Bioenergetic Manipulation for the Treatment of Neurodegenerative Diseases
Treatment of Neurodegenerative Disorders
description
Transcript of Treatment of Neurodegenerative Disorders
-
Treatment of Neurodegenerative DisordersStephen P. Salloway, MD, MSButler Hospital and Brown Medical School
-
Disclosure Research Support, Consultation and Honorarium: Eisai, Pfizer, Johnson and Johnson, Forest, Lilly, Novartis, Aventis, Athena, Ono, Neurochem, Elan, Myriad and Sention, NIH, Alzheimers Association
Off label discussion of CHEI for mild cognitive impairment and Memantine for mild-moderate AD
-
Median survival of women in the longest-lived countries has increased 3 months per year since 1840Most of Us Will Be Living Out Our Full Lifespan and a Major Goal Is Healthy (Brain) AgingOeppen J et al. Science. 2002;296:1029-1031
-
Projected Prevalence of AD161412024681045.86.88.711.314.3Millions4 Million AD Cases Today Over 14 Million Projected Within a GenerationYearEvans DA et al. Milbank Quarterly. 1990;68:267-289.
-
Alzheimers Disease RisksEstablishedAgeApolipoprotein E 4 genotype 4/4 increases risk 8 fold, any 4 increases risk 3 foldChromosome 1, 14, 21 mutationsFamily history of dementia-RR 3.5Family history of Down syndrome-RR 2.7Head trauma with LOC-RR 1.8History of Depression-RR 1.8OthersLow educational level, female genderGeldmacher, 2001; Knopman, 2002
-
Age is the biggest risk factor for AD
*
Cumulative Incidence of Alzheimers Disease
-
Teaching Old Dogs New Tricks 2 year study, old beagles (7-11 years; n=48) 4 groups divided into 1) antioxidant-fortified diet, 2) program of behavioral enrichment, 3) both, or 4) neither. Discrimination and reversal learning ability decline progressively with advanced age in beagles, but the rate of decline was delayed by both behavioral enrichment and antioxidant supplementation. Behavioral enrichment and antioxidant supplementation combined were more effective than either alone.Milgram et al., Neurobiology of Aging 26 (2005) 7790.
-
Keeping Our Synapses HealthyStay mentally and physically active-read, do crossword puzzles, play bridge and games, walk, exercise, go to the gymStay involved with people and projects- socialize, pursue hobbies and volunteer work, learn new things, play music, participate in church activitiesControl risk factors-weight, BP, chol, blood sugar, stop smokingEat a balanced diet with Vit E-animals on calorie restriction live longer, low calories may decrease risk of AD. ? Red wine-resveratrol
-
Mild-Mod AD, Mod-Severe AD
-
Defining the Diagnostic Threshold for Dementia
Cognitive Continuum
Talk/Meeting: Management of Psychosis and Behavioral Symptoms in DementiaSpeakers: Donna Masterman, M.D., M.S. and Stephen Salloway, M.D., M.S.Mtg: 2001 PC ISS 410
ISS 410
-
Normal AgingPsychomotor SlowingTaking longer to do thingsA 75 year old marathon runner takes twice the time to complete the race as he or she did at age 25.Recalling names or trouble finding specific wordsWhat did I come here for?
Troublesome signsBeing repetitive and not just for emphasisNot coming up with the names or words laterNot recalling that conversations or events ever took placeNot realizing that there is a memory problem
-
Age 27Time: 2:37:07 (1st Place)1935Age 83Time: 5:42:541991John A. Kelley in the Boston Marathon
-
Ed Whitlock, Age 73 First person over 70 to break the three-hour mark. Ran Toronto Waterfront Marathon in 2:54:49, placing 26th out of 1,690 finishers. Was a runner in high school and university, then stopped running for 20 years. Began running again at age 41.Ed Whitlocks Fastest Times Since Turning 70 EVENT TIME AGE 5,000 meters 18:22 73 10,000 meters 37:33 73 15,000 meters 58:55 72 Marathon 2:54:49 73
-
Subtypes of Mild Cognitive Impairment
-
Not all patients with MCI have AD, but almost all patients with AD pass through an MCI stage
-
What is Mild Cognitive Impairment?Disorder of short-term memory (> 1.5 SD)Misplacing things a lotHard to recall messages, remember details, and appointmentsNormal functioning overall More than a nuisanceRisk factor for AD (12-15% per year)
-
Subtle Findings in MCIMMSE=26MMSE=21MCIAD
-
1/29/2004MMSE=26
-
Volume of AD Cases by SpecialtySource: NDTI (Diagnosis codes: 3310, 2900, 2901, 2902, 2903, 2904, 3109, 2912), Moving Annual Total (MAT). March 2001. Source: Market Measures, February 2000.1200IMSpecialists providing careNumber of dementia patients in physicians practiceNeuroPsych180996312160GP/FP48PCP 67%Neuro 18%Psych 8%Other 7%
-
Recommendations for ScreeningAt annual physical or when warning signs appearAsk the patient and a knowledgeable informant about any problems with memory, mood, behavior or problems drivingDo a baseline MMSE and clock drawingIf time is short do the 3 word recall during the exam and clock drawing
-
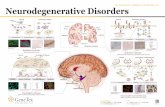
Neurodegenerative DisordersProtein dysmetabolismVulnerable cell populationsNeural systems affectedSpecific regions and neurotransmittersClinical phenotypeSystems linked to cognitive and behavioral changesDisabilityAge dependent onsetGenetic and environmental risk factorsApoE and head injury
-
The Temporal Course of Neuropathological Changes of AD in Downs Syndrome
Mann DMA. BMJ. 1997(Oct 25);315:1078-1081
-
Courtesy of Dr. Mark Mintun
-
Braak Staging of ADTrans-entorhinal (I-II)Limbic (III-IV)Isocortical (V-VI)
-
% of nl conversion rate>50% of nl 9%1-50%26%1st %50%ADMCINormalChange in Hippocampal Volume from Normal Aging through ADJack Neurology 1999;52:1397-1403
Impact - Dr. Sallowy: Title is needed for this slideAlso, the suggestion was made to insert a workup slide previous to this one.
Thanks
-
PET for the Diagnosis of DementiaMedicare GuidelinesAtypical course for AD and FTD is suspected Comprehensive eval conducted by a physician experienced in dementia PET reading done by a physician experienced in dementia imaging No prior SPECT or PET Clinical trials using PET for dx of early dementia may be covered
-
Amyloid ImagingPittsburgh compound
-
AssessmentClinical historyPrimary symptoms from patient and informantOnset and courseGradual, abruptWere there events?Determining baseline cognitive and functional ability
-
AssessmentCognitiveMemory, languageFluctuations?Activities of daily living (ADLs)IADLs, BADLs, driving, hobbiesBehavioralMood, irritability, impatience, apathyDelusions, visual hallucinations, paranoiaSubstance useSleep, appetiteDomainsIADLs = instrumental ADLs; BADLs = basic ADLs
-
AssessmentMotor and Gaitweakness, numbness, lateralizing?ParkinsonismBladder controlOther medical conditions and medicationsFamily history: dementia, psychiatric, neurological
-
Modern medicine relies on the premise of early diagnosis and treatment to prevent or delay morbidity.
*
Predicted Result of Early Treatment
No Treatment
Early Treatment
Time
Cognitive Function
-
Moderate ADAge 77Sep 1998Age 79Aug 2000Age 82Oct 2002MMSE: 19MMSE: 15MMSE: 12Age 842004MMSE 10
- *p
-
Cholinesterase Inhibitors for ADTacrine (Cognex)Donepezil (Aricept)Physostigmine SR (Synapton)Rivastigmine (Exelon)MetrifonateGalantamine
-
*
Outcomes Measured in Reminyl (galantamine HBr) Phase III Trials
-
Benefits of CHEI for ADStabilize functioning during the first year and make subsequent decline more gradualDelay time to nursing home placementMay decrease behavioral symptomsShow some benefit in moderate severe stages of AD
The CHEIs have similar efficacy but may have differences in tolerability and ease of use
-
Donepezil Pivotal Trials ADAS-cog scores in mild to moderate AD2.51.50.5-0.5-1.5-2.5-3.5ClinicalimprovementClinicaldeclineBaselineBaseline61218Study week2430Mean change from baseline ( SE)Donepezil 5 mg/dDonepezil 10 mg/dPlaceboRogers SL, et al. Neurology.1998;50:136-145.
-
*
Long-term Effects of Donepezil on Cognition: ADAS-Cog Mean Change From Baseline
0 6 12 14 26 38 50 62 74 86 98
Decline in ADAS-Cog score based on the natural history of untreated patients with moderate Alzheimers disease
-6
0
6
12
18
Improve
Decline
-
Delay Time to Nursing Home Placement
-
Most Common Side-Effects With Cholinesterase InhibitorsGastrointestinalNausea, Vomiting, Loose stools, DiarrheaAnorexia and weight lossVivid DreamingSymptoms are usually transient and dose related-titrate slowly and take with foodA small percentage become agitated on CHEIs
-
MCI - Amnestic
MCI-amnestic
52
48
32
45
44
58
48
Baseline
Early AD
55
54
80
66
67
68
72
Baseline
Moderate AD
58
52
80
75
75
75
78
Baseline
VaD
77
74
68
50
49
52
80
Baseline
FTD
72
75
60
52
53
54
80
Baseline
Profile scores
DxSpeedAttentionDelayed RecallRecognitionSpatial/ConstrLang/NamingExecutive
MCI -amnestic52483245445848
Early AD45462034333228
Moderate AD42482025252522
Vascular23263250514820
FTD28254048474620
NPH
DLB
Sheet2
Sheet3
-
Cognitive Change in the 24 week Donepezil MCI TrialP=.044P=.007(n=130)(n=132)(n=83)(n=100)*FE=fully evaluableSalloway et al. Neurology. 2004;63:651-657.ITT-LOCFFE*
-
Results of the 36 month ADCS MCI Conversion TrialConversion rate to dementia was 13% per year, 98% determined to be to ADAPOE-4 + 55.1%. Rate of conversion was significantly higher in the APOE4 positive group There was no significant effect of donepezil or vitamin E on conversion over the full 3 year study Donepezil appeared to decrease the probability of conversion for up to 18 months and delay the conversion to dementia by 6 months overallThe delay to conversion was greatest in the APOE4 positive group
-
Lancet 2004;363:2105-2115
-
Driving and DementiaNormal DrivingNo driving due to crashBad Option!
-
Driving
-
Spectrum of Neuropsychiatric Symptoms in ADMega et al, 1996
-
Helping Caregivers CopeFace the situation directlyCommon sense problem solvingGet educated and develop a support networkStructuring the home environmentFamiliar, calm environment with a predictable routineKeep it simple, limit choices Match activities to capacities and preferencesAvoid arguing and overwhelming situations and challengesDriving and home safety
-
Use of Glutamatergic Agents for Rx of Memory LossGlutamate plays an important role in memory consolidation and LTPTherapeutic approaches-NMDA agonists and antagonists, AMPA receptor modulators, glycine modulatorsMemantine is a low to moderate affinity, uncompetitive NMDA-receptor antagonist, voltage-dependent, fast blocking/unblocking kineticsBlocks the effects of abnormal glutamate activity that may lead to neuronal cell damage/loss and cognitive dysfunctionPreserves physiological activation of NMDA receptor required for learning and memorySources:Rogawski MA, et al. CNS Drug Reviews. 2003;9:275-308.Danysz W, et al. Neurotoxicity Res. 2000;2:85-97.
-
Memantine: Mod-Severe Monotherapy AD Trial28 week trial of memantine 20mg/d vs placebo in mod-severe AD, MMSE 7.9N=252OutcomesPrimary-CIBIC+ and ADLSecondary-SIB, MMSE, NPISig slower decline in the memantine group in CIBIC, ADL and SIBNo sig difference in MMSE and NPICaregiver time was sig less in the drug groupNEJM 2003;348:1333-41
-
Memantine: Mod-Severe Monotherapy AD Trial
- Memantine Plus Aricept for Mod-Severe AD28 week study, n=403, mean MMSE 10, range 5-14Aricept 10 plus memantine 20/d vs Aricept 10 and placeboHad to be on Aricept 10 mg for at least 6 months, mean duration of Aricept Rx-24 mos.Outcomes Primary- ADL and CIBIC+Secondary-SIB, NPIPatients on combined Rx declined at a sig slower rate and showed improvement on the SIBAricept-memantine combination well tolerated? Decreased benefit in the
-
Memantine Plus Aricept for Mod-Severe AD
-
What about the new preventative and disease modifying treatments?Vitamins Anti-inflammatory agentsEstrogenStatinsMood stabilizersTreatments to reduce amyloid loadAmyloid vaccineSecretase inhibitorsHeavy metal chelatorsShunting AD patients
-
New Targets for Treatment of Alzheimers Disease
-
Three approaches to Altering Brain Amyloid in Alzheimers DiseaseReduce -amyloid productionInhibit -amyloid fibrillogenesisPromote -amyloid clearance
-
New Targets for Treatment of Alzheimers Disease
-
Proteolytic Cleavages of Amyloid Precursor Protein (APP) That Produce A PeptideSelkoe DJ et al. JAMA. 2000;283:1615-1617.alpha-secretaseAbeta-42Abeta-42Abeta-40
-
Parietal neocortex, immunized ADpatient in Elan AN-1792 Trial Parietal neocortex, Nonimmunized patient at comparable stage of AD
-
The Meningoencephalitis Induced by Active Amyloid Immunization With AN-1792 Was T-Cell Mediated CD3 T-cell antibody stain shows extensive meningeal reactivity in response to AN-1792CD79a B-cell antibody stain shows no meningeal reactivity in AN-1792induced meningoencephalitisHock et al. Neuron. 2003;38:547-554.
-
Tau HyperphosphorylationArt from ADEAR
-
Improving the Treatment of DementiaDevelop routine screening for memory loss and behavior change in older peopleDiagnose and treat signs of dementia early and maintain persistent treatmentEducate caregivers about the illness, help them structure the daily routine and assist them with obtaining support over the long-termWork with determination to develop effective new treatments that dispel the angst associated with AD Build a partnership of civic leaders, scientists, clinicians, and families to wage a concerted fight against AD
-
3/15/2004MMSE=22Leaves out numbers on left side
-
3/15/2004MMSE=22
-
Picture of Alois Alzheimer--first described the disease in 1907 in a 50 year old woman. Same time as Freud. Major advance, first neurologic disease that had an organic cause--could not be treated by therapy.
Primary care practitioners provide the majority of medical care for Alzheimers disease patientsThe average PCP sees more than 48 patients per monthKey PointsAt baseline, patient was started on Aricept 5 mg/d and increased to 10 mg/d after 10 weeks. Agitation resolved 10 days after starting Aricept.At 2-year follow-up, no change in memory for the preceding 12 months was noted. At 4-year follow-up, patient resided at home, attended day care 2/week; family managed his care; gradual decline in short-term memory and ADLs; performed basic ADLs with minimal prompting; behavior problems have not returned; sister with AD not on treatment resided in a nursing home.At 4.5 year follow-up, patient remains on Aricept 10 mg/d.
Talk: Clinical Neurochemistry and NeuroimagingSpeaker: Stephen Salloway, M.D.Meeting: 2001 Board ReviewTalk/Meeting: Management of Psychosis and Behavioral Symptoms in DementiaSpeakers: Donna Masterman, M.D., M.S. and Stephen Salloway, M.D., M.S.Mtg: 2001 PC ISS 410
Mega et al, 1996, looked at the spectrum of behavioral changes seen in AD over the course of the disease. The spectrum included personality alterations, mood disturbances, perceptual disturbances such as delusions and hallucinations, vegetative symptoms and motor disturbances. Purpose: To highlight memantines properties and focus on the new target for thetreatment of AD
Key Points:Memantine is the first and only NMDA-receptor antagonist approved for the treatment of moderate to severe AD.Memantine is the first of a new class of medications for AD with a mechanism of action distinct from currently available therapies.Memantine blocks the damaging effects of abnormal glutamate activity while preserving physiological processes dependent on glutamate without causing serious side effects. (There is no evidence that memantine prevents or slows neurodegeneration in patients with Alzheimers disease.)