Treatment of chronic femoral osteomyelitis with platelet-rich plasma (PRP): A case report
Click here to load reader
Transcript of Treatment of chronic femoral osteomyelitis with platelet-rich plasma (PRP): A case report

Available online at www.sciencedirect.com
Transfusion and Apheresis Science 38 (2008) 167–173
intl.elsevierhealth.com/journals/tras
Treatment of chronic femoral osteomyelitis withplatelet-rich plasma (PRP): A case report
Ting Yuan, Changqing Zhang *, Bingfang Zeng
Orthopaedic Department, Shanghai Sixth People’s Hospital, Shanghai Jiaotong University, Shanghai, China
Received 14 October 2007; accepted 16 January 2008
Abstract
Chronic osteomyelitis is a serious problem in developing countries. A lot of patients with chronic osteomyelitis have tobe treated for a very long period and get several operations including complete debridement, antibiotic bead implant, bonegrafts, etc. However, traditional methods seem to be ineffective in some patients, who always have a high incidence ofrecurrence.
We report a case of chronic osteomyelitis in bilateral femurs, which has been treated with long time antibiotic therapy,about twenty debridements, yet the sinus remained unhealed for over four years. At the end of this period, we used PRP totreat the unhealed sinus and obtained good results. Though the mechanism by which PRP treats chronic osteomyelitis isnow unclear, the results encourage study further.� 2008 Elsevier Ltd. All rights reserved.
Keywords: Platelet; Platelet-rich plasma; Growth factor; Chronic osteomyelitis
1. Introduction
Platelet-rich plasma (PRP) is a concentration ofautologous platelets, which contains growth factorssuch as platelet-derived growth factor (PDGF)-AA,-BB, -AB; transforming growth factor (TGF)-beta1and -beta2; epidermal growth factor (EGF); vascu-lar endothelial growth factor (VEGF); and insulingrowth factor (IGF), which are known to enhancebone and wound healing [1]. Furthermore, PRPcontains high concentrations of leukocytes, which
1473-0502/$ - see front matter � 2008 Elsevier Ltd. All rights reserved
doi:10.1016/j.transci.2008.01.006
* Corresponding author. Tel.: +86 21 64369181 8062; fax: +8621 64701361.
E-mail address: [email protected] (C. Zhang).
contribute to local debridement and exhibit bacteri-cidal activities in a chronic wound. The topicalapplication of PRP in the treatment of chronicwounds appeared to be effective in the published lit-erature [2].
Chronic osteomyelitis is a serious problem indeveloping countries, and as yet there are no satis-factorily effective methods of treatment. The patho-genesis of chronic osteomyelitis is similar to that ofchronic wounds, with treatment including debride-ment of infected tissues, systemic antibiotics, andcoverage with healthy soft tissue if possible. Weapplied PRP to treat a patient with chronic osteo-myelitis of bilateral femurs after all conventionaltreatments had seemed to be ineffective, and pre-vented recurrence for a long time.
.

Fig. 1. A plain radiograph showed a lateral cortical defect andsinus. The thick callus was strong enough to support the patientto ambulate normally.
168 T. Yuan et al. / Transfusion and Apheresis Science 38 (2008) 167–173
Our search of the literature revealed that no caseof long bone chronic osteomyelitis treated with PRPhad been reported. The case that we are reportingraises questions about the mechanism by whichPRP prohibits the development of necrosis andreduces inflammatory extravasate. The patient wasinformed that data concerning the case would besubmitted for publication.
2. Case report
A 53-year-old man whose both lower extremitieswere crushed by a falling heavy steel bar wasbrought to our orthopedic emergency departmentin November 2002. His vital signs were normaland stable, and he was fully conscious. Both thighswere deformed, shortened, and swollen without anopen wound. Pulsation was felt and sensation wasnormal bilaterally. Plain radiographs showed bilat-eral femoral shaft fractures. Before surgery, tibialtuberosity tractions were placed for one week.
One week later, the patient was operated on withantegrade interlocking intramedullary nailing to fixthe bilateral femoral fractures with lateral small inci-sions to assist reduction of the fractures. Four daysafter surgery, the patient had a high fever of 40 �C,with redness, swelling and warmth around thewound, which drained pus. Dressing changes wereneeded every day because a great deal of pus was con-tinuously draining, and the canal reached the perios-teum. Bacterial culture showed methicillin resistantStaphylococcus aureus (MRSA) infection and sensi-tive antibiotics (vancomycin) was used for six weeks.
The sinus had been draining thick yellow secre-tions continuously for about one year. In January2004, radiographs showed thick bone callus aroundthe fractures and the patient ambulated normally.The left intramedullary nail was first removedbecause of symptoms in the left thigh which weremore serious than that of the right thigh. In July2004, the right intramedullary nail was removed.However, the sinuses in both thighs had been drain-ing pus after removal of the intramedullary nails,and dressing changes were needed every day.
In October 2004, surgical debridement was per-formed to remove necrotic bone and contaminatedsoft tissue, and the medullary cavity was lavagedwith antibiotic solution repeatedly. Ten days afterthis operation, the wounds of both thighs were with-out recurrence for one year.
In September 2005, swelling, redness and warmthpresented again around the wound, and abscesses
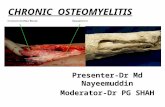
could be observed. Debridement was performedagain. During the operation, a great deal of yellow-ish pus and necrotic bone fragments were observedin the original fracture sites and there was a largesinus in the callus (Figs. 1–3). From then on, thewounds were unhealed and drained thick yellowsecretions until January 2007 (Figs. 4 and 5). Dur-ing the period between September 2005 and January2007, nineteen operations were performed, includ-ing debridement, removing dead bone and soft tis-sue, irrigation of the medullary cavity, muscle flapcoverage, implantation of local antibiotic beads,etc. But all these methods seemed to be ineffective.After each operation, the quantity of pus dischargedwas less, however, it would increase gradually untilthe next operation had to be performed.
In January 2007, the patient refused any openoperation, so we suggested the use of PRP to repairthe sinus and he agreed. Thirty millilitres of wholeblood was drawn from the elbow vein by a syringewith 5 ml citrate phosphate dextrose (CPD) toachieve anticoagulation. With a centrifuge rate of200g for 10 min, the blood was then centrifuged intoits three basic components: red blood cells, PRP,and platelet-poor plasma (PPP). Because of differen-

Fig. 2. Computed tomograph of the right thigh showed a lateralcortical defect, sequestration, and involucrum.
Fig. 3. Computed tomography of the left thigh also showedlateral cortical defect, sequestration, and involucrum.
Fig. 4. The wound in the left thigh. One forceps reached themedullary cavity through the sinus and a great deal of drainingpus was seen in the dressing.
T. Yuan et al. / Transfusion and Apheresis Science 38 (2008) 167–173 169
tial sedimentation coefficients, the red blood celllayer formed at the lowest level, the PRP layer inthe middle, and the PPP layer at the top. About fourfifths of the red cells were drawn out from the mid-dle tube (Fig. 6). The remainder was agitated forseveral seconds and centrifuged again at 200g for10 min, then the blood was centrifuged into two lay-ers, the supernatant was PPP, and the lower layerwas platelet concentrate. About three-quarters ofthe supernatant was discarded, the remainder(approximately 5 ml) was drawn into a syringe.Another syringe with thrombin and 10% calciumchloride was fit together with the PRP syringe (seeFig. 7). After cleaning the sinus with alcohol andcotton balls, PRP and thrombin/calcium chloridewas injected into the sinus with a long tube in orderto reach the medullary cavity (Fig. 8). A 3 M mem-brane was used to cover the sinus.
The patient felt that pain and swelling wasreduced the next day after the PRP application.
Two weeks later, the 3 M membrane was removed,and the wound was healed (Figs. 9 and 10). There

Fig. 5. The wound in the right thigh. There was one sinus whichreached the medullary cavity, and there was also a great deal ofpus.
Fig. 7. After the second centrifugation, PPP was drawn out fromthe lateral tube.
Fig. 6. After the first centrifugation, red cells were drawn outfrom the middle tube. Fig. 8. The mixture of PRP and thrombin and CaCl2 was
injected into the sinus.
170 T. Yuan et al. / Transfusion and Apheresis Science 38 (2008) 167–173
was no recurrence in either thigh for the next threemonths (Figs. 11 and 12). However, in March 2007,a red prominence appeared in the wound (Fig. 13)1
of the left thigh. Debridement surgery was per-formed to remove inflammatory soft tissue and
1 (For interpretation of the references in colour in this figurelegend, the reader is referred to the web version of this article.)
infected bone. PRP was injected into the sinusthrough a long tube during the operation. Twoweeks later, the wound healed again, with no recur-rence until August 2007. This time we did not injectPRP into the sinus, instead, we just changed thedressing normally for ten days and the wound wasnot healed and more and more pus was discharged.

Fig. 9. Two weeks after PRP application, the left wound healed,and no redness and warmth were apparent; the patient felt well.
Fig. 10. Two weeks after PRP application, the right woundhealed.
Fig. 11. Two months after PRP application, the wounds healedgradually, the color of the wound skin seemed close to normal.This figure shows the left wound.
Fig. 12. Two months after PRP application, the wounds healedgradually, the color of the wound skin seemed close to normal.This figure shows the right wound.
Fig. 13. Recurrence was observed in the wound of the left thightwo months after the application of PRP.
T. Yuan et al. / Transfusion and Apheresis Science 38 (2008) 167–173 171
In the end, we applied PRP like before, and thewound healed again. There has been no recurrenceup to the time this article was written in October6, 2007. There was no recurrence in the right thighafter the first PRP application (Fig. 14).
3. Discussion
It may be hematogenous infection, or surgerywhich created the access for infection for this caseresulting in chronic osteomyelitis from closed frac-tures. In the early period of infection, the reasonsthat the intramedullary nailings were not removed

Fig. 14. Three months later, the patient had no recurrence.
172 T. Yuan et al. / Transfusion and Apheresis Science 38 (2008) 167–173
and fixed with an external fixator was that externalfixation of a femoral fracture is not stable enough tobear the force of rotation and bending of the thighmuscles. An external fixator would easily lead tonon-union. Furthermore, an external fixator pre-vents function training of the thigh and might leadto stiffness of the knee. So, the removal of the intra-medullary nails was performed after a strong thickcallus formed and the patient ambulated normally.
Infection after intramedullary nailing has been aserious problem. In this case, many kinds of treat-ments had been previously applied, but were noteffective. During the operation, we observed a greatdeal of canal or sinus in most of the callus, and deadbone could be seen from the radiographs. However,it was difficult to remove all of these dead tissues,because if these were removed, the femur wouldfracture again. Furthermore, in the latter period,the patient refused any open operation under anaes-thesia. So, we had to choose minimal or non-inva-sive methods of treatment.
We attempted to use PRP to treat the patient, asthere were no alternatives to be chosen. To our sur-prise, the wound healed after PRP application.Though there was a recurrence in the left woundthree months later, the result was much better thanbefore. From September 2005 to January 2007, wehad to change dressings every day, for a great dealof pus extruded from the sinus every day, and con-tinuous redness, warmth, and pain were present.The reason that recurrence took place was thatexisting organisms and dead tissues could not beremoved because of the patient’s rejection of anyinvasive treatments. The right wound had no recur-rence for nearly ten months. So, we think PRP ishelpful to treat chronic osteomyelitis on the basis
of absolute debridements. We do not know whetherthe wound will reoccur, but the facts tell us thatapplication of PRP prevents recurrence for at leastthree months. And If PRP was not used, the woundwould never have healed for even one day.
Why is PRP helpful in the treatment of chronicosteomyelitis?
PRP contains highly concentrated white bloodcells, for the density of white blood cells are similarto that of the platelets, and after centrifugation,platelets and white blood cells drop into the samelayer. These white blood cells phagocytize organ-isms and debride dead tissues, and inhibit inflamma-tory reaction. Crovetti [2] reported that chronicwounds lack the availability of growth factor byway of decreased release, trapping, excess degrada-tion or a combination of these mechanisms. Quickgrowth factor metabolization frequently appearsbecause of the presence of a proteinase having abacterial or cellular origin. In addition, growth fac-tor reduction is a consequence of a sequestrationmechanism by fibrin sleeves that are rolled aroundthe capillaries. So, application of PRP provideshighly concentrated growth factors and white bloodcells to accelerate angiogenesis and tissue repair,inhibit the inflammatory reaction, and all the abovemechanisms may be helpful to prove the effective-ness of PRP in the treatment of chronic wounds.
Namazi [3] pointed out that PRP may be a noveltherapeutic agent in osteomyelitis. Bielecki [4]observed that PRP inhibited the growth of Staphy-
lococcus aureus, which was the most common infec-tive organism in chronic osteomyelitis and webelieved that the antimicrobial properties of PRPcan improve the treatment of infected delayed heal-ing and non-union.
Though PRP seemed helpful in the treatment ofchronic osteomyelitis, basic principles should notbeen ignored, including absolute debridement, cov-erage of soft tissue, systematic appropriate antibiot-ics, and stability of the fracture.
As an extremely inexpensive, simple and safemethod, PRP may be a novel method in chronicwounds and osteomyelitis. However, the detailedmechanisms of PRP in the treatment of osteomyeli-tis still remain unclear and large clinical trials orbasic researches are needed.
References
[1] Marx RE. Platelet-rich plasma: evidence to support its use. JOral Maxillofac Surg 2004;62(4):489–96.

T. Yuan et al. / Transfusion and Apheresis Science 38 (2008) 167–173 173
[2] Crovetti G, Martinelli G, Issi M, Barone M, Guizzardi M,Campanati B, et al. Platelet gel for healing cutaneous chronicwounds. Transfus Apheresis Sci 2004;30(2):145–51.
[3] Namazi H. Platelet-rich plasma as a novel therapeutic agentin osteomyelitis. Med Hypotheses 2007.
[4] Bielecki TM, Gazdzik TS, Arendt J, Szczepanski T, Krol W,Wielkoszynski T. Antibacterial effect of autologous plateletgel enriched with growth factors and other active substances:an in vitro study. J Bone Joint Surg Br 2007;89(3):417–20.