Traction Splint AnglTraction Splint AnglTraction Splint AnglTraction Splint Angl
description
Transcript of Traction Splint AnglTraction Splint AnglTraction Splint AnglTraction Splint Angl

64 JEMS | AUGUST 2004
PHO
TOS
CO
URT
ESY
MIN
TO R
ESEA
RCH
& D
EVEL
OPM
ENT
INC
.
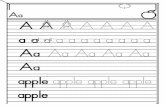
The Sager splint appliescounter-traction against theischial tuberosity medial tothe shaft of the femur.
This splint applies counter-traction to the ischial tuberosity from below the femur shaft,which can cause movement of the bone ends.

WWW.JEMS.COM | AUGUST 2004 | JEMS 65
Traction splints have been a part of ourequipment inventory for as long as EMS
has existed. Application of the traction splint isone of the most fundamental of EMT skills. Thepurpose: immobilize femoral fractures throughtraction. Application of the traction splint is be-lieved to reduce hemorrhage, secondary tissuedamage and pain. But does it make a significantimpact on patient care in the modern EMS eraor has it become an EMS relic? Now that I haveyour attention, let’s move on.
Historical reviewJohn Hilton introduced the first traction splintfor lower extremity fractures in 1860. In the1870s, Hilton’s splint was refined by notedBritish surgeon and bone setter Hugh O.Thomas. This later version of the splint came tobe known as the Thomas splint and was widelyused for treatment of femoral fractures.1
During World War I, Sir Robert Jones sug-gested using the Thomas splint to manage acutefemoral fractures.2 The advent of trench warfarehad resulted in a marked increase in the numberof open femur fractures from gunshots andjagged shell fragments. Because of this new styleof warfare, military surgeons saw a sharp in-crease in mortality secondary to these injuries.The surgeons obviously had to change their
strategy for managing these injuries, and theThomas splint seemed like the perfect tool. TheThomas splint was introduced into militarymedical practice as a method of treating obviousfemur fractures in 1916.
Following widespread usage of the Thomassplint, a significant decrease in mortality fromfemur fractures was reported. However, the de-gree to which mortality decreased is open toconjecture. Various percentages in improvedmortality secondary to use of the traction splintwere anecdotally reported—a phenomenon thatbecame known as the “Thomas splint boast.”However, in a report, renowned World War Isurgeon and British Colonel Sir Henry Graynoted that the mortality from femoral fracturesdropped from 80% in 1916 to 15.6% in 1917after the Thomas splint was used for 1,009 casesin a particular battle.3
Although the Thomas splint was introducedfor the treatment of femoral fractures, it seemedintuitive to several physicians that it would beuseful for initial immobilization of femoral frac-tures in the prehospital setting. Because of this,the American College of Surgeons Committeeon Trauma included the traction splint in itsdocument Essential Equipment for Ambulancesin the early 1970s, and it remains a mandatedpiece of equipment today.4
AN EMS RELIC? By Bryan E. Bledsoe, DO, FACEP, & Donn Barnes, LP
PHO
TOS
A.J
. H
EIG
HTM
AN

How does it work?Regardless of the type or manufacturer, the femur traction splint con-sists of a frame that extends from the proximal thigh to an area distal tothe heel. The splint has a padded portion that fits against the ischialtuberosity, which serves as the anatomical fixation point. The proximalportion of the splint may be a ring that encircles the proximal thigh, apartial ring or simply a padded bar. A traction device is located on thedistal part of the splint. The traction device can be a commercial ratch-et-type mechanism or a simple windlass and triangular bandage twistedto take up the slack and create distal traction of the femur. The thighand leg are usually supported by several soft and/or elastic supports.
The femur is the largest bone in the body, and fractures can causesignificant blood loss and tissue damage. The blood loss results from thefracture itself and from surrounding tissues damaged by sharp boneends. Losses of up to 2–4 units (1,000–2,000 mL) of blood have beenreported with femoral fractures.
The theory behind the traction splint is that it reduces potentialblood loss by separating and aligning the fracture segments throughtraction. This serves to keep the thigh at its normal length and relative-ly normal circumference—thus decreasing the potential space for bloodloss.1
How often does the traction splint enhance EMScare?In present EMS practice, the traction splint is indicated only for isolat-ed fractures of the femur.5,6 It is contraindicated for:
• Pelvic fractures;• Hip injuries with gross
displacement;• Any significant injury to the knee; and• Avulsion or amputation of the ankle and foot.7
With a single indication and numerous contraindications, how oftenis the traction splint actually used in prehospital care? Researchers stud-ied the incidence of traction splint usage in Evanston, Ill. (population73,200 in 8.5 square miles), for a one-year period in 1999. They re-viewed 4,513 run reports and found 16 patients with mid-thigh trau-ma. Of these 16 patients, 11 had minor trauma and five had clinicalfindings suspicious for femoral shaft fractures.
Of the five patients with findings suspicious for femur fractures, para-medics attempted traction splint application in three. One patient whodid not receive a traction splint had a possible hip injury, a contraindi-cation. The other patient who did not receive the traction splint waspain-free when paramedics arrived and was simply transported in a po-sition of comfort without incident.
Of the three cases in which EMS personnel attempted application ofthe traction splint, only two were successful. The third patient was an82-year-old woman who had mid-thigh trauma due to a fall. When thecrew applied the splint and traction, it resulted in severe pain for the pa-tient, and the splint was subsequently removed. A rigid splint was thenplaced on this patient, and she was transported without incident.
Thus, in this study group, two of 4,513 patients had indications fortraction splint application. Stated another way, only 0.11% of patients(1/11th of one percent) had clinical findings suggestive of a femoralshaft fracture, and only 0.07% met criteria for using the splint. The au-thor of this study concluded, “Traction splints as essential ambulanceequipment may be unnecessary.”8
Are traction splints safe? As a rule, traction splints are safe when used according to the criteriapresented above. However, several recent studies have detailed compli-cations associated with EMS use and misuse of the traction splint.Researchers in Buffalo, N.Y., recently described two patients who de-veloped peroneal nerve palsies following inappropriate application oftraction splints. The Buffalo study demonstrated how traction splintscan aggravate certain soft tissue lower extremity injuries.9
The peroneal nerve (also called the fibular nerve) crosses over theknee and is vulnerable to injury near the knee. Application of a tractionsplint can cause the head of the fibula to be displaced laterally, stretch-ing or tearing this nerve.
This problem is made worse when an injury affects the integrity ofthe knee. One of the patients in the Buffalo study had a (Thomas) trac-tion splint applied because of lower thigh pain and swelling. By the timethe patient arrived in the radiology department, he could not move hisfoot or great toe and had numbness on the bottom of his foot. X-rayswere negative, and orthopedic consultation revealed a severe kneesprain. The splint was removed, and his peroneal nerve palsy eventuallycleared.
The second patient also received a traction splint after EMTs sus-pected a distal femur frac-ture due to a fall. At theED, the patient also ex-hibited peroneal nervepalsy. X-rays of the affect-ed leg were negative, andthe patient’s nerve palsyslowly cleared after re-moval of the splint.
A Pennsylvania study
66 JEMS | AUGUST 2004
TRACTION SPLINT
Traction is applied and Velcro™
straps are secured.Traction is maintained as the splint is placed under the patient.
PHO
TOS
JOE
HEI
GH
TMA
N

WWW.JEMS.COM | AUGUST 2004 | JEMS 67
detailed the case of a 22-year-old man who fell 40 feet from a rooftopparty and briefly lost consciousness. EMS was called and found the manhemodynamically unstable, but without any neurological or vasculardeficits. IV therapy was initiated, and a traction splint was applied for anobvious thigh deformity. The patient was transported to a trauma cen-ter, where he was found to have multiple injuries (left pneumothorax,liver hematoma and multiple fractures). X-rays revealed a comminutedleft mid-shaft femur fracture and a comminuted left calcaneus fracture.
The patient remained in the traction splint for six hours, at whichtime he was found to have numbness and coldness of his left foot. Theleft foot was severely swollen, and the pulses in the foot were absent, in-dicating a compartment syndrome. The traction splint was removed,and the patient was taken to the operating room where the compart-ment syndrome was surgically decompressed. Vascular surgeons re-moved clots from the posterior tibial artery and dorsalis pedis artery torestore blood supply to the foot. The patient later required skin graftsto cover the wounds from surgical decompression of the foot.10
A recent prospective study of 40 patients with multi-system traumawho had a traction splint applied found that 38% of patients had thetraction splint applied despite the fact that its usage was contraindicatedby other injuries.11
These studies clearly illustrate that inappropriate use of a tractionsplint can cause injury or aggravate existing injury and, in the overallscheme of things, the indications for using a traction splint in the pre-hospital setting are limited. Therefore, it’s appropriate to ask, is it pru-dent to stock the traction splint on ambulances and rescue vehicleswhen it is so infrequently used?
Most femoral fractures are accompanied by other injuries that maycontraindicate use of the traction splint. Of the remaining isolatedfemoral fractures, most can be adequately treated through immobiliza-tion with a rigid or adjustable splint or on a long spine board or a vac-uum splint/mattress. For systems that still carry medical anti-shocktrousers (MAST), isolated femoral fractures are one of those few re-maining indications in which the MAST may be indicated.
SummaryTraction splints have been used in EMS for more than 40 years.However, they were originally designed for the treatment of femoralfractures—not temporary stabilization. Multi-system trauma and otherinjuries contraindicate traction splint usage for many femoral fractures.Thus, with the relatively low usage of the traction splint, it may be timeto revisit guidelines that require traction splints on every ambulance andrescue vehicle. They may be, in essence, an EMS relic we may want topart with.
Bryan Bledsoe, DO, FACEP, EMT-P, is an emergency physician in Texas. Hecan be contacted at [email protected].
Donn Barnes, LP, works off the Ivory Coast as a paramedic in the petrole-um industry. He can be contacted at [email protected].
References1. Henry BJ, Vrahas MS: “The Thomas splint: Questionable boast of an
indispensable tool.” American Journal of Orthopedics. 25(9):602–604,1996.
2. Jones R: “Treatment of acute fractures of the thigh.” British MedicalJournal. 11:1086–1087, 1914.
3. Gray HMW: The Early Treatment of War Wounds. H Frowde, Hodderand Stoughton: London, 1919.
4. American College of Surgeons, American College of EmergencyPhysicians: Equipment for Ambulances. 2000.www.facs.org/trauma/publications/ambulance.pdf
5. Campbell JE: Basic Trauma Life Support, 4th ed. BradyPublishing/Pearson Education: Upper Saddle River, N.J., pp. 193–195,2000.
6. Clark JD: “Femur fractures: complications and treatments of traumaticfemoral shaft fractures.” JEMS. 28(4):82–83, 2003.
7. McSwain, et al: Basic and Advanced Prehospital Trauma Life Support,revised reprint 5th ed. Mosby: St. Louis, p. 285, 2003.
8. Abarbanell NR: “Prehospital midthigh trauma and traction splint use:Recommendations for treatment protocols.” American Journal ofEmergency Medicine. 19:137–140, 2001.
9. Mihalko WM, Rohrbacher B, McGrath B: “Transient peroneal nervepalsies from injuries placed in traction splints.” American Journal ofEmergency Medicine. 17:160–162, 1999.
10. Watson AD, Kelikan AS: “Thomas splint, calcaneus fracture, and com-partment syndrome of the foot: A case report.” Journal of Trauma.44:205–208, 1998.
11. Wood SP, Vrahas M, Wedel SK: “Femur fracture immobilization withtraction splints in multisystem trauma patients.” Prehospital EmergencyCare. 7:241–243, 2003.
TRACTION SPLINT IN EMS:FUNDAMENTAL CARE
Don’t Jump the GunBy Lawrence H. Brown & Elizabeth A. Criss
he article by Bledsoe and Barnes is sure to raise a few eyebrowsamong EMS professionals throughout the world—and well it
should. As the authors point out, traction splinting has been a funda-mental component of EMS care since the very beginning of the disci-pline. It is important, though, to read the article carefully and to payclose attention to what the authors are saying. Bledsoe and Barnes arenot advocating the abandonment of traction splints; they’re question-ing whether traction splinting is a necessary EMS intervention. Thereis a difference.
Bledsoe and Barnes are absolutely correct: Very little science wentinto the original decision to include traction splinting in the EMSscope of practice. Anecdotal case reports and descriptive case series cannever carry the same weight as well-designed, prospective, comparativestudies.
In the early days of EMS, however, there was no good science uponwhich to base decisions about what skills to include and exclude fromthe standard of care. Physicians and other leaders had to make the bestdecisions they could on the basis of the information available at thetime.
The fact that early decisions had to be made in the absence of goodscience should not be upsetting; what should be upsetting is that morethan 30 years later we still haven’t conducted scientifically sound re-search on most of the EMS scope of practice.
At the same time, the absence of strong studies proving the effec-tiveness of any given intervention does not necessarily mean that inter-vention is not important. Traction splinting is only one of dozens, ifnot hundreds, of EMS interventions that have never been subjected torigorous evaluation. Indeed, if we removed every EMS device and sus-pended every EMS intervention that has yet to be scientifically proventhere would be very little left for EMS to do.
The papers that Bledsoe and Barnes cite describing adverse effects
T

68 JEMS | AUGUST 2004
TRACTION SPLINT
associated with traction splinting are worrisome. The science behindthese anecdotal case reports and descriptive case series, however, is nomore sound than the science that got traction splints placed on EMSvehicles in the first place. These reports raise questions; they do notgive answers.
It is perfectly appropriate to raise questions. Bledsoe and Barnesshould be applauded for pointing out the lack of science supporting,and the anecdotal evidence questioning, traction splints. We shouldnot, however, change our current practices simply because someonehas raised a question about them. We should answer the question. Wemust do the research—well-designed, prospective, comparative re-search—to evaluate the efficacy of prehospital traction splinting.
And then we must do the research to address whatever questionsBledsoe, Barnes and anyone else raises next.
Lawrence Brown and Liz Criss are regular contributors to the JEMS ResearchReview column, and both serve on the board of advisors for the Prehospital CareResearch Forum.
Proper Splint Design & Application Are the KeysBy Anthony G. Borschneck, MD, co-creator of the Sager Emergency Traction Splint
r. Bryan Bledsoe’s and Donn Barnes’ thought-provoking articlequestions the value and efficacy of traction splinting of fractured
femurs in today’s prehospital setting. However, before we rush tocondemn traction splints as an EMS relic we must first evaluate threekey issues: 1) the leading cause of complications using today’s tractionsplints; 2) the incidence of femoral fractures within the United States,as well as the value of having equipment on board to treat them; and 3)the necessary control of blood loss and pain management. I will elabo-rate:
1) The leading cause of complications using today’s tractionsplints: The contraindications of traction splinting noted by Bledsoeand Barnes are: pelvic fractures, hip injuries with gross displacement,knee injuries, and avulsion and amputation of the foot. Fractures/dis-locations of the hip are also included. I would suggest that proximalthird fracture of the femur with gross displacement is not a con-traindication and requires some qualification.1
Not all traction splints are the same. Almost all traction splints—with the exception of the Sager splint—apply counter-traction to theischial tuberosity from below the shaft of the femur (see p. 64). Theoriginal Thomas full-ring and half-ring splints applied counter-trac-tion on the ischial tuberosity medial to the shaft of the femur.2 Thebottom of the ring was well below the femoral shaft and did not im-pinge on it (see top of p. 65).
People should not assume that today’s modified half-ring (ischialbar/pad type) splints have the exact design specifications and func-tionality of the original Thomas half-ring splint. They don’t.
In thin, young, small patients and some adults, the proximalpad/bar of many of today’s half-ring splints may push up against theshaft of the femur in order to apply a non-slip perch against the ischialtuberosity. Tightening of the thigh strap to prevent slippage off the is-chial tuberosity may enhance distortion at the fracture site.
If you look at a lateral projection of a supine human pelvis andfemur, you’ll note that the ischial tuberosity and the shaft of the femurare on the same plane. The ischial tuberosity projects no more thanone-half to one inch (1 or 2 cm) below the level of the femur.3
In proximal third fractures, these splints may cause injury to the sci-atic nerve and its branches, popliteal and peroneal, as well as bloodvessels and tissue.
A review of the various models of ischial pad splints still in use todayshow pad elevations of 1.75 inches, 2.5 inches and 3.5 inches. Thesame elevations exist in pediatric models. These elevation ranges areinconsistent with the pediatric anatomy of most toddlers, pre-school-ers and other young school-age children of small stature.
Counter-traction groin straps on some models pull laterally andmay constrict blood flow to the femoral artery and vein in the proxi-mal anterior thigh if excessive traction force is applied. Similar actionof the strap below the thigh may cause injury to the sciatic nerve andits branches as well.
Sager Emergency Traction Splints were designed to apply counter-traction against the ischial tuberosity medial to the shaft of the femurin a manner consistent with the original Thomas full and half-ringsplints. Simon and Koenigsknecht note in Emergency Orthopedics: TheExtremities, “the [Sager] splint does not have a half-ring posteriorly,which eliminates any pressure on the sciatic nerve and most impor-tantly eliminates the angulation of the fracture site, which occurs withhalf-ring splints.”4
By design, Sager splints provide anatomically correct, straight in-line traction and immobilization. There is minimum movement of theinjured limb during application, and the Sager figure “8” strap re-stricts distal rotation.
The Sager Model S304 (Sager Form III Bilateral) features “con-tainment within the body silhouette”; it does not extend beyond thepatient’s heels and thus eliminates transport complications in helicop-ters, fixed-wing aircraft and van-type ambulances.
Sager splints provide “gentle,” quantifiable traction that is dynam-ic in nature. As such, Sager splints were designed to permit graded re-duction of the traction force as the muscle spasm decreases and theleg length increases.5 The Sager traction handle/scale enables first re-sponders to set and document the traction force applied. Minto rec-ommends a traction force of an estimated 10% of the patient’s bodyweight with a maximum of 15 lbs. of traction force (for single frac-tures). Only rarely will more traction be required.6
An unpublished retrospective study of 53 patients with lowerlimb fractures recorded at one hospital during a five-year period in-dicated a single case of “cool foot” below the ankle harness.However, the physician reported normal dorsalis pedis and poste-rior tibial pulses.
Two cases of unrelieved pain were also recorded. The average timein traction for all patients was 2.56 hours. No other splint complica-tions were reported. Because the bulk of these injuries occurred inrural areas, transportation times were long.7
Another study, conducted in 2002 and involving 183 volunteerEMTs, paramedics and instructors, demonstrated that an attempt tomanually pull 15 lbs. of traction resulted in a wide range of tractionforce, from 3.5 lbs. to 111 lbs. The group average was two and one-half times the recommended amount—at a force of 37.99 lbs.8
Misuse of traction splints is suggestive of educational deficits; much
D

WWW.JEMS.COM | AUGUST 2004 | JEMS 69
more emphasis should be placed on trac-tion splint design as well the indicationsand contraindications regarding the useof traction splints.
2) The incidence of femoral frac-tures in the United States: Bledsoe’sand Barnes’s questioning of the necessityor limited use of traction splints is basedprimarily on three studies. TheAbarbanell (Evanston) study was limitedto a single-year evaluation of femoralfractures treated with Hare and FernoTrac splints.1,9 Both of these splints areindicated only for use in mid-shaftfemoral fractures.1,10 The two otherstudies referenced do not specify whichtraction splints were used (the Watsonand Kelikian study identifies the splintonly as a Thomas splint).1,10,11 Sagersplints are indicated for treatment inproximal third and mid-shaft femoralfractures and as such, have a much widerrange of application and use. Therefore,much broader, long-term and more inclu-sive studies are needed before an accurateevaluation of the usage of traction splints can be made.
With respect to the incidence of femoral fractures within theUnited States, it should be noted that a 1997 estimate of the totalnumber of femoral fractures was 474,551 patients. Of these, only 9%(41,012) were mid-shaft fractures, and 84% (399,484) were proximalthird fractures.12
The actual reportage of incidences involving femoral fractures forthe year 2002 was 438,496. Given these figures, the value of havinga traction splint onboard to treat femoral fractures should not be soeasily discounted nor underestimated.13
3) Control of blood loss & pain management: It’s importantfor prehospital personnel to recognize that the main functions andobjectives of traction splinting are to: 1) align the fractures, 2) providesecure immobilization, 3) control spasm, 4) control and reduce bloodloss, 5) provide pain relief, 6) prevent further injury to blood vessels,nerves and tissue, and 7) lower the incidence of clinical fat embolism.
In femoral fractures, especially if the fracture is in the proximal end,traction splinting is the best-known prehospital treatment for immo-bilization of the joints above and below the fracture site.
When a patient suffers a fractured femur, the amount of pain felt bythe patient is in part related to the amount of muscle in spasm, as wellas the degree of spasm. This is why a fractured femur typically resultsin much more pain than a fractured humerus.
The application of traction on the muscle tires and pulls it out ofspasm, consequently relieving much of the patient’s pain. It also re-stores the cylindrical shape of the leg and, in the process, increases tis-sue pressure within the thigh, which inhibits further blood loss.Traction splinting also aides in shock prevention, and, therefore, itsuse as a treatment option should not be denied to patients.
In “The Thomas splint: Questionable boast of an indispensabletool,” Henry and Vrahas note, “Although the Thomas splint’s life-
saving abilities may not be as dramatic as many authors have sug-gested, it still has a place in the acute setting of femoral fractures,when applied appropriately and continued until definitive treatmentcan be attained … Thus continued use of traction splints in acutemanagement of femoral shaft fractures seems appropriate.”18
Recognizing the potential for hypovolemic shock to accompany afemoral fracture, minimizing blood loss with prompt traction and im-mobilization, and providing effective pain management and reliefshould continue to be the standard of care.
If prehospital personnel have a greater understanding of anatomyand select appropriate equipment, the incidence of treatment compli-cations with traction splints would be greatly reduced. In an effort toensure safe, complication-free treatment of patients with fractured fe-murs, Minto Research & Development Inc. provides training videos,application posters, user handbooks and instructor’s manuals withexams.19
Anthony Borschneck, MD, is vice president of Medical Research for MintoResearch & Development Inc. (Redding, Calif.). He is an emergency physi-cian (ret.) with more than 35 years’ experience treating femoral fractures.Dr. Borschneck co-developed the Sager Emergency Traction Splint. For moreinformation on Sager Emergency Traction Splints, contact Minto Research& Development Inc. at 800/642-6468, via e-mail at [email protected] online at www.sagersplints.com. Sager is a registered trademark of MintoResearch & Development Inc.
References1. Bledsoe B, Barnes D: “The traction splint: An EMS relic?” JEMS.
29(8):64–69, 2004.2. Borschneck AG, Wayne M: “Sager Emergency Traction Splint: A new
splinting device for lower limb fractures.” The EMT Journal. 4(1):42–47,1980.
1957 ARC First Aid book instructions for use of cravats with the Thomas half-ring splint.

3. Merrill V: Atlas of Roentgenographic Position and StandardRadiologic Procedures, 3rd ed., Mosby, p. 189.
4. Simon RR, Koenigsknecht SJ: Emergency Orthopedics: The Extremities,3rd ed. Appleton & Lange: Norfolk, Conn., p. 8, 1995.
5. Borschneck AG: “Why Traction?” JEMS. 10(7):45, 1985.6. AAOS: Emergency Care and Transportation of the Sick and
Injured,8th ed. Jones & Bartlett Publishers: Sudbury, Mass., p. 653, 2002.
7. Retrospective study of 53 cases of fractures of the long bones of thelower limb treated with Sager Emergency Traction Splints, January1973 to June 1978, Chilliwack General Hospital, Chilliwack, B.C.,Canada.
8. Borschneck AG, Spotts C: “Traction force challenge.” EmergencyMedical Services Magazine. 31(5):72–74, 2002.
9. Abarbanell NR: “Prehospital midthigh trauma and traction splint use:Recommendations for treatment protocols.” American Journal ofEmergency Medicine. 19:137–140, 2001.
10. Wood SP, Virahas M, Wedel SK: “Femur fracture immobilization withtraction splints in multi-system patients.” Prehospital Emergency Care.7(2):241–243, 2003.
11. Watson AD, Kelikian AS: “Thomas splint, calcaneus fracture, and com-partment syndrome of the foot: A case report.” The Journal ofTrauma: Injury, Infection, and Critical Care. 44(1):205–208, 1998.
12. Confidential QMPDC Work Project: Projected Potential US FemurFracture Hospital Admission, ICD9 Data Files.
13. Knowledge Enterprise Inc., No. 1510, p. 2, Inpatient fractures 1999-2002, ICD9 codes 820.00-820.09, 821.00-821.39.
14. Jones R: “Treatment of acute fractures of the thigh.” British MedicalJournal. 11:1086–1087, 1914.
15. Sinclair M: The Thomas Splint and Its Modifications in the Treatmentof Fractures. Oxford University Press, p. 152, 1927.
16. Jones RS: Notes on Military Orthopedics. Cassell & Company Ltd., pp.112–121, 1917.
17. Kendrick DB: “Blood program in World War II (Supplemented byExperiences in the Korean War),” In Historical Note Blood Transfusionsin World War One. Office of the Surgeon General, Department of theArmy: Washington D.C., pp. 5–9, 11–12, 1989.
18. Henry BJ, Vrahas MS: “The Thomas splint: Questionable boast of anindispensable tool.” American Journal of Orthopedics. 25(9):604, 1996.
19. Instructor Manual & Portfolio. Minto Research & Development Inc.:Redding, Calif.
Military Use: SOPBy Richard S. Wiegert, SFC, NREMT-P, Advanced Training Branch(BNCOC); Joaquin R. Soliza, SFC, NREMT-I, Dept. of CombatMedic Training; Juan M. Almonte, SSG, NREMT; Ernest J. Barner,SSG, NREMT; Nathan M. Chipman, SSG, NREMT, 82d AirborneDivision*; Renan Cortez, SGT, NREMT, 1st Infantry Division;Jacques C. Hope, SGT, NREMT, 3rd Infantry Division*
raction splints remain a universal part of medical equipment sets(MES) in most U.S. Army evacuation vehicles, from ground am-
bulances (both wheeled and tracked) to aircraft. Traction splints, likeany durables in the MES (KED, litters, straps, spine boards, etc.) areusually exchanged at an ambulance exchange point (AXP) or landingzone (LZ) when an aircraft picks up the patient.
TrainingBattlefield care operates under the tenets of Tactical Combat CasualtyCare (TCCC), emphasizing the total continuum of care in an opera-tional environment. TCCC is broken down into three phases of care:
1) Care under fire—Care rendered by the medic at the scene of in-jury while under direct, effective hostile fire. Things to consider: First, themedic is limited to what they carry in a leg pack and aid bag on theirback. Second, hemorrhage control and getting the patient under coverare the key objectives at this phase of care.
72 JEMS | AUGUST 2004
TRACTION SPLINT
T The U.S. military utilizes theREEL Splint System for trac-tion splinting and immobiliz-ing angulated knee injuries. The process:1) traction applied; 2) ischial strap padded and
secured; 3) straps secured; and 4) patient logrolled onto
backboard.
1
2
3
4
PHO
TOS
CO
URT
ESY
REE
L RES
EARC
H &
DEV
ELO
PMEN
T

WWW.JEMS.COM | AUGUST 2004 | JEMS 73
2) Tactical field care—The care rendered by the medic once they areno longer under direct, effective hostile fire or when an injury occursbut there is no hostile fire.
3) Casualty evacuation care (CASEVAC)—The care rendered oncethe casualty has been picked up by vehicle, aircraft or boat.
Combat medics are taught traction splinting in the EMT portion oftheir entry-level medic training (91W). Traction splinting is trained andtested to NREMT and DOT standards. It is also part of sustainmenttraining in most Army medical units’ training plans.
OperationalBecause the traction splint is part of the MES in most evacuation plat-forms, it is usually applied at the AXP during patient exchange. Patientswith indications for traction may arrive at the AXP with the extremityimmobilized, often in field-expedient fashion (e.g., anatomical splint-ing, cravats/wraps). If time and situation allow traction splinting at theAXP, it is often done (when indicated) at this level of care.
The Bledsoe article mentions patients who have developed palsiesfrom compression, or in the case of the patient left in the splint for sixhours, a cold, vascular-compromised extremity. A few perspectives fromthe military address these complications:
In operational environments, evacuation times and methods (e.g.,ground vs. air) are often governed by the current mission situation.Patients can be in the “evacuation chain” from minutes to (potentially)several hours. Given this, we assert and stress the importance of the on-going exam. Medics are drilled in “checking distal PMS” before andafter splinting, and during evacuation to avoid complications.
Army ground evacuation vehicles are designed to negotiate nearlyany terrain and a patient in traction and on a spine board may poten-tially have an uncomfortable, rough ride. Civilian EMS courses andNREMT testing emphasize “securing splint to spine board.” However,this is difficult at times in the field. Therefore, in the military, the splint-ed leg is often supported or suspended separate from the backboard toprevent injury aggravation.
Traction splinting is a tool used by Army medical personnel as a wayto stabilize obvious femur fractures in an operational environment.Although isolated femur fractures are rare, traction splints are still car-ried in most Army evacuation vehicles. Army medics continue to betrained in traction splinting, with emphasis on the CASEVAC phase ofTactical Combat Casualty Care. Ultimately, the unit medical officer(MD/DO/PA) will guide protocol on application and/or removal ofexisting splints for traction application.
*Units served with during Operation Enduring Freedom/IraqiFreedom.
Note: The Chief, Academic Division, Department of Combat MedicTraining, authorized the operational feedback provided. It does notrepresent the position of the Department of Combat Medic Training,AMEDD Center & School or the U.S. Army.
Sins of Commission vs. Sins of OmissionBy Sam Slishman, MD, ED physician & traction splint developer
’m an emergency physician at the University of New Mexico. Sixyears ago I developed a lightweight, easy-to-apply, multi-use trac-
tion splint. It is now manufactured in Italy by Gipron and distributed
by Galls in England. It’s called the Slishman splint. Because of this his-tory, my perspective on Dr. Bledsoe’s article is certain to be very biased.This is unavoidable.
Patients who suffer this injury are typically miserable. Some presentunconscious due to multitrauma. But the large majority that I’ve seenare wide awake and in agony. Pain causes the large quadriceps to con-tract, forcing sharp femur fragments into surrounding tissue, causingfurther discomfort. This feedback loop results in excruciating pain. Byproviding traction to the spastic quad, this painful experience can be sig-nificantly alleviated. An additional reason to apply traction is to limitbleeding within the thigh.
For me, the question is not whether traction limits pain and helps pa-tients, but how to best apply traction. A perfect traction splint is onethat can be applied quickly with minimal training, requires minimal ma-nipulation of the injured limb during application, permits modificationof traction for patients awake and capable and causes few complications,such as peroneal nerve or vascular injury.
I’ll conclude with the topic of complications. It boils down to ourcomfort with sins of commission vs. those of omission. Should we notapply splints to every femoral fracture for fear that someone may suffera peroneal nerve palsy, venous thrombus, pressure sore or other prob-lem due to splint application? Such complications as pain, further tissuetrauma from fracture fragments, conversion of fractures from closed toopen and, perhaps, exsanguination may also result from not applyingtraction splints. But it is more difficult to lay blame for not taking anyaction. If it is my leg, I want a traction splint.
Questioning CommendedBy Sam Scheinberg, MD, The Seaburg Co. Inc.
ur company does not manufacture, sell or have any financial rela-tionship with any femoral traction splints. I would like to com-
mend Bledsoe and Barnes on their willingness to question establishedbenefits. It’s exactly that kind of thinking and courage that has pro-duced many of the major advances in the health-care field.
The fact that one community experienced a low incidence of femoralfractures has little meaning. I practiced orthopedics in an equally smallcommunity and at one point treated eight femoral shaft fractures inthree separate hospitals. Is this normal? Of course not, but it does illus-trate that types of trauma can vary according to many factors, includingspeed limits and road conditions.
Bledsoe and Barnes cite complications regarding the improper use offemoral traction splints and make specific reference to a lengthy use ofsix hours. I can state only that the improper use of any device (e.g., dry-ing your hair in a microwave oven) could lead to serious complications.
Recognizing that blood loss, vascular and neurological complicationsand morbidity can vary according to fracture type, transport time,provider skills, immobilization techniques, age, pre-injury health statusand associated injuries, I believe the overriding reason for prehospitalfemoral traction (excluding the wilderness setting) is for pain relief.During my 30 years as an orthopedic surgeon, I have witnessed the dra-matic pain relief provided by femoral traction splints and significant in-crease in pain when these devices were removed. Therefore, I can onlyhope such a device is applied to me or my family members if we are everso unfortunate to suffer such a terrible injury. JEMS
I
O