Understanding the causes and symptoms of IBD · What is IBD? IBD is a chronic long-term...
Transcript of Understanding the causes and symptoms of IBD · What is IBD? IBD is a chronic long-term...
16 Nursing Times 12.11.14 / Vol 110 No 46 / www.nursingtimes.net
Nursing PracticeReviewGastroenterology
Keywords: Inflammatory bowel disease/Aetiology/Diagnosis ●This article has been double-blind peer reviewed
Abdominal pain is a feature of inflammatory bowel disease
Author Veronica Hall is consultant nurse gastroenterology, Royal Bolton Foundation Trust. Abstract Hall V (2014) Inflammatory bowel disease 1: understanding the causes and symptoms of IBD. Nursing Times; 110: 46, 16-19.This two-part series provides general nurses with key information on inflammatory bowel disease (IBD). As this long-term condition can seriously affect patients’ quality of life, it is vital nurses know what causes it, recognise the symptoms and understand how best to treat it. Part 1 explores the aetiology, pathophysiology, signs and symptoms, and assessment of IBD, while Part 2, which will be published next week, looks at managing patients and the nurse’s role in the delivery of care.
A recent audit assessing gastro-intestinal ward nurses’ knowl-edge about inflammatory bowel disease (IBD) high-
lighted a poor knowledge base (Sephton et al, 2013); this was an unexpected finding. Further work compared the IBD know-ledge of these nurses with that of respira-tory ward nurses, with little difference identified between the two groups (Sephton et al, 2013). It is vital nurses caring for patients with IBD understand how this long-term condition affects health and quality of life, and have the appropriate knowledge and skills to pro-vide effective evidence-based care.
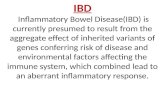
What is IBD?IBD is a chronic long-term inflammatory condition of the bowel and is generally
5 key points
1 Inflammatory bowel disease
(IBD) is a long-term condition
2The condition generally
presents in adolescents or people who are in their 20s
3Reported incidence
rates of IBD are increasing
4Incidence rates in Western
countries are higher than those in developing countries
5Diet has not been proven to
be a cause of IBD
used to describe ulcerative colitis (UC) and Crohn’s disease (CD). These are chronic disorders characterised by gastrointestinal inflammation (Orchard et al, 2011). There is no known cause for IBD but we do know that environmental factors, the immune system and genetic factors play a part in the disease (Hanauer, 2006).
IBD affects all ages but commonly presents in adolescents and people in their early 20s; this then impacts on their fertile reproductive years as well as quality of life. Men and women are diagnosed in equal numbers (IBD Standards Group, 2013). The condition is incurable and treatments aim to induce remission and reduce symptoms, thereby improving quality of life.
IBD is unpredictable and characterised by exacerbations and remission. Exacerba-tions are referred to as a relapse or “flare-up” when the disease is active (IBD Stand-ards Group, 2013). The pattern of relapse and remission can vary from patient to patient, and in severity and duration. The unpredictable nature of the condition can make some aspects of life very difficult, including planning anything from a simple shopping trip to a major holiday. Remission is defined as complete resolu-tion of symptoms plus mucosal healing, identified by endoscopic imaging such as ultrasound or a magnetic resonance imaging (MRI) scan (Hommes et al, 2012).
More than 50% of patients with CD will undergo surgery within 10 years of diagnosis (IBD Standards Group, 2013). The lifetime risk of needing surgery may be as high as 70-80% in CD and 20-30% in UC, depending on the severity of the
In this article... Causes of inflammatory bowel disease (IBD) Groups that appear to experience higher rates of IBD Symptoms of Crohn’s disease and ulcerative colitis, forms of IBD
Inflammatory bowel disease can have a negative impact on a patient’s quality of life. Understanding the condition and its aetiology will help nurses provide optimal care
Understanding the causes and symptoms of IBD
INflAmmAToRy BoWel DISeASe: PART 1 of 2
www.nursingtimes.net / Vol 110 No 46 / Nursing Times 12.11.14 17
Alam
y, Ca
ther
ine
Holli
ck
TAble 1. moNTReAl ClASSIfICATIoN foR ulCeRATIve ColITIS Classification Distribution Description
E1 Proctitis Involvement limited to the rectum
E2 Left-sided Involvement limited to the proportion of the colon distal to the splenic flexure
E3 Extensive Involvement extends proximal to the splenic flexure and includes pancolitis. Disease affects the whole large intestine
Source: Satsangi et al (2006)
disease and its location in the gastrointes-tinal tract (Mowat et al, 2011). Surgery is required to manage complications that are non-responsive to medical therapy or potentially life threatening, such as a com-plete blockage or perforation of the bowel. In UC there is also an established link between IBD and a greater risk of devel-oping colorectal cancer, which is increased by the extent, duration and severity of the IBD (IBD Standards Group, 2013).
epidemiology The prevalence of IBD in the UK is 400 per 100,000 people; it is estimated that there are approximately 240,000 people in the UK who have the condition (Mowat et al , 2011). The incidence of CD in the UK increased markedly between the 1950s and the 1980s and it has continued to do so, albeit at a slower rate (Mowat et al, 2011). This increase is not thought to be due to an increase in incidence reporting.
ulcerative colitis UC is an inflammatory condition that affects the colon and rectum. It is sug-gested that it may be an autoimmune con-dition. The epithelial barrier in the gut plays an important role in the mucosal immune system (MIS); the single layer of epithelial cells maintains the integrity of the intestinal mucosa and provides defence against micro-organisms.
The epithelial cells are constantly exposed to antigens, which are part of the
natural flora of the gut, but MIS down reg-ulates its response to these antigens and stops an inflammatory response. With IBD there is a dysfunction in the regulation of this response, exposure to normal flora triggers an immune response resulting in inflammation and tissue damage (Fig 1). Some researchers believe an immune response to a viral or bacterial infection may fail to “turn off ” once the infection has resolved and so continues to cause inflammation (Hanauer, 2006).
Genetics may also play a part in the development of UC and the condition is linked to environmental factors, such as where patients live. As an example, the condition is more common in urban areas of northern parts of Western Europe and North America (Podolsky, 2002). The effects of air pollution and certain diets have been studied but no factors have been identified so far.
Symptoms The symptoms of UC usually include: » Bloody diarrhoea; » Mucopurulent discharge;» Urgency to defecate.
Patients may also experience:» Faecal incontinence; » Cramp-like abdominal pain; » Discomfort around the left iliac fossa,
usually relieved by defecation. As the severity of UC increases, patients
may experience nocturnal diarrhoea. Sys-temic symptoms including fever, malaise and anorexia are associated with acute severe colitis – a medical emergency.
The most feared complication of UC is the development of toxic megacolon. It occurs as a result of extension of the inflammation beyond the submucosa into the muscularis (muscular layer of the bowel responsible for peristalsis), causing loss of contractility and resulting in a dilated colon. Dilation of the colon is asso-ciated with a worsening of patients’clinical condition and development of fever. It is associated with mortality and the patient may require a colectomy.
Anal complications such as excoriation and fissures (tears in the skin around the anal canal) can accompany severe disease but anything more complex than simple fissures should raise a suspicion of the presence of CD.
DiagnosisAn IBD diagnosis is confirmed by clinical evaluation and a combination of haemato-logical, endoscopic, histological or imaging-based investigations. With UC, the diagnosis should be made based on: » Clinical suspicion; » Appropriate macroscopic findings on
sigmoidoscopy or colonoscopy;» Histological findings on biopsy; » Stool examinations that have tested
negative for infectious agents (Mowat et al, 2011).UC can vary in terms of the extent of
bowel affected and the severity of the
Normal colon
Goblet cellsAbsence of goblet cells
Crypt distortion and abscess
Ulcerative colitis
A�ects mucosal layer only
fig 1. HISToloGy of ulCeRATIve ColITIS
“Work in a number of fields before choosing to specialise”Ann Regan p25
18 Nursing Times 12.11.14 / Vol 110 No 46 / www.nursingtimes.net
inflammation. It is classified as:» Remission;» Mild;» Moderate; » Severe.
UC starts in the rectum and extends uppermost in a continuous, confluent manner. Atypical cases not involving the rectum (usually a sign of CD) can be seen in children (Stange et al, 2006). This variant can pose a dilemma for clinicians who need to rule out CD by undertaking bowel investigations. Approximately 5% of patients with IBD affecting the colon are unclassifiable after clinical, radiological, endoscopic and pathological investiga-tions, because they have some features of both UC and CD. This is termed “IBD, type unclassified” (Dignass et al, 2012).
The distribution of UC is classified by the Montreal classification (Satsangi et al, 2006); it is important to know the distribu-tion of the disease so treatment and man-agement can be tailored appropriately. The classification is outlined in Table 1.
Crohn’s disease The features of UC and CD have similarities but are distinguishable. Crohn’s disease can affect any part of the gastrointestinal tract with patchy or discontinuous inflamma-tion, commonly described as skip lesions. It is potentially an aggressive and progressive disease, which can lead to complications such as perianal fistulas.
Both inflammation and fibrosis can lead to a narrowing of the lumen of the bowel, causing intestinal strictures that may lead to obstructive bowel symptoms. Strictures can progress to perforation of the gut wall and abscess formation. Management involves establishing whether the stricture is fibrotic or inflam-matory so the most appropriate treatment can be given.
CD can be further characterised by loca-tion, as well as the nature or pattern of the disease. The location could: » Be confined to the terminal ileum
(terminal ileal); » Be confined to the colon (colonic);
» Affect both the ileum and colon (ileo-colic);
» Affect any other part of the upper gastrointestinal tract (upper gastroin-testinal).The pattern of CD can be characterised
as follows:» Inflammation;» Formation of strictures in the gastro-
intestinal tract; » Formation of fistulas connecting
parts of the bowel, or connecting the bowel to organs such as the bladder and vagina.The classification of CD is outlined in
Table 2.
Causes CD is more common in developed parts of the world, such as the UK and the US, and the incidence has increased considerably in the UK between the 1950s and 1980s; since the 1980s, however, it has continued to rise at a much slower rate. This increase suggests some link to Western lifestyles but the reason for this is unclear (Gunesh et al, 2008; Armitage et al, 1999).
There is also evidence to suggest genetics plays a role in the development of CD and a familial link has been identified. Twin studies have confirmed this, with 50% concordance in identical twins with CD (Xavier and Podolsky, 2007). CD is more common in some ethnic groups, such as Caucasians and Ashkenazi Jews, but there has been an increased incidence in Asian people migrating to the developed world, which supports the view that both genetics and environment have a role (Hanauer, 2006) in the disease development.
An autoimmune response and history of a previous bowel infection, as described in the section in this article on UC, may also play a part, and some researchers have linked a virulent form of E coli with CD (Rampton, 2010).
Smokers are twice as likely to develop CD compared with non-smokers, and smoking may aggravate symptoms. Stress may also trigger relapses (Stange et al, 2006). Diet has no known pathogenic
triggers but CD often improves when ordi-nary food is removed and replaced with a liquid formula diet.
Symptoms Symptoms can vary depending on the severity and location of the condition, and may be associated with signs of malnutri-tion and weight loss. Patients usually expe-rience diarrhoea, which may contain blood if there is rectal involvement. If the ilium in the upper gastrointestinal tract is involved, it is unusual to have bloody diarrhoea but fat, bile and salt may be malabsorbed, leading to pale stools that are difficult to flush away or stools that are watery.
Abdominal pain may be related to oedema of the bowel wall or stricture for-mation. If the pain is due to strictures, symptoms usually occur one or two hours after eating and may be associated with abdominal bloating. Important signs of CD are as follows:» Perianal disease;» Presence of an abdominal mass; » Growth failure in children (Stange et
al, 2006).
extraintestinal manifestations Extraintestinal manifestations (EIMs) are present in both UC and CD they relate to areas outside the bowel and commonly occur with active luminal disease (Orchard et al, 2011). The most common EIMs affect the skin, musculoskeletal system, eyes and hepatobiliary system. The IBD Standards Group (2013) states that a named rheuma-tologist and ophthalmologist in IBD ser-vices should be involved in the manage-ment of EIMs and, in many circumstances, it is also necessary to engage with a derma-tologist.
Skin EIMSkin EIMs affect 2-34% of patients with IBD (Ardizzone et al, 2008). The most common is erythema nodosum, which usually occurs on the shin region of the legs and presents as painful pink nodules around 2cm in diameter that fade to blue (Fig 2). They are usually associated with flare-ups and treatment is of the underlying disease.
Pyoderma gangrenosum has a preva-lence of 0.4-2.0% (Orchard et al, 2011) and is characterised by pain that precedes the development of pustules. The pustules can develop into necrotic ulcers, which appear mainly on the lower leg but can also occur on the abdomen and elsewhere (Fig 3).
Musculoskeletal EIM Musculoskeletal EIMs in the form of arthritis can affect the axial or the
Nursing PracticeReview
TAble 2. moNTReAl ClASSIfICATIoN foR CRoHN’S DISeASeAge at diagnosis Location Behaviour
A1 <16yrs L1 – Ileal B1 – Inflammatory
A2 17-40yrs L2 – Colonic B2 – Stricturing
A3 >40yrs L3 – IleocolonicL4 – Isolated upper gastrointestinal disease
B3 – Penetrating+p perIanal disease
Source: Satsangi et al (2006)
www.nursingtimes.net / Vol 110 No 46 / Nursing Times 12.11.14 19
For more on this topic go online... Best practice in colorectal cancer care
Bit.ly/NTColorectalCancer
peripheral joints. Those affecting the axial skeleton include ankylosing spondylitis and sacroileitis, which have a prevalence of 1-6% (Orchard et al, 2011). Sacroileitis is characterised by buttock pain after rest, which improves with movement. Diag-nosis is made clinically and radiologically. Ankylosing spondylitis is progressive, leading to immobility of the spine; fusion of the vertebrae results in a characteristic question-mark-shaped posture. MRI is the gold-standard diagnostic tool. Treatment involves intensive physiotherapy along with treatment of the underlying disease.
Peripheral arthritis is the most common EIM and occurs in 30% of patients with CD (Orchard et al, 2011). Type 1 arthritis is associated with active intestinal inflam-mation, it is important to treat this underlying intestinal condition. Type 2 arthritis is a more persistent type, treat-ment with immunosuppressant therapy and, sometimes, biologic therapy may be required. Type 1 and type 2 arthritis do not lead to deformation or erosion of the joints.
Ocular EIM Ocular EIMs occur in less than 10% of patients (Orchard et al, 2011). Manifesta-tions include: » Episcleritis – inflammation of the layer
between the sclera and conjunctiva. This is the most common ocular manifestation. It presents with burning, itching and the presence of dilated blood vessels at the site of inflammation. It is managed with topical steroids and treatment of the underlying disease;
» Scleritis – inflammation of the sclera
(white of the eye) is more serious and can result in visual impairment and even retinal detachment. Is it usually managed with systemic steroids, non-steroidal anti-inflammatory drugs or immunosuppressant therapy;
» Uveitis – inflammation of the middle layer of the eye, including the iris, choroid and ciliary body and can occur independent of underlying disease. It presents with painful red eyes, photophobia and blurred vision. Treatment is topical and sometimes systemic steroids are required.
Hepatobiliary EIMs Primary sclerosing cholangitis (PSC) involves fibrosis of the extra and intrahe-patic biliary tree. It is associated with UC and is most common in young males who have UC. Typically UC is mild with few flare-ups but PSC can occur years before the onset of colitis and persist even after total colectomy.
PSC can also be complicated by the development of cholangiocarcinoma and increase the risk of colorectal cancer, necessitating annual colorectal endo-scopic surveillance (Mowat et al, 2011). Specialist advice is important in the man-agement of PSC as patients may eventually require a liver transplant.
ConclusionHaving an awareness of the background of IBD can empower a nurse to deliver the most appropriate care to patients who are diagnosed with the condition. Sys-tematic holistic assessment will enable the development of a patient-centred care plan, which is embedded in the 6Cs of nursing. This will be covered in part two of this series, published next week, which will look at how best to manage the condition. NT
ReferencesArdizzone S et al (2008) Extraintestinal manifestations of inflammatory bowel disease. Digestive and Liver Disease; 40: Suppl 2, S253-S259.Armitage E et al (1999) Incidence of juvenile- onset Crohn’s disease in Scotland. The Lancet; 353: 9163, 1496–1497. Dignass A et al (2012) Second European evidence-based consensus on the diagnosis and management of ulcerative colitis Part 1: definitions and diagnosis. Journal of Crohn’s and Colitis; 6: 10, 965-990.Gunesh S et al (2008) The incidence of Crohn’s disease in Cardiff over the last 75 years: an update for 1996-2005. Alimentary Pharmacology and Therapeutics; 27: 3, 211-219. Hanauer SB (2006) Inflammatory bowel disease: epidemiology, pathogenesis, and therapeutic opportunities. Inflammatory Bowel Diseases; 12: Suppl1: S3–S9. Hommes D et al (2012) Changing Crohns disease management: need for new goals and indices to prevent disability and improve quality of life. Journal of Crohn’s and Colitis; 6: Suppl 2, S224-234. IBD Standards Group (2013) Standards for the Healthcare of People who have Inflammatory Bowel Disease (IBD). tinyurl.com/IBDStandards Mowat C et al (2011) Guidelines for the Management of Inflammatory Bowel Disease in Adults. tinyurl.com/BSGIBDGuidelines Orchard TR et al (2011) An Atlas of Investigation and Management: Inflammatory Bowel Disease. Oxford: Clinical Publishing. Podolsky DK (2002) Inflammatory bowel disease. New England Journal of Medicine; 347: 417-429. Satsangi J et al (2006) The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut; 55: 6, 749–753. Sephton M et al (2013) A Comparison of Gastroenterology and Non-gastroenterology Nurses’ Knowledge of Inflammatory Bowel Disease. tinyurl.com/ECCONursesIBDKnowledgeStange EF et al (2006) European evidence based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. Gut; 55: (Suppl 1), i1-i15.Xavier RJ, Podolsky DK (2007) Unravelling the pathogenesis of inflammatory bowel disease. Nature; 448: 427-434.
fig 2. eRyTHemA NoDoSum
fig 3. PyoDeRmA GANGReNoSum
For a Nursing Times Learning unit on assessment and management of diarrhoea, go to nursingtimes.net/diarrhoea