that is not
an immediate threat to life,
limb or organ survival)
The target time to theatre
is within days of decision
to operate.
Elective Elective (Surgical
procedure planned or
booked in advance of
routine admission to
hospital)
APPENDIX 3: American Society of Anesthesiology Grading System American Society of Anesthesiologists (ASA) grade is the most commonly used co-morbidity
grading system.
ASA Grade Physical status
ASA I Healthy patient
ASA II
Mild systemic disease with no functional limitation - for example, controlled hypertension
ASA III Severe systemic disease with definite functional limitation - for example, chronic obstructive pulmonary disease
ASA IV
Severe systemic disease that is a constant threat to life - for example, unstable angina
ASA V Moribund patient who is not expected to survive for 24 hours with or
without surgery - for example, with a ruptured abdominal aortic aneurysm

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
58
APPENDIX 4: Odds ratios for 30 day mortality following surgery calculated from the WBCA risk adjustment model. In brief, a backward stepwise method was used which first creates a model that fits the
observed data using all predictor variables. An iterative process then tests each predictor
variable in turn to determine if its removal significantly affects the fit of the model and thus
whether it should be included. The best fit model was used to calculate adjusted rates of
mortality.
The table below presents the adjustment in mortality risk according to the variables that were
used in calculating risk-adjusted mortality in the WBCA. The risks are presented as an odds
ratio. These data show that the risk of 30 day mortality for a >85 year old is 4.4 times
greater than a 64 year old undergoing the same operation, with the same ASA score,
surgical urgency and Dukes’ stage. It can be seen that being ASA IV or V has the biggest
mortality risk. The reduced odds associated with laparoscopic surgery is almost certain to
be a reflection that laparoscopic surgery is usually used in elective, rather than urgent /
emergency surgery and that pathologically advanced tumours (with higher Dukes’ stage) are
less likely to be successfully performed laparoscopically.
Risk Factor Odds ratio Age <65 1.0
65-74 1.7 75-84 3.6 >85 4.4
ASA score I 1.0 II 1.8 III 3.7 IV & V 12.5 Missing ASA 4.7
Dukes’ stage A 1.0 B 2.0 C 2.1 D 3.7 Missing Dukes’ 2.1
Surgical Urgency
Elective / Scheduled 1.0 Urgent 2.7 Emergency 2.6 Missing urgency 2.0
Surgical access Open 1.0 Laparoscopic 0.6 Missing access 1.0

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
59
APPENDIX 5: DATA
This appendix contains the data that underlies charts percentages and analysis in the main
report. Each table is entitled “data relating to table/figure x” together with the caption of the
analysis that is generated from it. In electronic format these are hyperlinked to the relevant
document in the main.
Index for data relating to figures/tables in the main text
Data relating to: Title of figure Page
Table 3 Data quality by MDT for the variables used in the calculation of risk adjusted mortality
60
Figure 1 Proportion of colon cancers being operated on by MDT and year 61
Figure 2 Proportion of rectal cancers operated on by MDT and year 61
Figure 3 Proportion of colon cancer cases being resected by MDT and year 62
Figure 4 Proportion of rectal cancer cases being resected by MDT and year 62
Figure 6 Proportion of Dukes’ D stage by MDT and year for all colorectal cases
63
Figure 7 Proportion of operated cases that were classed as emergency/urgent in the management of colorectal cancer in Wales
63
Figure 8 Surgical urgency by MDT and year 64
Figure 11 Percentage of elective/scheduled cases performed laparoscopically by MDT
65
Figure 12 Variation in known surgical access for elective major colon resections by year and resection type
66
Figure 14 Overall median length of stay after surgery reported by MDT performing surgery (in days), surgical access and year
67
Figure 16 Proportion of elective major resected rectal cases seen by an MDT, with CMI in a 3 year period
67
Figure 17 Major resection procedure rates for elective rectal cases (2009/10 and 2010/11 combine
68
Figure 18 Proportion of major surgical resections achieving the 12 node median harvest guidance
68
Figure 19 Median lymph node harvest by MDT for colorectal major resections
69
Table 9 CMI in patients having elective surgery for rectal cancer according to operation performed
69
Table 10 Data quality for items used in risk adjusted mortality calculations. 70

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
60
Data relating to Table 3: Data quality by MDT for the variables used in the calculation of risk adjusted mortality a.
2009/10 data
Age recorded
Dukes stage recorded
ASA recorded
Surgical urgency recorded
Total no. operated on cases
YG 144 137 114 144 144
YGC 101 101 100 101 101
YMH 107 94 100 106 107
POW & NPT 131 123 130 131 131
SWANSEA 186 165 173 166 186
WWG & PPH 131 112 131 131 131
WITHYBUSH 78 69 75 78 78
BRONGLAIS 38 38 38 38 38
NHH 80 59 71 80 80
RGH 181 160 171 181 181
CARDIFF 191 183 167 188 191
RGLH 90 86 89 89 90
PCH 127 107 127 127 127
ALL WALES 1585 1434 1486 1560 1585
b.
2010/11 data
Age recorded
Dukes stage recorded
ASA recorded
Surgical urgency recorded
Total no. operated on cases
YG 123 115 105 123 123
YGC 115 107 113 115 115
YMH 105 77 103 105 105
POW & NPT 129 119 129 129 129
SWANSEA 159 146 157 159 159
WWG & PPH 101 91 97 100 101
WITHYBUSH 67 66 66 67 67
BRONGLAIS 49 47 49 49 49
NHH 92 84 87 92 92
RGH 199 179 189 199 199
CARDIFF 152 146 137 152 152
RGLH 78 75 77 78 78
PCH 88 76 88 88 88
ALL WALES 1457 1328 1397 1456 1457

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
61
Data relating to Figure 1: Proportion of colon cancers being operated on by MDT and year
Colon 09/10 data 10/11 data
Operated on Total Operated on Total
YG 116 139 94 123
YGC 76 112 90 120
YMH 74 97 76 120
POW & NPT 104 137 97 123
SWANSEA 128 140 103 119
WWG & PPH 106 134 85 116
WITHYBUSH 59 67 54 70
BRONGLAIS 30 34 39 43
NHH 64 76 71 88
RGH 129 158 148 198
CARDIFF 140 190 114 169
RGLH 65 75 58 76
PCH 78 88 61 72
ALL WALES 1169 1447 1090 1437
MDT data relating to Figure 2: Proportion of rectal cancers operated on by MDT and year
Rectal 09/10 data 10/11 data
Operated on Total Operated on Total
YG 28 39 29 49
YGC 25 42 25 58
YMH 33 46 29 58
POW & NPT 27 37 32 48
SWANSEA 58 68 56 67
WWG & PPH 25 31 16 33
WITHYBUSH 19 26 13 25
BRONGLAIS 8 11 10 14
NHH 16 32 21 30
RGH 52 73 51 82
CARDIFF 51 71 38 65
RGLH 25 41 20 30
PCH 49 55 27 35
ALL WALES 416 572 367 594

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
62
Data relating to Figure 3: Proportion of colon cancer cases being resected by MDT and year
09/10 data 10/11 data
Resected Total Resected Total
YG 113 139 101 123
YGC 70 112 87 120
YMH 75 97 85 120
POW & NPT 110 137 98 123
SWANSEA 120 140 95 119
WWG & PPH 95 134 83 116
WITHYBUSH 56 67 56 70
BRONGLAIS 31 34 41 43
NHH 64 76 68 88
RGH 127 158 151 198
CARDIFF 124 190 103 169
RGLH 61 75 56 76
PCH 73 88 54 72
ALL WALES 1119 1447 1078 1437
Data relating to Figure 4: Proportion of rectal cancer cases being resected by MDT and year
09/10 data 10/11 data
Resected Total Resected Total
YG 25 39 28 49
YGC 24 42 25 58
YMH 35 46 30 58
POW & NPT 27 37 33 48
SWANSEA 47 68 46 67
WWG & PPH 20 31 15 33
WITHYBUSH 18 26 13 25
BRONGLAIS 8 11 8 14
NHH 17 32 16 30
RGH 47 73 42 82
CARDIFF 51 71 34 65
RGLH 24 41 20 30
PCH 40 55 22 35
ALL WALES 383 572 332 594

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
63
Data relating to Figure 6: Proportion of Dukes’ D stage by MDT and year for all colorectal cases
2008/09 2009/10 2010/11
DUKES D Total DUKES D Total DUKES D Total
YG 35 177 40 178 31 172
YGC 46 143 47 154 43 178
YMH 28 153 32 143 30 178
POW & NPT 38 160 40 174 32 171
SWANSEA 32 207 39 208 38 186
WWG & PPH 21 135 38 165 30 149
WITHYBUSH 28 104 21 93 22 95
BRONGLAIS 7 41 10 45 15 57
NHH 16 103 15 108 30 118
RGH 49 203 36 231 52 280
CARDIFF 44 247 78 261 69 234
RGLH 24 95 23 116 34 106
PCH 17 125 27 143 14 107
ALL WALES 385 1893 446 2019 440 2031
Data relating to Figure 7: Proportion of operated cases that were classed as emergency/urgent in the management of colorectal cancer in Wales
No. emergency/urgent
cases
Total no. operated
cases
2010/11 306 1457
2009/10 328 1585
2008/09 287 1480

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
64
Data relating to Figure 8: Surgical urgency by MDT and year
Elective/scheduled Emergency/urgent
YG 2009/10 111 33
2010/11 109 14
YGC 2009/10 76 25
2010/11 73 42
YMH 2009/10 92 14
2010/11 85 20
POW & NPT 2009/10 114 17
2010/11 121 8
SWANSEA 2009/10 124 42
2010/11 117 42
WWG & PPH 2009/10 111 20
2010/11 74 26
WITHYBUSH 2009/10 65 13
2010/11 51 16
BRONGLAIS 2009/10 24 14
2010/11 43 6
NHH 2009/10 51 29
2010/11 69 23
RGH 2009/10 142 39
2010/11 155 44
CARDIFF 2009/10 149 39
2010/11 115 37
RGLH 2009/10 64 25
2010/11 59 19
PCH 2009/10 109 18
2010/11 79 9
ALL WALES 2009/10 1232 328
2010/11 1150 306

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
65
MDT data relating to Figure 11: Percentage of elective/scheduled cases performed laparoscopically by MDT
2009/10 data 2010/11 data
No. performed
laparoscopically
Total no. of
elective cases
No. performed
laparoscopically
Total no. of
elective cases
YG 47 109 87 107
YGC 35 75 51 71
YMH 1 91 13 83
POW & NPT 27 113 42 121
SWANSEA 57 124 46 116
WWG & PPH 4 110 2 74
WITHYBUSH 28 65 36 50
BRONGLAIS 0 24 1 43
NHH 5 49 15 69
RGH 58 142 72 153
CARDIFF 90 144 78 114
RGLH 9 63 4 59
PCH 83 108 72 79
ALL WALES 444 1217 519 1139

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
66
All-Wales data relating to Figure 12: Variation in known surgical access for elective major colon resections by year and resection type
2009/10 data 2010/11 data
No. performed laparoscopically
No. performed open
No. performed laparoscopically
No. performed open
AR 175 196 183 173
APER 36 92 39 55
Ext R Hemi 10 49 15 39
Hartmann's 11 30 10 31
Laparotomy/Laparoscopy only
0 6 3 1
L Hemi 32 42 22 33
Other 6 19 1 8
R Hemi 124 177 170 148
Sigmoid colectomy 37 65 46 57
Colostomy only 8 30 18 20
Ileostomy only 0 7 3 6
TC & IRA 2 19 7 23
Proctocolectomy 2 25 2 10
Restorative Proctocolectomy
0 1 0 6
Trans colectomy 1 1 0 2
Total 444 759 519 612

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
67
MDT data relating to Figure 14: Overall median length of stay after surgery reported by MDT performing surgery (in days), surgical access and year
Median length of stay 2009/10 data 2010/11 data
Open Laparoscopic Open Laparoscopic
YG 13 9 13 7
YGC 9 6 11 5.5
YMH 8 4.5 8 6
POW & NPT 8 6 7 6
SWANSEA 8 5 8.5 5
WWG & PPH 10 13 8.5 1
WITHYBUSH 8 10 8 4
BRONGLAIS 13 - 11.5 14
NHH 8 6 10 4.5
RGH 10 6 9 6
CARDIFF 12 6 11 6
RGLH 8 9.5 8 4
PCH 10 5 9 5
ALL WALES 9 6 9 6
MDT data relating to Figure 16: Proportion of elective major resected rectal cases seen by an MDT, with CMI in a 3 year period
2008/09 data 2009/10 data 2010/11 data
CMI no. of elective rectal major resections
seen by MDT with a known CMI
CMI no. of elective rectal major resections
seen by MDT with a known CMI
CMI no. of elective rectal major resections seen by MDT with a known
CMI YG 4 28 0 22 1 20
YGC 1 22 1 22 0 20
YMH 1 22 1 26 1 20
POW & NPT 6 32 0 24 2 30
SWANSEA 1 37 3 38 0 37
WWG & PPH 1 16 2 17 0 6
WITHYBUSH 1 15 0 16 1 9
BRONGLAIS 0 4 1 5 4 8
NHH 0 1 1 13 5 15
RGH 1 12 4 43 0 38
CARDIFF 3 37 3 36 4 30
RGLH 5 20 3 21 0 20
PCH 4 18 4 32 1 16
ALL WALES 28 264 23 315 19 269

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
68
MDT data relating to Figure 17: Major resection procedure rates for elective rectal cases (2009/10 and 2010/11 combined)
APER Anterior resection Hartmann's procedure Other Total
YG 18 26 1 0 45
YGC 17 21 4 1 43
YMH 12 33 0 6 51
POW & NPT 15 21 15 4 55
SWANSEA 33 39 3 6 81
WWG & PPH 15 12 2 2 31
WITHYBUSH 10 15 2 0 27
BRONGLAIS 5 8 0 0 13
NHH 10 13 4 2 29
RGH 24 51 5 1 81
CARDIFF 18 50 1 2 71
RGLH 19 17 5 1 42
PCH 19 32 8 1 60
ALL WALES 215 338 50 26 629
All-Wales data relating to Figure 18: Proportion of major surgical resections achieving the 12 node median harvest guidance
No. cases with >= 12 nodes removed Total no. of major resections
2008/09 856 1332
2009/10 868 1434
2010/11 862 1324

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
69
MDT data relating to Figure 19: Median lymph node harvest by MDT for colorectal major resections
2009/10 median no. lymph nodes 2010/11 median no. lymph nodes
YG 12 10
YGC 15 17
YMH 13 19
POW & NPT 17 15.5
SWANSEA 16 17
WWG & PPH 9 12
WITHYBUSH 16 12
BRONGLAIS 9 10
NHH 15 16
RGH 12 12.5
CARDIFF 15 15
RGLH 13 11
PCH 12 12
ALL WALES 13 14
All-Wales data relating to Table 9: CMI in patients having elective surgery for rectal cancer according to operation performed
2009/10 data 2010/11 data
Operation performed CMI Total no. elective rectal surgeries
CMI Total no. elective rectal surgeries
Anterior resection 4 176 5 162
APER 14 123 10 92
Hartmann's procedure 4 26 3 24

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
70
MDT data relating to Table 10: Compliance with Cancer NSAG Clinical Indicators a
2000
-
2010
da
ta CN
S se
en
No.
ele
ctiv
e ca
ses
Dis
cuss
ed a
t M
DT
All
case
s
CT s
can
done
All
oper
atio
ns
(exc
l ste
nts
&
poly
ps)
MRI
sca
n do
ne
All
rect
al
elec
tive
re
sect
ions
CMI r
ecor
ded
All
maj
or r
ecta
l re
sect
ions
Med
ian
no.
node
s
All
maj
or
rese
ctio
ns
YG 119 122 178 178 137 144 23 24 23 23 12 133
YGC 74 76 153 154 95 101 19 23 23 24 15 94
YMH 97 97 138 143 96 107 25 33 27 32 13 104
POW & NPT 119 125 173 174 125 131 22 27 24 25 17 126
SWANSEA 119 124 202 208 152 186 29 41 44 45 16 165
WWG & PPH 108 115 165 165 122 131 14 19 17 19 9 109
WITHYBUSH 66 66 91 93 71 78 17 18 16 17 16 73
BRONGLAIS 14 25 43 45 35 38 3 5 8 8 9 38
NHH 5 58 100 108 51 80 7 17 13 14 15 75
RGH 150 152 229 231 173 181 36 47 43 43 12 163
CARDIFF 141 160 244 261 171 191 45 49 37 41 15 161
RGLH 56 65 116 116 82 90 17 23 21 22 13 82
PCH 110 111 140 143 113 127 32 40 32 39 12 111
ALL WALES 1178 1296 1972 2019 1423 1585 289 366 328 352 13 1434

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
71
b
2010
-201
1 da
ta
CNS
seen
No.
ele
ctiv
e ca
ses
Dis
cuss
ed a
t M
DT
All
case
s
CT s
can
done
All
oper
atio
ns
(exc
l ste
nts
&
poly
ps)
MRI
sca
n do
ne
All
rect
al
elec
tive
re
sect
ions
CMI r
ecor
ded
All
maj
or r
ecta
l re
sect
ions
Med
ian
no.
node
s
All
maj
or
rese
ctio
ns
YG 114 125 172 172 120 123 25 28 20 23 10 114
YGC 77 78 178 178 110 115 21 25 20 20 17 105
YMH 98 98 177 178 83 105 23 27 22 23 19 98
POW & NPT 124 133 167 171 127 129 29 33 30 30 15.5 124
SWANSEA 107 117 183 186 147 159 29 44 38 44 17 139
WWG & PPH 72 78 149 149 87 101 12 14 7 13 12 93
WITHYBUSH 45 54 91 95 63 67 11 12 10 11 12 65
BRONGLAIS 42 45 56 57 46 49 8 8 8 8 10 47
NHH 68 71 116 118 87 92 14 15 16 16 16 84
RGH 169 172 278 280 192 199 33 41 39 39 12.5 176
CARDIFF 111 119 229 234 146 152 31 34 30 32 15 132
RGLH 44 60 105 106 65 78 19 20 20 20 11 75
PCH 81 83 102 107 66 88 19 22 17 21 12 72
ALL WALES 1152 1233 2003 2031 1339 1457 274 323 277 300 14 1324

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
72
APPENDIX 6: REFERENCES 1 National Institute for Clinical Excellence. Colorectal cancer - laparoscopic surgery (review) (TA105),
London 2006 (reviewed 2010). 2 Finan P, Smith J, Scott N, Walker K, van der Meulen J, Greenaway K, et al. National Bowel Cancer
Audit Report 2012, 2012. 3 Welsh Health Circular WHC(2008)054 4 Evans M, Roberts L, Thomas R, Williams G, Smith J, Stamatakis JD. Cancer Services Co-ordinating
Group. Bowel Cancer in Wales: Presentation, Treatment and Outcomes April 2008 to March 2009,
2010. 5 Evans M, Harris M, TRoberts L, Williams G, Smith J, Stamatakis J. Cancer Services Co-ordinating
Group 4th Bowel Cancer Audit Report. Bowel cancer: presentation, treatment and outcomes in
Wales April 2007-March 2008., 2009. 6 Finan P, Smith J, Walker K, van der Meulen J, Greenway K, Yelland A, et al. National Bowel Cancer
Audit Report 2011, 2011. 7 Tekkis PP, Poloniecki JD, Thompson MR, Stamatakis JD. ACPGBI Colorectal Cancer Study 2002
Part B: Risk Adjusted Outcomes. The ACPGBI Colorectal Cancer Model.: ACPGBI, 2002. 8 Tekkis PP, Poloniecki JD, Thompson MR, Stamatakis JD. Operative mortality in colorectal cancer:
prospective national study. BMJ (Clinical research ed 2003;327(7425):1196-201. 9 Smith JJ, Tekkis PP, Stamatakis JD. Analysis of the 2001-2003 Wales Bowel Cancer Audit Data
from the ACPGBI database: nbocap. 10 Smith JJ, Tekkis PP, Stamatakis JD. Cancer Services Co-ordinating Group 2nd Bowel Cancer Audit
Report April 2003-March 2005. 11 Stamatakis JD, Smith JJ, Davies J, Evans MD. Cancer Services Co-ordinating Group 3rd Bowel
Cancer Audit Report April 2005-April 2007. 12 Mensink PBF, Kolkman JJ, van Baarlen J, Kleibeuker JH. Change in Anatomic Distribution and
Incidence of Colorectal Cancer Over a Period of 15 Years. Dis Col Rectum 2002; 10: 1393-96. 13 Evans M, Jayamanne H, Williams G, Chamary V, McKain E, Swarnkar K, et al. Declining use of
surgery to treat rectal cancer: myth or reality? Colorectal Dis 2010;12(Suppl 1). 14 Morris EJ, Taylor EF, Thomas JD, Quirke P, Finan PJ, Coleman MP, et al. Thirty-day postoperative
mortality after colorectal cancer surgery in England. Gut 2011;60(6):806-13. 15 Osler M, Iversen LH, Borglykke A, Martensson S, Daugbjerg S, Harling H, et al. Hospital variation in
30-day mortality after colorectal cancer surgery in denmark: the contribution of hospital volume and
patient characteristics. Ann Surg 2011;253(4):733-8. 16 Smith JJ, Tilney HS, Heriot AG, Darzi AW, Forbes H, Thompson MR, et al. Social deprivation and
outcomes in colorectal cancer. Br J Surg 2006;93(9):1123-31. 17 Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S, et al. Preoperative
radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC
CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet 2009;373(9666):811-20

Cancer National Specialist Advisory Group Wales Bowel Cancer Audit (published 2013)
73
18 GT Williams, P Quirke, NA Shepherd. Standards and datasets for reporting cancers: dataset for
colorectal cancer (second edition). 2007. Royal College of Pathologists 19 Prandi M, Lionetto R, Bini A, Francioni G, Accarpio G, Anfossi A, et al. Prognostic evaluation of
stage B colon cancer patients is improved by an adequate lymphadenectomy: results of a secondary
analysis of a large scale adjuvant trial. Ann Surg 2002;235(4):458-63. 20 Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, et al. Colon
cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of
intergroup trial INT-0089. J Clin Oncol 2003;21(15):2912-9. 21 Williams GT, Quirke P, Shepherd NA. Dataset for colorectal cancer (2nd edition): The Royal
College of Pathologists, 2007. 22 Logan RF, Patnick J, Nickerson C, Coleman L, Rutter MD, von Wagner C; English Bowel Cancer
Screening Evaluation Committee. Outcomes of the Bowel Cancer Screening Programme (BCSP) in
England after the first 1 million tests. Gut. 2012; 61:1439-46.