Vermont Medicaid BannerThe countdown has begun. The new Timely Filing Guidelines effective date is...
Transcript of Vermont Medicaid BannerThe countdown has begun. The new Timely Filing Guidelines effective date is...

1
Vermont Medicaid Banner Please share the information contained in the Banner with all staff members. To access Full Banners, please visit: http://vtmedicaid.com/#/bannerMain
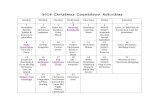
December 28, 2018 Reminder New Timely Filing Guidelines Effective 02/01/2019
The countdown continues. The new Timely Filing Guidelines effective date is rapidly approaching. There are only 5 weeks left to get all your outstanding timely filing reconsiderations in prior to the 02/01/2019 effective date. DVHA highly recommends having your reconsideration packets to DXC no later than 01/15/2019 to allow time for review and processing.
To recap, the Agency of Human Services (AHS) will be changing our timely filing guidelines. This change assures compliance with federal regulations at 42 CFR §§ 447.45 (d). The new timely filing guidelines will become effective for timely filing reconsideration requests received on or after 02/01/2019. More detailed information on the new timely filing guidelines can be found here: http://dvha.vermont.gov/news-info.
Provider Management Module (PMM) Training Training on the Provider Management Module (PMM) will begin in the Spring of 2019. We will be offering several different training options that include, live in person trainings, live webinars, recorded training sessions and a provider instructions manual. We can help you select which one is right for you and your team. Contact your provider relations representative with questions on training. We look forward to training with you. Happy Holidays!
December 21, 2018 Verify Your Provider Information Now
Did you know that in 2019 the Online Provider Management Module (PMM) will reduce the provider enrollment time frame from the average of 120 days to below 45 days? In addition, PMM will simplify data entry for providers from a paper-based process to a web-based portal. In order to help us make the transition smooth please make sure that all existing provider information is up to date, so the existing data can be transferred accurately for you.

2
To verify your existing provider information, visit http://www.vtmedicaid.com/#/home, click on Member Services and select Provider Lookup in the drop-down menu.
If you notice a discrepancy, use the Vermont Medicaid Provider Information Change Form to update your information. This form can be found at http://www.vtmedicaid.com/#/provEnrollDataMaint. Mail the form to DXC Technology, Attn: Provider Enrollment, PO Box 888, Williston, VT 05495, fax to 802.878.3440, or Email to: [email protected].
Reminder New Timely Filing Guidelines Effective 02/01/2019 The countdown has begun. The new Timely Filing Guidelines effective date is rapidly approaching. There are only 6 weeks left to get all your outstanding timely filing reconsiderations in prior to the 02/01/2019 effective date. DVHA highly recommends having your reconsideration packets to DXC no later than 01/15/2019 to allow time for review and processing.
To recap, the Agency of Human Services (AHS) will be changing our timely filing guidelines. This change assures compliance with federal regulations at 42 CFR §§ 447.45 (d). The new timely filing guidelines will become effective for timely filing reconsideration requests received on or after 02/01/2019. More detailed information on the new timely filing guidelines can be found here: http://dvha.vermont.gov/news-info.
Reminder: Hospice Billing The Department of Vermont Health Access (DVHA) and DXC Technology would like to remind providers that when billing Hospice services, it is required that claims are billed monthly, to ensure accurate and efficient claims processing. Hospice services should not be billed weekly or bi-weekly and may result in delayed process times and/or denials.
Fax Over Internet Protocol (FoIP) The Department of Vermont Health Access, Clinical Operations Unit recently implemented an electronic system to receive prior authorization requests. This means a new way of receiving faxes, commonly referred to as Fax Over Internet Protocol (FoIP). Below are links containing additional information, which cover:
* FoIP benefits
* Instructions on how to report fax issues
http://dvha.vermont.gov/for-providers
http://www.vtmedicaid.com/#/resources
Closed for Christmas Day and New Year’s Day The DVHA and DXC Technology offices will be closed on Tuesday, December 25, 2018 in observance of Christmas Day and on Tuesday, January 1, 2019 in observance of New Year’s Day.
December 14, 2018 Reconsideration Request Reminder
In 2018, DXC has returned approximately 61% of the Reconsideration Requests received, to the requestor. The top three reasons your requests are being returned are: DXC did not receive your request within 30 days of your Remittance Advice, mandatory documentation missing, and the request does not meet the criteria for a reconsideration. Providers are reminded to review section 1.2.7 of the Provider Manual prior to submitting a Reconsideration Request. If the required criteria for

3
a Reconsideration Request is not met, the request will be returned to the requestor and will not be forwarded to a DXC reviewer. In addition, providers are reminded that corrected claims should not be sent as Reconsideration Requests and will be returned. To avoid unnecessary delays, please send corrected claims through the normal claims process. If you have any questions regarding the Reconsideration Request process, please contact the Provider Help Desk at 800-925-1706 (in-state) or 802-878-7871 (local and out-of-state).
Provider Management Module (PMM) Roll Out Ending the year means we are getting closer to rolling out access to the online Provider Management Module (PMM). The Department of Vermont Health Access (DVHA), in collaboration with DXC, will be working together to ensure all providers will have the PMM module that will allow providers the capabilities to enroll, revalidate and make changes to existing provider data. Providers will no longer be required to mail paper enrollment applications and supporting documentation. Online enrollment and revalidation will decrease the amount of time it currently takes to enroll or revalidate with Vermont Medicaid.
Resource-Based Relative Value Scale Update The Department of Vermont Health Access (DVHA) is updating the discounting policy for non-physician services under Resource-Based Relative Value Scale (RBRVS) payments. DVHA last updated the discounting policy for non-physician RBRVS services on August 1, 2017 to include both Nurse Practitioner and Physician Assistants and to generally align with Medicare policy. For dates of service on or after December 1, 2018, DVHA will adjust this discounting policy so that the 10% reduction is only applied on codes from the Medicare physician fee schedule, and not the entire billed claim.
December 7, 2018 Reminder: New Timely Filing Guidelines Effective 02/01/2019
The Agency of Human Services (AHS) will be changing our timely filing guidelines. This change assures compliance with federal regulations at 42 CFR §§ 447.45 (d). The new timely filing guidelines will become effective for timely filing reconsideration requests received on or after 02/01/2019. More detailed information on this change can be found here: http://dvha.vermont.gov/news-info.
Prescription Assistance Programs There are two Prescription Assistance programs to help Vermonters pay for prescription medicines. VPharm pays for Medicare Part D plan premiums and prescription co-pays and requires participating seniors to be enrolled in Medicare Part D. Healthy Vermonters offers discounted prescriptions without monthly premiums and does not require participation in Medicare Part D. Providers should direct their patients to call Member Services at 800.250.8427 or visit http://www.greenmountaincare.org/ to print an application.
Server Maintenance – Sunday, December 9, 2018 The Provider Web Portal server maintenance is scheduled from midnight to 8:00AM on Sunday, December 9, 2018. During this time, all Provider Web Services will be unavailable. Providers wishing to check eligibility, receive other insurance information or determine if service limits have been reached are advised to use the automated Voice Response System (VRS). The VRS can be accessed by dialing 802.878.7871, option 1 and then option 1 again.

4
November 30, 2018 Billing Interpretive Services for Multiple Recipients During Same Session
When billing for sign language or oral interpretive services for each 15 minutes provided to multiple recipients during the same group therapy session, providers are instructed to bill procedure code T1013 on multiple claims with the appropriate modifier to indicate how many patients were served. The first claim should report T1013 without a modifier and include the total number of units for all patients served within the group session, as well as the charge amount for the total session. Additional claims should report T1013 with one of the appropriate modifiers listed below with 1 unit and no charge amount.
Appropriate Modifiers on claims 2-6: UN – 2 patients served UP – 3 patients served UQ – 4 patients served UR – 5 patients served US – 6 or more patients served
Please see section 9.8.3 of the provider manual for further clarification. This information can be found here, http://www.vtmedicaid.com/assets/manuals/VTMedicaidProviderManual.pdf.
Validate Your Provider Information Now The Department of Vermont Health Access (DVHA), in collaboration with DXC Technology, will be rolling out access to the online Provider Management Module (PMM) beginning in the Spring of 2019. For a smooth transition for all involved, it is important to be prepared by validating your existing provider information to make sure it is current. This includes addresses, group affiliations, and contact information. Your existing data will be converted on your behalf. We look forward to working with you on this exciting endeavor.
To verify your existing provider information, visit http://www.vtmedicaid.com/#/home, click on Member Services and select Provider Lookup in the drop-down menu.
If you notice a discrepancy, use the Vermont Medicaid Provider Information Change Form to update your information. This form can be found at http://www.vtmedicaid.com/#/provEnrollDataMaint. Mail the form to DXC Technology, Attn: Provider Enrollment, PO Box 888, Williston, VT 05495, fax to 802.878.3440, or email to: [email protected].
November 16, 2018 Closed for Thanksgiving
The DVHA and DXC Technology offices will be closed on Thursday, November 22, 2018 and Friday, November 23, 2018 in observance of the Thanksgiving holiday.
November 9, 2018 E0562 Heated Humidifier
Effective 12/1/2018, E0562 Heated Humidifier, used with positive airway pressure devices, will be added to the capped rental program. The humidifier will require a RR or NU modifier. The E0562RR will be reimbursed in 10 monthly installments. The E0562NU will be reimbursed in one installment for replacement humidifiers.

5
The humidifier along with the positive airway pressure device rentals recognize a three-month trial period, and months four through ten require prior authorization for completion of the capped rental period once medical necessity has been determined.
NDC Required for HCPCS/CPT Codes Providers are reminded that a valid NDC associated with the HCPCS/CPT code must be present on the claim when billing for a physician administered drug. For dates of service on/after 1/1/2019, this rule will also apply to 340B providers and drugs purchased with a 340B discount.
To assist you in determining the validity of an NDC, a searchable list is available on the DVHA website at http://dvha.vermont.gov/for-providers/drug-coverage-lists-1. This list is updated quarterly. Appearance on this list does not guarantee payment, and prior authorization may apply. Any claims submitted for physician administered drugs without a valid NDC will result in claim denials.
This policy is effective for professional claims billed on the CMS-1500 and hospital outpatient claims billed on the UB-04. Straight Medicaid as well as crossover (dual-eligible) claims will follow the policy. Please refer to section 10.3.38 of the Provider Manual for additional information on NDC billing requirements.
Provider Management Module Facts Did you know…
• that the Online Provider Management Module (PMM) will reduce the provider enrollment time frame from the average of 120 days to below 45 days?
• that PMM will simplify data entry for providers from a paper-based process to a web-based portal?
• the base system of the PMM module is currently being configured to fit Vermont’s specific requirements and needs?
• that we will be providing training to all providers starting Spring 2019? • that if you validate and update your existing provider information now, then all your existing
data will be converted on your behalf?
Server Maintenance – Sunday, November 11, 2018 The Provider Web Portal server maintenance is scheduled from midnight to 8:00AM on Sunday, November 11, 2018. During this time, all Provider Web Services will be unavailable. Providers wishing to check eligibility, receive other insurance information or determine if service limits have been reached are advised to use the automated Voice Response System (VRS). The VRS can be accessed by dialing 802.878.7871, option 1 and then option 1 again.
Closed for Veterans Days The DVHA and DXC Technology offices will be closed on Monday, November 12, 2018 in observance of Veterans Days.
November 2, 2018 ACO Prior Authorization
Under the Vermont Medicaid Next Generation ACO program, prior authorization requirements were waived in 2018 for all Vermont Providers for ACO-attributed members and services. Due to technological limitations, Medicaid’s claims-processing system continues to look for a prior authorization before it pays claims for certain services (additional units of services, additional

6
therapy visits, additional months of equipment rental for DME, etc.). To reduce administrative burden for this cohort of members, DVHA has created a shorter form to collect the information necessary for payment. This form may be used if the member and service in question are attributed to the ACO. This form does not require additional clinical documentation to be attached along with the request. The form and additional information can be found at http://dvha.vermont.gov/for-providers/clinical-coverage-guidelines. Please note, this short form is temporary and will only be in use until January 1, 2019 when the claims processing system is anticipated to be modified and documentation will not be needed (with minor exceptions). Further guidance to follow.
GC Modifier and Prior Authorization Requests The Department of Vermont Health Access, along with DXC Technology, continue to review opportunities to reduce the number of claims that suspend. A recent review was conducted on the use of the GC modifier. It has been determined that claims submitted using the GC modifier do not require review of the modifier/procedure combination. Due to this requirement being lifted, providers requesting prior authorization for applicable services, may or may not see the GC modifier included on their Notice of Decision approvals. Please note that the presence of the GC modifier on your Notice of Decision approval, or lack thereof, will not affect the processing of your claim. Providers should continue to bill their claims with the appropriate coding.
Unspecified Diagnosis Code List Review The Department of Vermont Health Access (DVHA) is continuing its review and edits of the unspecified code list. As a reminder, many of these diagnosis codes are specific to laterality. If there is a choice for left, right, bilateral, or unspecified please choose the most specific code outlined in the medical record. If the provider did not specify in the medical record, please reach out to the provider to specify and amend the record. A banner will be released when the revised list is complete and it will provide a new effective date.
Modifier 50 Allowed with CPT 76641 & 76642 Effective 8/1/2018, CPT codes 76641, Ultrasound, breast, unilateral, real time with image documentation, including axilla when performed; complete and 76642, Ultrasound, breast, unilateral, real time with image documentation, including axilla when performed; limited, will allow the use of modifier 50 (bilateral) on the claim. This does not apply to any other radiology CPT codes.
Announcement of Enhanced Provider Manuals The Department of Vermont Health Access (DVHA) in collaboration with DXC Technology is pleased to announce that in December 2018, enhanced Provider Manuals will be found at http://www.vtmedicaid.com/#/home. Stakeholders highlighted the need for increased usability of the manuals. DVHA listened to and addressed the concerns. Practitioners and other stakeholders were key partners in the Provider Manuals upgrade process. The upgraded manuals collection includes distinct manuals. 10 of the manuals are geared toward specific service area(s). The areas are: Applied Behavior Analysis, Mental Health and Substance Abuse Services; Dental; Durable Medical Equipment; Federally Qualified Health Centers & Rural Health Clinics; Home Health Agency, Assistive Community Care Services and Enhanced Residential Care; Pharmacy; Primary Care Provider; Physical Therapy, Occupational Therapy and Speech Language Therapy; Non-Emergency Medical Transportation and Vision. The General Provider Manual and the General Billing and Forms Manual contain information that is useful for all Practitioners and interested parties. Thanks to all the participants who lent their invaluable expertise.

7
Telemedicine Testimonial Recently, staff from DVHA’s Provider & Member Relations and Quality Improvement Units have been talking with local providers about their experiences offering services via telemedicine technology. We want to learn more about the benefits and challenges for them as providers and for their clients. The challenge of understanding the technology, researching the options and implementing the secure connection that complies with HIPAA is one that we’ve heard more than once. The benefits associated with convenience, flexibility and continuity of care stand out as well. As one local provider who is using telemedicine in his practice stated:
“Providers and patients are still getting familiar with the ins and outs of giving and receiving psychotherapy using live video. There are many good reasons to offer telehealth to patients as an option. It’s accessible and reimbursable. Sometimes it just takes one patient to want to try it and that starts the ball rolling. Many will always prefer in-person services. The more options the better.”
If you are interested in learning more about this topic in the future, please consider bookmarking this link to a new section on the DVHA website: http://dvha.vermont.gov/telehealth?portal_status_message=Changes%20saved.
October 26, 2018 Online Provider Management Module
As you know, the Department of Vermont Health Access (DVHA), in collaboration with DXC, will be rolling out access to the online Provider Management Module (PMM) beginning in the Spring of 2019. This module allows providers to enroll, revalidate and make changes to existing provider data. Providers will no longer be required to mail paper enrollment applications and supporting documentation. Online enrollment and revalidation will decrease the amount of time it currently takes to enroll or revalidate with Vermont Medicaid.
New Timely Filing Guidelines Effective 02/01/2019 The Agency of Human Services (AHS) will be changing our timely filing guidelines. This change assures compliance with federal regulations at 42 CFR §§ 447.45 (d). The new timely filing guidelines will become effective for timely filing reconsideration requests received on or after 02/01/2019. More detailed information on this change can be found here: http://dvha.vermont.gov/news-info.
DXC Technology Email Address Change Effective immediately, the domain name for DXC Technology emails has changed from @hpe.com to @dxc.com. When corresponding with DXC Technology please use the @DXC domain name going forward. Emails sent to @hpe.com will not be received.
It’s Time to Get Your Coding Books The Department of Vermont Health Access (DVHA) would like to remind practitioners to prepare for 2019 by purchasing new coding books for their practice or updating subscriptions. These resources provide all the codes, descriptions, guidelines, annotations, reference tables, colored illustrations and coding tips for speed and accuracy. Give your practice the boost it needs with more accurate coding upon first claim submission.

8
October 12, 2018 Provider Representative Coverage Changes
Effective immediately, the following changes have been made to the areas of coverage for our provider representatives. Unless otherwise specified, hospitals and facilities are to use the representatives for their county:
Margaret Haskins (802.857.2963; [email protected]): Grand Isle, Franklin, Orleans, Essex, Chittenden, UVMMC.
Nora Williams (802.857.2957; [email protected]): Rutland, Bennington, Windham, DHMC.
Jennifer Hanfield (802.857.2994; [email protected]): Addison, Washington, Caledonia, Orange.
Misty Griffith (802.857.2965; [email protected]): Lamoille, Windsor, Out of State.
A detailed map, including Provider Representative Contact information and territory, is available at: http://vtmedicaid.com/#/manuals.
Multiple Units on Surgical Codes Require Notes for Payment When billing multiple units for the same service, notes are required for payment to be considered. This includes claims 1) with the same code billed without a modifier and then again with modifier 59 on a separate detail, and 2) multiple units of the same code billed on one detail. If you receive a denial requesting notes, resend the information through the normal claims process. Please note that a reconsideration form is not necessary or appropriate and attaching one will result in your claim being returned to you. Be sure to include the original RA with your claim as proof of timely filing if necessary. To avoid unnecessary denials, submit these types of claims on paper with the notes instead of electronically.
Server Maintenance – October 14, 2018 The Provider Web Portal server maintenance is scheduled from midnight to 8:00AM on Sunday, October 14, 2018. During this time, all Provider Web Services will be unavailable. Providers wishing to check eligibility, receive other insurance information or determine if service limits have been reached are advised to use the automated Voice Response System (VRS). The VRS can be accessed by dialing 802.878.7871, option 1 and then option 1 again.
September 28, 2018 Telemedicine: Business Efficiency and Customer Satisfaction
Did you know that the adoption of telemedicine technologies in substance use disorder treatment has been found to be far lower than other fields in recovery care? At the same time, client interest in telemedicine techniques is quite high. Substance use disorder treatment providers may want to consider telemedicine as a path to improving efficiency within their business model, as well as to improving client satisfaction. One study found an 80% completion rate for a telehealth outpatient substance use disorder treatment program, which is nearly double the completion rate of 41% for traditional outpatient treatment. Some of the studies have even found that people prefer telehealth because of the convenience and increased confidentiality. Vermont Medicaid reimburses for these services as long as they are clinically appropriate and within the Medicaid provider’s licensed scope of practice.

9
September 14, 2018 Telemedicine: Improving Access to Substance Use Disorder Treatment
Telemedicine involves the use of electronic communications and software to provide clinical services to clients without an in-person visit. Diversifying treatment options for substance use disorders with telehealth is something you may want to consider as a supplemental way to ensure client recovery and well-being. Telemedicine can not only increase client access to treatment options, but also improve the quality and frequency of care. Telehealth can redistribute the knowledge of specialists over a larger geographic area and improve access no matter the location. Vermont Medicaid reimburses for these services as long as they are clinically appropriate and within the Medicaid provider’s licensed scope of practice.
September 7, 2018 Approved Carrier Codes
Providers are reminded when submitting claims to Vermont Medicaid with other insurance on the claim, that Vermont Medicaid/DVHA has a list available of approved carrier codes. Carrier codes not on the approved list that are submitted on a claim will cause the claim to be denied. To review the list of approved codes please visit the following website: http://www.vtmedicaid.com/assets/resources/CarrierCodeRpt.pdf.
Annual Depression Screening Effective for dates of service on/after 10/1/2018, the annual depression screening code (G0444) will be limited to one unit per calendar year per VT Medicaid member. Other codes are available for more frequent mental health assessments. Please refer to your coding books for options.
Telemedicine and Billing for Substance Use Disorder Treatment Are you hearing more about telemedicine lately? Telemedicine is the provision of health care services over a distance through the use of telecommunications technology. This type of service is reimbursable through Vermont Medicaid as long as it is clinically appropriate and within the provider’s licensed scope of practice. This includes the provision of substance use disorder treatment. Vermont Medicaid has an established telemedicine Place of Service (POS) code 02 (Telehealth) for use by practitioners providing telehealth services from off site. Modifier GT is not allowed on physician claims, but modifier GT is to be used on facility claims to identify telemedicine services. Physician claims will be identified by the use of POS code 02.
Server Maintenance – September 9, 2018 The Provider Web Portal server maintenance is scheduled from midnight to 8:00AM on Sunday, September 9, 2018. During this time, all Provider Web Services will be unavailable. Providers wishing to check eligibility, receive other insurance information or determine if service limits have been reached are advised to use the automated Voice Response System (VRS). The VRS can be accessed by dialing 802.878.7871, option 1 and then option 1 again.
August 31, 2018 Update on the Unspecified Diagnosis Code List
The Department of Vermont Health Access (DVHA) reviewed all diagnosis codes containing the word “unspecified”. A majority of these diagnosis codes are specific to laterality. If there is a choice for left, right, bilateral, or unspecified: claims with the unspecified code for billed services on or after 10/1/2018 will be denied.

10
As previously indicated, DVHA has been reviewing comments from providers per the Global Commitment Register (GCR) proposed policy 18-021: Unspecified Diagnosis Code List Update. The updated unspecified diagnosis code list will be posted online for providers to view no later than 9/1/2018. http://dvha.vermont.gov/for-providers/claims-processing-1.The edit will be put into the claims processing system on 10/1/2018 and will use the new list. Please contact your DXC Provider Representative if you have additional questions or comments.
Electronic Breast Pump Coverage Effective August 1, 2018, the following changes were made to electric breast pump coverage. New mothers, within 60 days post-partum, who expect to be away from their infant on a regular basis, such as returning to work or school, are eligible to receive a personal use double electric breast pump (E0603) with a prescription from their provider. E0603 will be reimbursed at $178.00/pump and is limited to one new pump every three years. Hospital-grade electric breast pumps (E0604) will only be available for rental, and the rental rates will remain at $139.03. Prior Authorization requirements for E0604 will be waived for the first month of rental but will be in place for the second and subsequent months of rental. The following supply codes will be covered for hospital grade breast pumps (E0604) only and can only be billed once per rental period: A4281-A4286. Please review updated Clinical Coverage Guidelines found at http://dvha.vermont.gov/for-providers/clinical-coverage-guidelines.
Telemedicine and Substance Use Disorder Treatment Did You Know: Substance use disorder treatment providers are eligible to receive reimbursement of existing Medicaid covered services outside a facility as long as it is clinically appropriate for delivery through telemedicine and within the Medicaid provider’s licensed scope of practice. This includes the provision of clinically appropriate substance use disorder treatment. Telemedicine does not include the use of audio-only telephone, email or facsimile. Please see the Provider Manual for Provider Eligibility Requirements and Billing Rules. This additional information can be accessed here: http://www.vtmedicaid.com/assets/manuals/VTMedicaidProviderManual.pdf, section 10.3.54, page 105.
Closed for Labor Day The DVHA and DXC Technology offices will be closed on Monday, September 3, 2018 in observance of Labor Day.
Reminder: Current Forms Are Required Vermont Medicaid regularly updates its forms and applications to reflect current state and federal requirements. All provider paperwork, including enrollment applications and forms, adjustment forms and refund forms, submitted on outdated versions, will be returned. Providers are encouraged to always check for the most current forms on the Vermont Medicaid website. http://www.vtmedicaid.com/#/home
August 17, 2018 Closed for Bennington Battle Day
The DVHA and DXC Technology offices will be closed on Thursday, August 16, 2018 in observance of Bennington Battle Day.

11
August 3, 2018 Unspecified Diagnosis Code – Updates
Due to the feedback from providers, regarding certain “unspecified” diagnosis codes may have been denied as of 7/1/2018, the Department of Vermont Health Access (DVHA) has temporarily removed this edit from the claims processing system – effective 7/19/2018. DVHA is actively reviewing comments from providers and will update the list of diagnosis codes when this review has been completed. The Global Commitment Register (GCR) proposed policy 18-021: Unspecified Diagnosis Code List Update is open for public comment through 8/23/2018. The updated list will be posted online for providers to view no later than 9/1/2018. The edit will be put into the claims processing system on 10/1/2018 and will use the new list.
If you had claims deny due to these diagnosis codes on claims billed between 7/1/2018 and 7/18/2018, please revisit the clinical note for the service and choose a more specific code if one is available. If a more specific code is not available, please resubmit your claim for processing. Please contact your DXC Provider Representative if you have additional questions or comments.
Childbirth Education Classes - Reimbursement Rate Change On or after 8/1/2018, providers who offer Childbirth education classes will have an increase in the reimbursement rate for code S9436. Childbirth education classes (S9436) will now be limited to bill one unit per nine months, regardless of the number of classes in the series, with a maximum reimbursement of $125. Providers should use the date of the first class as the date of service on the claim – not a span of days. Please review the fee schedule at http://www.vtmedicaid.com/#/feeSchedule.
FQHC/RHC Change in Scope Process The Department of Vermont Health Access has published the Change in Scope Process for Federally Qualified Health Centers and Rural Health Clinics. Information can be found in the VT Medicaid Provider Manual under section 10.3.24 Scope-of-Service Related Encounter Rate Adjustments. http://www.vtmedicaid.com/assets/manuals/VTMedicaidProviderManual.pdf
July 27, 2018 Modifier Required for 340B Drugs
Providers are reminded that all drugs purchased with a 340B discount must be billed to Vermont Medicaid with modifier UD or JG to indicate a 340B drug. If you are carved-in to the Vermont 340B program, and the claim does not have modifier UD or JG to indicate a 340B drug, the NDC must be present so the claim can be processed under the Drug Rebate Program.
Reminder – If the HCPCS code requires a Prior Authorization (PA), the UD or JG modifier must be included with the HCPCS codes on the PA request form. Failure to include the UD or JG modifier when appropriate will result in denial of the PA request and/or the resulting claim.
This policy is effective for professional claims billed on the CMS-1500 and hospital outpatient claims billed on the UB-04. Straight Medicaid as well as crossover (dual-eligible) claims will follow the policy.
Please refer to the 340B Medicaid Carve-In Program Manual located at http://www.vtmedicaid.com/assets/forms/340BMedicaidCarveInProgram.pdf for additional information.

12
NDC Required for HCPCS/CPT Codes Providers are reminded that when billing for a physician administered drug, not purchased with a 340B discount, a valid NDC associated with the HCPCS/CPT code must be present on the claim. To assist you in determining the validity of an NDC, a searchable list is available on the DVHA website at http://dvha.vermont.gov/for-providers/drug-coverage-lists-1. This list is updated quarterly. Appearance on this list does not guarantee payment, and prior authorization may apply. Any claims submitted for physician administered drugs without a valid NDC will result in claim denials.
This policy is effective for professional claims billed on the CMS-1500 and hospital outpatient claims billed on the UB-04. Straight Medicaid as well as crossover (dual-eligible) claims will follow the policy. Please refer to section 10.3.38 of the Provider Manual for additional information on NDC billing requirements.
Reminder to OPRA Providers The Department of Vermont Health Access (DVHA) would like to remind all non-billing providers, Ordering, Prescribing, Referring & Attending (OPRA) and residents that if they are affiliated with a Hospital, they must list the hospital that they are affiliated with on their enrollment application. Failure to do so will result in your application being returned to you. For the most current forms please visit, http://www.vtmedicaid.com/#/provEnrollDataMaint.
Multiple Modifiers If the service provided requires modifier 26 (professional component) or TC (technical component), and one or more other modifier(s), please be sure to put the 26 or TC in the first modifier position. Failure to do so could result in an incorrect paid amount and an audit finding. Most common errors that resulted in incorrect payments were because claims were billed with modifier 50 (bilateral procedure), 52 (reduced services), or 53 (discontinued procedure) in the first modifier position followed by the 26 or TC.
July 13, 2018 Reminder: Diagnosis codes containing “Unspecified”
The Department of Vermont Health Access has conducted a review of all diagnosis codes containing the word “unspecified” and determined that a number of those codes do not contain the specificity necessary to support the medical necessity of services provided. If these diagnosis codes are used for billed services on or after July 1, 2018, the payment for those services will be denied. If you receive this denial, please revisit the clinical note for the service and choose a more specific code. A majority of these diagnosis codes are specific to laterality. If there is a choice for left, right, bilateral, or unspecified please choose the most specific code outlined in the medical record. If the provider did not specify in the medical record, please reach out to the provider to specify and amend the record.
A list of diagnosis codes that are not accepted due to being “unspecified” has been posted to the Department of Vermont Health Access website. http://ovha.vermont.gov/for-providers/claims-processing-1
Server Maintenance – July 15, 2018 The Provider Web Portal server maintenance is scheduled from midnight to 8:00AM on Sunday, July 15, 2018. During this time, all Provider Web Services will be unavailable. Providers wishing to check eligibility, receive other insurance information or determine if service limits have been reached are advised to use the automated Voice Response System (VRS). The VRS can be accessed by dialing 802.878.7871, option 1 and then option 1 again.

13
June 29, 2018 D1320 Tobacco Counseling for the Control and Prevention of Oral Disease
On or after billed date 07/01/2018, dental providers may bill with CDT code D1320 for tobacco prevention and cessation services. On or after billed date 07/01/2018, dental providers will no longer be able to bill and be paid for smoking cessation codes 99406 & 99407 on a CMS-1500.
LARC Add-on Rate Increase For dates of service, starting 7/1/2018, postpartum long-acting reversible contraceptive (LARC) add-on will be set at the cost of the highest cost device. This change is happening to align with current inpatient prospective payments and to comply with Act 138 of 2018. Currently, the Vermont Medicaid LARC add-on rate is $800. The add-on payment will increase to $908.97 effective 07/1/2018, which matches the highest cost device as of 06/1/2018. This add-on payment will be reviewed every six months to ensure that the rate covers the cost of the highest cost LARC device. Although the new add-on cost will be increased starting 7/1/2018, there will be a delay updating this rate in MMIS. Once the rate is updated, DXC will reprocess any claims that were paid at the rate of $800 for dates of service on or after 07/1/2018.
June 15, 2018 DME Pricing Action Code I to Pricing Action Code 6 Codes
Reminder: the Department of Vermont Health Access (DVHA) has revised its payment methodology for certain DME codes for which there is no reimbursement rate in an established fee schedule. Before date of service 05/01/2018 these codes were paid at 60% of billed charges. For dates of service on or after 05/01/2018 these codes are paid using the manual pricing methodology, described in Section 11.6 Payment DVHA Primary/Manual Pricing of the Vermont Medicaid Provider Manual, found here; http://www.vtmedicaid.com/#/manuals. The code list can be found in GCR 18-044, found here: http://dvha.vermont.gov/global-commitment-to-health/global-commitment-register, and is open for public comment through 6/15/2018. For billed claims from 5/1/2018- 5/29/2018 that were paid at 60%, the provider may choose to recover the claims and resubmit following the manual pricing instructions.
Independently Billing Dental Hygienists Billable services for independently enrolled dental hygienists are now included on a separate Independently Billing Dental Hygienists 2018 Dental Procedure Fee Schedule. The effective date is 1/1/2018.
The fee schedule is available at: http://dvha.vermont.gov/for-providers/claims-processing-1
E-Prescribing Services Update On 4/20/2018, Vermont Medicaid, through its PBM Change Healthcare, established a connection with Surescripts to provide data for Medicaid members. Surescripts supports standard electronic prescription transactions to allow clinicians to securely e-prescribe within their existing workflow.
Providers who use electronic prescribing now have access to Vermont Medicaid data to assist them in managing prescriptions for Medicaid members more efficiently. Information that DVHA has made available through prescribers’ electronic health record software vendors includes:
• Member’s outpatient pharmacy claims history
• Member’s Medicaid eligibility/enrollment status

14
• The preferred status of prescribed drugs on the Medicaid Preferred Drug list
• Indication of a prior authorization requirement for a prescribed drug
If you’re unable to access Medicaid data for your patients, contact your electronic health record software vendor. The functionality of your system is determined by your software vendor. Questions can also be directed, via email, to Change Healthcare at [email protected]
Hearing Aid Coverage Effective 7/1/2018, the Department of Vermont Health Access (DVHA) will cover Clear in Canal (CIC), Contralateral Routing of Signals (CROS) and Bilateral Contralateral Routing of Signal (BI-CROS) hearing aids. The allowable batteries will increase to 12 batteries per side, per month for these three types of hearing aids. A completed Medical Necessity Form (MNF) substantiating the medical need for the hearing aid must be kept on file for auditing purposes.
In-Home Lactation Consultation Services Effective June 1, 2018, Vermont Medicaid will begin to reimburse for in-home lactation consulting services provided by International Board-Certified Lactation Consultants (IBCLCs). Provider Enrollment may commence prior to June 1st and the applicable forms can be found at http://www.vtmedicaid.com/#/provEnrollAppPackets. Lactation Consultants providing services to Vermont Medicaid members must be certified by the International Board of Lactation Consultant Examiners (IBLCE) and licensed and enrolled as a Medicaid provider. Services provided by IBCLCs may include breastfeeding health, education, and counseling services. Lactation consulting services must be performed within the Provider’s scope of practice and per IBCLC certification standards. Billing for services is only allowed on or after the Effective date of June 1, 2018. More information can be found at http://dvha.vermont.gov/global-commitment-to-health/proposed-gcr-17-037-in-home-lactation-consultations.pdf
PERM Audit Notice The Medicaid Payment Error Rate Measurement (PERM) claim review cycle, for the upcoming Reporting Year (RY) 2020, will be commencing soon! The cycle period will run from July 1, 2018 through June 30, 2019. This is a change from the prior cycle, which ran from October to September. Additionally, AdvanceMed Inc. is the new CMS medical record PERM Review Contractor (RC). AdvanceMed Inc.’s responsibilities will include reaching out to VT Medicaid providers during the cycle to obtain claim verification medical documentation. Medical documentation verification will be required for all claims that are selected in the RY 2020 samples pulled for review. We look forward to working with our VT Medicaid providers during this upcoming cycle. For additional information please visit: http://dvha.vermont.gov/for-providers/
Two Dental Procedures Added to GA Vouchers Two dental procedures on the current 2018 Dental Procedure Fee Schedule have recently been added to the list of procedures allowable for use with valid General Assistance (GA) Vouchers covering emergency dental treatment. Both are effective 1/1/2018. Please check the GA Voucher list regularly to ensure you are using the most current information.
Deep Sedation/General Anesthesia – First 15 Minutes
Intravenous Moderate (Conscious) Sedation/Analgesia – First 15 Minutes

15
General Assistance guidelines for emergency dental treatment (including the list of allowable procedures) are available at: http://www.vtmedicaid.com/assets/resources/GAGuideEmrgDentalTrmt.pdf
Keep Your Provider Demographic/Other Information Up-to-Date Providers are required to notify DXC of changes specific to demographics, group affiliation, and address information (billing, mailing, service, prior authorization and legal addresses) in a timely manner. Failure to notify Vermont Medicaid of these changes can result in denied claims, undeliverable correspondence or delayed claims’ payment.
The current Provider Information Change Form is available on the Vermont Medicaid Web Portal at: http://www.vtmedicaid.com/assets/provEnroll/VTMedProviderInfoChangeForm.pdf
Whenever changes occur, please complete the form and return it to the DXC Enrollment Unit. See the form for directions. Contact the DXC Enrollment Unit for further assistance at Out-of-State, (802) 878-7871, In-State, (800) 925-1706, option 4.
June 8, 2018 Reminder: Current Forms Are Required
Vermont Medicaid regularly updates its forms and applications to reflect current state and federal requirements. All provider paperwork, including enrollment applications and forms, adjustment forms and refund forms, submitted on outdated versions, will be returned. Providers are encouraged to always check for the most current forms on the Vermont Medicaid website. http://www.vtmedicaid.com/#/home
Server Maintenance – June 10, 2018 The Provider Web Portal server maintenance is scheduled from midnight to 8:00AM on Sunday, June 10, 2018. During this time, all Provider Web Services will be unavailable. Providers wishing to check eligibility, receive other insurance information or determine if service limits have been reached are advised to use the automated Voice Response System (VRS). The VRS can be accessed by dialing 802.878.7871, option 1 and then option 1 again.
June 1, 2018 Billing Supplies Policy Change
The Department of Vermont Health Access (DVHA) is changing the policy for billing supplies during the rental period of certain items of durable medical equipment. Effective for dates of service on or after May 1, 2018, the DVHA will reimburse for supplies during the rental period for the following codes: E0445, E0465, E0466, E0470, E0471, E0565, E0600, and E0601. The change is currently limited to supplies associated with the codes listed. DVHA is also soliciting comments from the public regarding additional codes and supplies that are not listed through the public comment process associated with GCR 18-044 found here: http://dvha.vermont.gov/global-commitment-to-health/global-commitment-register. This change aligns with Medicare billing for supplies and is part of DVHA’s ongoing strategy to modernize the way it pays for healthcare services.
Integrated Humidifier Requirements The Department of Vermont Health Access will cover a humidifier separately from the positive airway pressure device whether it is built-in/integrated humidifier OR a stand-alone humidifier. If the positive airway device is purchased, the humidifier must also be purchased at the same time. If the positive airway pressure device is rented, the humidifier must also be rented. Rentals recognize a three-month

16
trial period, and months four through ten require prior authorization for completion of the capped rental period once medical necessity has been determined.
May 18, 2018 Vision Services Change
Vision Providers – the Department of Vermont Health Access has recently performed a review of services covered by Vision Insurance Policies, and have found vision policies cover many more services today, than they have in the past. We have modified our edits to match the current industry standard for Vision services. When a member has a vision insurance policy, coverage type 08, please be sure to bill the member’s primary Vision Insurance before billing Medicaid for any unreimbursed balances.
May 11, 2018 New eWEBS Pharmacy Provider Portal
The Department of Vermont Health Access (DVHA) is pleased to announce the launch of the eWEBS Pharmacy Provider Portal. This new portal will help simplify access to member and drug information. It will provide users access to check member eligibility, member drug history and preferred drug list (PDL) information. For more information regarding the eWEBS Pharmacy Provider Portal, visit http://dvha.vermont.gov/for-providers/ewebs-notificaiton-final.pdf.
Server Maintenance – Sunday, May 13, 2018 The Provider Web Portal server maintenance is scheduled from midnight to 8:00AM on Sunday, May 13, 2018. During this time, all Provider Web Services will be unavailable. Providers wishing to check eligibility, receive other insurance information or determine if service limits have been reached are advised to use the automated Voice Response System (VRS). The VRS can be accessed by dialing 802.878.7871, option 1 and then option 1 again.
May 4, 2018 Integrated Humidifier Update
The Department of Vermont Health Access will cover a positive airway pressure device that has a built-in/integrated humidifier OR a positive airway pressure device without a built-in/integrated humidifier and the stand-alone humidifier. If the positive airway device is purchased the humidifier must also be purchased at the same time. If the positive airway pressure device is rented the humidifier must also be rented. Rentals recognize a three-month trial period, and months four through ten require prior authorization for completion of the capped rental period once medical necessity has been determined.
Determining ACO-Attribution Status Beginning in 2017, certain Medicaid members began to be attributed to OneCare Vermont through the Vermont Medicaid Next Generation Accountable Care Organization (VMNG ACO) Program. Through this program, prior authorization is waived for certain services for these members for any provider in or out of the ACO. To determine if a certain member qualifies for this prior authorization waiver, providers may now check a member’s ACO attribution status through DVHA’s secure provider portal when they check for a member’s Medicaid eligibility. If a member is attributed to the ACO, it will be indicated as ACO Attributed, Yes or No, and this would apply for the entire calendar year. This information is located to the right of the Max Co-Pay information in the list of that member’s service types in the eligibility portion of the eligibility status page.

17
April 27, 2018 Billing for Multiple Procedures
When billing for multiple units of the same procedure code, providers are instructed to bill the procedure code on one line, indicating the number of units performed. Be sure to append any applicable diagnosis to support the units billed. Submitting claims with multiple procedure lines of the same code could result in a duplicate denial.
Diagnosis codes containing “Unspecified” The Department of Vermont Health Access has conducted a review of all diagnosis codes containing the word “unspecified” and determined that a number of those codes do not contain the specificity necessary to support the medical necessity of services provided. If these diagnosis codes are used for billed services on or after July 1st, 2018, the payment for those services will be denied. If you receive this denial, please revisit the clinical note for the service and choose a more specific code. A majority of these diagnosis codes are specific to laterality. If there is a choice for left, right, bilateral, or unspecified please choose the most specific code outlined in the medical record. If the provider did not specify in the medical record, please reach out to the provider to specify and amend the record.
A list of diagnosis codes that are not accepted due to being “unspecified” will be posted to the Medicaid website.
Timely Filing Reconsideration Requests Providers submitting timely filing reconsideration requests to the Department of Vermont Health Access (DVHA), should use the updated forms that are now located on the Vermont Medicaid website (http://www.vtmedicaid.com/#/forms). These forms are to be used for timely filing reconsideration requests only; there is a separate form for non-timely filing reconsideration requests. Effective 06/01/2018, any old versions of the timely filing reconsideration request forms will no longer be accepted and will be returned to the provider.
Please note the DVHA will review a decision of an untimely claim in unusual circumstances, if the claim has previously denied for timely filing. Requests that include claims that have not previously denied for timely filing will be returned to the provider.
Please do not send medical records with timely filing reconsideration requests, instead please send account notes showing the follow-up actions that were taken resulting in the late submission.
Please note the multiple claims form is for a single member. Requests containing more than one member will be returned to the provider.
April 20, 2018 Ladies First Fee Schedule
The 2018 Ladies First Fee Schedule has been added to http://dvha.vermont.gov/for-providers/2018-fee-schedule-pdf-format-no-dx-color.pdf. Ladies First providers are encouraged to review the fee schedule. If you don’t see a diagnosis code on the list, call Ladies First billing specialist at 800.508.2222 for claim review and possible manual payment.
April 13, 2018 Face-to-Face Requirements
The Agency of Human Services (AHS) will require physicians enrolled in Vermont Medicaid to document that a face-to-face encounter occurred for the initial ordering of home health services,

18
durable medical equipment, and supplies within specified timeframes. This change assures compliance with federal requirements at 42 CFR §440.70(f). Documentation indicating that the face-to-face visit occurred shall be included in the physician’s initial order for services. The list of DME items subject to the face-to-face requirement can be found here and also includes power wheelchairs. Additional information on the face-to-face visit requirement can be found in the Medicaid Provider Manual. Full text of The Global Commitment Register can be found at http://dvha.vermont.gov/global-commitment-to-health/global-commitment-register.
DMEPOS - PAC Change effective 01/01/2018 The following codes were part of the DMEPOS 01/01/2018 Fee Schedule update and listed as PAC 3, $0.00: A4321, A4483, A6513, A8002, A8003, A8004, E0485, E0486, E0619, E2216, E2217, E2218, E2372, L0452, L0623, L0624, L0629, L0632, L0634, L1001, L3956, L4002.
Per the Centers of Medicare and Medicaid Services (CMS), these codes are manually priced by the DME MAC's. In keeping with CMS, the Department of Vermont Health Access will follow suit and these codes will be PAC 6 (manually priced) retroactive to date of service 01/01/2018.
If a provider has a paid claim with a $0.00 rate for one of the above codes on or after date of service 01/01/2018, please rebill following the Adjustment Request information found in section 8.1 of the Provider Manual, as well as the DME Manual pricing instructions found in section 11.6 Procedure Codes & Pricing.
New Medicare Card Information Beginning 4/1/2018, Medicare will begin transitioning from the traditional Health Insurance Claim Number (HICN) to the new Medicare Beneficiary Identifier (MBI). This is the result of the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015, which mandates the removal of Social Security Numbers (SSNs) from all Medicare cards. For more information on timelines, etc. please visit https://www.cms.gov/Medicare/New-Medicare-Card/index.html.
Please note this change is being conducted by Medicare in order to accommodate the removal of social security numbers from the member’s ID card. There is no impact/change to how providers bill Vermont Medicaid.
April 6, 2018 Server Maintenance – April 8, 2018
The Provider Web Portal server maintenance is scheduled from midnight to 8:00AM on Sunday, April 8, 2018. During this time, all Provider Web Services will be unavailable. Providers wishing to check eligibility, receive other insurance information or determine if service limits have been reached are advised to use the automated Voice Response System (VRS). The VRS can be accessed by dialing 802.878.7871, option 1 and then option 1 again.
March 30, 2018 Provider Name/Number Mismatch
Reminder: For all claims (paper and electronic) the billing provider name must match the name on file with VT Medicaid. When the billing provider is an individual provider, the last name is followed by first name (e.g. SMITH, JAMES). When the billing provider is a group, the full group name should be entered (e.g. THE RANDOM HOUSE). Note that if the enrolled name starts with “THE”, the billing provider name must start with “THE”. Claims where the billing provider name does not match the name on file will be denied.

19
Providers that have multiple VT Medicaid IDs under a single NPI should take special care to make sure their NPI / taxonomy combination matches up with the correct VT Medicaid ID and name they are intending to bill.
Providers seeking verification of the name on file with VT Medicaid should contact Provider Services at 802.878.7871.
Providers seeking to change the name on file with VT Medicaid should contact Enrollment at 802.879.4450 Option 4.
Ambulance Services Provided During a Beneficiary’s Inpatient Stay This is a reminder that all Ambulance providers should review Vermont Medicaid transportation policies concerning services provided to a beneficiary during an inpatient stay. Section 10.3.2 of the Vermont Medicaid Manual outlines scenarios for allowable services. Any hospital transfer during an inpatient stay which involves a return to the original hospital before discharge should not be billed to Vermont Medicaid. In most circumstances, the hospital in which the trip originates is the entity who will pay for these services. Ambulance providers are encouraged to speak with hospitals in their service area to learn about payment during this scenario.
Multiple Surgery Billing Requirements Vermont Medicaid prices multiple surgery payments in order of the procedure code’s Relative Value Unit and will price all surgical procedures in decreasing percentages of 100%, 50%, 40%, 30%, 30%...This includes surgical procedures billed with multiple units.
As of date of submission 05/01/18, providers are required to bill multiple surgeries on a single claim. Any subsequent claims that are billed for multiple surgeries on the same day will be denied. If any billing changes need to be made, the original claim will need to be adjusted by the provider.
In an effort to speed up the processing of multiple surgery claims, we are asking that claims be sent with surgery procedure codes in the RVU order from highest to lowest. We are looking at ways to automate this process for quicker claims processing which would require the procedure to be submitted in the RVU order in the future.
PERM Update The Payment Error Rate Measurement (PERM) FFY2016 cycle finalized as of August 31, 2017. Subsequently, Vermont received its final Federal Fiscal Year (FFY) 2016 PERM findings report (Final Error for Recovery Letter) from Centers for Medicare & Medicaid Services (CMS). CMS notified Vermont that its error rates for both Medicaid and Children’s Health Insurance Program (CHIP) were well below the Cycle II (Cycle II = 17 states) average. As a result, for both Medicaid and CHIP, Vermont’s sample sizes for Reporting Year (RY) 2020 will be lower. Vermont’s PERM team is currently working on implementing Medicaid and CHIP Corrective Action Plans (CAPs). Our objective is to reduce overall errors as we move forward. Vermont Medicaid would like to again express its appreciation to all Medicaid Providers that participated in the FY16 Payment Error Rate Measurement (PERM) Audit (i.e. October 1, 2015 - September 30, 2016). The PERM FFY16 final findings report will be posted on the DVHA PERM website very soon. http://dvha.vermont.gov/for-providers/payment-error-rate-measurement-perm/view

20
March 16, 2018 Capped Rental Guidance
In an effort to be consistent with Medicare’s requirements, the Department of Vermont Health Access (DVHA) will use the Medicare capped rental code list and, like Medicare, when renting, will only allow a RR rental modifier. The exception to this rule is the small sub-set of codes included within the capped rental category with a rent OR purchase option. This change has been in effect since 1/1/2018.
For a full list of codes, please see Medicare’s DMEPOS fee schedule here: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/DMEPOSFeeSched/DMEPOS-Fee-Schedule.html.
DVHA will not institute variable rental pricing depending on the month of rental and instead, will use Medicare guidance to set the rental rates to equal 1/10 of the purchase price of the capped rental.
Medical Documentation for WIC Formula The Vermont WIC Program recently updated the medical documentation forms used when requesting medical formula or medical food. A medical diagnosis and corresponding ICD 10 code is required when making WIC formula requests.
The updated versions of WIC’s medical documentation forms now includes check boxes for the most common nutrition-related ICD-10 diagnosis and code. You may also access the forms at www.healthvermont.gov/children-youth-families/wic/resources-health-professionals.
The Vermont WIC Program currently contracts with Abbott Nutrition for infant formula and receives a lower cost which in turn allows us to serve more families. Keep this in mind when considering a formula for your infant patients. Often families need to purchase additional formula each month due to WIC being a supplemental program.
“Pro” Line and “Non-GMO” products are not WIC-eligible.
Although the “Pro” line of Similac products and Non-GMO Similac are from Abbott, they are not produced in the WIC eligible size so therefore are not covered by WIC. Please contact Abbott if you have further questions as to their decision not to make these available to WIC families. https://abbottnutrition.com/
For information about the updated forms or any WIC topic visit www.healthvermont.gov/wic.
March 2, 2018 Current Forms Required
Vermont Medicaid regularly updates its forms and applications to reflect current state and federal requirements. All provider paperwork, including enrollment applications, adjustment forms and refund forms, submitted on outdated versions, will be returned. Providers are encouraged to always check for the most current forms on the Vermont Medicaid website. http://www.vtmedicaid.com/#/home
GT Modifier for Facility Claims Only Reminder: Effective 01/01/2018, modifier GT is not allowed on professional claims but will continue to be used on facility claims. This change is to align with Medicare guidelines. Please continue to use

21
POS 02 on professional claims to identify telemedicine services. If GT is submitted on a professional claim for dates of service on or after 01/01/2018, the claim will be denied.
Closed for Town Meeting Day The DVHA and DXC Technology offices will be closed on Tuesday March 6, 2018 for Town Meeting Day.
February 9, 2018 Server Maintenance – February 11, 2018
The Provider Web Portal server maintenance is scheduled from midnight to 8:00AM on Sunday, February 11, 2018. During this time, all Provider Web Services will be unavailable. Providers wishing to check eligibility, receive other insurance information or determine if service limits have been reached are advised to use the automated Voice Response System (VRS). The VRS can be accessed by dialing 802.878.7871, option 1 and then option 1 again.
January 26, 2018 Provider Representative Coverage Changes
Effective immediately, the following temporary changes have been made to the areas of coverage for our provider representatives. Unless otherwise specified, hospitals and facilities are to use the representatives for their county:
Margaret Haskins (802.857.2963): Chittenden, Essex, Franklin, Grand Isle, Lamoille, Orleans counties and UVM MC.
Nora Williams (802.857.2957): Bennington, Rutland, Windham, Windsor counties, DHMC and Out of State Providers.
Rebecca Gangl (802.857.2966): Addison, Caledonia, Orange and Washington counties.
A detailed map, including Provider Representative Contact information and territory, is available at: http://vtmedicaid.com/#/manuals
New PES Release (2.32) A new version of Provider Electronic Solutions (PES 2.32) has been released on the VT Medicaid web portal. Upgrading is encouraged, but not mandatory (see PES Users – New Taxid (EIN)). Version 2.32 will automatically change your data to reflect the new DXC Tax ID. For details please read PES News. The 2.32 Full Install, Upgrade, and PES News can be found at: www.vtmedicaid.com under Information, PES Software and Resources. For questions regarding the Full Install or Upgrading, please contact the EDI Coordinator at 802.879.4450 Option 3 or send an email to [email protected].
Provider Referral Verification Reminder Providers who refer patients for laboratory and other services must ensure the providers that patients are being referred to are enrolled with Vermont Medicaid.
Prior to making referrals, please check at http://www.vtmedicaid.com/#/providerLookup to verify that the Entity where the patient is being referred is actively participating with Vermont Medicaid.

22
Updated DME Restrictions List Effective with date of service 02/01/2018, the Department of Vermont Health Access (DVHA) will post a revised DME Restrictions List that contains changes to several codes such as limitations, modifiers required, with specific time frames for each item. The list is on the VT Medicaid Portal and can be found at http://www.vtmedicaid.com/#/resources.
Please note the DVHA will not separately cover the cost of a humidifier for a positive airway pressure device that has a built-in/integrated humidifier. For those devices that do not have an integrated system, the humidifier must be rented along with the positive airway device for the first 3 months. After the three-month trial period, prior authorization for humidifier and the positive airway device will be required if medical necessity continues to exist.
Reimbursement methodologies have been updated for Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) payments according to the fee schedule.
The list of codes is provided for reference purposes only and may not be all inclusive. Listing of a code does not imply that the service described by the code is a covered or non-covered health service. Please refer to the Fee Schedule for coverage.
Prior authorization is required for items in excess of the limits when medically necessary.
Electronic Asset Verification Coming for MABD Medicaid Programs The Department of Vermont Health Access is pleased to announce that the electronic asset verification service (AVS) was implemented at the end of 2017. This will increase the accuracy of eligibility determinations by automating most of the asset verifications for resource tests for Medicaid for the Aged, Blind, and Disabled, including Long-Term Medicaid. Although this will not completely eliminate the need for Vermonters to submit paper documentation, it should greatly reduce the burden on applicants as well as State eligibility staff. Implementing an electronic asset verification system puts us in compliance with the requirement under section 1940 of the federal Supplemental Appropriations Act.
January 19, 2018 Change to Provider Remittance Advice Due to SSNRI
As of February 1, 2018 a member’s Medicare HICN number will no longer appear on your Remittance Advice. This change is to align with the Social Security Number Removal Initiative (SSNRI). Additional information regarding SSNRI can be found at http://go.cms.gov/ssnri.
Rental of Oxygen and Oxygen Related Equipment Effective January 1, 2018, any code billed for the rental of oxygen or oxygen related equipment will require the RR (rental) modifier. RR should be used on ALL rentals, regardless of whether the code language includes the wording "rental". The Department of Vermont Health Access is making this change to be consistent and align with Medicare billing & coding practices.
Modifier U9 Usage When submitting claims for the placement of sealants on deciduous molars, bicuspids and anterior teeth, you must add the U9 modifier to the end of procedure code D1351. For example, when submitting for a sealant placed on tooth #28, use procedure code D1351U9.

23
DMH to discontinue use of codes H2019 and H2032 The Department of Mental Health (DMH) has discontinued the use of HCPCS codes H2032 (Activity Therapy: Group Therapy) and H2019 (Therapeutic Behavioral Services) effective for date of services on or after 1/1/2018. Services that were previously billed with H2019 and H2032 should now be billed with one of the appropriate CPT codes: 90832, 90834, 90837, 90846, 90847, or 90853. Please refer to the DMH fee schedule and FFS manual for additional information.
Elimination of the GT Modifier for Telehealth Effective 01/01/2018, modifier GT will no longer be required to identify telemedicine services on physician claims but will continue to be used on facility claims. This change is to align with Medicare guidelines. Please continue to use POS 02 for physician claims.
January 12, 2018 Closed for Martin Luther King Jr. Day
The DVHA and DXC Technology offices will be closed on Monday, January 15, 2018 in observance of Martin Luther King Jr. Day.
Server Maintenance – January 14, 2018 The Provider Web Portal server maintenance is scheduled from midnight to 8:00AM on Sunday, January 14, 2018. During this time, all Provider Web Services will be unavailable. Providers wishing to check eligibility, receive other insurance information or determine if service limits have been reached are advised to use the automated Voice Response System (VRS). The VRS can be accessed by dialing 802.878.7871, option 1 and then option 1 again.
January 5, 2018 PES Users – New Tax ID (EIN)
For those using PES that have not yet upgraded to version 2.32, please do the following to change to the new DXC Tax ID starting in January 2018.
• Logon to PES • From the gray screen click Tools, Options • Click on the Payer/Processor Tab • Delete the old Tax ID and enter the new Tax ID (822287119) in the ETIN and Identifier Code
fields • Click OK
FQHC and RHC Cost Settling Update Effective for date of service on or after 01/01/2018, VT Medicaid will no longer be cost settling encounter claims for Federally Qualified Health Centers and Rural Health Centers for services provided. As a reminder, it is imperative to follow proper billing and correct coding guidelines when submitting claims.
Reminder for DME Providers The Department of Vermont Health Access (DVHA) would like to remind all DME providers that the Usual and Customary rules apply to the Capped Rental Policy, DME Manual Pricing, and the DME Fee Schedule. This information must be followed at all times.