Vats
Transcript of Vats

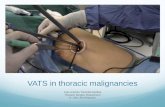
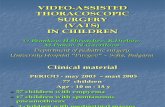
Video-Assisted Thoracic Surgery for Wedge Resection, Lobectomy, and PneumonectomyVideo-assisted thoracic surgery (VATS) is an appealing alternative to thoracotomy for many types of pulmonary resections. DefinitionThe exact definition of a VATS lobectomy (VL) is controversial. The controversies center around the issues of rib spreading, instrumentation, and anatomic dissection. Basically, a VL should include the following: a true anatomic dissection with nodal sampling or dissection
an incision <10 cm long with no rib spreading,
and visualization on a monitor rather than through the incision.
Vats Resection of Lung NodulesThe emergence of VATS has changed the algorithm for the diagnosis of a lung nodule. Needle biopsies are performed less often. Currently, because the morbidity and mortality of a wedge resection is so low, there is a lower threshold to perform a VATS biopsy of a suspicious lung mass. VATS is the most common and simplest method for lung biopsy.
Localization of Lung Nodules by VATSResection of a lung mass begins with identification of the mass. Because the small incisions used for VATS make palpation of the lung more challenging than through a thoracotomy, a key to successful resection of a lung mass via VATS is the ability to find the lesion. Therefore accurate localization of a lung mass requires an excellent understanding of the correlation between computed tomography (CT) images and lung anatomy to identify the target area of the lung. An experienced thoracic surgeon can almost always find a lung mass in this fashion. The lung is quite mobile, so most areas of the lung can be brought to a finger placed through the incision in the fourth intercostal space in the midaxillary line. Other thoracic surgeons are facile at “feeling” the lung with an instrument that basically acts as a finger extension.There are techniques to assist with intraoperative identification of a small mass that cannot be palpated.5,13,28 Indications for these techniques

include ground-glass opacities <1 cm, small masses <5 mm, and masses >2 cm below the pleural surface. In some cases, the small ground-glass opacities (GGOs) have been difficult to palpate even after the lung tissue has been removed from the patient; therefore the use of a wire has helped the pathologist to prepare slides from the correct area in the lung. Under CT guidance, the radiologist places a hook wire into or adjacent to the nodule. This is the same hook wire used for localization of a breast mass. The wire should be cut flush with the chest wall. (If the wire has been taped to the chest without being cut, the wire may become dislodged from the mass if the patient develops a pneumothorax and the lung pulls away from the chest wall.) As Mack and colleagues13 noted, this technique is associated with minimal complications (e.g., rare dislodgment of the wire or pneumothorax). Wire localization was used more often in the early days of VATS, before surgeons realized that it was rarely necessary. This technique has again become more common, because screening CT scans identify small nodules that may be difficult to locate with VATS.Daniels and associates5 have described a technique using transthoracic percutaneous radiotracer injection with VATS radioprobe localization and excision of small pulmonary nodules. Using this technique, a CT-guided injection of radiotracer solution is made into or adjacent to the nodule on the day of surgery. Next, an intraoperative gamma probe is used to localize the lesion, followed by VATS excision of the lesion.5
Wedge ResectionanesthesiaUnder one-lung general anesthesia, the patient is placed in a lateral decubitus position with a slight posterior tilt. A double-lumen tube allows better decompression of the lung to be biopsied than a single-lumen tube with a bronchial blocker.
Position The bed is flexed to help get the hip out of the way of the trocar and thoracoscope. It may also help to open the intercostal spaces.
Incision The incisions for our approach to video-assisted thoracic surgical lobectomy, including the following: (1) incision 1 in the mid-clavicular line for the stapler; (2) incision 2 for the trocar and the thoracoscope; (3) the utility incision 3; and (4) incision 4, the auscultatory triangle for an assistant's instrument.

Technique for Wedge ResectionThe wedge resection begins with a ring forceps through incision 3 to hold the lung. Care should be taken to not crush the mass because it may no longer be palpable after it is crushed.
A ring forceps through incision 1 may compress the lung parenchyma below the mass to hold the lung for palpation and compress thicker lung parenchyma to facilitate passage of the stapler across the lung tissue.
The endoscopic stapler is then passed through incision 1 (Fig. 35-2) and fired.
In some cases, the stapler through incision 1 can complete the resection.
In other cases, a stapler through incision 3 can complete the resection.
If there is a possibility that the mass is malignant, then the specimen is placed in a standard Endocatch bag (US Surgical, Norwalk, CT) for removal (Fig. 35-3) because cancer has recurred in VATS incisions after biopsy.3
If frozen section shows that the mass is inflammatory, cultures of the specimen are sent.
If the mass proves to be a lung cancer, then VATS lobectomy is performed.
Alternatively, a lung mass can be carved out with electrocautery and the lung parenchyma sutured.
This requires proper exposure, traction, and countertraction.
This is certainly more challenging with VATS than via an open procedure. Smoke from the electrocautery can be problematic.
Suction in the thoracic cavity causes the lung to reexpand unless air can flow into the thoracic cavity through at least one of the incisions.
Many thoracic surgeons find endoscopic suturing difficult, so this approach is less common than wedge resection with staples.
Postoperative Care After Wedge Resection

While there are reports of outpatient lung biopsies,the procedure is usually an inpatient procedure. Postoperatively, unless the patient has severe respiratory compromise, it is uncommon for the patient to go to the intensive care unit. The chest is usually drained with a single 28-Fr chest tube and the chest drainage system need not be attached to suction unless the patient develops significant subcutaneous emphysema. Postoperative pain is usually controlled with Dilaudid SQ and Vicodin PO. The patients have no dietary restrictions and are ambulated immediately. No routine labs or chest x-rays are necessary unless clinically indicated (fever, excessive chest drainage, management of diabetes, etc.). The chest tube is removed when there is no air leak and the chest tube drainage is <300 mL in 24 hours (usually on the first postoperative day). The length of stay is often 1 day for a wedge resection.
General Approach for a VATS LobectomyA VATS lobectomy should be the same procedure that is performed through a thoracotomy. This includes the individual ligation of vessels and bronchus for the lobectomy and a lymph node dissection or sampling.Most lobectomies can be performed by VATS. Importantly, the procedure should be the best operation for the patient.
Indications for Video-Assisted Thoracic Lobectomy
Clinical stage IA and IB lung cancer Tumor size <5 cm Benign disease (giant bulla, bronchiectasis, etc.) Physiologic operability
Possible Contraindications to Video-Assisted Thoracic Surgical Lobectomy
Significant nodal disease (benign or malignant) adherent to vessels
Chest wall or mediastinal invasion (T3 or T4 tumor) Need for sleeve lobectomy Neoadjuvant chemotherapy (relative) Neoadjuvant radiation therapy (relative) Positive mediastinoscopy

Technique for VATS LobectomyThis section first describes the techniques common to all VATS lobectomies and then discusses some features that are unique to resection of specific lobes.
One-Lung VentilationAfter induction of general anesthesia with one-lung ventilation, the patient is placed in a lateral decubitus position with a slight posterior tilt. A double-lumen tube is preferable because a single-lumen tube with a bronchial blocker does not collapse the lung as well. To maximize lung collapse, one-lung ventilation is instituted while the patient is positioned and the surgeon goes to the scrub sink. If the lung has not collapsed enough when the procedure begins, the bronchoscope is passed into the ipsilateral mainstem bronchus for suctioning to encourage further atelectasis. Insufflation of CO2 is rarely needed.IncisionsProper placement of incisions is critical to the ease of performing a lobectomy via VATS. The incisions for a VATS lobectomy are basically the same as those for a wedge resection described above. The full 5-cm length of the utility incision (incision 3) for a VATS lobectomy is made as soon as the decision is made to proceed with a lobectomy, so that the entire incision can be used for performance of the lobectomy with the passage of multiple instruments and the ultimate withdrawal of the specimen through the utility incision.
From the edge of the latissimus dorsi muscle, it extends anteriorly for 4 to 6 cm.
With the patient in the lateral decubitus position, the incision is directly up from the superior pulmonary vein for an upper lobectomy and one interspace lower for a middle or lower lobectomy.
The ribs are not spread, but a Weitlander retractor may be used to hold the soft tissues of the chest wall open for easier passage of instruments and to prevent the lung from expanding when the pleural space is being suctioned. Incision 4 in the auscultatory triangle (three finger breadths below the tip of the scapula and halfway to the spine), is often helpful for a VATS lobectomy.

Lower placement of this posterior incision improves the angle of the stapler for the superior pulmonary vein and assistance with a lower lobectomy. Slightly higher placement of the incision helps with paratracheal node dissection but makes the angle for the stapler on the pulmonary vein more difficult. Thisincision greatly helps a thoracic surgeon assisting a fellow or resident with a VATS lobectomy.
Position of the SurgeonFrom the front side of the patient, the surgeon begins dissection of the hilum. This is the approach used for lung resection through an anterolateral muscle-sparing thoracotomy, which makes a VATS lobectomy much easier than trying to perform it with the approach used for a posterolateral thoracotomy. The lobectomy is performed from anterior to posterior. There is no dissection in the fissure because the fissure is transected with the stapler as needed to help the lobectomy progress.
Hilar DissectionVessels in the hilum are dissected sharply through the utility incision with standard thoracotomy instruments, such as Metzenbaum scissors and DeBakey pickups. The hilar structures are easily accessible for dissection through the utility incision. A right angle clamp passes around vessels to prepare them to be stapled (Fig. 35-4). Hilar vessels can be tied just as with an open procedure because a finger can usually reach through this incision to the vessels. Removal of lymph nodes (level 10 on the right or level 5 and 6 on the left) facilitates the ease and safety of mobilization of the vessels. Spreading widely with the right angle clamp makes it much easier to pass the nonarticulating endoscopic stapler (EZ 35, Ethicon or Endo-GIA, US Surgical, Norwalk, CT) across the pulmonary vessels.
Stapling DevicesThe fissure, bronchus, and pulmonary vessels larger than 5 mm are transected with the endoscopic stapler. The vascular (20-mm) staples are used for the vessels, and the green cartridge (48-mm) staples are used on the fissure and the bronchus. Occasionally, elevating the vessel with a tie aids placement of the stapler across the vessels or passing a red Robinson catheter behind the vessel guides a stapler around the vessels. Articulation of the stapling devices is not necessary if the incisions are placed properly. The incision that offers the best angle for stapling these structures are as follows;Posterior incision (incision

4) Superior pulmonary veinAnterior trunk of upper lobe arteryMiddle lobe artery and veinLeft upper lobe bronchus
Utility thoracotomy incision (incision3) Minor fissure
Right upper lobe bronchusInferior pulmonary vein
Midclavicular incision (incision 1) Inferior pulmonary veinAnterior trunk of upper lobe arteryMajor fissureMinor fissureAdditional left upper lobe arteryLower lobe arteryLower lobe bronchus
Alternatively, small vessels can be clipped or tied. The utility incision is positioned so that the surgeon may tie extracorporeal knots and a finger can push the knot to the vessel without the need for a knot pusher.Completeness of the FissureThe completeness of the fissure is not a factor in determining the feasibility of performing a VATS lobectomy through an anterior approach. Vessels are dissected anteriorly, not through the fissure; the fissure is usually completed after the vessels and bronchus are transected.
Specimen RemovalTo minimize the risk of contaminating the incision with the tumor, the lung specimen is placed in a bag for removal through the utility thoracotomy incision (Fig. 35-6). An Endocatch (US Surgical, Norwalk, CT) may be large enough for a middle lobe, but it will rupture if it is pulled through the utility incision with a larger lobe. The other lobes or the entire lung require the LapSac (Cook Urological, Bloomington, IN)

because it is a larger bag. The lobes usually have a pyramidal shape. Removal of the lobe is easier if the narrow part of the lobe is removed first. Rarely, the ribs may be spread or shingled for larger tumors or lobes.
Lymph Node DissectionEither a mediastinal node sampling or complete lymph node dissection should be part of a VATS lobectomy (Fig. 35-7). For a paratracheal node dissection, the lung is retracted posteriorly so the dissection can begin with incising the pleura along the trachea, superior aspect of the azygos vein, and superior vena cava. Paratracheal node dissection is easier if the azygos vein is first transected with an endoscopic vascular stapler. From posteriorly, a ring forceps lifts the pleura and the paratracheal nodes as the surgeon dissects in the planes along the superior vena cava, trachea (with preservation of the vagus nerve), and pericardium over the ascending aorta, from the pulmonary artery to the innominate artery.
Subcarinal node dissection begins with anterior retraction of the lung through the utility thoracotomy incision or incision 1 for exposure of the subcarinal space. The pleura is incised posterior to the inferior pulmonary vein and superiorly toward the bronchus intermedius. A ring forceps from posteriorly lifts the pleura over the nodes so the pleura can be incised along the intermediate bronchus, and blunt dissection is performed on the surface of the bronchus intermedius and pericardium. Clips are applied to any tissue that does not easily separate with spreading. The vagus nerve and esophagus are identified and preserved. Upon completion of the subcarinal dissection, the left and right mainstem bronchi and the esophagus should be well exposed.Aortopulmonary window (level 5), para-aortic (level 6), and hilar lymph nodes usually are resected before left upper lobectomy because it makes mobilization of the pulmonary vessels easier and safer. The pleura is cut parallel to the phrenic nerve and then along the superior margin of the superior pulmonary vein from the pericardium and laterally along the apical vein as it crosses the anterior trunk. The nodes and pleura are then lifted to mobilize the tissue from the pulmonary artery. The pleura is incised parallel to the vagus nerve. The recurrent laryngeal nerve is identified and preserved. The lymph node tissue is then dissected off the aorta.
Adequacy of VATS Nodal DissectionSagawa26 performed a prospective study in which one surgeon would perform a lobectomy and as complete a nodal dissection as possible by VATS. After the VL was completed via a thoracotomy, another thoracic

surgeon removed any additional tissue that could be found in the areas where a nodal dissection had been performed by VATS. On the right side, the average numbers of resected lymph nodes by VATS and lymph nodes removed by thoracotomy were 40.3 and 1.2, respectively. The average weights of dissected tissues by VATS and by thoracotomy were 10.0 g and 0.2 g, respectively. On the left side, there were 37.1 and 1.2 lymph nodes and 8.3 g and 0.2 g of weight of dissected tissues. No metastases were observed in the lymph nodes removed at thoracotomy. The nodal dissection by thoracotomy showed no significant additional tissue. Therefore a thoracic surgeon committed to performing a complete nodal dissection by VATS can do so.
Simultaneous Stapling LobectomyLewis and Caccavale11 have reported thoracoscopic lobectomy with simultaneous individual stapling (SIS lobectomy) of the vessels and bronchus rather than individual ligation. This procedure has created considerable controversy because some surgeons view it as a glorified wedge resection. With this technique, the lobe is mobilized by partially completing the fissure. A TA stapler, used for open procedures, is fired across the remaining fissure, vessels, and bronchus. Most surgeons do not agree with this technique because they believe that the vessels should be individually dissected and ligated for a lobectomy.
Techniques for Specific Lobectomies
Right Upper LobectomyThe anterior approach for a right upper lobectomy begins in the hilum. The pleura is incised along the superior vena cava, azygos vein, and the superior aspect of the hilum. Removal of the tissue in this triangle removes the hilar (level 10) lymph nodes and defines the right mainstem bronchus, anterior trunk of the pulmonary artery, and the vein from the apical segment. Blunt dissection along the superior apect of the anterior trunk at this time prepares the artery for its later transection. The middle and upper lobe veins are defined by removing the lymph node between these structures. The stapler is then lined up with the confluence of the veins and the fissure to complete the minor fissure. The stapler goes through incision 1. Completion of the minor fissure creates a pathway through which a vascular stapler passes from the posterior incision 4 to transect the upper lobe vein. Removal of lobar nodes between the main pulmonary artery and the anterior trunk allows a right angle to mobilize the anterior trunk so it can be transected with a stapler. The best angle for the stapler to reach the anterior trunk is through incision 4 in the auscultatory triangle. The posterior ascending artery can then be easily

seen as it courses between the upper lobe and intermediate bronchi. Through the utility thoracotomy incision, the artery is mobilized and clipped. The final maneuver is completion of the remaining fissure and stapling the upper lobe bronchus with the stapler through incision 1.
Middle LobectomyMiddle lobectomy begins by defining the confluence of the upper and middle lobe veins. A right angle clamp through the utility incision mobilizes the middle lobe vein. The vascular staple through incision 4 transects the vein. This exposes the bronchus so that it can be mobilized with the right-angle clamp through the utility incision. Either incision 4 or the utility incision provide a good angle for stapling the middle lobe bronchus. This exposes the middle lobe artery. The lobectomy is finished by completing the major fissure between the lower and the middle lobe and then the minor fissure.A second artery for the middle lobe may be found posterior to the bronchus. If present, this artery is transected before the bronchus is addressed.
Right Lower LobectomyThe operation for a lower lobectomy begins by taking down the pulmonary ligament as the lung is retracted superiorly. It is then retracted anteriorly for removal of the subcarinal lymph nodes to expose the posterior aspect of the inferior pulmonary vein. With posterior retraction of the lobe, dissection between the superior and inferior veins completes the mobilization of the inferior pulmonary vein so that it can be stapled through incision 1 or the utility incision. The lung is returned to its normal anatomic position so staples can complete the major fissure between the middle lobe and the lower lobe. The bronchus and the artery can then be #####`identified by lifting lung parenchyma in the fissure superiorly. Dissection along the surface of the artery creates a tunnel to complete more of the fissure with a stapler from incision 1. Lobar lymph nodes are removed to provide good exposure for individual transection of the artery and bronchus. Finally, the fissure by the superior segment is completed with the stapler through incision 1.
Left Upper LobectomyThe technique for a left upper lobectomy is similar to that for a right upper lobectomy. The approach begins anteriorly with dissection of the hilar, level 6, and level 5 nodes. This continues on the superior aspect of the hilum along the superior pulmonary vein and anterior trunk of the

artery. The superior pulmonary vein is mobilized and transected, with care to make sure that there is not a common trunk of the vein. A stapler through incision 1 completes the major fissure between the lingula and the lower lobe to expose the lingular artery that can be tied from the utility incision or stapled from incision 1. The bronchus is thus exposed. The most dangerous part of a left upper lobectomy is mobilization of the bronchus, because a right-angle clamp must be passed between the bronchus and the artery. After mobilization, the bronchus is stapled from posteriorly. The remaining branches of the artery can then be seen. Dissection through the utility incision mobilizes these arteries to tie or clip them. Finally, the fissure is completed with multiple firings of the stapler through incision 1.Left Lower LobectomyA left lower lobectomy is performed with the same technique as is used for a right lower lobectomy.
VATS PneumonectomyA pneumonectomy on either side is simpler than a lobectomy.
The superior pulmonary vein is mobilized through the utility thoracotomy incision and stapled through the midclavicular incision.
This exposes the artery.
Because there are reports of endoscopic staples cutting without stapling the vessel, it is advisable to either use an endoscopic noncutting stapler or an open stapler (TX, Ethicon or Endo-GIA, TA, US Surgical, Norwalk, CT).
The inferior pulmonary vein is stapled from anteriorly. Removal of subcarinal nodes provides access to the mainstem bronchus at the level of the carina.
Through the utility thoracotomy incision, a 30-mm TA stapler is then fired on the bronchus.

An entire lung can usually be removed through the same size incision as a lobe if the apex of the lung is passed first through the incision.
Potential Benefits of VATS Versus Thoracotomy Less pain and less narcotic requirement10
Less impact on immune system33
Lower incidence of pneumonia34
Less atrial fibrillation (possibly)17
Less compromise on shoulder range of motion12
Less hospital and anesthesia charges20
Reduced need for transfer to skilled nursing unit1
Better chance to complete adjuvant chemotherapy23
Better postoperative pulmonary function21
Easier for elderly patients19