Use of linezolid for complicated drug-resistant TB: experience inHIV infected and uninfected
Click here to load reader
description
Transcript of Use of linezolid for complicated drug-resistant TB: experience inHIV infected and uninfected

Jennifer Hughes
msfb-khayelitsha-
Background
Treatment outcomes for multi-drug resistant TB (MDR-TB) in South Africa are poor, with a treatment success rate of <50%. Existing treatment options are
severely limited for patients with extensively drug resistant TB (XDR-
TB), resulting in even worse outcomes and significant early mortality, particularly among HIV-infected individuals.
Linezolid has been shown to be effective in the treatment of DR-TB in combination with second line drugs. Access to the drug for many patients is
severely limited due to the exorbitantly high cost.
Khayelitsha township is situated 30 km from Cape Town and has a population
of more than 500,000. Antenatal HIV prevalence was 33% in 2010; ~6,000 TB
cases are diagnosed annually, with 73% of TB patients co-infected with HIV. An estimated 400 patients are infected with DR-TB each year, with 54% actually
diagnosed. A majority (>70%) of DR-TB patients are managed at primary care
level as part of the decentralised DR-TB programme in Khayelitsha.
Between July 2011 and Feb 2013, fourteen patients (4 HIV positive) started a linezolid containing regimen for the following indications:
• 9 patients had pre-XDR or XDR TB;
• 5 patients had standard M/XDR treatment failure.Median treatment duration with linezolid: 8 months (range: 1 – 20 months)
Of the four HIV-infected patients:
INTERIM
TREATMENT
OUTCOMES:
Aim
In order to ultimately improve treatment outcomes, we aim to describe the use of linezolid (LZD) within individually tailored treatment regimens for selected
M/XDR-TB patients, including HIV infected patients requiring antiretroviral
therapy (ART).
13 patients (4 HIV positive)on linezolid >3 months
10 (77%) culture converted and still
culture negative;
treatment ongoing(3 HIV positive)
2 (15%) treatment failure after:
- 8 months (HIV
negative)-9 months (HIV
positive)
1 (8%) potential treatment failure: (HIV
negative), no culture
conversion after 5 months on LZD;
treatment ongoing
CD4 count at LZD initiation:
• CD4 >350 in 3 patients
• CD4 113 in the fourth patient
On ART at linezolid initiation:• 3 on first-line ART (d4T or AZT, 3TC,
EFV)
• 1 on second line ART (TDF, 3TC, Aluvia)
69
6960
41
0
20
40
60
80
100
0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24
Perc
enta
ge A
live
Months from diagnostic sputum sample
Rif mono MDR, no SL res MDR plus SL res
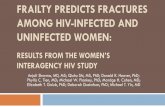
Results
Figure 1: DR-TB mortality rates, Khayelitsha 2009 cohort
Use of linezolid for complicated drug-resistant TB: experience in HIV infected and uninfected patients in Khayelitsha, Cape Town
Jennifer Hughes1, Helen Cox1,2, Johnny Daniels1, Vivian Cox1
1Médecins Sans Frontières, Khayelitsha, South Africa; 2University of Cape Town, South Africa
Methods
Candidates are then presented to a local Clinical Advisory Committee who consider:
� clinical status and comorbid conditions (with concurrent medications)
� history of exposure to TB drugs� ART regimen
� social circumstances and treatment adherence record
� laboratory results of drug sensitivity testing and genotyping� availability of existing second-line drugs (including capreomycin and PAS) and
other group 5 drugs such as clofazimine and linezolid
The initial dose of linezolid is 600 mg once daily orally, with dose adjustment
through treatment as necessary. All other drugs are dosed according to South
African national guidelines. All HIV-infected patients are fast tracked for ART regardless of CD4 count, and ART regimens are modified according to known or
possible interactions with second line TB drugs.
Summary
•Addition of linezolid to individually tailored treatment regimens for DR-TB results in high sputum culture conversion and an improved chance of potential
cure.
•Adverse events were significant but manageable with close treatment monitoring. HIV infection and ART do not appear to reduce the efficacy of
linezolid nor result in increased adverse events.
•Restricted access to linezolid due to prohibitively high cost limits the number of patients who may be offered a potentially effective treatment regimen, thereby
leaving a majority of DR-TB patients with an extremely poor prognosis; high risk
of mortality; and ongoing transmission of highly resistant TB strains in the communities where they live.
Acknowledgements
• City of Cape Town Health
• Western Cape Province
• Stellenbosch University
ADVERSE EVENTS:Candidates for linezolid are identified among patients diagnosed with DR-TB in any of the 10 primary care clinics
in Khayelitsha and the following inclusion criteria:
• diagnosis of (pre)-XDR-TB (i.e. MDR-TB with additional
fluoroquinolone and / or second-line injectable resistance)
• failure of standard MDR treatment regimen despite good adherence to treatment (i.e. no culture conversion after 6
months or culture re-conversion to positive anytime)
• National Health Laboratory Service
• Busisiwe Beko (DR-TB counsellor)
• Lizo Nobanda TB Centre staff
Adverse Event Patient Description Outcome
ANAEMIA
2 patients, both
HIV negative
• One mild (Hb drop from 11.2 to 9.7 over one month)
• One severe (Hb drop from 13.8 to 6.1 over two months)
• Resolved without dose change; (Hb 12.0 two months
later)
• Blood transfusion; LZD dose reduction to 300mg; (Hb
maintained >11.0 over next five
months)
NEUROPATHY
2 patients, both
HIV positive
• Peripheral neuropathy after 3 months on LZD (also on
D4T)
• Possible optic neuropathy
after 5 months on LZD (also
insulin-dependant diabetic)
• LZD withdrawn and D4T changed to TDF; symptoms
resolved 5 months later
• LZD withdrawn after 8
months, ophthalmology review
pending
therapy (ART). positive)
both now deceased
treatment ongoing
581
503
92
140
100
200
300
400
500
600
700
No. MDR cases diagnosed
No. MDR with second line DST done
No. pre-XDR, XDR, and MDR Tx failure
Started Linezolid
Num
ber
of patients
Potentially
eligible to receive
linezolid
Figure 2: Khayelitsha DR-TB patients diagnosed 2010 – 2013