Therapeutic Hotline Treatment of Prurigo Nodularis and Lichen Simplex Chronicus With Gabapentin
-
Upload
apiffaulia -
Category
Documents
-
view
6 -
download
0
description
Transcript of Therapeutic Hotline Treatment of Prurigo Nodularis and Lichen Simplex Chronicus With Gabapentin

THERAPEUTIC HOTLINE
Treatment of prurigo nodularis andlichen simplex chronicus
with gabapentinGulsum Gencoglan, Isil Inanir & Kamer GunduzDepartment of Dermatology, Medical Faculty of Celal Bayar University,Turkey
ABSTRACT: Psychocutaneous conditions are frequently encountered in dermatology practice. Prurigonodularis and lichen simplex chronicus are two frustrating conditions that are classified in this cat-egory. They are often refractory to classical treatment with topical corticosteroids and antihistamines.Severe, generalized exacerbations require systemic therapy. Phototherapy, erythromycine, retinoids,cyclosporine, azathiopurine, naltrexone, and psychopharmacologic agents (pimozide, selective sero-tonin reuptake inhibitor antidepressants) were tried with some success. Here five cases with lichensimplex chronicus and four cases with prurigo nodularis, who responded well to gabapentin, arepresented.
KEYWORDS: gabapentin, lichen simplex chronicus, prurigo nodularis, pruritus, therapy
Introductiondth_1314 194..198
Psychocutaneous conditions are frequentlyencountered in dermatology practice. At least onethird of dermatology outpatients require consider-ation of associated emotional and psychosocialfactors (1). Emotional stress especially plays a keyrole in inducing itch, followed by scratching.Prurigo nodularis (PN) and lichen simplex chroni-cus (LSC) are two frustrating conditions classifiedin this category (2,3).
Prurigo nodularis is characterized by multiplefirms, generally 0.5–2 cm-sized papules andnodules, whereas LSC appears as lichenified, thick-ened palm-sized plaques. These two conditions
have several similarities and some authors havegrouped them together (2). Intense pruritus andscratching are the main symptoms and strictly cor-relate to the persistence and the progression of skinlesions. Patients report having temporary relief withscratching. Thickening, pigmentation, and rarelyulceration are clinical features. Atopy and an asso-ciated systemic pruritic disorder may be associatedwith these two disorders. Psychogenic factors play adominant role in both; pruritus becomes worse,lesions are induced and triggered with stress.
Related with the unclear pathogenesis, treat-ment of PN and LSC is difficult. Topical antipruriticagents, corticosteroids, calcineurin inhibitors andcapsaicin, systemic antihistamines, and photo-therapy mainly have been used to treat these dis-eases (2,4). In calcitrant and severe forms of PN,cyclosporine, thalidomide, opiate receptor antogo-nists, laser, and naltrexone have been usedwith variable success (4–6). Herein, we describe
Address correspondence and reprint requests to: GulsumGencoglan, MD, Assistant Professor, Department ofDermatology, Medical Faculty of Celal Bayar University, 45030Manisa, Turkey, or email: [email protected].
194
Dermatologic Therapy, Vol. 23, 2010, 194–198Printed in the United States · All rights reserved
© 2010 Wiley Periodicals, Inc.
DERMATOLOGIC THERAPYISSN 1396-0296

five patients with LSC, and four patients with PN,who responded well to gabapentin, are presented.
Patients and methods
All nine patients (four with PN and five with LSC)were treated with gabapentin. Four males and fivefemales with an average age of 44.8 years hadseverely pruritic papules and nodules existing for2–20 years. Lesions were only on extremities inthree patients; the other six patients also hadtruncal involvement. All nine patients been treatedwith antihistamines, corticosteroids, photo-therapy, and antidepressants. Gabapentin 300 mg/day treatment was initiated and the dosage wasgradually increased to 900 mg/day (300 mg/day, 3days; 600 mg/day, 3 days, and finally 900 mg/day).The patients were seen every month. Improvementwas assessed, with pruritus severity evaluated bythe patient and clinical observation carried out bya physician. Data on the patients’ medical historyand therapy are shown in Table 1.
Results
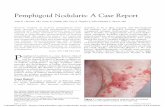
After 2 months, all patients had at least partialremission. This improvement continued in sevenpatients throughout the therapy period, except inthe first patient (Table 2). This patient had severeanxiety and depression and stopped gabapentinafter 4 months when his lesions had gone worse.Gabapentin was used 900 mg daily for 3 or 4months until a desired effect was achieved. Inpatients 2 and 6, response to gabapentin was suffi-cient so that it was discontinued after 3 months. Inthe remaining patients, gabapentin was reducedgradually from 600 mg/day to 300 mg/day. Totaltreatment period ranged from 4 to 10 months.Patients were followed for 3 months after stoppinggabapentin, and the clinical improvement wasconsistent in the follow-up period (Table 1). Half ofthe patients reported mild pruritus at the end ofthe therapy and in the follow-up period, but theirlesions have not recurred. In all patients prurituswas never as severe as in the beginning and whatwas present responded to topical lubricants. Noside effect was experienced, except tolerable seda-tion in three patients (FIG. 1).
Discussion
Pruritus is an unpleasant sensation that induces adesire to scratch. This complex process involves
the stimulation of free nerve endings in the skinand transmission through the C fibers to the dorsalhorn of the spinal cord, and then, via the spinotha-lamic tract to the cerebral cortex for processing.Along with scratching, inflammatory mediatorssuch as histamine, serotonin, cytokines, andopioids which induce or aggravate pruritus arereleased, resulting in an itch–scratch cycle (7).Scratching and rubbing lead to several skin condi-tions like PN and LSC, which are generally resistantto therapy. Our patients did not respond to severaltopical or oral medications given previously.
Gabapentin is a potent anticonvulsant alsoused for the treatment of neuropathic pain syn-dromes such as diabetic neuropathy and post-herpetic neuralgia (8–10). Itch follows similarneural pathways to pain from skin to the sensorycortex, thus leading to the use of gabapentin forpruritus. In recent years, the efficacy of gabapen-tin for notalgia paresthetica (11), uremic (12), bra-chioradial (13,14), idiopathic (15), and post-burnpruritus (16) has been reported. Dereli et al.reported a patient with PN treated successfullywith gabapentin (5).
The action mechanism of gabapentin on pruri-tus is unknown; however, various hypotheses havebeen suggested. Pruritus is a nociceptive stimulusand gabapentin was shown to increase the thresh-old of nociception (17). Its primary effect may berelated to an increase in the concentration of theexcitatory neurotransmitter gamma-aminobutyricacid (GABA) as in pain syndromes. Gabapentinblocks the calcium channels located in the spinalcord and inhibits the release of GABA as wells asincreasing the synthesis of GABA by altering theactivity of glutamic acid decarboxylase (10). Anincrease in GABA in the spinal cord secondarily
a b
FIG. 1. (a) Before treatment. (b) After treatment.
Prurigo nodularis and lichen simplex chronicus
195

inhibits release of calcitonin gene-related peptide(CGRP, an itch mediator) from afferent neurons. Italso affects central itching by modulating m-opioidreceptors (15). Opioid peptides also have a periph-eral action, potentiating itching due to otheragents. The origins of pruritus in the conditionsnoted above are not well understood but may beperipheral, central, and psychogenic (18). There-
fore, more than one mechanism seems to be asso-ciated with the effect of gabapentin.
Another therapeutic, botulinum toxin, has alsobeen found useful in pruritic syndromes of notalgiaparesthetica and lichen simplex (19,20). It inhibitsthe release of substance P and CGRP like gabapen-tin. It seems that the antipruritic effects of bothdrugs depend upon at least these itch mediators.
Table 1. Medical data of the patients
Patientno. Age Sex
Durationof disease(years) Previously admitted therapy
Medicalhistory Therapy period (months)
Duration ofremission(months)
1 17 M 2.5 Hydroxyzine hydrochlorideLoratadinEscitalopramAmitriptyline HCLTopical corticosteroids
Anxietydisorder
4 months (900 mg/day) –
2 39 F 5 Hydroxyzine hydrochlorideDesloratadinCetirizine hydrochlorideMethyl prednisolone
(30 mg/day)
None 3 months (900 mg/day) 4
3 78 M 20 Cetirizine hydrochlorideAmitriptyline HCLMianserin HCLTopical corticosteroidsEmollientsUVB
COPD 3 months (900 mg/day)+3 months (600 mg/day)+4 months (300 mg/day)
10
4 21 M 15 Hydroxyzine hydrochlorideCetirizine hydrochlorideDapsonPrednisolone 302 mg/dayAmitriptyline HCLSertralin HCLTopical corticosteroids
None 3 months (900 mg/day)+3 months (600 mg/day)+4 months (300 mg/day)
7
5 40 F 10 Hydroxyzine hydrochlorideLoratadinAmitriptyline HCLSertralin HCLTopical corticosteroids
None 4 months (900 mg/day)+2 months (600 mg/day)+4 months (300 mg/day)
6
6 52 F 2 Hydroxyzine hydrochlorideAcrivastinCetirizine hydrochlorideTopical corticosteroids
DiabetesHypertensionHyperlipidemia
3 months (900 mg/day) 10
7 53 M 29 AcrivastinCetirizine hydrochlorideHydroxyzine hydrochlorideLoratadinTopical corticosteroids
None 4 months (900 mg/day)+2 months (600 mg/day)
9
8 58 F 2 LoratadinHydroxyzine hydrochlorideAcrivastinTopical corticosteroids
DiabetesHyperlipidemia
4 months (900 mg/day)+2 month (600 mg/day)
8
9 46 F 15 AcrivastinCetirizine hydrochlorideHydroxyzine hydrochlorideLoratadinTopical corticosteroids
None 1 months (900 mg/day)+3 months (600 mg/day)+4 months (300 mg/day)
9
COPD, chronic obstructive pulmonary disease; HCL, hydrochloric acid; UVB, ultraviolet B.
Gencoglan et al.
196

Therapeutic dosing of gabapentin is different invarious trials. It is generally started at 300 mg dailydose and increased with the same amount in neu-ropathic syndromes. Besides the most commonadverse effect of sedation, it can rarely cause pan-cytopenia, cholestasis, hypersensitivity syndrome,and dyskinesia. It has been safely dosed to amaximum of 3600 g/day (21). In pruritic condi-tions, it was found to be effective with dosesof 600 mg/day for notalgia paresthetica (11),1200 mg/day for PN (5), and 1800 mg/day for gen-eralized pruritus (15). It is hard to have a consensuson dosing with these case reports, but all dosesreported were under the safety margin. Prurituswas controlled with 900 mg/day in our patients,and only a few tolerable side effects were observed.We suggest starting with 300 mg/day and increas-ing gradually until the effective minimal dose.
In conclusion, we suggest that gabapentin mightbe an important alternative in patients with chronicprurigo. Although it has been used for several neu-ropathic pain disorders and pruritus of differentdisorders, there is only one case report on the effi-cacy of gabapentin in chronic PN (5). The smallnumber of patients in our study, the uncontrolledand retrospective nature of the study, the unequalfollow-up periods, and treatment schedules are thelimitations of this report. Controlled trials are indi-cated to confirm our results in addition to a moreuniform dosing. The results of therapy with gaba-pentin in our patients are encouraging.
References
1. Gupta MA, Gupta AK. Psychodermatology: an update. J AmAcad Dermatol 1996: 34: 1030–1046.
2. Burgin S. Nummular Eczema and Lichen SimplexChronicus/Prurigo Nodularis. In Wolf K, Goldshimith LA,Katz SI, Gilchrest BA, Paller AS, Leffel DJ, eds. Fitzpatrick’s
dermatology in general medicine, Vol. I, 7th ed. New York,NY: Mc Graw-Hill Companies, 2008: 158–162.
3. Lotti T, Buggiani G, Prignano F. Prurigo nodularis andlichen simplex chronicus. Dermatol Ther 2008: 21: 42–46.
4. Lee MR, Shumack S. Prurigo nodularis: a review. Australas JDermatol 2005: 46: 211–220.
5. Dereli T, Karaca N, Inanır I, Öztürk G. Gabapentin for thetreatment of recalcitrant chronic prurigo. Eur J Dermatol2008: 18: 85–86.
6. Wallengren J. Prurigo: diagnosis and management. Am JClin Dermatol 2004: 5: 85–95.
7. Stander S, Weisshaar E, Luger TA. Neurophysiological andneurochemical basis of modern pruritus treatment. ExpDermatol 2008: 17: 161–169.
8. Singh D, Kennedy DH. The use of gabapentin for the treat-ment of postherpetic neuralgia. Clin Ther 2003: 25: 852–889.
9. Rose MA, Kam PC. Gabapentin: pharmacology and its usein pain management. Anaesthesia 2002: 57: 451–462.
10. Bennett MI, Simpson KH. Gabapentin in the treatment ofneuropathic pain. Palliat Med 2004: 18: 5–11.
11. Loosemore MP, Bordeaux JS, Bernhard JD. Gabapentintreatment for notalgia paresthetica, a common isolatedperipheral sensory neuropathy. J Eur Acad DermatolVenereol 2007: 21: 1413–1450.
12. Gunal AI, Ozalp G, Yoldas TK, Gunal SY, Kirciman E,Celiker H. Gabapentin therapy for pruritus in haemo-dialysis patients: a randomized, placebo-controlled,double-blind trial. Nephrol Dial Transplant 2004: 19:3137–3139.
13. Bueller HA, Bernhard JD, Dubroff LM. Gabapentin treat-ment for brachioradial pruritus. J Eur Acad DermatolVenereol 1999: 13: 227–228.
14. Winhoven SM, Coulson IH, Bottomley WW. Brachioradialpruritus: response to treatment with gabapentin. Br J Der-matol 2004: 150: 786–787.
15. Yesudian PD, Wilson NJE. Efficacy of gabapentin in themanagement of pruritus of unknown origin. Arch Dermatol2005: 141: 1507–1509.
16. Mendham JE. Gabapentin for the treatment of itching pro-duced by burns and wound healing in children: a pilotstudy. Burns 2004: 30: 851–853.
17. Gustafsson H, Flood K, Berge OG, Brodin E, OlgartL, Stiller CO. Gabapentin reverses mechanical allodyniainduced by sciatic nerve ischemia and formalin-inducednociception in mice. Exp Neurol 2003: 182: 427–434.
Table 2. Outcome of the therapy
Patient no.
Intensity of pruritus Status of the lesions
Pretreatment 2 months End of the therapy 2 months End of the therapy
1 Severe Slight Very intense Partial remission No remission2 Severe Slight Slight Partial remission Complete remission3 Severe Moderate Slight Partial remission Complete remission4 Severe Moderate Slight Partial remission Complete remission5 Severe Slight None Complete remission Complete remission6 Severe Slight None Partial remission Partial remission7 Severe Slight None Partial remission Complete remission8 Severe Slight None Partial remission Complete remission9 Severe Moderate Slight Partial remission Partial remission
Prurigo nodularis and lichen simplex chronicus
197

18. Yosipovitch G, Greaves M, Schmelz M. Itch. Lancet 2003:361: 690–694.
19. Weinfeld PK. Successful treatment of notalgia parestheticawith botulinum toxin type A. Arch Dermatol 2007: 143:980–982.
20. Heckmann M, Heyer G, Brunner B, Plewig G. Botulinumtoxin type A injection in the treatment of lichen simplex:
an open pilot study. J Am Acad Dermatol 2002: 46: 617–619.
21. Backonja M, Glanzman RL. Gabapentin dosing for neuro-pathic pain: evidence from randomized, placebo con-trolled clinical trials. Clin Ther 2003: 25: 81–104.
Gencoglan et al.
198

Copyright of Dermatologic Therapy is the property of Wiley-Blackwell and its content may not be copied or
emailed to multiple sites or posted to a listserv without the copyright holder's express written permission.
However, users may print, download, or email articles for individual use.










![Prurigo [L. “the itch”]](https://static.fdocuments.us/doc/165x107/56815d3c550346895dcb422a/prurigo-l-the-itch.jpg)






![Prurigo nodularis - vid svårare symtom kan …1 Prurigo nodularis är ett tillstånd som kännetecknas av lång-varigt bestående kliande knutor i huden [1]. Det är ovanligt och](https://static.fdocuments.us/doc/165x107/5e3500118904ec496a0dae54/prurigo-nodularis-vid-svrare-symtom-kan-1-prurigo-nodularis-r-ett-tillstnd.jpg)
