Thyroid pathology notes
-
Upload
roger961 -
Category
Health & Medicine
-
view
5.724 -
download
0
Transcript of Thyroid pathology notes

thyroid pathology

Preliminary stuffLecture informationEndocrine PathologyPathology for Dental Students (LaMP 5-100)University of Minnesota School of Dentistry
LecturerKristine Krafts, [email protected] only Elvis CDs in the car.Vidistine nuper imagines moventes bonas?*
Outline Introduction Hyperthyroidism Hypothyroidism Non-neoplastic diseases Neoplastic diseases Review
Further readingRobbins Basic Pathology, 8th edition, pages 758-771
* Seen any good movies lately?
thyroid pathology | 2 of 24

Introduction
Thyroid anatomy and histologyEmbryology The thyroid develops from pharyngeal
epithelium that descends down into the anterior neck.
If this pathway (called the thyroglossal duct) is not fully obliterated, it may give rise to thyroglossal duct cysts (little, fluid-filled cysts in the midline neck, anterior to the trachea), which occasionally get infected.
Gross Normal thyroid weight: about 15 – 20
grams. Situated near the parathyroid glands and
the recurrent laryngeal nerves (important during surgery).
Histology The thyroid has two lobes, which are divided
into lobules, each containing about 20 – 40 follicles.
The follicles are lined by cuboidal to low columnar epithelium, and are filled with colloid (which contains thyroglobulin).
Between the follicles, there are parafollicular cells (or C cells), which secrete very small amounts of calcitonin.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Normal thyroid glandPost-mortem photoTwo lobes
Normal thyroid folliclesHematoxylin and eosin stainLow and high power
thyroid pathology | 3 of 24

Thyroid physiologyWhat does the hypothalamus have to do with it?The hypothalamus secretes TRH (thyrotropin-releasing hormone), which stimulates the anterior pituitary to secrete TSH (thyroid-stimulating hormone, or thyrotropin).
What does the pituitary have to do with it?TSH stimulates growth of the thyroid gland, uptake of iodide, and synthesis and release of thyroid hormones.
Remember how thyroid hormones are made?
Iodide is transported into the thyroid gland, converted to iodine, and attached to tyrosine residues on the big thyroglobulin molecule. These iodinated tyrosine molecules then couple to form the thyroid hormones: T4
(thyroxine) and lesser amounts of T3 (triiodothyronine).
What gets out into the blood?T4 and T3 are cleaved from thyroglobulin and released into the blood. T4 is then deiodinated to form either T3 or reverse T3 (a molecule without any apparent biologic activity).
What's the deal about bound vs. unbound?Most of the thyroid hormones are bound to plasma proteins (mostly TBG, or thyroxine-binding globulin) for transport to tissues. Only a small amount is in the active, free form. This means that the body can keep the level of active (free) thyroid hormone within a narrow range, while maintaining a big, easily-deployed backup reserve of inactive (bound) hormone.
What does thyroid hormone do?Free T3 or T4 enters its target cell and interacts with nuclear receptors to change gene expression, increase carbohydrate and fat breakdown, and stimulate protein synthesis. Result: increased basal metabolic rate.
How does the poor thyroid gland adjust?The thyroid gland is very responsive to stimuli and is in a constant state of adaptation (how exhausting). When the thyroid is more active (puberty, pregnancy, physiologic stress, thyroid-stimulating drugs such as thiourea), the follicular epithelial cells become hyperplastic (get taller, sometimes forming little buds or papillae), more thyroglobulin gets resorbed, and the body’s metabolic rate goes up. When the thyroid is less active (when stimuli abate), the epithelial cells flatten down, the
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
TRH
TSH
T3, T4
thyroid pathology | 4 of 24

amount of colloid increases, and the body’s metabolic rate goes down.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
thyroid pathology | 5 of 24

Clinical pointsThyroid disease is common and easily treated……but the symptoms are variable and often subtle, and the onset is often insidious.Thyroid disease is often overlooked. You have to think of it to diagnose it!
Laboratory testingThe most commonly-used laboratory tests are:
TSH (thyroid stimulating hormone) This test measures the amount of TSH in the
blood. It’s very sensitive, so it can detect very low levels of TSH.
Even a very small fluctuation in T4 will cause a rapid, inverse change in TSH. So the TSH is a good initial test to screen for hyper- or hypothyroidism. If your patient is symptomatic, get a free T4 too (see below). TSH is also a good test to use when following patients on thyroid medication.
Free T4 (thyroxine) This test tells you how much active (unbound,
free) T4 your patient is making. Don’t confuse this with the total T4, which
gives you all the T4 (99% of which is bound and inactive). The total T4 level is more of a reflection of how much binding protein is around.
Use this test to screen for hypo- and hyperthyroidism.
Here’s a simple way to interpret TSH and free T4 levels.
low normal high
lowsecondary
hypothyroidismsecondary
hypothyroidism1primary
hypothyroidism
normal
subclinical hyperthyroidism
euthyroidismsubclinical
hypothyroidism
highprimary
hyperthyroidismsecondary
hyperthyroidism2
secondary or tertiary
hyperthyroidism
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
TSH
T4
Most common thyroid tests:
TSHFree T4
thyroid pathology | 6 of 24

1 You wouldn't think you'd find a normal TSH with a low T4, but it can happen! Sometimes the pituitary makes TSH that's normal in quantity (so the lab test measuring TSH appears normal), but abnormal in quality (it's structurally abnormal, and it doesn't stimulate the thyroid the way it should, so the patient becomes hypothyroid). A patient with this disorder would be said to have secondary hypothyroidism, because the problem is in the pituitary.2 Here's another strange occurrence: a normal TSH with a high T4. Sometimes, TSH-producing pituitary adenomas will show this pattern of laboratory results. The more likely findings in a patient with a TSH-producing pituitary adenoma, though, are a high TSH and a high T4 (and this is what you should try to remember, otherwise you'll get confused).
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
thyroid pathology | 7 of 24

Occasionally-used laboratory tests include:
Free or total serum T3 (triiodothyronine) This test tells you how much free or total T3
your patient is making. Sometimes, hyperthyroid patients have
elevated levels of T3 instead of T4 (called “T3
thyrotoxicosis”). A serum T3 would be very useful in this setting.
T3 uptake and rT3
These tests estimate how much thyroid-binding protein a patient has.
You might see these tests mentioned once in a while, but they really aren’t used much anymore.
Anti-thyroid antibody tests These antibodies come in three flavors: anti-
peroxidase (or anti-microsomal), anti-thyroglobulin, and anti-TSH-receptor. Use these when you suspect autoimmune thyroid disease.
Anti-peroxidase antibodies are pretty sensitive and specific for Hashimoto’s disease, whereas anti-thyroglobulin and anti-TSH-receptor antibodies can be present in either Hashimoto’s or Graves disease.
Radioiodine thyroid scanning The patient is given a little radioactive iodine
(123I), and then the thyroid gland is scanned to see how well it takes up the iodine.
Areas of thyroid that are more active (making a lot of thyroid hormone) take up a lot of 123I and appear “hot.” Areas of thyroid that are less active (not making much hormone) take up little 123I and appear “cold.”
Two uses for this test: (1) Evaluation of thyroid nodules. Hot nodules are virtually always benign; cold nodules are usually, but not always, benign (about 10% turn out to be malignant). (2) Determination of appropriate therapeutic dose of radioactive iodine.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Radioiodine scan showing cold nodule
Hot nodules:almost always benign
Cold nodules:occasionally malignant
thyroid pathology | 8 of 24

introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
thyroid pathology | 9 of 24

HyperthyroidismDefinition: a hypermetabolic state caused by elevated levels of thyroid hormone.
CategoriesPrimary hyperthyroidism: the thyroid is over-functioning because of some intrinsic thyroid gland problem (e.g., Graves disease).
Secondary hyperthyroidism: the thyroid is over-functioning because there is too much TSH around (causing over-stimulation of the thyroid). Main problem here is in the pituitary (e.g., pituitary adenoma that secretes TSH). Rare!
Tertiary hyperthyroidism: the thyroid is over-functioning because there is too much TRH around (causing release of too much TSH, resulting in over-stimulation of the thyroid). Main problem here is in the hypothalamus (e.g., TRH-producing adenoma). Rare, rare, rare!
Signs and symptomsCardiac manifestations (increased oxygen demand = increased contractility) rapid pulse cardiomegaly arrhythmias (especially atrial fibrillation. George
Bush Sr. had this.)
Neuromuscular manifestations (overactivity of sympathetic nervous system) nervousness tremor (see this best by placing a sheet of paper
on the patient’s outstretched hands) emotional lability (can lead to a psychiatric
misdiagnosis)
Eye manifestations (overstimulation of the muscle opening the upper eyelid) lid lag wide, staring gaze
Skin manifestations (the body is trying to lose heat) warm, moist, flushed skin
Gastrointestinal manifestations (overstimulation of gut = increased motility) diarrhea weight loss
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
A patient with hyperthyroidism:wide, staring gaze
thyroid pathology | 10 of 24

Skeletal manifestations (thyroid hormone causes increased bone resorption) osteoporosis.
Thyroid storm The most dreaded complication of
hyperthyroidism. Occurs when a hyperthyroid patient undergoes
some other major physiologic stress. Lots and lots of thyroid hormone is released.
The patient suddenly develops extreme hypermetabolism, which can lead to coma and death.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
thyroid pathology | 11 of 24

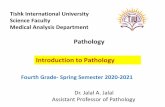
Causes (discussed in depth later)
Common Graves disease (85% of cases of hyperthyroidism
in US!) hyperfunctioning (hormone-producing)
multinodular goiter hyperfunctioning thyroid adenoma
Uncommon thyroiditis: DeQuervain thyroiditis, lymphocytic
thyroiditis ingestion of thyroid hormones (as treatment for
hypothyroidism) hyperfunctioning thyroid carcinoma TSH-producing pituitary adenoma struma ovarii (an ovarian tumor composed mostly
of thyroid tissue!) factitious hyperthyroidism (patient ingesting
thyroid-stimulating drugs to treat obesity or depression)
Diagnosis A diagnosis of hyperthyroidism is suspected
based on clinical findings (have a high index of suspicion!) and confirmed using laboratory tests.
Best screening tests for hyperthyroidism: TSH and free T4
The free T4 level is increased in hyperthyroidism (obviously). The TSH is decreased in primary hyperthyroidism, but elevated in secondary or tertiary hyperthyroidism.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Hyperthyroidism: T4 Primary:
TSH Secondary:
TSH
Most common cause of hyperthyroidism:
Graves disease
Most common cause of hyperthyroidism:
Graves disease
thyroid pathology | 12 of 24

HypothyroidismDefinition: a hypometabolic state caused by decreased levels of thyroid hormone.
CategoriesPrimary hypothyroidism: the thyroid gland is under-functioning because of some intrinsic thyroid gland problem (e.g., Hashimoto thyroiditis).
Secondary hypothyroidism: the thyroid is under-functioning because there is too little TSH around (causing under-stimulation of the thyroid). Main problem here is in the pituitary (e.g., pituitary gland destruction).
Tertiary hyperthyroidism: the thyroid is under-functioning because there is too little TRH around (causing diminished release of TSH, resulting in under-stimulation of the thyroid). Main problem here is in the hypothalamus (e.g., tumor replacing hypothalamus).
Signs and symptomsSlowing of mind and body Mental slowness, fatigue, irritability, loss of
interest. Often mistaken for depression. Some patients develop a bizarre sense of humor
(“myxedema wit”) or frank psychosis (“myxedema madness”). Note: People with Down syndrome often (50% of
the time) get hypothyroidism – watch carefully for signs of hypothyroidism, and don’t automatically attribute mental slowness to Downsyndrome.
Myxedema Accumulation of hydrophilic ground substance (e.g.,
glycosaminoglycans, hyaluronic acid) throughout the connective tissues of the body
Leads to non-pitting edema, coarsening of facial features, enlargement of the tongue, and deepening of the voice
Cardiac manifestations Slow pulse Diminished contractility Need to treat hypothyroid patients with care!
Gastrointestinal manifestations (understimulation of gut causes decreased motility) constipation
Skin manifestations (the body is trying to retain heat)
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Hypothyroidism is often misdiagnosed as depression.
thyroid pathology | 13 of 24

dry, cool, pale skin
Cold intolerance (from poor perfusion of the extremities)
Delayed deep tendon reflexes (“hung reflexes”) a useful physical exam sign to remember
Myxedema coma For some reason, hypothyroid patients may lapse
into stupor or coma when they get mild illnesses, or when they are exposed to cold weather.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
thyroid pathology | 14 of 24

CausesCongenital hypothyroidism (cretinism)*
Definition: hypothyroidism first presenting in infancy or childhood
Two causes: (1) iodine deficiency (epidemic cretinism)
In the past, this was common in places far away from the sea (Himalayas, inland China, and Africa). Now, foods are supplemented with iodine, so cretinism due to iodine deficiency is
less common. (2) developmental or genetic problems (sporadic
cretinism) These are rare. In these cases, the thyroid gland doesn’t form; thyroxine synthesis/release is defective; or thyroid hormone
receptors are defective. Symptoms reflect the impaired development
of the skeletal and central nervous systems and vary from mild (failure to thrive) to severe (profound mental retardation, short stature, and coarse facial features).
Treatment: thyroid hormone replacement (this helps – but doesn’t reverse damage). Prevention is best (in the US, babies are screened for hypothyroidism).
Acquired hypothyroidism (myxedema) Common causes
1. Hashimoto thyroiditis (the most common cause of hypothyroidism in U.S.)
2. iatrogenic causes: surgery, radiation, thyroid-inhibiting drugs Uncommon causes
1. goiter 2. infiltrative diseases (amyloidosis, sarcoidosis) 3. thyroiditis 4. dietary problems, such as excess iodine 5. secondary hypothyroidism6. tertiary hypothyroidism
Diagnosis Hypothyroidism is easy to diagnose and treat, but
you have to think of it! Best screening tests for hypothyroidism: TSH and
free T4 (sound familiar?)
* Cretin is from the French chrétien, meaning Christian or Christ-like. It was used to describe these children because they were considered so mentally handicapped as to be incapable of sinning.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Two patients with cretinism
Most common cause of hypothyroidism:
Hashimoto thyroiditis
thyroid pathology | 15 of 24

The free T4 level is decreased in hypothyroidism (obviously). The TSH is increased in primary hypothyroidism, but decreased in secondary or tertiary hypothyroidism.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
thyroid pathology | 16 of 24

Non-neoplastic thyroid disease ThyroiditisGeneral information Definition: inflammation of the thyroid gland. Four types of thyroiditis, as listed below. Hashimoto is by far the most common type of
thyroiditis. Women are affected more often than men. Patients with thyroiditis may be euthyroid,
hyperthyroid, or hypothyroid. Radioactive iodine uptake is decreased in
thyroiditis (radioiodine scans show diffuse “cold” thyroid tissue). Compare this to Graves disease!
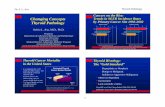
Hashimoto thyroiditis (aka: chronic autoimmune or chronic lymphocytic thyroiditis)
1. Clinical findings Common ( 1 million cases in US! Hashimoto
thyroiditis is the most common cause of hypothyroidism in areas of the world where there’s enough iodine).
Typical age range: 45 – 65. Female predominance in Hashimoto is even
more pronounced than in other types of thyroiditis (F:M = 10:1 to 20:1). This is typical of autoimmune disease.
Signs and symptoms: Enlarged, non-tender thyroid.
Patients gradually lose thyroid function and eventually become hypothyroid. (Sometimes, early on, there is transient hyperthyroidism as follicles are destroyed and colloid leaks out.)
2. Laboratory testing Thyroid function tests reflect the patient’s thyroid
status (eventually, overt hypothyroidism supervenes). Anti-thyroid autoantibodies can be useful. Anti-
peroxidase antibodies are pretty sensitive and specific for Hashimoto thyroiditis, whereas anti-thyroglobulin and anti-TSH-receptor antibodies can be present in either Hashimoto thyroiditis or Graves disease.
These autoantibodies are often detected using immunofluorescence testing (the tissue in question is stained with a fluorescent antibody that recognizes anti-peroxidase antibodies, or whatever autoantibodies you’re looking for). If the tissue has the antibody, it will light up.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Hashimoto antibodies:Anti-peroxidase.
thyroid pathology | 17 of 24

3. Histology Whopping lymphoid infiltrate: lots and lots of
lymphocytes, some plasma cells, and germinal centers. Hürthle cells: big follicular epithelial cells with
abundant, eosinophilic, granular (mitochondrion-stuffed) cytoplasm.
Damaged, disrupted follicles are abundant early on. Later, the gland is overrun by inflammation.
4. Pathogenesis Autoimmune destruction of thyroid gland. Main problem lies in the T cells: they recognize thyroid
antigens as foreign! So they stimulate B cells to make anti-thyroid antibodies, and are themselves cytotoxic to thyroid cells.
The unsuspecting B cells make lots of different anti-thyroid antibodies. The most important of these is the anti-TSH-receptor antibody. It blocks the action of TSH, leading to hypothyroidism.
DeQuervain thyroiditis (aka: subacute or granulomatous thyroiditis)
1. Clinical findings Much less common than Hashimoto thyroiditis Typical age range: 30 – 50. Recent history of upper respiratory infection.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Hashimoto histology:
1. lymphoid infiltrate (including germinal centers)2. Hürthle cells
De Quervain follows an URI, and it hurts!
Hashimoto thyroiditisImmunofluorescent stainFollicular epithelial cells positive for anti-peroxidase antibodies.
Hashimoto thyroiditisHematoxylin and eosin stainLymphoid follicle (center), lymphocytes (left), and Hürthle cells (big pink cells, right).
thyroid pathology | 18 of 24

Signs and symptoms: abrupt onset of pain in throat, radiating to ear. Painful, often enlarged, thyroid. Flu-like symptoms.
Patients are hyperthyroid for the first few weeks, then may develop transient, usually asymptomatic, hypothyroidism over the next few weeks.
The disease is self-limiting (unlike autoimmune thyroiditis, which is self-perpetuating), disappearing on its own in weeks to months.
2. Histology lymphocytes, histiocytes, and plasma cells damaged, disrupted follicles multinucleate giant cells (as in any foreign-body
giant cell reaction)
3. Pathogenesis Caused by viral infection (most commonly
coxsackie, but also mumps, measles, and others). Many patients have the HLA-B35 antigen.
Probably, some viral antigen, presented with HLA-B35, stimulates production of cytotoxic T cells that damage thyroid epithelium.
Damaged follicles leak colloid, causing a foreign-body giant cell reaction and enlargement of the thyroid gland.
The transient hyperthyroidism seen early in the disease is due to follicle damage (as in other cases of thyroiditis). The transient hypothyroidism occasionally seen late in the disease is presumably due to focal gland destruction.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
DeQuervain thyroiditisNote multinucleated giant cell (upper left) and residual, damaged follicle (lower right)
De Quervain histology:
1. Damaged follicles2. FBGC reaction
thyroid pathology | 19 of 24

Silent thyroiditis (aka: lymphocytic, painless, or subacute thyroiditis)
1. Clinical findings Much less common than Hashimoto thyroiditis. Typical age range: middle age; also occurs with
increased frequency following pregnancy. Signs and symptoms: painless, occasionally
slightly enlarged, thyroid. Some patients are completely asymptomatic (hence the name “silent”).
Mild, transient hyperthyroidism may develop over the first few weeks and last up to two months.
Disease is self-limited.
2. Histology Abundant lymphocytes. Some damaged, disrupted follicles. No germinal centers, plasma cells, or Hürthle
cells (like in Hash).
3. Pathogenesis Unresolved. Inherited component? High frequency of HLA-
DR3 and -DR5 in patients with lymphocytic thyroiditis. Autoimmune component? Patients make anti-
thyroglobulin and anti-thyroid peroxidase antibodies. Many have a family history of autoimmune thyroid disease, and some go on to develop overt autoimmune thyroiditis.
Reidel thyroiditis (aka: fibrosing thyroiditis)
1. Clinical findings Rare. Signs and symptoms: rock-hard, “woody” neck
mass. Patients may also have fibrosis elsewhere in the body (e.g., in retroperitoneum).
If enough of the gland is involved, hypothyroidism may ensue.
If the disease progresses far enough, may need surgery to relieve pressure on the trachea.
2. Histology Fibrosis.
3. Pathogenesis Fibroblasts proliferate and lay down collagen.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Silent thyroiditis histology:
1. lymphocytes2. no features of Hash
Reidel histology:
fibrosis
thyroid pathology | 20 of 24

Graves diseaseClinical findings1. Common disease (affects up to 2.5 % of US women!).2. F>>M. Typical age range: 20 – 40.3. Textbook clinical triad:
hyperthyroidism (thyroid gland is big and hyperfunctional)
ophthalmopathy (the usual “lid lag” of hyperthyroidism, plus exophthalmos)
dermopathy (“pretibial myxedema” – scaly thickening of skin over shins)
4. Real-life clinical picture: All patients with Graves have a goiter with at least some of the usual symptoms of hyperthyroidism (tachycardia, palpitations, tremor, anxiety). Many have ophthalmopathy, but only a few have dermopathy.
Laboratory testing free T4; TSH uptake of radioactive iodine (scans show
diffusely “hot” thyroid tissue).
Histology Crowded follicular epithelial cells form little
papillae. Lots of interstitial lymphocytes. Scanty colloid with scalloped borders (because
the epithelial cells are resorbing colloid).
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
The classic textbook triad – hyperthyroidism, ophthalmopathy (left) and dermopathy (right) – occurs in
Reidel thyroiditisTons of fibrosis with somepoor little trapped follicles.
thyroid pathology | 21 of 24

Pathogenesis1. Graves is an autoimmune disease caused by antibodies against the TSH receptor.
Autoantibodies bind to TSH receptors, where they cause thyroid hormone release and follicular epithelial proliferation.*
Thyroid over-functions (makes too much hormone) and overgrows (gets big).
2. The exact trigger for this autoimmune reaction is unknown. Genetic factors play a role in causing Graves disease, but it’s unclear exactly what that role is.
3. Autoimmune factors also cause ophthalmopathy and pretibial myxedema.
T cells and autoantibodies cross-react with eye muscles and with retro-orbital tissues, leading to inflammation and accumulation of matrix components. The increased pressure leads to exophthalmos.
T cells and autoantibodies probably also cross-react with pre-tibial fibroblasts, causing accumulation of matrix components and myxedema.
Treatment 1. Decrease symptoms.
A β-blocker will help alleviate the symptoms of hyperthyroidism related to increased sympathetic tone (tachycardia, palpitations, tremor, anxiety).
If exophthalmos is severe enough, it can occlude retinal vessels and lead to blindness. Surgical decompression of the orbit may be necessary.
2. Decrease thyroid hormone synthesis. drugs (propylthiouracil) radioiodine ablation (a one-time dose of 123I. Many
patients will later become hypothyroid and need hormone replacement.)
* The anti-TSH antibodies in Graves’ disease and the anti-TSH antibodies in Hashimoto’s disease recognize different epitopes on the TSH receptor! They also produce different results when bound to the TSH receptor. This is why the anti-TSH antibodies in Graves’ cause hyperthyroidism and the anti-TSH antibodies in Hashimoto’s cause hypothyroidism.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
fibrosis
Graves disease: epithelial cell papillae, scalloped colloid.
Graves: autoimm
une anti-TSH-
receptor antibodies.
What other disease has anti-TSH receptor antibodies?
Nobody except Ross reads these little comments.
thyroid pathology | 22 of 24

surgery
Simple and multinodular goiters General points1. “Goiter”1 just means a big thyroid gland (for whatever
reason). 2. Plain old garden-variety goiters (in other words, enlarged
thyroids that don’t show features of Graves disease or thyroiditis) are caused by defects in thyroid hormone synthesis. Either the patient is not getting enough iodine (endemic goiter), or there is some other defect (sporadic goiter). Bottom line: the thyroid makes less thyroid hormone, the TSH level goes up, and the thyroid grows bigger.
2. Simple and multinodular goiters are just two stages in this process.
Simple goiter (diffuse nontoxic goiter, colloid goiter)
the first stage (most long-standing simple goiters eventually evolve into multinodular goiters)
the thyroid may be normal in size or enlarged, and is smooth (no nodules)
Multinodular goiter the second stage (develops from a
preexisting simple goiter) the thyroid is huge and nodular
(bumpy)
Clinical findings Early on, patients have a simple goiter. Years later, multinodular (and huge!) goiter
develops. Most patients are euthyroid. Some patients have hyperfunctioning
nodules, which produce lots of thyroid hormone and cause hyperthyroidism (this is called Plummer syndrome or toxic multinodular goiter).
A few patients, even with their great big thyroids, just can’t make enough thyroid hormone and become hypothyroid.
Laboratory testing
1. Most patients with goiters are euthyroid.
1 The word goiter comes from the middle French word goitron which comes from the Latin guttur, which means throat.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
multinodular goiter
thyroid pathology | 23 of 24

Laboratory values in patients with goiters
Some (with a hyperfunctioning nodule) are hyperthyroid, and a few (especially those with hereditary enzyme defects) are hypothyroid.
thyroid status T4 TSH
euthyroid normal hyperthyroid hypothyroid
2. Radioiodine uptake is uneven, with “hot” active areas, and “cold” inactive areas.
Histology Early on (in simple goiter), the follicular
epithelial cells, stimulated by all the TSH around, become hyperplastic (cells get taller, pile up).
Later (still in simple goiter stage), the epithelium gets exhausted and involutes, resulting in oversized, colloid-packed follicles.
Hyperplasia and involution occur in cycles. Some areas of the thyroid may be hyperplastic, and others may be involuting. All this hyperplasing (hyperplasing?) and involuting causes hemorrhage and fibrosis.
Finally (this is the multinodular stage), the hemorrhage and fibrosis become massive, and the thyroid gets really big (>100 grams). The parenchyma separates into nodules (composed of follicles) bound by fibrotic bands.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
A patient with a multinodular goiter
GoiterHematoxylin and eosin stainProliferating (left) and involuting (right) follicular epithelium.
thyroid pathology | 24 of 24

Pathogenesis1. Endemic goiter is caused primarily by iodine deficiency.
Lack of iodine in the diet ( can’t make thyroid hormone TSH goes up thyroid gland becomes hyperplastic).
A diet rich in foods called goitrogens (such as cabbage, brussels sprouts, turnips, cauliflower, cassava root) doesn’t help matters. Goitrogens interfere with T3
and T4 synthesis, causing TSH elevation and thyroid gland hyperplasia.
2. Sporadic goiter is caused by things other than iodine deficiency. In most patients, a specific cause is never found. Some of the known causes include: ingestion of substances that interfere with
thyroid hormone synthesis hereditary enzyme defects that interfere with
thyroid hormone synthesis (for example, defects in iodide absorption or transport).
Treatment Often these patients are treated with
levothyroxine (acts like thyroid hormone) in the hope that TSH will be suppressed, and the goiter will shrink.
Caution! The iodine-deficient multinodular goiter is under heavy TSH stimulation…if you give iodine to this patient (even the small amount given in radiographic procedures), acute hyperthyroidism and even hyperthyroid crisis can occur! This is called the Jod-Basedow phenomenon.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Eat your goitrogens(but not too many).
thyroid pathology | 25 of 24

Neoplastic thyroid diseaseIntroduction: the thyroid noduleThe bump that gets attention Most thyroid neoplasms are discovered when
the patient (or physician) feels a bump (or nodule) on the thyroid.
Thyroid nodules are common! 5 million people (2-4% of adults) in the US have one.
Fortunately, most turn out to be benign: either adenomas, or big nodules in a multinodular goiter.
Thyroid carcinoma is uncommon (accounts for <1% of all thyroid nodules) and is usually not very aggressive (most patients live at least 20 years after diagnosis).
Still, every thyroid nodule needs a work-up.
Is it cancer? How to work up a thyroid nodule:1. Clinical clues
You can look at all sorts of things for clues to whether a nodule is cancerous: patient’s age and sex, whether nodule is solitary or multiple, whether it takes up radioactive iodine or not (see Robbins p. 1140 for what these clues mean).
BUT: these things just hint at the likelihood of cancer. If you are at all concerned about malignancy, you need to look at the nodule under a microscope.
2. Making a diagnosis First, get a fine-needle aspiration (FNA). Fine
needle aspiration has become a routine procedure (and not just for thyroid nodules, but for any suspicious lump or bump within needle’s reach). It’s a great screening technique (cheap, fast, pretty painless) to find out which bumps need to be cut out..
The nodule needs to be cut out if the FNA shows any of these: obvious cancer lots of follicles (even if they look
benign) Orphan Annie nuclei, or nuclei with
grooves
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
nodule nodule
thyroid pathology | 26 of 24

Thyroid adenomaClinical findings Common. Most patients are adults. Most patients are euthyroid. Occasionally,
an adenoma will become hyperfunctional (produce lots of thyroid hormone); these patients may become hyperthyroid.
Laboratory testing Most patients have normal levels of thyroid
hormone and TSH. Radioiodine scanning: most adenomas look
“cold.” The few adenomas that are hyperfunctional look “hot.”
Histology Lots of thyroid follicles. Follicles are lined by well-differentiated
epithelial cells (that is, cells that look almost exactly like normal (non-neoplastic) follicular epithelial cells).
Don’t memorize the different adenoma subtypes that Robbins lists (non gradus anus rodentum)*. All adenomas, whatever their histologic appearance, act the same.
Treatment/prognosis Remove it surgically. Why, if it’s just a benign
tumor? Because it’s often difficult (on biopsy or FNA) to distinguish an adenoma (benign, with lots of follicles) from a follicular adenocarcinoma (malignant, with lots of follicles). So just take the thing out, to make sure it’s not cancer.
Excellent prognosis (thyroid adenomas are benign, and have virtually no tendency to turn malignant).
* Not worth a rat’s ___.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Thyroid adenomaLots and lots of
thyroid pathology | 27 of 24

Thyroid carcinomaPapillary adenocarcinoma1. Clinical findings
Most common type of thyroid carcinoma (80% of all cases).
Best prognosis of all types of thyroid carcinoma.
Affects adults, primarily, but also occurs in children.
2. Histology Growth pattern: papillary (looks like
inside-out, branching glands). Cells:
origin: follicular epithelium nuclei look empty or cleared-out, like
Orphan Annie’s eyes*
contain nuclear grooves and pseudo-inclusions (from cytoplasmic invaginations)
Other features: psammoma bodies concentrically lamellated calcium
structures
* Papillary adenocarcinoma memory aid: think of Orphan Annie!1. often affects younger women.2. tends to stay around for years without getting any bigger.3. is usually well-behaved; seldom kills people.4. has nuclei that resemble Orphan Annie’s eyes5. has psammoma bodies (from the Greek psammos, or sand): Annie’s dog is named
Sandy.(From Ed’s pathology notes at www.pathguy.com)
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
thyroid pathology | 28 of 24

also seen in papillary carcinomas of other organs
not seen in other types of thyroid carcinoma
3. Treatment/prognosis Surgical removal Metastases are usually via lymphatics, to
adjacent nodes Excellent prognosis (10-year survival is
98%)
Follicular adenocarcinoma1. Clinical findings
Uncommon (~15% of all thyroid carcinomas) 2. Histology
Growth pattern: follicular (can look a lot like normal thyroid!
Cells: origin: follicular epithelium uniform; often well-differentiated*
no papillary carcinoma cell features
* A well-differentiated tumor is one that closely recapitulates its tissue of origin. A poorly-differentiated tumor looks very little like its tissue of origin (sometimes, it’s hard to tell what kind of tumor it is). Well-differentiated follicular adenocarcinomas of the thyroid have lots of easily-recognizable follicles lined by cells that look a lot like normal, benign follicular epithelial cells. Well-differentiated tumors can be hard to distinguish from their benign neoplastic counterparts – or even from normal tissue! In general, well-differentiated tumors tend to behave better than poorly-differentiated tumors.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
nuclear pseudo-inclusion
cleared-out nuclei
nuclear grooves
papillary pattern psammoma body
thyroid pathology | 29 of 24

3. Future pathologists beware: This tumor can be hard to distinguish from a thyroid
adenoma! *
Sometimes the only signs of malignancy are:1. epithelial cells invading blood vessels (“vascular
invasion”)2. tumor cells extending through the thyroid capsule
4. Treatment/prognosis Surgical excision. May give some thyroid hormone to
suppress the patient’s TSH (to prevent tumor stimulation).
Metastasis is usually via blood vessels, to lungs or bone. Good prognosis.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
follicular pattern vascular invasion
thyroid pathology | 30 of 24

Medullary carcinoma1. Clinical findings
Rare (~5% of all thyroid carcinomas)
Medullary carcinoma is an endocrine tumor (papillary and follicular thyroid carcinomas are epithelial tumors). The cell of origin is the thyroid C-cell.
It may occur sporadically, or as part of MEN-II, or as part of familial thyroid carcinoma syndrome.
2. Histology Pattern:
cells often form vague nests Cells:
large, polygonal Other
features: amyloid deposits 3. Treatment/prognosis
Anyone you suspect of having MEN-II or familial thyroid carcinoma needs genetic counseling and close follow-up.
Bad prognosis overall (5 year survival is 50%), and it’s even worse when in the setting of MEN-II.
Anaplastic thyroid carcinoma1. Clinical findings
Rare (<5% of all thyroid carcinomas) Presents as a rapidly-enlarging, bulky
neck mass, which has often already metastasized widely.
2. Histology Pattern: cells often in sheets Cells: anaplastic*
Future pathologists: because this tumor is so poorly-differentiated, it can be hard to distinguish it from other types of tumors (e.g., lymphoma). Special stains (that stain calcitonin brown) can help.
3. Treatment/prognosis No effective treatment. Very bad prognosis (most patients die
within one year).
* Anaplastic means undifferentiated. Anaplastic cells of any type tend to be pleomorphic (varying in size and shape), with a high nuclear-cytoplasmic ratio, hyperchromatic (dark-staining) nuclei, and visible nucleoli. See Robbins p. 273 for a refresher.
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
Medullary carcinoma.Vague nesting pattern (left) and amyloid (right).
Anaplastic thyroid carcinoma.Wild anaplasia, including a giant
thyroid pathology | 31 of 24

Review1. Describe the common signs and symptoms, causes, and laboratory workup of:
Hypothyroidism (congenital and acquired) Hyperthyroidism
2. Fill in the following tables. Try to pick just 2 or 3 words so you can remember them.
AKAClinical findings
Hypo-, hyper- and/or
euthyroid?Histology Pathogenesis
Hashimoto
De Quervain
silent
Reidel
Graves
Common or rare? HistologyOther unique features,
if anyPrognosis
Adenoma
Papillary CA
Follicular CA
Medullary CA
Anaplastic CA
3. Fill in the following table with the most likely diagnoses. Which are the most common combinations?
low normal high
low
normal
high
4. How would you work up a patient with a thyroid nodule?
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
TSH
free T4
thyroid pathology | 32 of 24

Can you name the disease?
introduction | hyper- | hypo- | non-neoplastic | neoplastic | review
thyroid pathology | 33 of 24