VAGAL CONTROL OF GLUCAGON RELEASE IN MAN
Transcript of VAGAL CONTROL OF GLUCAGON RELEASE IN MAN

546
and in one study similarly reduced stores were
recorded in healthy old people living at home.*’ Oneof the striking features of this study has been the dra-matic rise in ascorbic-acid levels during therapeuticsupplementation. Griffiths 10 and Andrews et allwere able to show similar biochemical improvementin geriatric patients following ascorbic-acid supple-mentation, whilst Brocklehurst et al.12 and Dymockand Brocklehurst 13 found both clinical and biochemi-cal improvement following therapy with a multivita-min preparation.Ham and Elliott 14 have shown that ascorbic acid is
an important factor for the normal synthesis and main-tenance of collagen in the repair of tissues, so that whenascorbic acid is deficient the hydroxylation of theaminoacids proline and lysine in the protocollagenmolecule is inhibitedY In addition, Dunphy andUdupa 16 have reported delay in wound healing withprotein deficiency, and that this delay can be reversedby administering methionine. However, in guineapigswith both protein and ascorbic-acid deficiency ascor-bic acid as well as methionine is necessary for normal
collagen synthesis. Although we have no direct evi-dence that our patients were protein-depleted ourresults do show that some had subnormal ascorbic-acid levels. The patients in this study had a meanpre-treatment ascorbic-acid level of 23 jU,g. per 108white blood-cells, which is only slightly above thelower limits of our normal range of 18 µg. per 108white blood-cells. Ascorbic acid therapy increasedthese levels as has been reported previously.9,IOAs the rates of healing were significantly improved(p<0.005) in the ascorbic-acid-treated group, wewould postulate that ascorbic acid is of value in thetreatment of pressure-sores. However, correction ofprotein deficiency, prolonged direct pressure, anaemia,ischæmia, and incontinence must also be regarded asimportant factors in the treatment of pressure areas.It remains to be determined whether ascorbic-acid
supplementation may have a role in the prevention ofpressure-sores.
We thank Mr Norman Shaw, under whose care these
patients were admitted; Dr F. Meichen, of E. Merck Limited,who kindly supplied the ascorbic-acid preparations; and Prof.J. M. Evanson for encouragement and advice.
Requests for reprints should be addressed to I. W. D.,Department of Medicine, Withington Hospital, ManchesterM20 8LR.
REFERENCES
1. Wolbach, S. B., How, P. R. Archs Path. 1926, 1, 1.2. Hunt, A. H. Br. J. Surg. 1941, 28, 436.3. Crandon, J. H., Lund, C. C., Dill, D. B. New Engl. J. Med. 1940,
223, 353.4. Hunter, T., Rajan, K. T. Paraplegia, 1971, 8, 211.5. Denson, K. W., Bowers, E. F. Clin. Sci. 1961, 21, 157.6. Andrews, J., Brooks, M. Lancet, 1966, i, 1350.7. Griffiths, L. L., Brocklehurst, J. C., Scott, D. L., Marks, J.,
Blackley, J. Geront. clin. 1967, 9, 1.8. Milne, J. S., Lonergan, M. E., Williamson, J., Moors, F. M. L.,
McMaster, R., Percy, N. Br. med. J. 1971, iv, 383.9. Dymock, I. W., Judge, T. G. Unpublished.
10. Griffiths, L. L. in Vitamins in the Elderly (edited by A. N. Exton-Smith and D. L. Scott). Bristol, 1968.
11. Andrews, J., Letchner, M., Brooks, M. Br. med. J. 1969, ii, 416.12. Brocklehurst, J. C., Griffiths, L. L., Taylor, G. F., Marks, J.,
Scott, D. L., Blackley, J. Geront. clin. 1968, 10, 309.13. Dymock, S. M., Brocklehurst, J. C. Age and Aging, 1973, 2, 172.14. Ham, A. W., Elliott, H. L. Am. J. Path. 1938, 14, 323.15. Stone, N. L., Meister, A. Nature, 1962, 194, 555.16. Dunphy, J. E., Udupa, K. N. New Engl. J. Med. 1955, 253, 847.
VAGAL CONTROL OF GLUCAGON RELEASEIN MAN
S. R. BLOOM N. J. A. VAUGHANR. C. G. RUSSELL
Middlesex Hospital, London W1
Summary A significant fall in fasting plasma-pancreatic-glucagon was produced by
injection of atropine. After arginine infusion atropinereduced the normal rise of glucagon by 33% andglucose by 40%. Eleven patients studied during in-sulin hypoglycæmia after a selective vagotomy showeda peak rise in plasma-glucagon of 173 pg. per ml.,which was not significantly different from the glu-cagon rise in ten preoperatve controls (168 pg. perml.). The glucagon response to insulin hypoglycæmia(81 pg. per ml.) in a matched group of ten patients withtruncal vagotomy was significantly less than afterselective vagotomy. This evidence of parasympatheticcontrol of the alpha cell accords with morphologicaland laboratory-animal findings. Maintenance of nor-mal glucagon release after selective vagotomy favoursthe use of this operation rather than the cruder truncalvagotomy.
Introduction
Langerhans in 1869 observed that autonomic-nerve fibres were closely associated with the pancreaticislets, and many histologists have since confirmed thisfinding.2,3 Electron-microscopy has demonstrated
cholinergic nerve terminals applied to the surface ofthe alpha cell.4 In 1973 Iverson demonstrated, in theisolated perfused dog pancreas, that the addition ofacetylcholine to the perfusion medium caused an
immediate large release of glucagon.5 Later, directstimulation of the peripheral end of the thoracic vagusnerve in the anaesthetised calf was shown to produce arapid rise of plasma-glucagon.6 In the conscious calf
atropine lowered the fasting plasma-pancreatic-glucagon and substantially delayed the glucagonresponse to insulin hypoglycsemia. The importanceof the parasympathetic innervation in the calf wasshown even more clearly by division of the splanchnicsympathetic nerves, thus removing the very sensitivesympathetic control mechanism.’ Sympathetic divi-sion alone did not significantly alter the glucose or
glucagon response to insulin hypoglycsmia, but theadditional administration of atropine almost totallyabolished the expected glucagon rise and caused a
much greater glucose fall with development of hypo-glycasmic convulsions.The role of the parasympathetic innervation in the
control of circulating glucagon concentration has botha physiological interest and a practical importance.Vagotomy for the treatment of duodenal ulceration ispopular, but there is argument concerning the meritsof a selective vagotomy, in which the vagal innerva-tion of the pancreas is preserved, versus the simplerand easier operation of truncal vagotomy. We havetried to establish the importance of this parasympa-thetic pancreatic innervation in glucagon control in
man.

547
Methods
Nine healthy young volunteers were studied after an
overnight fast, and at least 1 hour’s preliminary rest ona couch in order to diminish any postural changes or
stress due to travel to the laboratory and the introductionof the venous catheters. Each volunteer received at
random 15 µg. per kg. atropine, or a similar volume ofsaline, on separate days. This was given by intravenousinjection over 2 minutes. Volunteers also received two30-minute infusions of arginine (0-5 g. per kg. as 15%solution) administered 30 minutes after the atropine or
saline injections. Blood-sampling was continued for a
further half-hour after discontinuation of the arginineinfusions.Three groups of patients were studied during insulin
hypoglycaemia: ten preoperative patients with duodenalulcer (mean age 34 years, weight 64’1 kg.), eleven patientsafter selective vagotomy and drainage (mean age 40’4years, weight 64’3 kg., time postoperative 7 months), andten patients with truncal vagotomy and drainage (meanage 46 years, weight 68-0 kg., time postoperative 11
months). No clinical difference was detected between thetwo postoperative groups, all patients having had a satis-factory result from the surgery for their duodenal ulcer.The patients were studied as part of the normal pre-operative and postoperative assessment of gastric function.An insulin gastric-secretion test was performed on eachpatient after an overnight fast using 0-2 units insulinper kg. intravenously after a basal period. Samples ofgastric juice were collected to assess that the vagotomyhad been satisfactory by Hollander’s criteria.8 Only thosepatients whose vagotomy was complete were investigated,so approximately 80% of those who had initially under-gone selective or truncal vagotomy could be included inthis study.
Degradation of glucagon in blood-samples was pre-vented by the addition of 1000 kallikrein-inhibiting unitsof aprotinin (’Trasylol ’) per ml. of blood, rapid centri-fugation, and storage of the plasma at -20°C until thetime of assay. Plasma-glucagon was measured by a
radioimmunoassay utilising a pancreatic glucagon specific(C-terminal reacting) antiserum at a final dilution of
1/400,000. This antiserum cross-reacts less than 5%with enteroglucagon preparations. Duplicate assay tubes
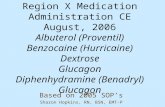
Fig. 1-Changes in plasma-glucagon, blood-glucose, plasma-insulin, and pulse-rate after intravenous atropine (15 µg. perkg.) administration to five subjects.The plasma-glucagon concentration, drawn as a dotted line,
shows the changes after a control intravenous saline injection.Vertical bars indicate s.E.m.s.
contained 20% unknown or, in the standard curve,glucagon-free plasma. A charcoal-separation procedurewas used after a 4-day incubation at 4°C. Addition ofplasma containing 50 pg. glucagon per ml. caused a 10%fall in the percentage glucagon 1251 bound to antibody. Asa further precaution against error due to unsuspectedenteroglucagon cross-reaction, the samples were also
assayed using an antibody which fully reacts with entero-glucagon. Blood-glucose was measured by a glucose-ferricyanide 10 technique.
Results
Atropine caused a fall in the resting plasma-pancre-atic-glucagon in all nine volunteers when comparisonwas made between the mean of the five basal samplesand the mean of the four samples between 15 and 30minutes after atropine. The mean fall was 7-4 pg.
(35.2±2.2 to 27.8 ±1.8 pg. per ml.) and was significant(p<0.02). No change was seen in plasma-pancreatic-glucagon after saline injection (fig. 1), nor was a
change demonstrated in either group by the assaymeasuring enteroglucagon. There was no significant
to 30 DU
MinutesFig. 2-Plasma-glucagon, blood-glucose, and plasma-insulinduring a 30-minute intravenous arginine infusion (05 g. perkg.).Dotted lines indicate the results after prior administration of
atropine (15 µg. per kg.). Vertical bars show S.E.M.S.
Mmuces
Fig. 3-Plasma-glucagon changes during insulin hypoglyca:mia.Ten preoperative duodenal-ulcer patients (), elevenpatients after selective vagotomy ( - - - - ), and ten
patients after truncal vagotomy ( ), Vertical barsshow S.E.M.s.

548
change in either blood-glucose or plasma-insulin afteratropine.During arginine infusion, pancreatic-glucagon, glu-
cose, and insulin all rose rapidly (fig. 2). A highlysignificant reduction in the increase of plasma-glucagonand glucose was caused by prior administration of
atropine. The mean reduction in glucagon was 33-0%±6-3 (P<001) and in glucose was 39-6% ± 70(P<0005). This reduction was observed in all fivevolunteers studied and was statistically significant(P<005, paired t test) in four. Insulin levels, ratherunexpectedly, showed a 44-5 % ± 10-8 (P<0-02) greaterrise during the arginine infusion after atropine.The rise in glucagon during insulin hypoglycaemia
in the three groups of patients is shown in fig. 3. The
peak glucagon increment was 168 ± 34 pg. per ml. inthe preoperative duodenal-ulcer patients and 173 ± 20pg. per ml. in those who had a selective vagotomy.Patients with a truncal vagotomy showed a very muchsmaller peak glucagon rise of only 81 ± 15 2 pg. perml. The difference between the glucagon responsesafter the two types of vagotomy was most apparentat the 50, 60, and 75 minute points (P<0.01). The
glucose fall was not significantly greater in the truncal-vagotomy patients, however. The lowest blood-glucosevalues occurred at 40 minutes, being 28 ± 3 -3 mg. per100 ml. for preoperative patients, 28 ±2-7 mg. per100 ml. for selective-vagotomy patients, and 26 ±3-1ml. per 100 ml. for patients who had had a truncalvagotomy.
Discussion
The anatomical evidence for autonomic innervationof the islets of Langerhans is very strong, but it hasoften been ignored in previous work on islet-cell func-tion. Evidence that catecholamines caused insulin
suppression (a receptor) or stimulation (&bgr; receptor),!’for example, was thought to be an aspect of adrenalmedullary function rather than an effect of direct sym-pathetic innervation of the pancreatic &bgr; cell. Our re-sults show that the parasympathetic, or vagal, innerva-tion of the pancreas has a significant influence on thealpha cell in man. Administration of atropine reducesfasting plasma-glucagon, and total vagal section greatlyimpairs the glucagon response to hypoglycæmia. Nochange in resting blood-glucose or significant increasein insulin hypoglycæmia is seen with the reduced
glucagon levels, and this may be considered surprising.However, there are many regulatory influences on
blood-glucose, and any of these may act to prevent afall. For example, direct stimulation of the sympa-thetic innervation of the liver can rapidly mobilisehepatic glycogen,12 and this effect can also be producedby elevating circulating levels of catecholamines.13 Themaintenance of blood-glucose is probably a " belt andbraces " situation where removal of just one mechan-ism may have little effect. Glucagon may thus playa significant role in elevating glucose in normal
circumstances, but compensation could occur when itsrelease is chronically suppressed. In some individualsor circumstances such compensation may fail-indeedreactive hypoglyca2mia is a recognised complication ofvagotomy and pyloroplasty.14 Not only did the aboli-tion of vagal tone by atropine result in diminishedglucagon release and a smaller glucose rise after
HOMEOSTASIS STRESS
Fig. 4-Hypothesis explaining the dual role of autonomic inner-vation of the pancreatic alpha-cell, homœostatic controlbeing parasympathetic and control in stress sympathetic.
arginine infusion, but it also caused a significantlygreater insulin response. The effect on insulin is un-expected because in the isolated pancreas studiesacetylcholine stimulates insulin release and in-vivoatropine or vagotomy can block reflex insulin release,15suggesting that this insulin release is caused by theparasympathetic innervation. It may be, however,that the parasympathetic system can cause eitherinsulin release or insulin inhibition, depending on thecircumstances. This theory would be analogous insome respects to the opposing actions on insulinrelease of the a and &bgr; receptors of the sympatheticsystem. The finding of greater insulin release afteraminoacid stimulation with atropine suggests another
possible mechanism for the reactive hypoglycsmiathat may occur after meals in the vagotomised patient.The effects of vagotomy per se on the function of theendocrine pancreas have not been extensively studied,and the long-term metabolic effects are unknown. Thepotential complications should now perhaps be con-sidered a significant reason for preferring the operationof selective vagotomy, and preservation of the vagalinnervation of the pancreas.
In the adrenalectomised calf splanchnic-nervestimulation can cause the plasma-.glucagon to rise veryrapidly to over 3000 pg. per ml. within 10 minutes’;many times higher than the peak glucagon level
occurring in insulin hypoglycæmia.6 Similar dramaticrises have been observed in primates put undersudden stress,t6 and glucagon is increased in stress inman.17,18 This effect is probably mediated by the
direct sympathetic innervation of the alpha cell. Thusthere seems to be a dual autonomic control of the
pancreatic islets. A hypothesis for the roles of alphacell innervation is shown in fig. 4. The potentialimportance of this autonomic innervation is seen inthe glucagon response to hypoglycæmia in the calf,which can be practically obliterated by autonomicblockaded In the 19th century all bodily functionswere thought to be controlled by nervous reflexes, butthese ideas were largely forgotten with the discoveryof the hormones. Perhaps the pendulum has swungtoo far.
Dr J. D. N. Nabarro gave considerable encouragement andhelp in organising these studies. We thank Mrs S. Mitchell.

549
Mrs S. Jones, and Mrs E. Brocklehurst for technical assistance.S. R. B. was in receipt of a Medical Research Councilclinical research fellowship, and support was received fromthe British Diabetic Association and the Peel Trust.
Requests for reprints should be addressed to S. R. B.
REFERENCES
1 Langerhans, P. M.D. thesis, Berlin, 1869 (translated by H.Morrison). Baltimore, 1937.
2. van Campenhout, E. Archs Biol. Liège, 1927, 37, 121.3. Munger, B. L. in Glucagon (edited by P. J. Lefebvre and R. H.
Unger); p. 429. Oxford, 1972.4. Renold, A. E. Diabetes, 1971, 21, suppl. 2, p. 619.5 Iverson, J. ibid. 1973, 22, 381.6. Bloom, S. R., Edwards, A. V., Vaughan, N. J. A. J. Physiol.,
Lond. 1974, 236, 611.7. Bloom, S. R., Edwards, A. V., Vaughan, N. J. A. ibid. 1973, 233,
457.8. Hollander, F., Gastroenterology, 1948, 11, 419.9. Bloom, S. R. Br. med. Bull. 1974, 30, 62.
10. Hoffman, W. S. J. biol. Chem. 1937, 120, 51.11. Porte, D., Robertson, R. P. Fedn Proc. 1973, 32, 1792.12. Edwards, A. V. J. Physiol., Lond. 1972, 220, 315.13. Edwards, A. V., Silver, M. ibid. 1972, 223, 571.14. Goligher, J. C., Pulvertaft, C. N., Irvin, T. T., Johnston, D.,
Walker, B., Hall, R. A., Wilson-Pepper, J., Matheson, T. S.Br. med. J. 1972, i, 7.
15. Wood, S. C. Am. J. Physiol. 1972, 223, 1424.16. Bloom, S. R., Daniel, P. M., Johnston, D. I., Ogawa, O., Pratt,
O. E. Q. Jl exp. Physiol. 1973, 58, 99.17. Bloom, S. R. Postgrad. med. J. 1973, 49, 607.18. Wilmore, D. W., Moylan, J. A., Pruitt, B. A., Linsey, C. A.,
Faloona, G. R., Unger, R. H. Lancet, 1974, i, 73.
CHANGES IN CORTISOL METABOLISM
FOLLOWING RIFAMPICIN THERAPY
OWEN M. EDWARDS
J. M. GALLEYR. J. COURTENAY-EVANS
JOHN HUNTERALEX D. TAIT
Department of Investigative Medicine, University ofCambridge, and Addenbrooke’s Hospital,
Hills Road, Cambridge
A patient with Addison’s diseaseSummary required increased corticosteroid
dosage whilst receiving rifampicin. The pharmaco-logical half-life of cortisol was reduced, but returnedto normal when rifampicin was stopped. Cortisol-
production rates in four patients with pulmonarytuberculosis rose during treatment with rifampicin, asdid urinary D-glucaric-acid excretion, an index of livermicrosomal-enzyme activity. The alteration of thecorticosteroid requirement in the patient with Addi-son’s disease and the elevation of the cortisol-produc-tion rates were attributed to increased cortisol cata-bolism following hepatic microsomal-enzyme induc-tion by rifampicin.
Introduction
RIFAMPICIN, one of the group of macrocyclic anti-biotics produced by Streptomyces mediterranei, isnow recognised to be of great value in the treatmentof tuberculosis 12 Side-effects are infrequent, butthere may be a transient rise in the level of serum-transaminases 2 or frank hepatitis.3 We report a pre-viously unrecognised effect of rifampicin-increasedcatabolism of cortisol, probably the result of hepaticmicrosomal-enzyme induction. This led to greatdifficulties in the management of a patient with
pulmonary tuberculosis and Addison’s disease. Wedescribe the clinical course of this patient and thesubsequent study of the effect of this drug on cortisolmetabolism of four patients with pulmonary tuber-culosis.
Case-reportA 23-year-old man complained in April, 1972, of a year
of progressive weight-loss, increasing lassitude, and frequentattacks of epigastric pain, associated with vomiting. Atthe age of 4 years, he had had pulmonary tuberculosis. Theblood-pressure was 80/50 mm. Hg standing and 90/70mm. Hg lying. There was extensive buccal pigmentation.Physical examination was otherwise normal.
Biochemical investigations showed that plasma sodiumwas 130 meq. per litre, potassium 5’2 meq. per litre, andbicarbonate 14 meq. per litre, blood-urea was 55 mg. per100 ml. A tetracosactrin test was performed 4; the basalplasma-cortisol was 6 ju.g. per 100 ml. and did not rise.The basal urinary 17-oxogenic steroids were 4’9 mg. per24 hours and 17-oxosteroids 7-6 mg. per 24 hours. Afterintramuscular administration of corticotrophin (40 i.u.
daily for 3 days) the values were 7-3 and 1-6 mg. per 24
hours, respectively.Plain abdominal X-ray revealed no adrenal calcification.
A chest X-ray showed an increase in the apical infiltrationwhen compared to previous films, but sputum cultures werenegative.
Treatment was started with streptomycin 0-75 g. daily,isoniazid 300 mg. daily, and rifampicin 600 mg. daily,together with fludrocortisol 0’2 mg. daily and cortisoneacetate 50 mg. daily as steroid-replacement therapy. The
patient failed to improve, having further attacks of abdomi-nal pain and vomiting. On one occasion, the plasma-sodium fell to 124 meq. per litre, potassium 5’7 meq. perlitre, and chloride 85 meq. per litre, and the blood-urearose to 72 mg. per 100 ml. The plasma-sodium concen-tration remained low, between 125 and 129 meq. per litre.When dexamethasone 2 mg. daily was substituted for corti-sone acetate, an addisonian crisis followed, for which itwas necessary to administer intravenous hydrocortisonehemisuccinate and physiological saline solution. In con-
sequence, the cortisone acetate was subsequently increasedto 100 mg. daily in divided doses and the fludrocortisolto 0-4 mg. daily. On this dosage symptoms disappeared,the blood-pressure rising to 110/70 mm. Hg with no pos-tural fall. The plasma sodium concentration rose to 138meq. per litre, potassium 4’3 meq. per litre, and bicarbon-ate 23 meq. per litre, and the blood-urea fell to 23 mg. per100 ml. There was no evidence of steroid overdosage.The pharmacological half-life of cortisol was measured 6
and was found to be much reduced at 58 minutes (normal75-120 minutes).The same treatment was continued and the patient
remained clinically well, with no evidence of steroid over-dosage, the range of blood-pressure being between 120/70and 130/85 mm. Hg. ’Plasma-electrolyte concentrationswere also normal. After 8 months the patient becamenauseated; this was attributed to the rifampicin, which wasstopped and ethambutol substituted for it. A month laterthe blood-pressure was 170/100 mm. Hg and there wassome facial mooning. The dosage of cortisone acetate andfludrocortisol was reduced in stages to 37’5 mg. and 0’1 1mg., respectively. The blood-pressure then returned to
normal and the facial changes disappeared. The pharma-cological half-life of cortisol was repeated and found to be82 minutes.The urinary excretion of D-glucaric acid was measured
when the patient was taking rifampicin, when it was raisedat 33 plmol per 24 hours, and also when he was onethambutol, when it had fallen to 15 jumol per 24 hours(normal range 2-20 ,mol per 24 hours).