Ultrasound as a secondary screening tool in ... · with mammographically dense breasts because of...
Transcript of Ultrasound as a secondary screening tool in ... · with mammographically dense breasts because of...

IntroductionAlthough mammography is known to be the most effective
form of breast screening, it has limitations. In particular, it isknown tohave limitations in high-riskpatients especially thosewith mammographically dense breasts because of the radio-graphicallyoccultnatureofsuchbreasts.Itwillbepresentedthatalthoughultrasoundalsohasits limitations, itcanhaveaviableroleinthesecondaryscreeningofdensebreasts.Thepurposeofscreening will be defined and the limitations of mammographywillbedescribedwithparticularrelevancetobreastdensity.Thebenefitsandlimitationsofultrasoundasascreeningtoolwillbeevaluatedafter reviewofcurrent literatureand itwillbeshownthatthelimitationsofultrasoundcanbeminimisedtoachievethebestpossibleoutcomeforthegeneralpopulation.
The results of breast screeningBreastscreeningiswhereasymptomaticwomenareimagedfor
theearlydetectionofbreastcancerwiththeaimofreducingthemorbidityandmortalityofbreastcancer.
Itiswidelyacceptedthattheprimarymethodofbreastscreen-ing ismammographyand that theuseofultrasound is themosteffective adjunct to mammography in helping to distinguishbenignfrommalignantdisease.�,2,3,5Mammographyhasascreen-ing detection rate of between 0.20 per cent and 0.70 per centwhichispartlydependentonpatientage.5
BreastScreen Victoria, however, reports in its 200� AnnualStatisticalReport,�2thatscreeningmammographydetectsahigheraverage of 0.73 per cent of cancers. The 40-49-year-old agegroup,whichismorelikelytohavedensebreasts,isreportedashaving a 0.38 per cent detection rate. Ultrasound, as a primaryscreeningtool,isreportedtodetectapproximately0.30percentofbreastcancers.2,3,4,6
Mammography has its limitations and the use of ultrasoundas a secondary screening tool, especially in high risk patients,mustbeconsidered.3,4,5Thesensitivityofanimagingmodalityisdefinedasthepercentageofcancersdetectedamongallcancersdetected with any modality.�3 Mammography in symptomaticpatients is reported tohaveasensitivityofup to98percent inwomenwith fattybreasts.However, inwomenwithverydensebreastsitisreportedtodiminishtoalowofonly48percent,withanaverageof78percent.Thesensitivityofultrasoundinwomenwithdensebreasts isaround75percent.Theuseofultrasoundcombinedwithmammography in thesewomencan increase thesensitivity to 97 per cent.�3Therefore, it is clear that ultrasoundcanplayaroleinthesecondaryscreeningofdensebreasts.
What is a dense breast?Theinterpretationofthedensityofabreastisverysubjective.
Some studies rate the denseness of the breast according to theBreastImagingReportingandDataSystem(BIRADS)assetby
Ultrasound as a secondary screening tool in mammographically dense breasts
Kylie Griggs
MaroondahHospitalRadiologyDepartmentDaveyDrive,EastRingwood,Victoria3�35,Australia
Correspondenceemail[email protected]
Abstract Itiswellknownthatbreastscreeningisapartofoursocietyandisdesignedtoreducethemortalityandmor-bidity frombreastcancer.Mammography is the imagingmodalityofchoice inabreast-screeningenvironment.Boththedetectionrateofmammographyinascreeningenvironmentandthesensitivityofmammographyinsymptomaticwomenareknowntobegreaterthanthatofultrasound.However,afterareviewofliteraturebothofthesearesaidtoincreasewhenthetwoimagingmodalitiesarecombined.Thispaperwillpresentthatmammographyhaslimitationsinbreastimaging,especiallyinwomenwithdensebreastsandthatultrasoundcanhaveabenefitasasecondaryscreeningtoolinthesewomen.Itwillbeshownthatalthoughultrasoundalsohasitslimitations,thesecanbeminimisedwiththeimplementationofeffectiveeducationandimagingprotocols.
The paper will conclude that although further research into ultrasound as screening tool is required, its use as acomplementtomammographycanonlybeofbenefittothegeneralpopulation.
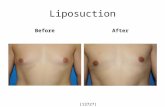
Figure 1 mediolateral oblique views of three different breast densities. Rang-ing from scattered fibroglandular densities in (A) to a heterogeneously dense breast (B) to being an extremely dense breast (C).
AustralianInstituteofRadiography
TheRadiographer2006:53(�):20–23
A B C
Clinical practice

The Radiographer 2�
theAmericanCollegeofRadiologists.Kolbet al.6definetheBIRADSclassificationofbreastdensity
asbeing:4–beinganextremelydensebreast;3–anheterogeneouslydensebreast;2–scatteredfibroglandulardensitiesinthebreastand;�–abreastthatisalmostentirelyfat.Other studies simply rate thedensityof thebreast into three
categories,beingdense,mixedandfattybreast.7,9Thedensityofthebreastisgradedbyvisualmeansonly.Itisclearthatthedefi-nitionofadensebreastneedstobedefinedobjectivelyinordertocarryoutstudiesonthesensitivityofultrasoundindensebreasts.Figure�showsvaryingbreastdensities.
It is understood that, with the introduction of digital mam-mography and computer aided detection (CAD), the densenessofabreastwillbeabletobedefinedmoreobjectively,however,the use of digital mammography may also reduce the effect ofbreastdensityonthesensitivityofmammography.6Itisreportedthat thedifferentdefinitionsofbreastdensity invaryingstudiesmaybe thecauseforvaryingresultsand,asbreastparenchymadensitycanvary in thesamepatient, thedifficultyofdefinitionwillalwaysbethere.
The limitations of mammographyMammography is based on the contrast differences between
fattyandglandulartissue.Theglandularareasinthebreastshowasareasofincreaseddensity.However,mammographically,breastcancerscanalsoshowasareasofincreaseddensity.Therefore,indensebreasts,cancersmayberadiographicallyoccult.Althoughthebiologicalbasisisunclear,itissuggestedthatthedensenessofthebreastcontributestobreastcancerrisk,4andinunderstand-ingthisfailureofmammographyinimagingdensebreastsotherimagingmodalitiesneedtobeconsidered.9
AstudybytheWesleyBreastClinic7suggestedthatthenum-berofmammographicallyoccultcancersper�000mammogramswasalmosttwiceasmanyindensebreastsasinaveragedensitybreasts,whichiswhyultrasoundmustbeconsideredasasecond-ary screening tool. Mammography also has limitations relatedtopatientage, theuseofhormone replacement therapyand thelocationofa lesion in thebreast,4 theseallaffect thesensitivityofmammography.
With much publicity today about the effectiveness of breastimagingandtheincreasedknowledgeofourpatients,itisofcon-cernthatmammographyalonecannotalwayssatisfyandreassurethepatientwhoisathighriskofbreastcancer.2
Ultrasound as a breast-imaging toolUltrasoundinbreastimagingisaveryusefuladjuncttomam-
mography as it can help to classify the nature of lesions seenin the breast. Stavros et al.�� showed in their landmark studythat sonography improves the specificity of diagnoses of breastlesions, both benign and malignant. It is the most commoncomplement to mammography and can often be necessary forcompleteevaluationofthebreast.
Ultrasound is the recommended adjunct for mammographi-callydensebreastsas fibroglandular tissueappearshyperechoicandbreastcancersusuallypresentashypoechoic.Therefore,itisthoughtthatcancerscanbewellvisualisedinthisbackground.4,6
SeeFigures2and3.Ultrasoundhasfewerlimitationswhenitcomestopatientage
andpositioning.Unlikemammography, the locationof a lesionin the breast is of decreased significance with ultrasound usu-allyprovidingeasyaccess forguidingneedlecorebiopsiesandlocalisations.
As an imaging tool, ultrasound has limitations that make itunsuitable for use as a primary screening modality. Ultrasoundcannot detect microcalcifications and is operator dependent. Itisreportedasnotbeingcosteffectiveasascreeningmodalityifperformedbyradiologists.3
Stavros3alsoreportsamedicolegaldisincentiveforperform-ingwholebreastultrasoundintheUnitedStates.Hestatesthat:
‘Aradiologistcanbeheldliableonlyforamissedcancerthatliesinthepartofthebreastthatwasexaminedsonographically.Heorshecannotbeheldliableforamissedcancerthatliesinapartof thebreast thatwasnotexaminedsonographically.Thus,certain American radiologists have tended to avoid scanningareasotherthantheimmediateareaofclinicalormammographicconcern.’3
Ultrasound,however,needsfurther investigation if it is tobeusedasasecondaryscreeningtool.
There are no hard data on the effectiveness of sonographicscreening.Ultrasoundneeds tobeexploredfurtherasasecond-ary screening tool with newer high resolution equipment andimprovedscantechnique.2,3
Madjar2conductedasmallpilotstudyonasymptomaticwomenthatshowedthatultrasoundwasafeasibleoptionforsecondaryscreening.Healsoshowedthatoperatorskillcanbe transferredwitheffectiveeducationandtraining,thuspartlyovercomingtheissueofoperatordependence.Madjaralsobelievestheextracostofultrasound is justified inhigh riskpatients, asdoesStavros.3Stavrosreportsthecostofcancerfoundbyultrasoundissimilar
Figure 2 mediolateral (A) and craniocaudal (B) views of a 52-year-old woman with heterogeneously dense breasts. The mammogram was normal while an ultra-sound (C) revealed an invasive ductal carcinoma in the right breast at 10 o’clock. The carcinoma is hypoechoic in a hyperechoic background.
Ultrasound as a secondary screening tool in mammographically dense breasts
A B C

The Radiographer22
tothecostofcancerfoundatscreeningmammographyandthatultrasoundisviablewhenthemammogramisnegativeinahighriskpatient.
Crystal et al.4 also reports the effectiveness of ultrasound asa secondary screening tool. Their study shows a 0.46 per centcancerdetectionrateforscreeningultrasound.Theybelievethatultrasoundisnotcosteffectiveforallpatientsbuthasthepoten-tial tobebeneficial forpatientswithdensebreasts.Their studyachievedahighratebecauseofthehighnumberofpatientswithdensebreasts.It isbelievedthatif therehadbeenmorepatientswithlessfattybreaststhedetectionratewouldnothavebeenashighwithultrasoundandwould, therefore,notbeascosteffec-tive.ThestudybyCrystalet al.alsousedmodernhighresolutionequipmentastheyrecognisedtheneedforthis.However,Crystalet al.recognisetheneedforfurtherstudiesinthisareatorepro-duce their results and to look at the cost effectiveness of ultra-sound.Ofcoursethecostofultrasoundasascreeningmodalitywill vary between countries depending on different regulations.Thetruebenefitfromultrasound‘cannotbedeterminedotherthanbyperformanceofarandomisedcontroltrial(RCT)usingdeathastheendpoint’.4ARCTisactuallyunlikelyintoday’stimesaswomenarebetterinformedand,therefore,thereismorelikelytobe less compliance resulting in contamination. It is known thatwomenwhovolunteerforatrialbutwhoareassignedtothecon-trolgrouparelikelytoseekinformationoutsidethetrialandwilltherefore, receive the examination anyway. This contaminationwouldlikelyaffectthedifferenceinmortalitybetweengroups.5
Kolbet al.6founda0.30percentdetectionrateforscreeningultrasoundalone.They found that the sizeandstageofcancersdetectedwasnotstatisticallydifferenttothosedetectedbyscreen-ingmammography.Theyagreethat,becauseofthelimitationsofmammography,asecondaryscreeningmethodneedstobeinvesti-gatedasfindingcancersbymammographyisjustasbeneficialasfindingthembyultrasound.Again,itisthoughtthatmorestudiesusinghighresolutionequipmentneedtobeperformedtoassesswhether the benefits of the increased detection outweigh theincreasedcostsandtimeassociatedwithsecondaryscreening.
Minimising the limitations of ultrasoundThemainconcernforultrasoundisthefactthatitissoopera-
tordependent.However,itcanalsobearguedthatmammographyis operator dependent as well. The introduction of guidelinesfor a screening program including comprehensive training andaccreditation for mammographers has helped to overcome thisproblem.IthasalreadybeenstatedthatMadjar2demonstratedin
hisstudythatgoodultrasoundtechniquecanbelearnedandtrans-ferred.Thereisnoreasonwhy,withtheavailabilityofdedicatedbreast ultrasound training programs, that the effect of operatordependencecanbeminimisedinacontrolledscreeningenviron-ment. Standards for ultrasound examinations of the breast arealreadysetbyvariousbodiessuchas theAustralianSocietyforUltrasound inMedicineand theInternationalBreastUltrasoundSchooltoensureasystematicapproachtotheimagingprocess.
Previousstudiesreportanincreasedcostofultrasoundscreen-ing because of a radiologist performing the scan.3,4,6 These areoverseas studies. The author believes that, with the quality ofsonographyinAustralia,inconjunctionwithcontinuededucationstandardsassetbytheAustraliasianSonographersAccreditationRegistry,thereisnoreasonwhyfeasiblestudiescannotbeunder-taken with sonographers rather that sonologists in this country.Thiswould reduce thepreviouslynotedhigh cost of secondaryscreening ultrasound. The time taken for screening ultrasoundand the increasedanxiety levelofpatientsundertakinganextratesthasbeenreportedasanegativeaspectinultrasoundscreen-ing. However, the time for a screening ultrasound examinationhasbeenreportedasbetween4–�5minwithanaverageofonly7min.4Also,ifthescreeningultrasoundisperformedimmediatelyfollowing themammogram, thusnegating theneed fora recall,timeissavedandtheeffectofadversepsychologicalconsequenc-esfromarecallisreduced.4
ConclusionIthasbeenshownthatscreeningmammographyhasits limi-
tationsespecially inhigh-riskpatients suchas thosewithdensebreasts.Becauseof these limitations, it is generally agreed thatasecondaryscreeningoptionneedstobeconsidered.Weneedtoimproveourabilitytodetectbreastcancersinmammographicallydensebreasttosatisfytheexpectationsofthegeneralpopulation.Ultrasound,althoughithasitsownlimitations,isaviableoptionas a secondary screening tool as it has been shown to improvecancerdetectionratesinthishigh-riskgroup.Itisknown,though,thatmoreresearchneedstobecarriedouttoproveitseffective-nessandtoreproducetheencouragingresultsalreadyobtained.
References� Breast imaging: a guide for practice 2002, National Breast Cancer Centre,
NSW.
2 MadjarH.ThePracticeofBreastUltrasound,Thieme,Stuttgart2000.
3 StavrosAT,RappCL,ParkerSH.BreastUltrasound,Lippincott,Williams&Wilkins,USA2003.
4 CrystalP,StranoSD,ShcharynskiS,KoretzMJ.Usingsonographytoscreen
Figure 3 Mediolateral (A) and craniocaudal (B) views of a 48-year-old woman with dense breasts. The mammogram was normal while the ultrasound revealed a tubular carcinoma with invasive components in the left breast at the 12.30 position. There were no clinical indications.
Kylie Griggs
A B C

The Radiographer 23
women with mammographically dense breasts. Am J Roentgenol 2003; �8�(�):�77–82.
5 GordonPB.Ultrasoundforbreastcancerscreeningandstaging.Radiolog Clin Nth Am2002;40(3):43�–4�.
6 Kolb TM, Lichy JL, Newhouse JH. Occult cancer in women with densebreasts:DetectionscreeningUS-Diagnosticyieldand tumorcharacteristics.Radiology �998;207(�):�9�–99.
7 FoxcroftLM,EvansEB,JoshuaHK,HirstC.Breastcancersinvisibleonmam-mography.Aust NZ J Surg 2000;70(3):�62-67.
8 MehtaTS.Currentusesofultrasoundinevaluationofthebreast.Radiol Clin Nth Am 2003;4�:84�–56.
9 SaarenmaaI,SalminenT,GeigerU,HeikkienenP,HyvarinenS,IsolaJet al.Theeffectofageanddensityofthebreastonthesensitivityofbreastcancerdiagnosticbymammographyandultrasonography.Breast Can Res Treat200�;67(2):��7–23.
�0 WatsonL.Theroleofultrasoundinbreast imaging. Radiol Technol;7�(5):44�–62.
�� StavrosAT,ThickmanD,RappCL,DennisMA,ParkerSH,SisneyGA.Solid
Ultrasound as a secondary screening tool in mammographically dense breasts
breastnodules:useofsonography todistinguishbetweenbenignandmalig-nantlesions.Radiology �995;�96(�):�23–34.
�2 BreastScreenVictoria.200�AnnualStatisticalReport.
�3 KolbTM,LichyJL,NewhouseJH.Comparisonoftheperformanceofscreen-ingmammography,physicalexamination,andbreastUSandevaluationoffac-torsthatinfluencethem:Ananalysisof27,825patientevaluations.Radiology 2002;225(�):�65–75.
Bibliography� International Breast Ultrasound School. International Breast Ultrasound
School guidelines for the ultrasonic examination of the breast. RetrievedOctober27,2003,fromhttp://www.ibus.org/guidelines.html
2 AustralianSocietyforUltrasoundinMedicine(ASUM).(�999).PoliciesandStatements,Breast examinationand reporting.RetrievedFebruary�4,2004,fromhttp://www.asum.com.au/open/P&S/policie_d4.htm
3 Lewis,D.TheWrittenAssignment:aguidetothewritingandpresentationofassignments,QUTPublicationsandPrinting,Queensland2002.