Tissue Nematodes Pharmacy
-
Upload
microscopegeek -
Category
Documents
-
view
219 -
download
0
Transcript of Tissue Nematodes Pharmacy
-
8/6/2019 Tissue Nematodes Pharmacy
1/54
REVISION
Types of Life Cycle in Trematoda
and Cestoda
-
8/6/2019 Tissue Nematodes Pharmacy
2/54
Life cycle in human trematodes
-
8/6/2019 Tissue Nematodes Pharmacy
3/54
Life cycles in human intestinal cestodes
-
8/6/2019 Tissue Nematodes Pharmacy
4/54
Life cycles in human larval cestodiases
-
8/6/2019 Tissue Nematodes Pharmacy
5/54
NEMATOD
A
1. Intestinal nematodes
2.
Tissue nematodes
-
8/6/2019 Tissue Nematodes Pharmacy
6/54
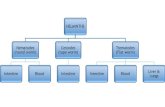
Classification of nematodes by habitat and
development.
Adult intestinal nematodes with pre adult larval lungmigratory phase:
Ascaris, Hookworms, strongyloides.
Adult Intestinal nematodes without larval migratory phase:
Enterobius, Trichostrongylus, Capillaria and Trichuris.
Intestinal nematodes with post-adult larval tissue invasion:
Trichinella.
Larval tissue nematodes with developmental arrest:
visceral and cutaneous larva migrans.
Adult tissue nematodes:
Dracunculus and filariae.
-
8/6/2019 Tissue Nematodes Pharmacy
7/54
Nematodes according to mode of infection
1. Ingestion of eggs:
Ascaris, Enterobius, Trichuris.
2. Ingestion of larva:
Trichostrongylus (on vegetable), Trichinella (in pork),Dracunculus (in cyclops), Capillaria (in fish).
3. Active penetration of skin by larva:
Ancylostoma, Necator, Strongyloides.
4. Entrance of skin by larva transmitted by insect:
Filarial worms : Wucheraria, Onchocerca, Loa,Acanthocheilonema, Mansonella.
-
8/6/2019 Tissue Nematodes Pharmacy
8/54
Nematode infection by ingestion
-
8/6/2019 Tissue Nematodes Pharmacy
9/54
Nematode infection via skin
By larvae
-
8/6/2019 Tissue Nematodes Pharmacy
10/54
Tissue Nematodes
1. Adult tissue nematodes:
Adult tissue nematodiases: filarial wormsand Medina worm
2. Intestinal nematodes with post-adult larvaltissue invasion:
Trichinella. See intestinal nematodes.
3. Larval tissue nematodiases withdevelopmental arrest:
visceral and cutaneous larva migrans.
10
-
8/6/2019 Tissue Nematodes Pharmacy
11/54
Adult Tissue Nematodiases:
Filarial worms
Dr Mohieddin M
Abdul-Fattah
11
-
8/6/2019 Tissue Nematodes Pharmacy
12/54
1. Wucheraria bancrofti and brugia malayi.
A. Biology:
Final host: - Man only in W. bancrofti, - Man, cats andmonkey in B. malayi
Habitat: afferent Lymph vessels and nodes in the lower
half of the body. Exit stage: microfilaria from peripheral blood through
mosquito bite.
Morphology: long and slender worms; (4 cm) & (10 cm) with 100m wide. Brugia is half as long.
12
-
8/6/2019 Tissue Nematodes Pharmacy
13/54
8. L3 migrates to
mosquito proboscis
1. Mosquito takes blood meal
and L3 enters through bit wound
2. Adults in lymphatics
3.Produce sheathed
microfilaria (MF) in
blood & lymph4. Mosquito
takes blood
meal &
ingests MF
5. microfilaria
penetrate the
midgut &
migrate to
thoracic
muscles
6. L1
Wucheraria & Brugia LC
-
8/6/2019 Tissue Nematodes Pharmacy
14/54
Wucheraria and Brugia
B. Epidemiology:
1. Distribution: In tropics and subtropics. In Egypt they are present in
Sharqiya, Dakahliya and others.
2. Transmission:
Intermediate host:
Mosquitoes as Culex, Aedes and Anopheles.
Reservoir host:
No. Reser
voir hosts in W.
bancrofti.
Cats and monkeys in B. malayi.
Infective stage: 3rd stage filariform larva.
Mode of infection: Infective larvae enter skin through
the bite wound of the mosquito..14
-
8/6/2019 Tissue Nematodes Pharmacy
15/54
Wucheria and Brugia
C.Host parasite relationship:
1. Asymptomatic amicrofilaraemic: Immune persons in endemics , they show specific
antibody seropositivity and antigen negativity).
2. Symptomatic amicrofilaraemic with filarial
antigenemia:
Tropical pulmonary eosinophilia:
hypereosinophilia, cough, wheeze, lung fibrosis, Itresponds to antifilarial therapy.
3. Asymptomatic microfilaraemic:
These are tolerant persons in endemic areas.
15
-
8/6/2019 Tissue Nematodes Pharmacy
16/54
Host-Parasite relationship; continued
C. Host parasite relationship:
4. Early disease: incubation period ~ 1 year followed by
episodes of fever with lymphangitis and epidydmo-orchitis
for years.
5. Late disease:D
amage of lymphvessels due to 2ry
bactaerial infection (the symbionts; Wolbachia)
Obustructive manifestations;
hydrocele, and elephantiasis in the leg, scrotum and breast
(in Wucheraria).
Elehpantiasis is limited below the elbow and knees in
brugian type.
16
-
8/6/2019 Tissue Nematodes Pharmacy
17/54
Acute (early) and chronic (Late)
17
Lymphangitis
DermatitisHydrocele Elephantiasis
-
8/6/2019 Tissue Nematodes Pharmacy
18/54
Wucheraria and Brugia
D. Lab diagnosis:1. Detect eosinophilia, and sheathed microfilaria in 10
p.m.2 a.m. concentrated blood samples or
2. Detect filarial antigens by immuno-chromatographictest (ICT) or
3. Detect antifilaria antibodies by Elisa.
Characteristics of microfilaria tails
Wucheraria: tapered anucleate tail.
Brugia: with 2 discrete nuclei reaching tip of the tail.
18
-
8/6/2019 Tissue Nematodes Pharmacy
19/54
Wucheraria and Brugia
E. Treatment:
Ivermectin one dose 20g/kg can be repeated every year..
Diethycabamazine (DEC); 2mg/kg tds for 12 days.
For lymphedema Benzopyrone (coumarin) 400 mg/day PO
or using compression garments (hard to use).F. Control:
Mass treatment by:
annual single dose of albendazole (400mg) plus ivermectin
(100-400g) or DEC to stop transmission, and vector
control.
19
-
8/6/2019 Tissue Nematodes Pharmacy
20/54
Loa loa
A. Biology: Final host: - Man only
Habitat: subcutaneous tissue and sub-conjunctival.
Exit stage: 250m tightly sheathed microfilaria from
peripheral blood through mosquito bite.
Morphology: long and slender transparent worms;
(3cm) & (7 cm) with 100m wide.
20
-
8/6/2019 Tissue Nematodes Pharmacy
21/54
Adults in S.C. tissues
3. They produce
sheathed microfilaria
in blood, urine, CSF
and sputum
4. Fly takes blood
meal & ingest
microfilaria (MF)
5. MF
penetrate
midgut to
thoracic
muscles
8. L3 migrateto the fly
mouth parts
1. Fly takes
blood meal &
L3 enter the
bite wound
Human stagesChrysops stages
Loa loa LC
Loa loa LC
-
8/6/2019 Tissue Nematodes Pharmacy
22/54
Loa loa
B. Epidemiology:
1. Distribution: Forests of central and West Africa.
2. Transmission:
Intermediate host: Tabanid flies (chrysops).
Reservoir host: No.
Infective stage: 3rd stage filariform larva.
Mode of infection:
I
nfective lar
vae enter the skinthrough the bite of Chrysops
22
-
8/6/2019 Tissue Nematodes Pharmacy
23/54
Loa loaC. Host parasite relationship:
i. Calabar swelling:
non-pitting transient subcutaneous swelling
due to hypersensitivity to worm metabolites.
i. Transient conjunctivitis due to sub-conjunctival
adult migration.
ii. Meningoencephalitis, glomeruolnephritis,and endomyocardial fibrosis in heavy
infections treated by DEC.
23
-
8/6/2019 Tissue Nematodes Pharmacy
24/54
Loa loa
D. Lab diagnosis: detect eosinophilia, tightly sheathed microfilaria in
conc. blood samples,
or Loa antibodies by Elisa.
E. Treatment:
Diethylcarbamazine,
albendazole
F. Control:
clear forest, screen houses
and vector control24
-
8/6/2019 Tissue Nematodes Pharmacy
25/54
Onchocerca volvulusA.Biology:
Final host: - Man only
Habitat: subcutaneous tissue,found coiled in nodules.
Exit stage:300-m microfilaria inskin by bite of the black fly(Simulium)
Morphology : long and slenderworms; (3cm) & (50 cm) with100m wide.
25
-
8/6/2019 Tissue Nematodes Pharmacy
26/54
9. L3 moves
to black fly
mouth parts
6. MF migrate
to thoracic
muscles
1. Fly takes blood and L3
enter through bite wound
2. Subcutaneous
tissues (SC)
3. Adults in
SC
4. Adults
shed MF in
skin
Onchocerca Life cycle
Human stagesSimulium
stages
5. Fly takes
microfilaria (MF) in
blood meal
-
8/6/2019 Tissue Nematodes Pharmacy
27/54
OnchocercaB. Epidemiology:
1. Distribution: Tropical Africa, Yemen, central and south America
among farmers who get contact with these flies that
concentrate around rivers.
2. Transmission: Intermediate host:
Black fly (Simulium). This breeds in rapidly flowing
freshwater and bite nearby.
Reservoir host: No. Infective stage: 3rd stage filariform larva.
Mode of infection:
Infective larvae enter skin through the wound induce by
bite of Simulium.27
-
8/6/2019 Tissue Nematodes Pharmacy
28/54
OnchocercaC. Host parasite relationship:1. Adult enclosed in fibrous tissue over
bony prominences subcutaneous firm
nodules These are seen over the pelvic brim, the
sacrum greater trochanters and head.
2. Immune reactions to dying microfilariain skin and eye lead to:
Dermatitis severe itching thickening, edema, blackening (Sowda),lichenfication, and loss of elastic fibers(hanging groin).
Punctate keratitis and opacities, panus,iritis, and chorioretinitis with opticatrophy.
These lead to blindness called riverblindness.
28
-
8/6/2019 Tissue Nematodes Pharmacy
29/54
Keratitis and liver blindness Chronic microfilaremia in
the eye leads to sclerozingceratitis (a hardeninginflammation of thecornea)
The cornea becomesopaque
Nodules directly on thehead result in more mfburden for the eyes
29
-
8/6/2019 Tissue Nematodes Pharmacy
30/54
D. Lab diagnosis:
Detect unsheathed microfilaria inbloodless skin snips from the vicinity of
nodules or section of adult in excised cutaneous
nodules.
Eosinophilia is moderate.
Detect anti-Filaria IgG4.E. Treatment:
Ivermectin (150g/kg). It should be avoided in patients with
heavy Loa loa infection as this may leadto fatal encephalitis.
F. Control:
Aerial spraying of rivers withinsecticides.30
-
8/6/2019 Tissue Nematodes Pharmacy
31/54
Dracunculus medinensisDracontiasis
y Final host: - Man, cattle, horse and dogs.
y Habitat: subcutaneous tissue.
y Exit stage: Adult female gives birth to
rahbditiform larva through ulcer onto water.
y Morphology and life cycle: long and slender
worms; (3cm x 0.5mm) & (100 cmx1.5mm).
I. BIOLOGY
-
8/6/2019 Tissue Nematodes Pharmacy
32/54
1. Human drinks water
containing Cyclops
infected with L32. L3 penetrate
the intestine,
migrate to bodycavity and
mature to adults
3.-A year later migrate to
skin, induce blister, emerge
and discharge L1 into water
4. Cyclops ingests
L1 in water
5. L1 molttwice to L3
Dracunculus
LC
-
8/6/2019 Tissue Nematodes Pharmacy
33/54
II. Epidemiology
y Distribution: Areas depending on wells waterin Yemen, west and East Africa, India and
Brazil.
y
Transmission:Intermediate host: Cyclops.
Reservoir hosts: cattle, horse and dogs.
Infective stage: Coma shaped larva in theCyclops.
Mode of infection: Drinking water
contaminated by infected Cyclops.
-
8/6/2019 Tissue Nematodes Pharmacy
34/54
III. Host-Parasite Relationship
i. When the worm emerges, it cause burningsensation and forms blister..
ii.After discharging larvae,
the worms die in a process that takes manyweeks leading to ulceration and spread of 2rybacteria infection.
causing fever and disability for months especially
in presence of multiple worms.iii.Migrating worms near joints cause arthritis with
effusion.
-
8/6/2019 Tissue Nematodes Pharmacy
35/54
IV. Diagnosis, treatment, and control
A. Lab diagnosis: white cloud of larvae,extruded by female worms in water, ischaracteristic.
B. Treatment: Metronidazole, albendazole.Safe extraction of the worm by slow windingon a stick.
C.C
ontrol: 1-Provision of safe drinking water.2-Straining water through to filter out
Cyclops.
-
8/6/2019 Tissue Nematodes Pharmacy
36/54
1. Intestinal nematodes with post-
adult larval tissue invasion
Trichinella spiralis
Larval tissue nematodes
-
8/6/2019 Tissue Nematodes Pharmacy
37/54
Trichinella spiralisA. Biology:
Final host: Pigs, wild boars, rats, bears, walruses, and manyother carnivores including man.
Habitat: -
i. Adult in Small intestines while females inhabit rows of
epithelial cells of the mucosa of duodenum and jejunum.
ii. Larvae live in Striated muscle fibers (cells).
Exit stage:
i. Males in the faecal streams.
ii. Larvae have no exit as they encyst in muscle fibers.
Morphology: 2.5 mm long with tapering post. end and 1.2mm long with 2 caudal appendages. puts 5000 larvae each
100m long.
1 M i
-
8/6/2019 Tissue Nematodes Pharmacy
38/54
Circulation
5. Larva encysts instriated muscles
3. enterintestinalmucosa
copulates
4.Larva deposited in the mucosa
1. Man ingestsencysted larvain undercooked
pork
Rodents
Carnivorism
Pigs
Life cycle of Trichinella
1. Encystedlarva from pigs
2. Larvae releasedin intestine,mature to adults
-
8/6/2019 Tissue Nematodes Pharmacy
39/54
B. Epidemiology:
Distribution: Worldwide; prevalent in pork eatingcountries (USA and Europe).
Transmission:
Intermediate host (IH): Pigs.
One host may serve as both final and IH. Humans aredead end IH.
Reservoir host: Pigs, wild boars, rats, bears,
walruses, and many other carnivores. Infective stage: Encysted larvae in muscles.
Mode of infection: Ingestion of pork infected byencysted larvae.
-
8/6/2019 Tissue Nematodes Pharmacy
40/54
C. Host-parasite relationship:
1. Intestinal stage (20-24 hours): eneteritis nausea,vomiting, abdominal pain and diarrhea.
2. Migratory stage:
A. Invading skeletal muscles (1-2 weeks): fever, facialedema, conjunctivitis, pain, swelling and weakness ofthe involved muscles.
B. Invading cardiac muscles and CNS (3rd week):Myocarditis and CNS involvement are the mostfrequent two causes of death in trichinosis.
3. Encapsulation (3w 4 w): symptoms subside or decrease. Myocarditis persists
and may precipitate heart failure.
4. If the infective dose 100 larvae morbidity occurs. If it
is 300,000 death occurs
D Di i
-
8/6/2019 Tissue Nematodes Pharmacy
41/54
D. Diagnosis:
1. Symptoms.
2. detection of free or encapsulated larvae. From the
7th day onwarda) In compressed (trichinoscopy) or
b) Stained biopsy.
c) Or digested samples from deltoid, biceps,
gastrocnemius or Pectoralis muscles.d) Or by xenodiagnosis in rats.
3. Immune-diagnosis by
a. Bachman intra-dermal skin test (IDT).
b. Serology: from 2 weeks in heav
y infection and3
-4w in lighter ones:
BFT (2w), IFAT (2-3w) and Sandwich Elisa.
-
8/6/2019 Tissue Nematodes Pharmacy
42/54
E. Treatment:
Prednisolone 40 mg/day for 5d, with
Mebendazole 50 mg/kg/12h PO for 10 days.
F. Control: Properly cooking pork.
Feeding pigs on cooked garbage.
-
8/6/2019 Tissue Nematodes Pharmacy
43/54
2. Larval tissue nematodes withdevelopmental arrest
Dr Mohieddin M Abdul-Fattah
43
Visceral larva migrans Cutaneous larva migrans
-
8/6/2019 Tissue Nematodes Pharmacy
44/54
Toxocariasis: visceral larva migrans
Final host:1. cats (T.cati, cats Ascaris) and
2. dogs (T. cani; Dogs Ascaris)
Habitat in final host: small intestine.
Man acts only as blind end paratenic IH host
Habitat in man: larvae migrate in visceral tissuewithout further development.
Exit stage from dogs and cats: Ascaris like egg Morphology: beside to 3 characteristic ascarid lips
there are two cervical alae. Length is 4-6 cm in maleand 7-12 cm in females.
44
Aetiology: Toxocara cati and T.cani
5 To circulation
-
8/6/2019 Tissue Nematodes Pharmacy
45/54
1.Adult in dogIntestine passeseggs in feces
3. Dogs < 5 weekingest the egg
4.Larva releasedin the intestine
5. To circulation,lung alveoli,bronchi.
Then through
swallowed sputumto intestines
4.Larvaereleased inthe intestine
5. Larvae migrate
in various organs
Toxocara LC
Visceral larva
migrans
2
3
-
8/6/2019 Tissue Nematodes Pharmacy
46/54
Epidemiology
Distribution: worldwide, young children as they
are likely to ingest soil
Transmission:
1. Intermediate host: man is blind paratenic IH host
2.Reservoir host: old cats, dogs and birds
3. Infective stage: embryonated egg with 2nd stage
larva.
4. Mode of infection: Ingestion of soil, contaminatedwith mature egg.
46
-
8/6/2019 Tissue Nematodes Pharmacy
47/54
Host parasite relationship
Visceral larva migrans (in heavy infection):
due to migration lead to fever pneumonitis,
abdominal pain, myalgia ,.lymphadenopathy,
hepatomegaly and convulsion.
Ocular larva migrans (in lighter infection):
invasion of the eye granuloma in retina and
iridocyclitis with posterior synechiae
diminution ofvision and squint.
47
d l
-
8/6/2019 Tissue Nematodes Pharmacy
48/54
Diagnosis ,treatment and control
Lab diagnosis: Clinical picture and ELISA to
detect antibodies to (E-S) antigens of laboratorymaintained larvae.
Treatment:
Diethylcarbamazine 2-3 mg/kg PO tds for 3weeks.
Thiabendazole 16 mg/kg tds for 7-28 days,
depending upon tolerance. Prednisolone for ocular disease
Control: Personal hygiene and sanitation of
owned cats and dogs.48
Cutaneous Larva Migrans
-
8/6/2019 Tissue Nematodes Pharmacy
49/54
Cutaneous Larva Migrans.
Anckylostoma caninum and A. brasiliense
Final hosts:
1. cats (A. braziliense, cats Ankylostoma) and
2. dogs (A. caninum; Dogs Ankylostoma)
Habitat in final host: small intestine.
1. In man, larvae penetrate the stratum corneum of the
epidermis downwards, only, to the stratum basale.
2. They migrate in the epidermis for weeks or months
and cannot complete its life cycle (i.e. man act as
dead end transport host).
I. Biology
-
8/6/2019 Tissue Nematodes Pharmacy
50/54
I. Biology, continued
Exit stage from FH; dogs and cats: Ankylostoma
like egg. No exit stage from man
Life cycle and Morphology: characteristic ant.b
uccal capsule. Post. End of males hascopulatory bursa.
1 Adults in small
-
8/6/2019 Tissue Nematodes Pharmacy
51/54
1. Adults in smallintestine of dogs
and cats2. OvipositImmature eggsin intestine
3. Eggspassed in
feces
4. Rhabditiformlarvae hatch
5. Filariformlarvae in soil
6. Penetrateskin of dogsor cats
7. By circulationto lung
Larvae Penetrate
skin of man
Migrate inS.C. tissues
Can notcomplete LC
8. Larvae moltin alveoli
9. Enter bronchi,reach trachea
10. Swallowedinto esophagus,to intestine
11. Larvaemature to adults
-
8/6/2019 Tissue Nematodes Pharmacy
52/54
II. Epidemiology
y Distri
bution: worldwide, children andconstruction workers who are exposed to
contaminated soil.
y Transmission:
Intermediate host: man is dead end transport
host. It is not intermediate host.
Reservoir host: birds and other mammals
Infective stage: filariform larvae in soil.
Mode of infection: Larvae in soil penetrate
the skin.
III H i l i hi
-
8/6/2019 Tissue Nematodes Pharmacy
53/54
III. Host Parasite Relationship
Migration of the larvae intradermally causes in
inflammatory response. The lesions (creepingeruption) are extremely pruritic.
Other Causes of creeping eruption:
y Strongyloides stercoralis.
y Cutaneous myiasis (Hypoderma and
Gastrophullus).
-
8/6/2019 Tissue Nematodes Pharmacy
54/54
IV. Diagnosis, treatment, and control
A. Lab diagnosis: clinically and by serology.
B. Treatment:
Thiabendazole, 25mg/kg PObd for 5 days.It can be repeated after rest of 2 days.
C. Control:
Personal hygiene and sanitation of ownedcats and dogs.