· Web viewAs magnitude of stress increases with time, tendon/ligament may respond by adding...
Transcript of · Web viewAs magnitude of stress increases with time, tendon/ligament may respond by adding...
Atlanto-Occipital Joints
Concave oval superior facets of atlasConvex/rounded occipital condyles
Horizontal plane
Lateral Atlanto-Axial Joints
Flat circular inferior facet of atlasFlat circular superior facet of axis
Horizontal plane
Medial Atlanto-Axial Joints
Dens of axisArticular fossa for dens on posterior surface of anterior arch of atlas
Frontal plane
Cervical Facets (C3-7)
Permits extensive rotation as well as flexion, extension and lateral flexion.
Flat, oval superior and inferior facetsInferior face anterioinferiorSuperior face posteriosuperior
Frontal at about 45° to horizontal
Thoracic Region (T1-12)
Permits rotation, flexion, extension, and lateral flexion but magnitude of motion is limited by the attachment to the ribs.
Flat, oval superior and inferior facetsInferior face anteriorSuperior face posterior
Frontal at about 60° to horizontal
Upper Lumbar (L1-2)
Restricted rotation but allows forward and lateral flexion and extension.
Oval and slightly concave superior facetsOval and flat/slightly convex inferior facetsInferior face laterallySuperior face medially
Sagittal at about 90° to horizontal
Has cephalad and caudal menisci that attach to joint capsule
Lower Lumbar (L4-5) Oval and slightly concave superior facetsOval and flat/slightly convex inferior facetsInferior facets of L4 face anteriolaterally, L5 faces more anterior than lateralSuperior facets of L4-5 face posteriomedially
Diagnonal to sagittal and frontal at about 90° to horizontal
Has cephalad and caudal menisci that attach to joint capsule
*articular cartilage of facet joints is hyaline cartilage that is thick centrally and thin peripherally*jt. Capsule is dense irregular connective tissue containing collagen and elastic fibers*collagen limits facet joint movement- jt. Distraction, rotation and superor translation of inferior facets on the superior facet of the vertebra below as during forward flexion*elastic fibers prevent the capsule and synovial membrane from being pinched between the opposing facets, allow for movement between the facets, and return the capsule it its starting position. *menisci in lumbar region can become trapped between opposing articular surfaces producing a painful blockage of motion at the vertebral segment
INTERVERTEBRAL DISKS*fibrocartilaginous joint between vertebral bodies*Peripheral annulus fibrosis and central nucleus pulposus
ANNULUS FIBROSIS*6-10 rings of Fibrocartilage*collagen fibers in layers around nucleus are arranged loosely*collagen fibers in outer layers are densely packed and run obliquely between
vertebral bodies*collagen fibers in the outermost 1-2 layers show a herringbone pattern which
makes them strong in resisting tension*peripheral-most fibers attach to the smooth edge (rim) of vertebral body with
outermost fivers attaching to the periosteum and the anterior and posterior longitudinal ligaments
*other fibers attach to the hyaline cartilaginous end plate covering the rough articular surface of the vertebral bodyFUNCTIONS OF THE ANNULUS FIBROSIS
*contains nucleus pulposus*stabilization*permits multidirectional movement*shock absorbtion
NUCLEUS PULPOSUS*gelatinous mass of collagen fibers imbedded in a mucopolysccharide and
water *absorbs and retains large quantities of water*exchange of nutrients between disk and vertebral bodies*in cervical and thoracic regions, nucleus lies centrally within disk*in lumbar region, nucleus lies in the posterior ½ of disk
FUNCTIONS OF THE NUCLEUS PULPOSUS*absorbtion and retention of water*nutrition*force transmission*equalize unit stress in all directions to the annulus fibrosis*permits a rocking type segmental movement between vertebral bodies
*movement between adjacent vertebrae is needed as is the ability of the AF and NP to expand*NP expands at rest by drawing H2O & nutrients from blood vessels and lymphatics of the vertebral bodies*as NP is loaded, the nutrient fluid is forced out into the AF and waste products out of the nucleus into the vertebral bodies
*flow of fluid inwardly during rest and outwardly during loading provides for nutritional needs of the disk
SACROILIAC JOINT-synovial and fibrous articulation-synovial articulation: auricular surface of sacrum (S1-3) and auricular surface of ilium lying anterior to PSIS and inferior to iliac tuberosity-both auricular surfaces for the synovial portion have an irregular pattern of ridges and groves and both are covered with a thin layer of hyaline cartilage
Ligaments of the SpineAnterior Atlanto-occipital membrane Anterior arch of atlas with base of
occiputContinuous laterally with atlanto-occipital jt capsule
Posterior Atlanto-occipital membrane Posterior arch of atlas with occiputContinuous with lateral atlanto-occipital ligament
Anterior atlanto-axial membrane Body of axis to anterior arch of atlasContinuous with atlanto-axial jt capsule
Posterior atlanto-axial membrane Posterior body of axis to posterior arch of atlasContinuous with atlanto-axial jt capsule
Lateral atlanto-occipital ligament Transverse process of atlas with occipital bone and strengthens atlanto-occipital jt
Tectorial membrane Continuation of posterior longitudinal ligament connects posterior arch of axis to occipital bone covers cruciform, alar and apical ligaments
Cruciform ligament Consists of transverse ligament of atlas, superior band and inferior bandSuperior band attaches to occipital boneInferior band attaches to body of axis
Transverse ligament of atlas Cups posterior surface of densattaches to posterior surface of anterior arch of atlas on each side of the medial atlanto-axial joint
Alar ligaments (paired) Attach to sides and posterior surface of dens and run laterally with superior band attaching to occiput, middle band to lateral mass of atlas, inferior band to axis
Apical ligaments Anterior to the superior band of cruciform ligament Connects apex of dens to occiput
Anterior longitudinal ligament Attaches to anterior rim of vertebral bodies and anterior aspect of IVD
Runs from sacrum to atlasBecomes anterior atlanto-occipital membrane
Posterior longitudinal ligament Attaches to posterior rim of vertebral bodies and posterior aspect of IVDAnterior surface of spinal canal from sacrum to axisBecomes tectorial membrane
Ligament flava Paired segmental elastic ligaments on posterior aspect of spinal canal Sacrum to axis Connects lamina of adjacent vertebrae
Supraspinous ligament Attaches to tips of spinous processes from C7continuous with ligamentum nuchae to about L4Replaced by erector spinae fascia
Interspinous ligaments Inferior and superior aspects of adjacent SP from C7 to L5-S1
Ligamentum nuchae Complex fibrous septum that runs along posterior midline of neck from C7 to occiputConnects tips and superior and inferior aspects of cervical SP to the occiput
Intertransverse ligament Connects TP of adjacent vertebraeIliolumbar ligament Starts as muscle, ligament by 40
TP of L5(males)/L4-5 (females) to superior SIJ and ilium
Sacrotuberous ligament Runs obliquely from posterior surface of PIIS and Posteriolateral aspect of lower sacrum and upper coccyx to the medial aspect of the Ischial tuberosity and Ischial ramus
Sacrospinous lgament Runs obliquely from posteriolateral surface of lower sacrum and coccyx to Ischial spine
Interosseus SI ligament Connects the iliac and sacral tuberosities at the fibrous SI jt
Short dorsal SI ligament Run horizontally from dorsolateral aspect of the superior part of the sacral tuberosityto the dorsal aspect of the tuberosity of the ilium
Long dorsal SI ligament Runs obliquely from the dorsolateral aspect of the inferior part of the sacral tuberosity and the dorsal surface of the sacrotuberous ligament to the PSIS
Ventral SI ligament Runs horizontally from the ventrolateral margin of the sacrum to ventral aspect of the auricular surface of the ilium
Facet Joint Motion-forward bending exposes some 40% of the facet joint area-functional left sidebending causes more upward sliding of the right facet than does forward bending-rotation to the right causes right facet distraction and left facet compression; left facet slide forward with vertebrae tilting into left side bending-FWD BENDING: upward movement of inferior articular processes; slides up and forward-BWD BENDING: downward movement of inferior articular processes; slides down and back contacting the lamina below-LEFT ROTATION: gapping at left facet, right facet acts as a fulcrum-SIDEBENDING/ROTATION: downslide of inferior articular facets on side to which cervical spine rotates; upslide on opposite side
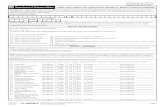
Region Flexion Extension Right Side Bend
Right Rotation
Atlanto-Occipital
Occipital condyles Roll anteriorlyGlide posteriorly
Occipital condyles Roll posteriorlyGlide anteriorly
Occipital condyles Roll rightGlide left
ROC moves slightly backLOC moves slightly forward
Atlanto-Axial Facets move forward
Facets move backward
Atlas slides right
RF moves back LF moves forward
C2/3-T2/3 Facets slide up and forward
Facets slide down and back
RF slides down and backLF slides up and forward
RF slides down and backLF slides up and forward
T3/4-T11/12 Facets slide up Facets slide down
RF slides down LF slides up
RF distractsLF compresses and acts as fulcrum
Lumbar Facets slide up Facets slide down
RF slides downLF slides up
RF distractsLF compresses and acts as fulcrum
Vertebrae Forward Flexion
Anterior tilting (rocking) of vertebral body over NPCompression & bulging of anterior IVD (AF)Tension on posterior IVD (AF)NP deforms posteriorlyIV foramen increasesSP separateDecreased compression on facet jtTension on supraspinous, interspinous,
intertransverse, ligamentum flava, posterior longitudinal ligamentSlack on anterior longitudinal ligament
Vetebrae Backward Extension
Posterior tilting (rocking) of vertebral body of NPCompression and bulging of the posterior IVD (AF)Tension on anterior IVD (AF)IV foramen decreasesSP convergeIncreased compression on facet jtSlack in supraspinous, interspinous, intertranverse, ligamentum flava, posterior longitudinal ligamentTension on anterior longitudinal ligament
Vertebral Side Bending/Lateral Flexion
(in cervical spine, coupling occurs- when head and neck are bent right, SP go left.)
Lateral tilting of vertebral body over nucleus on side toward movementCompression and bulging of IVD on side toward movementTension on IV on side opposite movementNucleus deforms to side opposite movementIV foramen decreases on side of movementIV foramen increases on side opposite movementIncreased compression on facet jt on side of movementDecreased compression on facet jt on side opposite movementTension on intertransverse lig on side opposite movementSlack on intertransverse lig on side of movement
Vertebrae Rotation Increased compression on NPShear stress on AFIncreased compression on facet opposite to rotationDecreased compression on facet joint on side of rotationTension on jt capsule on side of rotation
SI joint Movement limited to 1-3 degreesMovement mainly at anterioposterior directionRotation and translation occurNutation- movement of sacrum related to ilium as during fwd bending of trunk and squattingTorsion- movement of ilium relative to sacrum as in lying supine and brining the knee to the chest
Loads on the SpineCervical Spine
*Loads at the AO jt are lowest in full extension and highest in full flexion*Loads at C7-T1 are least when head is facing forward and chin is tucked*Loads at C7-T1 are slightly greater when the head is in the correct posture, greater still when the head is extended and greatest at full flexion
Lumbar Spine*Loads are least when lying supine*Loads are low with relaxed standing, greater with supported sitting, and still greater with unsupported sitting
*Compression loads on the lumbar spine are greatest near the toe off stage in walking*Loads increase on the lumbar spine as the velocity of walking increases
Muscle ActionsForward trunk flexion from standing
Abs and ilipsoas move trunk forward while gravity pulls downward. Erector spinae eccentrically control downward movement. At 60 degrees of trunk flexion, pelvis rotates anteriorly at hips. Glute max and hamstrings eccentrically control anterior pelvic rotation.
Trunk extension from full flexionErector spinae very active at full flexion in stabilizing spine. During initial 30 degrees of extension, pelvis rotates posteriorly at hips. Glute max and hamstrings concentrically produce pelvic rotation. Last 60 degrees of extension is produced by concentric contraction of erector spinae.
Trunk side bendingQL, erector spinae and abs on side of movement initiate side bending to same side. Gravity pulls trunk further to same side. ES, QL on opposite side act eccentrically to control the rate and distance of gravity produced sidebending. Return to erect posture is produced by concentric activity of the ES and QL on the side opposite the gravity produced side bending.
Line of Gravity (LOG)
Atlanto-Occipital Jt
Lower C-Spine (C3-7)
Thoracic Spine Lumbar Spine Sacroiliac Joint
passes through dens of C2, bodies of T1, T12, S2
Maximal gravitational torque occurs at C5, T8, L3 where apex of each spinal curve are furthest from LOG
LOG: anterior
Moment: flexion
Passive forces: ligamentum nuchae tectorial membrane
Active forces: posterior neck musckes
LOG: posterior
Moment: extension
Passive forces: anterior longitudinal ligament
Active forces: anterior scaleneLongus capitisLongus colli
LOG: anterior
Moment: flexion
Passive forces: posterior longitudinal ligmamentLigamentum flavumSupraspinous ligmanet
Active forces: extensors
LOG: posterior
Moment: extension
Passive forces: anterior longitudinal ligament
Active forces: rectus abdominusIAOEAO
LOG: anterior
Moment: flexion
Passive forces: sacrospinous ligamentSacrotuberous ligamentSacroiliac ligament
Active forces: TA
Excessive Anterior Pelvic Tilt
Excessive Lumbar Lordosis Excessive Thoracic Kyphosis
Excessive Cervical Lordosis
Increased compression of posterior bodiesIncreased L5-S1 disk pressureIncreased lumbosacral anglePotential slippage of L5 on S1
Increased compression of posterior bodiesIncreased compression of facet jtsIncreased disk pressireNarrowing of IV foramenIncreased tension on anterior AF
Increased compression of anterior bodiesIncreased disk pressureIncreased tension on facet capsule and posterior AFDorsal back and scap muscles stretchedALL shortened
Increased compression of posterior bodiesIncreased compression of facet jointsIncreased disc pressureNarrowing of IV foramenIncreased tension on anterior AF
Ab stretchedIliopsoas shortened
ALL stretchedPLL, interspinous, lig. Flavum, lumber extensors shortened
Anterior shoulder girdle and upper Abs shortened
ALL stretchedPosterior spinal ligaments shortenPosterior neck muscles shorten
TEMPOROMANDIBULAR JOINT- Full Fibrocartilage articular disc that is connected to anterior joint capsule
(attachment of superior head of lateral pterygoid)- Posterior disc attached to superior and inferior lamina- Superior lamina = elastic, stretches when disc moves anteriorly and recoils to
move disc posteriorly- Inferior lamina= collagen, tightens when disc moves anteriorly to restrict the
amount of anterior movement and slackens when disc moves posteriorly
Jaw Opening and ClosingStage 1 11-25 mm
between incisors
Anterior rotation of mandibular condyle in fossa and on discDisk does not moveSuperior and inferior lamina are relaxed
Stage 2 40-50 mm between incisors
Anterior rotation and anterior translation of the mandibular condyle over articular eminenceAnterior translation of the articular disc with condyle as condyle moves over articular surfaceSuperior lamina stretchesInferior lamina tightens
Initial Jaw Closing
40-50 mm to 11-25 mm
Posterior rotation and posterior translation of mandibular condyle back into mandibular fossaPosterior translation of articular disc with condyle as condyle returns to fossaSuperior lamina recoils pulling disc posteriorly into fossaInferior lamina slackens as disc moves posterior into fossaLateral pterygoid contractions to control the rate of posterior disc movement
Terminal Jaw Closing
11-25 mm to full closure
Posterior rotation of mandibular condyle in fossa and on discDisc is within fossaSuperior and inferior lamina are relaxed
Tissue Mechanics
Load-Deformation Curve describes the relationship between the amount of stress/force and the amount of strain/deformation
TOE REGION-start of curve-material is slack-small amount of stress produces proportionally more strain
ELASTIC/LINEAR REGION-material is tightening-amount of stress is proportional to amount of strain-when stress is released, material returns to original shape-ability of a material to return to it’s non-deformed starting point define the elastic region of the material
PLASTIC REGION-material is damaged -degree of damage increases as the stress increases-amount of strain/deformation increasing more relative to increase in stress-necking point occurs in plastic region where the degree of material change is so extensive that the amount of deformation remans large with a decrease in stress-material in plastic region is permanently deformed and will not return to it’s original position when the stress is removed
FAILURE is the point where the material completely breaks or ruptures
Stress/Strain curve for elastic material- as stress is applied, material deforms…when the stress is stopped, material returns to original size and shape….work lost during this process to deform the material is not completely recaptured once the forced are removed. Work lost is the area under the curves.
Young’s Modulus of ElasticityE=Stress/StrainDefines stiffness (resistance to deformation)High Young’s Modulus= high stiffnessLow Young’s Modulus= low stiffness
ResilienceResilience is the mechanical work lost during deformationR= work – change in work/workGreater loss of work= less resilience Less work lost= greater resilienceR=1 is perfectly resilient
1 2 3 4
1= good resilience and elastic
2= less resilient but still elastic3= poor resilience, not elastic4= not resilient, not elastic…good Damping
Damping is the opposite of resilience- styrofoam D=1-RToughness is resistance to mechanical failure *amount of energy a material will absorb before it breaks*toughness is not necessarily equal to strength*strength is the magnitude of the force needed to break a materialFragility is the opposite of toughness*Fragile material absorbs little energy before it breaksBrittleness describes materials that deform very little before failure*brittleness is not necessarily related to strength (can be brittle- little formation but strong as in a drill bit)Ductility is the ability of a material to deform progressively in tension without breaking*old bone is more brittle than young bone*young bone is more DUCTILE than old bone because young bone deforms farther when tension stress is applied than old bone.
CONNECTIVE TISSUE PROPER-CT is made up predominantly of collagen fibers-CT is formed from tropocollagen molecules (each has 3 polypeptide chains called alpha units that are wound about each other to form a triple helix)-Tropocollagens are packed end to end and stacked side to side to form collagen fibril-bound together by intra and inter chain bonds or cross-links between lysine and hydroxlysine-cross links also bind fibrils together-cross links contribute to high tensile strength, stability and stiffness of collagen so that collagen fibers with many cross-links are stiffer than collagen fibers with few cross-links
Type I collagen Found in dermis of skin, bone tendon, ligament, Fibrocartilage, and fasciaForms 90% of collagen in body and functions to resist tension and stretching
Type II collagen Found in hyaline cartilage and elastic cartilageFunction is to resist pressure
Type III collagen Found in CT of organs- liver, spleen, lungs, intestinesAlso in blood vessels, nerves and musclesFunction is structural support Important in wound closure
Type IV collagen Found n basement membrane of epithelium Function is to support tissue and act as a filter
Type V collagen Found in basal lamina of smooth and skeletal muscle cells and Schwann and Glia cellsFunctions as support system in these structures
Reticular Fibers- thin, delicate fibers that form lace-like networks around smooth muscle cells, sarcolemma of striate muscle, and endoneurium of peripheral nervesElastic Fibers-occur at varying quantities in CT and contain the protein Elastin; elastic fibers are abundant in some ligaments, large arteries, the trachea, and the dermis of the skin
Connective Tissue CellsCollagen producing cells Fibroblasts MyofibroblastsFibroblasts in CT properChondroblasts/Chondrocytes in cartilageOsteoblasts in boneSkeletal muscle cells in skeletal muscleSmooth muscle cells in blood vessels and some organs
Produce elastic and collagen fibersProduce glycosaminoglycans which form proteoglycans
Have properties of fibroblasts and smooth muscleProduce collagen but contain myofilamentsAbundant at sites of inflammationInvolved in wound closing
Ground SubstanceContains water, GAGs and ProteoglycansGAGs are polymers of disaccharide units
GAGs*attach at one end to a protein core and radiate out from core*arrangement forms a proteoglycan monomer*proteoglycan monomers attach to hyaluronic acid to form a proteoglycan aggregate*GAGs produce negative charge over periphery of proteoglycan monomers which repels adjacent negatively charged monomers as they approach which results in increased tissue stiffness*GAGs of proteoglycans are also hydrophilic so they attract and hold water which delivers nutrients to cartilage and produces compressive stiffness of cartilageMajor GAGs in CTHyaluronic Acid CT proper, cartilage and synovial fluidChondroitin 6 sulfateChondroitin 4 sulfate
hyaline and elastic cartilage, bone large blood vessels, and the nucleus pulposus
Dermatan Sulfate tendon, ligament, Fibrocartilage, nerve, arteries and the dermis
Keratin sulfate cornea, cartilage, nucleus pulposus and annulus fibrosus
Heparin Sulfate basal lamina, aorta, lung, liver, smooth muscle, and endoneurium
Types of Connective Tissue ProperLoose (areolar)
Fibers Few loosely arranged collagen fibersFew reticular and elastic fibers
Cells Fibroblasts, myofibroblasts, macrophages, plasma cells, mast cells, eosinophils, basophils, lymphocytes, fat cells
Locations Superficial fascia, epimysium, myofascia, papillary layer of dermis, tunica adventia of blood vessels
Functions Movement of neurovascular bundles during limb and trunk movementMovement of adjacent muscles to contract individuallyEnlargement of blood vessels
Dense Irregular
Fibers Densely packed collagen bundles arranged in many different directionsSome elastic fibers
Cells Few fibroblastsMacrophages
Locations Dermis of skin, periosteum, perichondrium, joint capsules, capsules around organs, aponeurosis
Functions Resists multidirectional tensile and shear forcesStabilizes jointsProtection
Dense Regular Fibers Densely packed collagen bundles in parallel rows running in same directionCells Few fibroblastsLocations Tendons, ligaments, fascia, aponeurosesFunctions Transmit unidirectional tensile forces
Stabilizes jointsElastic Connective Tissue
Fibers Mostly elastic fibers interwoven among collagen fibersCells FibroblastsLocations Ligamentum flavum, ligamentum nuchael, wall of large arteries, vocal
ligaments of larynxFunctions Dampen high pressure in arteries
Return structures to resting position
Biomechanics of FibersCollagen-shows very little elongation in tension but bends in compression-greater resistance to shear stress than elastic fibers-structures such as tendons that transmit muscular forces and ligaments that provide joint stability are composed mainly of collagen fibers making them strong and stiff in tensionElastic-less stiff than collagen fibers-easily elongate 1.6-2.0 times when tension is appliedTendon/Ligament Stress-Strain Curve-Toe region: collagen fibers on slack so that small stresses produce great deformation as fibers tighten-Linear/Elastic region: collagen fibers tightening and as they tighten greater stress is needed to produce deformation/strain-Progressive failure: some collagen fibers break and then material is damaged and permanently deformed; small increase in stress results in proportionately large deformation
-major failure: most of the collagen fibers are broken and the material is weak and permanently deformed; maintained or decreased stress continues to produce a proportionately large deformation-rupture: all collagen fibers are broken
Tendon/Ligaments response to rate of stress- As rate of applied tension on a tendon/ligament increases, increased stiffness
and decreased elongation result- Suggests that elongation of ligaments/tendons is best obtained by applying
low force for long durations- As magnitude of stress increases with time, tendon/ligament may respond by
adding collagen and increasing the number of cross-links which = increased strength
- Tension on tendons/ligaments at sub-failure levels stimulates fibroblasts to produce new collagen fibers
- Surgically repaired tendons/ligaments show accelerated healing with tension, increased strength of CT scar at repair site and direction of orientation of collagen fibers along the direction of stress
- Additional new collagen fibers results in increased thickness and stiffness of that structure
- Body strengthens tendons/ligaments to match the demands of increased muscle force and increased joint straction that occur with resistive exercise, increased workloads, and with growth
- Stiffness of collagen in tension changes with temperature- cold makes collagen brittle; heat makes collagen extensible; cold with low tensile loads breaks prematurely/heat with low tension elongate farther than normal before breaking
Creep and Load Relaxation -tendons and ligaments are viscoelastic materials and thus show phenomena for creep and load relaxation-creep is an increase in deformation that occurs over time when the load is constant-load relaxation is a decrease in stress over time when the magnitude of the deformation is constant-both creep and load relaxation are the result of reorganization of the collagen and proteoglycans in the material
Tendon and Ligament Injury-high levels of tension applied to tendons and ligaments will not produce failure of all collagen fibers at the same time…there will be microfailure (some collagen fibers fail)-microgailutrs cause some pain and weakness in the tendon/ligament but do not cause instability-where enough collagen is damaged and the tendon passes it’s yield point and there is permanent deformation and noticeable inflammation and joint instability-when all fibers fail= rupture
-laxity of ligaments causes hypermobility which creates a joint instability. This can causes subluxation or dislocation. Hypermobility exposes the joint surfaces to abnormal forces which produce abnormal wear and degeneration leading to pain and inflammation at both the joint and the soft tissues associated with movement at that joint.
Days 2-4 Clot formsInfiltration of macrophages and fibroblastsWeak and unstable type III collagen producedConnection is cellular and fragileStretching tears connection
Days 5-21 Still cellularIncreased collagen productionHigh collagen synthesis and degradationCollagen remodelingIncrease ROM and joint function during rehabTension helps direct collagen fiber direction, increase strength of connection and increase rate of healing and completeness of healing
Days 21-60 Well organized collagenFibrous rather than cellularIncreased strength of connectionIncreased number of stable bonds or cross linksDecreasing tissue response to treatment with time
Days 60-360 Large type I collagen mostlyConnection is mainly collagenStable connectionPoor response to treatment
Tension is important during fibroplasias and consolidation*activates fibroblast production of collagen*controls direction of collagen fiber alignment*produces large collagen bundles*increases scar strength by increasing alignment, amount, size and stability of collagen*increases healing rate and completeness of healing*DAYS 2-21= collagen increases in amount and strength of scar increases*DAYS 21-60= collagen amount levels off and is fairly constant but strength of the scar increases…fiber alignment, large bundles of collagent forming and increase in cross link formation contribute to strength*ligament and tendon replacements may need several weeks before they can be loaded in tension…replacement degenerates initially and then starts to heal. New collagen is produced at this point and tension becomes important to align collagen fibers and strengthen and heal the replacement as in regular tendon/ligament healing.
IMMOBILIZATION~ loss of tissue stiffness and strength~ 7 weeks of immobilization does not affect ligament or capsule if there is no inflammation~ if there is inflammation, adhesions and joint involvement occur within 4 weeks of immobilization
~ prevent and quickly elimate joint inflammation when a joint is immobilized
AGINGStiffness of tendons/ligaments changes with age
Young collagen will elongate more with less force than mature collagen because young collagen is less stiff in tension
As collagen matures, strength and stiffness increase because of increased collagen production and cross-link formation
Advancing age will decrease tensile strength and elasticity of ligaments/tendonsAmount of collagen decreaseNumber of large bundles of collagen decreasesElastic fibers are damagedSlight until 70 years old (decreases 5% up to 50, another 5% from 50-70, 10% after 70)
With aging, these changes are greater for ligaments than for tendons
CARTILAGE Typically avascular Chondrocytes lie in lacuna Ground substance contains H2O, proteoglycans and collagen H20 and proteoglycans give cartilage its hardness and its resistance to compression Collagen provides cartilage’s ability to resist tension
o Compaction of ground substance squeezes water from articular cartilage as it deforms. A s cartilage loses water, proteogylcans are compacted. Repelling negative ionic forces occur among the proteogylcans and the rigidity of the ground substance increases.
o When articular cartilage is unloaded, proteoglycans draw water back into cartilage and return to it’s pre-loading stiffness.
o Proteogylcans interact with H2O to produce stiffness so maintenance of proteoglycans is crucial for normal articular cartilage function.
o Loss of proteogylcans greatly reduces the loading capability of the cartilage.
Hyaline cartilage Fibers: fine network of type II collagen fibersCells: chrondrocytesLocations: costal cartilage, articular cartilage of joints, epiphyseal growth plate, trachea, skeleton of larynx, nasal septum
Elastic cartilage Fibers: abundance of densely packed elastic fibers interwoven among type II collagen fibersCells: chondrocytesLocations: auricle of ear, epiglottis, Eustachian tube, wall of external auditory canal
Fibrocartilage Fibers: dense network of type I collagen fibersCells: chondrocytesLocations: menisci (knee, SC, TMJ, etc), IVD, disk at pubic symphysis, tendo-osseous junctionSuperficial Tangential zone:
Surface 10-20% of articular cartilage
Collagen fibers parallel to articular surface and tightly interwoven
Tough and durableSmooth and slipperyContains proteogylcans within articular cartilage
Middle Zone: Middle 40-60% of articular cartilage Collagen fibers arranged randomly and loosely High concentration of proteoglycans between loosely arranged fibersDeep Zone:Bottom 30% of articular cartilageLarger than in superficial and middle zonesFibers vertical, perpendicular to surface of bonePenetrate into subchondral boneNutrition: Articular cartilage is avascularNutrition and removal of waste comes from joint loading and unloadingLeave with compression, return with unloadingWhen superficial zone is damaged, water and proteoglycans are loast and nutrition to the cartilage is decreased
TENDON STRESS STRAIN RELATIONSHIP TOE REGION- COLLAGEN FIBERS ARE SLACK BUT BEING LOADED IN TESNION AND ALIGNING
IN A DIRECTION TO RESIST TENSION LINEAR REGION- COLLAGEN FIBERS ARE STRETCHING AND BECOMING MORE AND MORE
TENSE AS STRESS INCREASES FAILURE- COLLAGEN FIBERS BREAK AND CARTILAGE TEARS
o TYPE II COLLAGEN IN ARTICULAR CARTILAGE IS LESS DENSE AND FIBERS ARE SMALLER THAN TYPE I COLLAGEN OF LIGAMENTS/TENDONS
o WATER AND PROTEOGLYCANS GREATER IN ARTICULAR CARTILAGE THAN IN LIGAMENTS/TENDONS
o ARTICULAR CARTILAGE TENDS TO FAIL WITHOUT A YIELD POINT AND PLASTIC REGION
Creep and Stress Relaxation Articular cartilage is a viscoelastic material and thus undergoes creep and stress
relaxationo Creep occurs after initial compression and extrusion of watero Further deformation of articular cartilage in time when constant stress is
being applied= creepo Results from collagen and proteoglycans reorganizing to teach an equilibrium
state
o Load relaxation occurs after initial compression and extrusion of water and when stresses are high toward the surface of the articular cartilage and low at the bottom
o With deformation of the articular cartilage remaining constant with time, redistribution of water, proteoglycans and reorganization of collagen occurs
o Even redistribution of stresses from surface to bottom of articular cartilage occurs producing a stress equilibrium state
SYNOVIAL JOINT LUBRICATIONBoundary lubrication Lubricant/Glycoprotein is in surface layer of articular cartilage
With extreme loading conditions, lubricant is extruded to lubricant articular surfaceLast method for protection of articular surface when other methods fail
Hydrodynamic lubrication
Used in joints where opposing joint surfaces are not parallel to each otherSynovial fluid drawn between surfaces as opposing articular surfaces move on each other
Squeeze film lubrication
Used in joints where opposing surfaces are parallel to each otherSynovial fluids tend to pool in concave surface of joint and are squeezed out between the joint surfaces when the joint is compressed
ARTICULAR CARTILAGE WEARInterfacial wear Adhesive wear
Chronic inflammation and disease may result in adherence of the opposing joint surfacesMovement pulls and tears at these adhesive areas causing surface wear
Abrasive wearParticles of cartilage or bone lying between opposing joint surfacesMovement compresses particles between joint surfaces and causes abrasionCrepitus is result of this type of wear
Fatigue wear Repeated stresses of articular cartilage producing tissue failure with timeGenerally occurs with ageCan result from low loads of high reps for a long time as with agingAlso results from high loads of high reps of a short time as with sports or occupations
Impact wear Rapid , very high impact loading of jointFew reps involved
Articular Cartilage Degeneration1. Fibrillation
a. Early articular cartilage degenerationb. Result of fraying of collagen fibers in superficial layer
2. Cavitationa. Cavities form in cartilage between collagen bundles
3. Vertical splittinga. Cavities deepen, clefts in cartilageb. Clefts extend as vertical splits from superficial to deep and even to subchondral bone
4. Continued erosion
a. Final stageb. Cartilage erosion continues in split areas
Articular Cartilage RepairNatural repair Limited due to avascularity
Superficial damage may be repaired but transient (2-3 weeks)Complete thickness tears extend to subchondral bone- blood from subchondral bone fills split and forms fibrous clot- fibrous scar matures and forms Fibrocartilage-like plug- may last for years
Surgical drilling Imitates natural repairModification would be to draw blood from patient and centrifuge it into firbrous paste and spread it over the cavities and splits in articular cartilage rather than drill holes
Cartilage transplant Small amount of healthy cartilage and subchondral bone removed from donor site and ground into pasteNatural growth factors are mixed with paste and it’s spread over damaged areaPatient is NWB for 4wks and uses CPM 6hr/day to allow new cartilage to grow and matureForms hyaline-like articular cartilageGood results
Joint lubricants Hyalgen, orthovisc, synvisc injected into joints for lubrication and to stimulate production of synovial fluidMay also stimulate cartilage growthMainly for osteoarthritis
Fibrocartilage (IVD) contains gel like nucleus pulposus surrounded by 8-10 rings of Fibrocartilage innermost rings have loose arrangement of collagen to allow deformation of
NP middle rings are dense collagen with fibers running in one direction fiber directions of sequential rings are perpendicular outermost rings are dense and show herrningbone pattern which indicates
material is strong in tension and shear tensile strength
o NP- 3kg/m2o Inner rings- 45kg/m2o Middle rings- 53 kg/m2o Outer rings- 80kg/m2
Menisci Fibrocartilage
Superficial collagen fibers are crossed in herringbone pattern to resist tension and shear
Deep fibers run circumferentially to strength menisci in anteriorposteriorly direction tension
With compression, proteogylcans can resist compression but shear and anterioposterior and med/later tension is resisted by collagen
o Function Increase surface area for force distribution which decreases unit
forms on femoral head and tibial condyles Increase surface area for lubrication of condyles Joint proprioception because anterior and posterior horns are
innervatedo Blood supply
Only in peripheral 10-30% in teens and adults Central 70-90% is avascular
Poor healing capacity Stress/Strain Properties and AgingHyaline Cartilage
Tensile properties (strength and elongation) show decline at 40 and decrease markedly after 50 and continues to decline
Compression (strength and compaction) show decline at 40, further decrease at 50 and then levels off
Decrease in compressive forces is less over time than tensileDisc Fibrocartilage
Tensile propertieso Breaking load is least for small cervical disk, intermediate for
thoracic disk and greatest for lumbar disko Breaking load corresponds to sizeo When disk size and strength and calculated, cervical disk is
tronger than lumbar and thoracic is least of allo Elongation greatest in cervical, intermediate in lumbar and
least in thoracico Tensile properties decrease less than 25% with age
Torsional propertieso Breaking load least with cervical disk, intermediate for
thoracic, greatest for lumbaro Torsional breaking load 9x greater for lumbar than cervicalo Torsional breaking load corresponds to disk sizeo When size is considered and strength is calculated, cervical and
lumbar are about the same and thoracic is slightly lesso Angle of twist for failure is highest for cervical, imtermediate
for thoracic and lowest in lumbar
o Angle of twist corresponds with amount of rotational movement allowed in that region of the spine
o Torsional properties decrease by less than 20% with age
BONE Types of bone
o Fibrous- irregular and unorganized pattern of bone, found during embryonic bone formation and development, fracture healing and pathological bone
o Lamellar bone- rows or concentric circles of bones, typical of skeleton Spongy or cancellous bone is formed by internal network of
delicate processes called trabeculae Abundant at ends of long bones in epiphyses Trabeculae align to resist common stresses in region of
bone where they are located Arranged in rows
Dense or compact bone is the solid bone found on the periphery of bone
Thin in region of epiphyses but usually thick in diaphyses of long bones
Consists of concentric circular layers of bone forming osteon or haversion system
Coveringso Covered externally by periosteum except in areas of articular cartilageo Periosteum contains osteogenic cells and is anchored to bone by
Sharpey’s fiberso Internal cavity of bones covered by thin cellular layer called endosteumo Endosteum contains osteogenic cells and bone absorbing cells called
osteoclasts Macroscopic Anatomy
o Ridged CT composed of collagen embedded in ground substanceo Collagen and ground substance form matrixo 65-70% of matrix is composed of inorganic salts most calcium
phosphate and calcium carbonateo 25-30% of matrix is composed of organic compounds of which 95% is
collagen and other 5% are proteoglycans and glycoproteins Osteon is structuralunit of compact bone and lie between peripheral layers of
the external circumferential system and the medullary layers of the internal circumferential system
Periosteum attaches by Sharpey’s fibers to the external circumferential system
Endosteum attaches to internal circumferential system
Interstitial system- area between osteons which is mainly remnants of old osteons after bone remodeling
Haversian canal- central canal that contains blood vessels to provide nutrients to bone cells called osteocytes and remove waste products, lymphatic channels and fine nerve fibers
Volkmanns canal- run transverse to haversian canals and transport blood vessels, lymphatics, and fine nerves to the haversian canals from nutrient foramen that lies on the surface of each bone
Each haversian canal is surrounded by rings of calcified bone called lamella and between the rings are bubble like structures called lacuna that contain more osteocytes
Osteogenic cells arise from embryonic mesenchymal cells, from periosteum and endosteum of mature bone and differentiate into osteoblasts
Osteoblasts are immature bone cells that secrete collagen and non-calcified ground substance called osteoid and become osteocytes when the surrounding matrix is calcified
Osteoclasts are large multinucleated cells that remove calcified bone and osteoid and are important in bone growth, bone remodeling, fracture healing and maintain blood calcium levels.
BONE REMODELING Remodeling during bone growth:
o Surface bone remodeling involves the simultaneous process of depositing new bone in one area by osteoblasts and the reabsorption of bone in a different area by osteoclasts
o Cylindrical bones- osteoblasts in subperiosteal area deposit bone while in the same region, osteoclasts in the subendosteal area reabsorb it
o Conical bone- osteoblasts in subendosteal area deposit bone and osteoclasts in subperiosteal area reabsorb it
Internal bone remodeling:o Starts with removal of old lamellar bone by osteoclasts that bore out
through longitudinal cylindrical cavity= cutting cone (relatively long, reaches diameter of new osteon)
o Osteoclasts in cutting cone along with blood vessels, perivascular connective tissue and numerous cells in mitosis that appear to give rise to osteoblasts
o Osteoblasts deposit collagen and osteoid (uncalcified bone) along walls of cone and the cutting cone becomes = closing cone (refilled from outside in with concentric circular layers of lamellar bone until the haversian canal remains)
Bone remodeling throughout life:o Old osteons and interstitial bone are removed and replaced throughout
lifespan
o Reasons for bone remodeling- Removes damaged bone from microfactures due to bone fatigue
or strain Replenishes osteocytes and maintains organic and inorganic
compounds of bone Adapts bone to long term changes in stress Makes calcium stored in bone available to body
BONE FRACTURES types of fractures
☼ complete- transects entire bone☼ incomplete- penetrates through only part of the bone☼ simple or closed- surrounding tissue intact☼ comminuted- splintering of bone☼ compound- bony ends are displaced and disrupt surrounding tissue and
skin fracture site
☼ depends on distribution of spongy and compact bone in an area and the type of load applied
☼ spongy bone is weaker than compact bone so more prone to fractures (spongy- epiphyses, tuberosities; compact- shaft)
☼ spongy and compound bone are weaker in tension than compression so the areas receiving tension are more susceptible to fracture than those receiving compression forces
☼ regional compression strength difference shaft is strongest ends of bones are weaker than shaft (more spongy, less
compact) except in portion 1 of ulna (thick olecranon is mainly compact bone)
causes of fractures☼ trauma☼ pathologies
osteoporosis- disorder characterized by decreased mass of spongy and compact bone but no abnormality in composition of bone
osteomalacia- reduced mineralization of bone during remodeling which results in softer bone and appears to be associated with lack of vitamin d
pagets disease (osteitis deformans)- metabolic disorder characterized by marked bone reabsorption followed by the formation of patches of new bone that lacks the strength of normal bone even through it is thick
osteogenesis imperfect (brittle bone)- inherited disorder resulting in abnormal collagen syntrhesis and absorption making bone brittle
Bone healing process1. Fracture results in local hematoma due to ruptured blood vessels2. Blood clot develops3. Capillaries grown in clot and form vascular network; connective
tissue grows into granulation tissue; macrophages remove dead tissue and osteoclasts remove bone fragments
4. Granulation tissue becomes dense CT where hyaline cartilage and Fibrocartilage develop- fibrocartilagenous callus- divided into large external callus and small internal callus
5. Disruption of periosteum and endosteum at fracture site stimulates osteogenic cell activity
6. Osteoid calcified and bony callus of fibrous bone is formed- not organized along mechanical lines of stress but layers are aligned in direction of cap
7. illaries8. Time and return of function allow bony callus to be remodeled and
fibrous bone is converted to lamellar bone Movements that produce rotation and traction and fx site should be avoided
during early healing as they displace bony ends and can prevent union of bones
Exercises that reflect functional activities will strain fx callus to direct remodeling so that remodeled bone aligns to resist appropriate mechanical loads
Factors that effect bone Exercise
strenuous exercise results in muscle fatigue which decreases shock absorption capability of muscle and produces altered movements and abnormal loading of the bone
abnormal loading changes force distribution and strain pattern on the bone which results in microfailures and possibly fractures
jogging compression forces on tibia at toe strike during jogging 2x greater than
at heel strike during walking tensile forces on tibia from toe strike to toe off are 4 greater than from
foot flat to heel off during walking immobilization
1% loss in bone mass per week Bone decreases in strength, stiffness and toughness
Bone stress and strain Compact and spongy bone
Compact is stiffer and stronger than spongy in compression, tension and shear Compact is most resistant to compression, then tension, then shear Trabeculae of spongy bone and osteons of compact bone are aligned to resist most
frequently occurring stress Wolff’s law- bone is deposited where needed to resist stress and absorbed where not
needed … seems to apply to all CT as well During ADLs, long bones of body are subjected to multiple stresses and strains by muscle
action, gravity or resistive loads Activities stress bones in tension, compression, bending, and torsion- because the long
bones differ in shape and size, the ability to resist these forces differs in each bone Breaking load- amount of force needed to break bone without consideration of the
size of that bone Strength- amount of force need to break bone relative to area of the bone Elongation, contraction, deflection, angle of twist all describe deformation or
strain
TENSIONo Strength: thin long bone is stronger in tension than thicko Strain: think long bones elongate more than thick when loaded in tension
COMPRESSIONo Thick long bones are stronger in compression than thin long boneso Compression strength is directly related to CSA of a boneo Larger CSA, greater resistance to compressiono Thin long bones compress more than thick long boneso Degree of compression of long bone is inversely related to CSAo Smaller CSA, greater amount of compression
BENDINGo Thick long bones stronger in bending than thin long boneso Directly related to CSA of bone- larger CSA, greater resistance to bendingo Thin long bones bend more than thick long bones o Degree of bending of a long bone is inversely related to CSA- less CSA, greater
amount of bending displacement TORSION
o Thick long bones stronger in torsion than thin long boneso Directly related to CSA, larger CSA- greater resistance to torsiono Thin long bones twist more than thick long boneso Inversely related to CSA – smaller CSA, greater angle of twist
Aging max strength in men and women 20-29 y/o decreases slowly in both genders 30-39 y/o before 30, osteoblasts more active than osteoclasts= increased thickness of cortical
bone
after 40, osteoblasts decrease but osteoclasts are unchanged- slow decrease in cortical bone thickness
less than 50, mechanical properties of bone are similar in male and females but males tend to have more bone than females
after 50, strength and amount of trabecullar bone decreases more rapidly in females than in males
after 50, tensile strength 75% of max, compressive strength 85% of max, bending strength 75% of max, torsional strength 85%
biomechanical properties and aging in vertebrae- tension
o lumbar tensile breaking load 4x greater than cervicalo lower thoracic breaking load 2x more than upper thoracic…both less than
lumbar and greater than cervicalo breaking load is a function of size o considering size, tensile strength is very similar among vertebraeo elongation is also similar among the vertebraeo with age, decreases in tensile properties are less than 20%
tensile breaking load down 20% tensile strength down 10% tensile strain down 15%
- compressiono lumbar breaking load 2x cervicalo lower thoracic breaking load 1.5x upper thoracic but middle thoracic is
only .15x greater than upper thoracico all thoracic breaking loads are less than lumbar and greater than cervicalo BL is function of sizeo Considering size- tensile strength of cervical vertebra is greatest, then
thoracic, then lumbaro Cervical strength 2x lumbar but thoracic are only about 20-25% greater than
lumbaro Contraction is greatest in cervical and least in lower thoracic and lumbar but
difference is only 30%o With age, decreases in compressive properties are 40-50%
Breaking load down 50% Strength down 45% Strain down 40%
- Torsiono Lumbar torsional BL 4x > than upper thor but only 35% > than lower thoro Lower thor BL 60% > than upper thor and middle thor BL is 45% > than
upper thoro All thor BL are less than lumbar and differences are a function of sizeo Considering size, torsional strength of upper thor is >, strength very similar
along thor and lumbar vertebrao Angle of twist is > in upper thor and prob cervical and least in lumbaro Upper and middle thor angles are 2x greater than that of lumbar but lower
thor is 60% of lumbar