UHA Drug Plan P · If a Preferred or Non-Preferred Brand Covered Drug is obtained when a generic...
Transcript of UHA Drug Plan P · If a Preferred or Non-Preferred Brand Covered Drug is obtained when a generic...

MKT-0876-102915
Topa Financial CenterBishop Street Tower
T 808.532.4000 800.458.4600
F 808.522.8894www.uhahealth.com
700 Bishop Street, Suite 300Honolulu, Hawaii 96813-4100
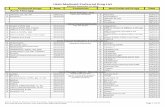
UHA Drug Plan P features a tiered co-payment structure. Your co-payment is based on the type of drug that is used to fill your prescription. Annual maximum out-of-pocket $3,850 per person; $5,200 per family(Excludes mandatory generic substitution or other DAW penalties)
*Or 20% of Eligible Charge if the Eligible Charge for a 30-day supply is over $200.00 for each original prescription or each covered refill except for medications coded by Medi-Span and approved by the FDA to treat Hepatitis B, Hepatitis C, Cancer, and HIV.
Oral chemotherapy drugs are covered in accordance with Hawaii law. Your co-payment would either be the preferred brand or generic tier (if a generic is available).
Mandatory Generic Substitution PolicyIf a Preferred or Non-Preferred Brand Covered Drug is obtained when a generic equivalent is available, the member is responsible for (i) the difference in Eligible Charge between the Preferred or Non-Preferred Brand Covered Drug and the generic equivalent, and (ii) the generic co-payment. By requesting generic drugs you can reduce your costs. Speak with your physician about the drug that is appropriate for your medical condition.
See back page for more information, or call UHA Customer Services at 532-4000, or 1-800-458-4600 from the neighbor islands
• Refills will be covered for up to twelve (12) months from the date the original prescription was written.• Drugs must be federally approved, medically necessary and obtained with a prescription from a licensed provider with prescriptive authority.
Drug Type (Non-diabetic)
Days’ Supply
ParticipatingPharmacy
Your Co-payment
Non-Participating Pharmacy Your Co-payment
Generic 30 $7* Any charges that exceed UHA’s payment of 70% of Eligible ChargePreferred Brand 30 $20* Any charges that exceed UHA’s payment of 70% of Eligible ChargeNon-Preferred Brand 30 $40* Any charges that exceed UHA’s payment of 70% of Eligible ChargeMail Order or Extended Fill Generic 90 $7* Not Covered
Mail Order or Extended Fill Preferred Brand 60 $20* Not Covered
Mail Order or Extended Fill Non-Preferred Brand 60 $40* Not Covered
Diabetic Benefits Days’ Supply
ParticipatingPharmacy
Your Co-payment
Non-Participating Pharmacy Your Co-payment
Diabetic Supplies 30 $0 Any charges that exceed UHA’s payment of 70% of Eligible ChargeDiabetic Drugs & Insulin—Generic or Preferred Brand 30 $7 Any charges that exceed UHA’s payment of 70% of Eligible Charge
Diabetic Drugs & Insulin — Non-Preferred Brand 30 $40 Any charges that exceed UHA’s payment of 70% of Eligible Charge
Mail Order or Extended Fill Diabetic Supplies 90 $0 Not Covered
Mail Order or Extended Fill Diabetic Drugs & Insulin—Generic or Preferred Brand
90 $7 Not Covered
Mail Order or Extended Fill Diabetic Drugs & Insulin— Non-Preferred Brand
60 $40 Not Covered
UHA Drug Plan PBETTER HEALTH • BETTER LIFE

30 Day Restriction On CoverageAll Covered Drugs are limited to a thirty (30) day supply, with the following exceptions:• A single standard size package may be dispensed even though a smaller quantity is prescribed for the following:
1. Fluoride, tabs and drops2. Children’svitaminswithfluoride(unbreakablepackage):TriViFlor,chewsanddrops;PolyViFlor,chewsanddrops;ViDaylin
F,chewsanddrops(andwithIron);ViDaylinF,ADCdrops(andwithIron);ViPentaF,chews;Adeflor,chewsanddrops;Luride, chews and drops
3. Nitroglycerineproducts(unbreakablepackage):NTG,(allstrengths)generic;Nitrobide;Nitrospan;Nitrostat4. Miscellaneous:Prenatalvitamins(requiringprescription);Creamsandointments(standardpackagesize);Liquids(standard
package size)5. Diabetic Supplies (unbreakable package): Syringes, needles, test strips, lancets
• Up to a sixty (60) day supply for brand name drugs (non-diabetic) or a ninety (90) day supply for generic and diabetic drugs may bedispensedformedicationsobtainedbymailorderserviceorExtendedFillProgram
Extended Fill ProgramMembersmayobtainanextendedsupplyoftheirmaintenancemedicationsatmostHawaiipharmacies.Thiswalk-inserviceallowsmembers to purchase a 60-day supply (for brand name drugs) or a 90-day supply (for generic drugs) under a single co-payment for theirprescriptionmaintenancemedication.Tostarttheservice,showyourPrescriptionIDCardwhenpickingupyourprescriptionfromyourlocalpharmacy,andaskifyouareeligibleforanextendedfill.Please visit: https://uhahealth.com/providers/search for the most current list of participating pharmacies (under Choose Specialty, select PHARMACY EXTENDED-FILL).
Drugs Not CoveredThefollowingareexpresslynotcoveredbythisdrugplan:• Injectable drugs except Lovenox,Glucagon,Imitrex,DepoProvera,Insulinandanaphylaxis(Epinephrine)kits• Non-oral immunization agents• Fertility agents• Drugs used for cosmetic purposes• Supplies, appliances and other non-drug items, except Diabetic Supplies• Drugs furnished to hospital or skilled nursing facility inpatients• Drugs prescribed for treatment plans that are not Medically Necessary• Anti-obesity drugs• Sexual function drugs• Anydrugthatmaybepurchasedwithoutaprescriptionover-the-counter(OTC),exceptasspecifiedbelow• OxyContin (or its generic equivalents ) and all other extended-release and long-acting narcotics, unless prescribed in compliance
withUHA‘sPriorAuthorizationconditionsandpaymentpolicies• DrugsforwhichPriorAuthorizationisrequiredbuthasnotbeenobtained• FordrugsinatherapeuticclassinwhichaformerprescriptiondruginthatclassconvertstoanOTCdrug,UHAreservestheright
toprovidecoverageonlyfortheformerprescriptiondrugthathasconvertedtoanOTCdrugandtoexcludefromcoverageallother drugs in that class
• New,FDA-approved,drugsduringthemandatoryefficacyandsafetyevaluationperiodassignedbyUHA,whichperiodwilllastatleast four (4) months, exceptmedicationsforHIVandcancer
• Drugsand/orDiabeticSuppliesobtainedbymailorderorextendedfillfromaNon-ParticipatingPharmacy• Non-essential,lowvalueandnovaluedrugs;someofwhicharenon-FDAapproved,someareapprovedbutholdnoidentifiable advantage over other more well-tested agents and some are considered to be of lower value by pharmacologists, professional organizations,otherauthorities,orallthree.Thislististobeupdatedannually.
Drugs And Related Supplies Obtainable Without A Prescription
CertainOTCdrugsandsupplies,althoughobtainablewithoutaprescription,arecoveredifaphysicianordersthemaspartoftheEligiblePerson’streatment,writesaprescriptionfortheitemstobepurchasedatapharmacy,andarerelatedtothepreventiveservicesmandatessetforthbythePatientProtectionandAffordableCareActof2010.
Drugs That Require Prior AuthorizationForalistofdrugsthatrequirePriorAuthorization,pleaserefertoUHA’slistofServicesThatRequirePriorAuthorizationonourwebsite at http://www.uhahealth.com/forms.asp.
How To File A Prescription Drug Claim1. PresentPrescriptionIDCardtotheproviderofservices2. Participatingproviderswillelectronicallyfileclaimsonbehalfofthemember,andpaymentismadetoprovider3. WhendrugsarepurchasedfromaNon-ParticipatingProvider,theproviderwillcompletePartBoftheclaimformandgiveittothe
memberalongwiththeprescription.ThemembershouldcompletePartAoftheclaimformandmailtheformtoUHA.Paymentswill be made to the member.
4. ContactyourproviderorUHACustomerServicestoobtainaPrescriptionDrugClaimform.Youmayalsodownloadthisformfromour website at www.uhahealth.com.
5. Claimsmustbefiledwithinninety(90)daysfromthedatethedrugispurchased
ThisinformationisintendedtoprovideacondensedexplanationofUHAdrugplanbenefits.Pleaserefertotheappropriatedrugplanridercertificateforcompleteinformationonbenefitsandprovisions.Incaseofadiscrepancybetweenthissummaryandthelanguagecontainedintheapplicableridercertification,theapplicableridercertificatewilltakeprecedence.