The RACGP’s has been updated and is in its 9th edition Practice/2017/… · late 2016, with new...
Transcript of The RACGP’s has been updated and is in its 9th edition Practice/2017/… · late 2016, with new...

www.racgp.org.au/goodpractice
INSIDE
Mental healthGPs’ role in better outcomes in
youth mental health in rural Australia
Rural medicineThe RACGP’s Fellowship in
Advanced Rural General Practice
Secure dataData backup and recovery is an essential
preventive activity in general practice
ISSUE 1–2, JANUARY–FEBRUARY 2017
The RACGP’s Guidelines for preventive activities in general practice has been
updated and is in its 9th edition


Good Practice is printed on PEFC certified paper, meaning that it originates from forests that are managed sustainably. PEFC is the Programme for the Endorsement of Forest Certification schemes. PEFC is an international certification programme promoting sustainable forest management which assures consumers that a forest product can be tracked from a certified, managed forest through all steps of processing and production in the supply chain by a Chain of Custody process.
3
Editorial notes
© The Royal Australian College of General Practitioners 2017. Unless otherwise indicated, copyright of all images is vested in the RACGP. Requests for permission to reprint articles must be made to the editor. The views contained herein are not necessarily the views of the RACGP, its council, its members or its staff. The content of any advertising or promotional material contained within Good Practice is not necessarily endorsed by the publisher.
We recognise the traditional custodians of the land and sea on which we work and live.
Published by
The Royal Australian College of General Practitioners 100 Wellington Parade East Melbourne Victoria 3002
03 8699 0414 [email protected] www.racgp.org.au/goodpractice
ABN 34 000 223 807 ISSN 1837-7769
Editor: Paul HayesJournalist: Amanda LyonsGraphic Designer: Nick HopkinsProduction Coordinator: Beverley GutierrezPublications Manager: Anthony Lynch
Advertising enquiriesSye Hughes0474 500 [email protected]
ContentsIssue 1–2, January–February 2017
06
04 Your College
RACGP news and events for February.
06 RACGP Resource
Preventive activities The RACGP’s Guidelines for preventive
activities in general practice has been updated and is now in its 9th edition.
10 Youth Mental Health
Mind the gap GPs are crucial to achieving better
outcomes in youth mental health throughout rural Australia.
14 Rural Healthcare
Advancing rural skills The RACGP’s Fellowship in Advanced
Rural General Practice offers GPs in rural and remote Australia the opportunity
to reflect on their abilities and develop further skills to help their communities.
17 Ethics in General Practice
Drugs of dependence Legislation and regulation.
18 Data Backup
Information lockdown Implementing an effective system for
data backup and recovery is an essential preventive activity for the health
of a general practice.
22 GP Profile
Patient connections Dr Wence Vahala continues a family
legacy of dedication to general practice.
24 In My Practice
City care Adelaide Health Care is a city practice
with an eclectic patient demographic and the skills to match.
26 RACGP Specific Interests
Disaster management The RACGP’s Disaster Management
network works hard to ensure GPs are included in disaster planning all
around Australia.
Reprinted from Good Practice Issue 1–2, January–February 2017
22
10
18
24

4
YOUR COLLEGE
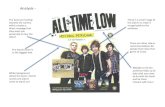
Your specialist in life The RACGP launched the latest phase of its community awareness campaign in late 2016, with new television, print and social media advertisements receiving overwhelmingly positive feedback.
‘We are delighted with the response to the new campaign,’ RACGP President Dr Bastian Seidel told Good Practice. ‘The feedback is validation of the fundamental role GPs play in the lives of people all over Australia.’
The campaign’s key message – ‘I’m not just a GP. I’m your specialist in life’ – clearly resonates with healthcare professionals, as well as the 86.5% of Australians who visit their GP at least once a year.
‘The main aim of our “Specialist in life” campaign is to highlight the special relationship we really have with our patients,’
Dr Seidel said at the launch. ‘Seeing your GP, for patients, is really not just a business transaction, it’s not a customer relationship. It’s much, much more than that.
‘We can make decisions on [patients’] health in partnership together and our patients know this. That’s why they come and see us on a regular basis.
‘They really know that we are looking after them and looking after their family. We know them really well.
‘We are indeed their specialist in life. We keep them well, we keep them healthy.’
According to Dr Seidel, this type of campaign is vital in not only raising the profile of GPs and the role they play, but also in creating greater awareness of the difficulties Australia’s primary care professionals are currently
facing in delivering high-quality services. This is particularly true in light of the Federal Government’s ongoing freeze on Medicare Benefits Schedule (MBS) rebates.
‘Patients have been unfairly targeted, general practice has been unfairly targeted,’ Dr Seidel said.
‘One in 20 patients already avoids seeing their GP because of costs.
‘If you delay treatment the consequences will be disastrous and you will end up in a hospital environment.
‘That’s bad for your health and it’s bad for the health system. It costs the taxpayer more in the long-run and patients potentially pay with their lives.
‘Patients are concerned. That’s what we are hearing day after day after day.’
RACGP President Dr Bastian Seidel speaking to the media at the launch of the ‘Specialist in life’ campaign.
Reprinted from Good Practice Issue 1–2, January–February 2017

5
RACGP events calendar
February 2017
VIC
Clinical Emergency Management Program intermediate Saturday 11 February, 8.00 am – 5.00 pm, Parkview Hotel, Melbourne
Contact 03 8699 0488 or [email protected]
QLD
Beyond pregnancy and birth – Surviving the fourth trimesterSaturday 18 February, 8.30 am – 4.30 pm, College House, Brisbane
Contact 07 3456 8930 or [email protected]
SA
Chronic conditions ALMSaturday 11 February, 8.30 am – 4.30 pm, Rydges South Park, Adelaide
Contact 08 8267 8310 or [email protected]
WA
New Fellows connect – Session 1: DermoscopyTuesday 21 February, 6.30–9.00 pm, College House, Perth
Contact 08 9489 9555 or [email protected]
WA
Skin Deep: Dermatology updateSaturday 11 February, 8.30 am – 5.00 pm, College House, Perth
Contact 08 9489 9555 or [email protected]
SA
SA New Fellows social eventFriday 24 February, 6.00–8.00 pm, College House, North Adelaide
Contact 08 8267 8310 or [email protected]
NSW
Starting a private practiceSaturday 11 February, 8.45 am – 4.15 pm, College House, North Sydney
Contact 02 9886 4700 or [email protected]
VIC
Perform CPR – A workshop for GPsTuesday 28 February, 6.00–8.00 pm, RACGP House, Melbourne
Contact 03 8699 0488 or [email protected]
QLD
New Fellows career development nightWednesday 15 February, 6.00–9.00 pm, ANZ Office, Brisbane
Contact 07 3456 8930 or [email protected]
SA
Emergency update for practice nurses (including CPR)Tuesday 28 February, 6.30–9.30 pm, College House, North Adelaide
Contact 08 8267 8310 or [email protected]
Visit www.racgp.org.au/education/courses/racgpevents for further RACGP events.
New triennium The RACGP Quality Improvement and Continuing Professional Development (QI&CPD) 2017–19 triennium commenced 1 January.
The QI&CPD Program supports Australian GPs in maintaining and improving professional knowledge and skills, allowing them to provide the best possible care. The 2017–19 triennium is focused on encouraging and facilitating reflective learning to help GPs identify opportunities that enhance their daily practice.
The RACGP has developed a new online planning learning and need (PLAN) quality improvement activity to help GPs structure their learning for the new triennium. The mandatory PLAN activity enables GPs to map out and document areas of learning on which they would like to focus in order to best meet the needs of patients and the community, as well as their personal aspirations.
The 2017–19 triennium requires a minimum of 130 QI&CPD points, consisting of:• one PLAN quality improvement activity • one category 1 activity • one cardiopulmonary resuscitation (CPR) activity.GPs’ continuing professional development includes a range of activities to meet learning needs relevant to their scope of practice. Activities that facilitate review and evaluation of GPs’ own practice include: • supervised clinical attachment • plan, do, study, act (PDSA)• clinical audit • general practice research • evidenced-based medical journal club • small-group learning • PLAN quality improvement activity. Visit www.racgp.org.au/education/qicpd-2017-19-program or contact a QI&CPD office for more information.
Selection managementThe RACGP will assume responsibility for selection of more than 90% of Australian General Practice Training (AGPT) Program candidates, commencing with the 2018 intake.
According to RACGP President Dr Bastian Seidel, this will ensure the most skilled registrar applicants are granted entry to general practice training.
‘The RACGP will be able to better align selection to the knowledge, skills and attitudes required of an RACGP Fellow,’ he said. ‘Responsibility and oversight at the entry stage of the recruitment program for GPs further endorses the RACGP’s commitment to ensuring GPs are providing the best possible patient care in Australia.’
The RACGP will work closely with the Department of Health, and regional training organisations to ensure the AGPT selection process is comprehensive and, importantly, improves alignment and continuity between application and RACGP Fellowship.
Reprinted from Good Practice Issue 1–2, January–February 2017

6 Reprinted from Good Practice Issue 1–2, January–February 2017
RACGP RESOURCE
Imag
es N
ick
Zwar
, Dan
ielle
Maz
za
PAUL HAYES
Preventive activities
The RACGP’s Guidelines for preventive activities in general practice has been updated and is now in its 9th edition.
Research and high-quality evidence are essential to the effectiveness of many professions. In the case of healthcare, these areas can move at a rapid pace and it is vital that medical practitioners are able to keep pace with what is best for them and their patients.
The 9th edition of the RACGP’s Guidelines for preventive activities in general practice (Red Book), released in late 2016, ensures Australia’s GPs have access to preventive recommendations that are based on the most up-to-date evidence-based guidelines.
‘Evidence changes and new studies are published, new techniques come along,’ Prof Nick Zwar, GP and Chair of the Red Book editorial committee, told Good Practice. ‘We need to look at the evidence and update the guidelines so GPs are abreast of what is supported by the best evidence.’
The Red Book, which was first published in 1989 and last updated in 2012, is designed to provide GPs and practice teams with guidance on opportunistic and proactive preventive care. The publication features a total of 15 chapters, covering areas such as genetic counselling and testing, communicable diseases, prevention of chronic disease, screening tests of unproven benefit, and many more (refer to breakout on page 8 for full list of chapters).
‘Preventive activities are crucial for population health,’ Prof Zwar said. ‘And in general practice and primary care, we can do a lot to address many of the health issues that affect our society and the way that, for example, tobacco use and risky alcohol consumption, can make a big difference to people’s health and use of health services.
‘Prevention is so important and the Red Book is a crucial resource.’
The update processOnce the decision was made in 2015 to update the Red Book, the RACGP established an editorial committee. This was comprised of experienced GPs from all over Australia, plus a consumer representative. A principal GP was assigned to be in charge of the content in each chapter.
The first stage of the update was a consultation phase to seek feedback on the 8th edition of the Red Book, and to allow GPs and other stakeholders to provide suggestions for improvement and evidence for the 9th edition.
Members of the editorial committee, with support from RACGP staff members, conducted thorough reviews of relevant guidelines and evidence from all over the world.
The committee met monthly over a period of 15 months to discuss key issues and any contentious areas, and to review the evidence and debate draft content.
The next step was a second consultation phase with key internal and external stakeholders.
All consultation was followed by finalisation of content, an internal review and RACGP Council endorsement.
The 9th edition of the Red Book was then officially launched at the RACGP’s Annual Conference for General Practice – GP16 – in Perth in October 2016.
‘The update is a long development,’ Prof Zwar said.
‘The content leads for various chapters take leadership of looking at the evidence, synthesising it and developing new text for the updated edition.
‘It’s a rigorous process that looks at all of the evidence and a lot of expert opinion.’
Prof Nick Zwar believes the Red Book is a crucial resource in helping GPs provide vital preventive services.

7Reprinted from Good Practice Issue 1–2, January–February 2017
Additions and updatesThe Red Book is intended to help GPs offer the best preventive care to all patients who walk through their doors. However, delivering such care to different socioeconomic and cultural groups can be difficult.
‘[In the updated Red Book] we have rewritten how we deal with health and equity,’ Prof Zwar said. ‘Because one of the challenges for prevention and preventive activities is delivering them to people who are less advantaged – people on low incomes, people who live in rural areas of Australia, Aboriginal and Torres Strait Islander peoples, people who don’t speak English, etc.
‘The health inequity sections were rewritten to try to present a more structured guide as to what GPs and general practice staff members might be able to do to address inequity in regards to prevention.’
The updated section includes various suggestions for GPs, such as the use of motivational interviewing and counselling techniques, plain language and culturally appropriate written materials, using interpreter services, and more.
Screening for early detection of cancers is another important area in which information and evidence have evolved in recent years.
‘The cancer section of the Red Book has been quite comprehensively reviewed,’ Prof Zwar said. ‘There is a lot happening in terms of cancer screening, and a lot of new studies related to prostate cancer screening.
‘But it’s not just [related] to prostate cancer screening. It’s also cervical cancer and breast cancer screening, and the risks as well as benefits of screening programs.’
In the case of cervical cancer, the information contained in the updated Red Book is particularly important in light of coming changes
to the National Cervical Cancer Program. From 1 May, women aged 25 and older will have their two-yearly Pap smear replaced with a human papillomavirus (HPV) test/cervical screening test every five years.
‘Cervical cancer screening in Australia has been extremely successful … and GPs are integral to the program because we are the major Pap test providers in the country,’ Prof Danielle Mazza, GP and content lead for the Red Book’s cervical cancer and breast cancer screening sections, told Good Practice.
‘Women have become accustomed to the two-yearly Pap smear and that consultation, which is often an opportunity for GPs to talk about a large range of preventive healthcare issues.
‘GPs will be the key component of the implementation of this new National Cervical Cancer Program and the new edition of the Red Book provides information about transitioning for the [cervical cancer screening] changes.’
The Red Book also includes new information on balancing the benefits and potential risks of mammography when screening for breast cancer.
‘This edition of the Red Book highlights the move towards giving increased significance to the individual risk of the patient who is sitting in front of you, rather than just having a broader approach [to breast cancer screening],’ Prof Mazza said.
‘It refers to Cancer Australia’s tools that help to determine what degree of breast cancer risk a patient might have. We also refer to the availability of various new options for women who have a high level of risk. For example, chemoprevention, which is the taking of medication to try and reduce risk.
‘We recommend GPs consider those and other options for their patients.’ >>
The Red Book
First published in 1989, The RACGP’s Guidelines for preventive activities in general practice (Red Book) is designed to provide GPs and practice teams with guidance on opportunistic and proactive preventive care. It is widely accepted as the main guide to the provision of preventive care in Australian general practice.
The Red Book provides an entry point to common conditions in general practice, and offers practical advice on the screening and services that should be provided to the general population.
Visit www.racgp.org.au/redbook for more information and to access the Red Book, and RACGP.TV to view its launch at GP16.
Prof Danielle Mazza feels the Red Book is a ‘wonderful resource’ unlike anything else available in Australia.

8 Reprinted from Good Practice Issue 1–2, January–February 2017
Imag
e Jo
hn L
itt
RACGP RESOURCE
>> More evidence regarding screening for prostate cancer has also come to light. While the RACGP maintains that prostate-specific antigen (PSA) testing not be recommended for population screening, the new edition of the Red Book recommends using ‘decision support’ to keep patients more informed about the benefits and potential harms of PSA screening.
‘[The latest research] confirmed the evidence from previous editions of the Red Book; that there is not a clear benefit of prostate cancer screening in asymptomatic men,’ Prof Zwar said. ‘We have now provided information about new trials and about tools to assist the discussion with men as to whether they want to have prostate cancer screening.
‘So if a man chooses to go down that path, they do so in an informed way after an evidence-based discussion with their doctor.’
Genetic counselling and testing is another aspect of preventive health where research and evidence have developed.
Identifying patients who may be at risk of a genetic disorder requires a comprehensive family history, and the 9th edition of the Red Book recommends the use of a simple family-history screening questionnaire (FHSQ).
The FHSQ is designed to help identify whether certain patients require a more detailed assessment of family history of cancer, heart disease or diabetes.
GPs can use the FHSQ as part of the assessment when a patient first visits a practice. In the event patients are uncertain of their family history, GPs can ask them to discuss the FHSQ with their relatives prior to completing the questionnaire.
‘The FHSQ is helpful in that it saves GPs going straight to technological things like testing people’s blood to look at their genes, which may throw up a whole lot of things and may
be of little relevance, but may just cause worry for the patient,’
Prof Zwar said.
Chapter guide The Red Book’s 15 chapters cover practical advice across several areas of preventive care:1. Preventive activities prior to
pregnancy2. Genetic counselling and testing3. Preventive activities in children
and young people4. Preventive activities in middle age5. Preventive activities in older age6. Communicable diseases7. Prevention of chronic disease8. Prevention of vascular and
metabolic disease9. Early detection of cancers10. Psychosocial11. Oral health12. Glaucoma13. Urinary incontinence14. Osteoporosis15. Screening tests of
unproven benefit Visit www.racgp.org.au/redbook for more information.
The unknownGiven one of the most important aspects of preventive medicine is knowing what not to do, it makes sense that the ‘Screening tests of unproven benefit’ chapter has expanded further in the updated edition of the Red Book.
‘Just because you can, doesn’t mean you should,’ Prof Zwar said.
What originally began as a relatively small section of the 5th edition of the Red Book (2003) now includes two very detailed tables: ‘Screening tests not recommended in low-risk general practice populations’ and ‘Screening tests of indeterminate value’.
According to Assoc Prof John Litt, content lead and original driving force for the chapter, the latest edition helps to provide more context as to why these tests may not necessarily be recommended.
‘We went through all of the current professional guidelines. When they all agreed that made it really easy and there wasn’t much to talk about,’ he told Good Practice.
‘Where there was mixed or variable quality of evidence, where one country is saying “you ought to be screening for this” and another country is saying “don’t do it”, then that leads to inconsistency and leaves GPs with different views.
‘We have tried to provide a little bit more of a discussion and the reasoning behind
recommendations when the evidence is weak, inconsistent or even lacking.’
Assoc Prof Litt believes that, in addition to the potential financial cost of tests of limited or no benefit, individual patients may experience needless concern in the face of what can appear to be a serious medical issue.
‘Every time we investigate a perceived problem or provide a diagnosis we give patients a medical label, which can have adverse consequences. These include anxiety and unnecessary investigations that may cause harm and uncertainty,’ he said.
‘For example, a lot of people with an abnormal PSA may worry about what it means even though, for many, the results may not progress. When the results do progress, you may end up treating with further investigations and interventions that can potentially cause harm. This is especially problematic if the person does not have an aggressive prostate cancer.
‘The instigation of unnecessary or poor screening tests commits the doctor to a series of subsequent investigations and treatments that put the patient at risk of significant harms.’
Valued sourceWidely accepted as the main guide to preventive care in Australian general practice, the Red Book continues to play a key role in the everyday practice of GPs throughout the country. Its function in supporting evidence-based preventive activities means its updates must be of the highest quality.
‘The Red Book has developed a certain status because people have learnt they can trust it,’ Prof Zwar said. ‘We have tried to keep it brief enough that it’s useful in day-to-day practice and I think it’s a vital publication.’
Prof Mazza described the Red Book as a ‘wonderful resource’ because it does what many other guidelines do not in that it offers patient-centred information.
‘It enables GPs to access information in a comprehensive way for the patient in front of them,’ she said. ‘The Red Book helps patients to understand prevention across reproductive health, cancer, dermatology, mental health and many other aspects of healthcare. It explains the risks and what the GP’s approach should be to address the risks and take a preventive approach.
‘The Red Book is a comprehensive document unlike anything else that’s available in Australia, and that’s what makes it the gold standard for prevention and preventive care in this country.’
Assoc Prof John Litt was content lead for the ‘Screening tests of unproven benefit’ chapter.


10 Reprinted from Good Practice Issue 1–2, January–February 2017
YOUTH MENTAL HEALTH
AMANDA LYONS
GPs are crucial to achieving better
outcomes in youth mental health
throughout rural Australia.
Dr Claudio Villella believes it is important to help young people feel welcome when they present to a GP with issues of mental health.
Dr Mary Emeleus has found involving young people in the decision-making process is vital when providing mental health services. Im
ages
iSto
ck; M
ary
Em
eleu
s; C
laud
io V
illella
and getting older,’ he told Good Practice. ‘But we don’t necessarily have services available to our rural youth that people in metropolitan areas would.’
Dr Nott has found that youth in rural areas can also face a number of pressures that are not routinely encountered by those in urban areas.
‘If you look at farming communities, there are stresses from environmental challenges – droughts, flooding, etc – with people losing huge amounts of their cropping, their potential income, for the year,’ he said.
The Australian youth development index 2016 report contained positive news on the nation’s youth, finding improvement in youth development index (YDI) scores – which measure overall levels of education, health and wellbeing, employment and opportunity, political participation and civic participation for young people – for almost all states and territories since 2006.1
However, the report also revealed that YDI health and wellbeing scores have deteriorated, with significant development gaps between Australia’s rural and urban youth.1
The National Rural Health Alliance (NRHA) has identified a comparative lack of access to mental health services, combined with a lower likelihood to seek help, as factors in higher rates of mental health issues in rural and remote areas. These issues include a higher suicide rate among young men and Aboriginal and Torres Strait Islander peoples.2
Dr Shannon Nott, a general practice registrar and former finalist for New South Wales (NSW) Young Australian of the Year, is not surprised by these findings.
‘There are the same issues [for urban and rural youth] surrounding transition in life and personal identity that come with growing up
‘Farms are mostly family-run businesses and I think the stresses parents feel from the loss of a crop, for example, will certainly be felt by the children as well.
‘Being able to provide young people capacity or ability to deal with those issues is key to addressing some of the mental health issues we see in rural Australia.’
Dr Mary Emeleus, GP and psychotherapist who works with young people in Townsville in north-eastern Queensland, emphasised that the GP’s role can be vital in this context.
‘In many small places, the GP is the primary place to go if young people do seek help,’ she told Good Practice.
Dr Claudio Villella, GP advisor for the national youth mental health foundation, headspace, believes this makes GPs particularly well placed to help young people in rural areas with issues of mental health.
‘Close to one in four young people will experience a mental health disorder, and three out of four of those people won’t seek help,’3
he told Good Practice. ‘But we know that those young people
are often seeing GPs, so GPs are a really good inroad into providing an opportunity for them to open up about the problems they’re experiencing.’
Mind the gap

11Reprinted from Good Practice Issue 1–2, January–February 2017
Training‘Cognitive behavioural therapy skills for general practice’ is an online mental health training option for RACGP members developed by RACGP Rural and gplearning.
The training provides GPs with foundational cognitive behavioural therapy (CBT) skills. While aimed at rural GPs, the course will be a useful resource for any GP interested in gaining skills in psychotherapy. Contact RACGP Rural on [email protected] for more information.
Building relationshipsAs the most likely source of assistance for young people in rural areas, how can GPs best help this patient population? Dr Villella believes making young people feel welcome is the first thing GPs should consider.
‘Engagement is really the first port of call,’ he said. ‘Making practices youth-friendly and having materials in waiting rooms that specifically engage young people, so that when a young person is sitting in a waiting room they can see themselves in some of the material that’s presented.’
Dr Villella also emphasised the importance of building a strong therapeutic relationship with younger patients.
‘If young people establish a relationship with a GP who they can see is going to give them time and support them, then they’re more likely to back to that GP if there’s any subsequent issues,’ he said.
Part of establishing this relationship involves explaining confidentiality, which is identified by many young people as a key barrier to accessing help for mental health issues, especially in small rural communities.
‘They might be nervous about discussing their concerns with the same GP that other family members, especially parents, are seeing,’ Dr Villella said.
Dr Villella has a number of recommendations when discussing confidentiality with young people who present with mental health issues.
‘If they present with a parent, it is important to say you would really like to spend some time alone with the young person, and explain
the limits of confidentiality while both are present,’ he said. ‘That way the parent can understand that if there is something serious going on they will find out about it.
‘In the more common scenario where you have, say, a 15-year-old who presents without a family member or parent, it’s really important to be clear about the limits of confidentiality. That is the first thing you should discuss with them.
‘You are setting the scene and if at some point you feel compelled to engage a family member or friend or carer, then you have provided the explanation up front.’
Dr Emeleus has found it is rare that family should be excluded from a young person’s care. Even in such cases, however, she believes it is vital to acknowledge the family’s role in the young patient’s life.
‘It’s important to keep them in mind even if you can’t practically involve them in consultations or the care plan,’ she said.
Taking time for relationship-building can present something of a difficult issue for time-pressured GPs, particularly in rural and remote areas. But, in Dr Emeleus’ experience, it can make a world of difference with younger patients.
‘We need to remember that some young people come from quite chaotic, disadvantaged or dysfunctional circumstances and may not actually have any other reliable, safe adults in their life who they can run things past,’ she said. ‘Doctors sometimes find themselves in that role, and I think we need not feel bad about that.
‘I think that can be a very important role.’ >>

12
Imag
e R
icha
rd D
unw
oody
YOUTH MENTAL HEALTH
Reprinted from Good Practice Issue 1–2, January–February 2017
e-Mental health resources for GPs• RACGP – e-Mental health: A guide for GPs
(www.racgp.org.au/your-practice/guidelines/e-mental-health) • headspace – Resources for health professionals working with young people
(https://headspace.org.au/health-professionals) • Black Dog Institute – Access a variety of online training for GPs in e-mental
health (www.blackdoginstitute.org.au/healthprofessionals/gps/emhprac.cfm)
Treating young peopleOnce a younger patient has disclosed mental health issues, it is important for GPs to keep in mind that they may need a different treatment approach than an adult would require.4 According to Dr Emeleus, this is partly related to the young person’s biology.
‘[A young person’s] brain is still developing and their social development still needs to occur,’ she said. ‘You need to consider what would normally be expected for somebody of this age and what developmental tasks should be happening.’
Dr Emeleus has also found that treatment of young people is more effective if they are engaged and included in the decision-making process.
‘Young people have told me [they value] the feeling of being respected and making collaborative decisions, so that the doctor educates them and provides advice,’ she said.
‘And then you work out the plan together, rather than them being told what to do.’
This shared planning includes decisions about prescribing selective serotonin reuptake inhibitors (SSRIs), or antidepressants, a treatment option that Dr Villella has found often doesn’t appeal to these patients.
‘Young people often really don’t want to be on medication,’ he said. ‘So if they are prescribed medication without having been engaged around their values in terms of the treatment, then that will disengage them.
‘It’s really important that GPs take a shared-decision approach.’
Medication is also less likely to be a definitively appropriate treatment path for younger patients.
‘The evidence for SSRIs in young people is not as strong as it is for adults,’ Dr Villella said.
‘Also, young people present some risks. If SSRIs are not taken regularly, with a very high level of compliance, they can actually make people feel worse. And young people can be not as compliant [as adults] when taking medication.’
For these reasons, a ‘stepped’ approach has been found to be effective when treating young people for mental health issues, with an emphasis on attempting psychological treatments before prescribing. e-Mental health services can also be especially helpful in a rural setting.
‘We need to be skilful in non-drug options,’ Dr Emeleus said. ‘This includes psychological interventions, knowing about e-mental health, and also how to help young people negotiate the social aspects of their world, which is where the family and carer inclusion comes in.’
Raising awarenessIn August 2016, Dr Nott jumped at a rather unique opportunity to increase awareness of the issue of youth mental health when he participated in the infamous Mongol Derby.
The Guinness World Record holder for the world’s longest and toughest horse race, the Mongol Derby is designed to replicate Genghis Khan’s postal route system during the height of his 13th-century empire, with a course that extends more than 1000 km across the Mongolian Steppe.
Participating in the race also offered Dr Nott the chance to raise funds for batyr, a NSW-based organisation that runs mental health education programs for students in schools and universities.
The Mongol Derby incorporates 25 horse stations, or rest stops, across its length. Riders can end each day in one of these stations, or ride further on and stay with a local family on the vast Mongolian landscape.
Given its stringent conditions, Dr Nott feels fortunate to have been included in the 2016 line-up for the race.
‘They only accepted 44 riders from around the world to race,’ he said.
‘Some of the people that raced with me are incredible horse-people – professional dressage riders, professional jockeys and people who have been their country’s endurance horse-riding champions.
‘So it was quite an honour to be able to race alongside these people in Mongolia.’
Dr Nott was also very pleased to have been able to raise money for an organisation like batyr and help in what is an extremely important area of Australian healthcare.
‘I was lucky to be able to raise over $5000 in total, but I’m also continuing to raise more money,’ Dr Nott said.
‘Hopefully I’ll be able to get more money in the future for batyr and will work with them into 2017 to look at how can we utilise some of those funds to provide some mental wellbeing and education programs for young people.’
References1. Australian Youth Development Technical Advisory
Committee. Australian youth development index: 2016 report. Woolloomooloo, NSW: Youth Action New South Wales, 2016. Available at www.youthaction.org.au/australian_ydi [accessed 28 November 2016].
2. The National Rural Health Alliance. Mental health in rural and remote Australia, fact sheet October 2016. Canberra, ACT: NRHA, 2016. Available at http://ruralhealth.org.au/sites/default/files/publications/fact-sheet-mental-health-2016.pdf [Accessed 28 November 2016].
3. headspace. Position Paper – Young people’s mental health. North Melbourne, Vic: headspace, 2011. Available at www.headspace.org.au/assets/Uploads/Corporate/Young-Peoples-Mental-Health.pdf [Accessed 28 November 2016].
4. James AM. Principles of youth participation in mental health services. Med J Aust 2007;187(7):57.
Dr Shannon Nott helped raise awareness of – and funds for – youth mental health when he participated in the 2016 Mongol Derby horse race.


14 Reprinted from Good Practice Issue 1–2, January–February 2017
Imag
es K
en W
angu
hu; R
AC
GP
; iS
tock
The RACGP’s Fellowship in Advanced Rural General Practice offers GPs in rural and remote Australia the opportunity to reflect on their abilities and develop
further skills to help their communities.
‘If you’ve seen one country town, you’ve seen one country town’
Context matters regardless of where a GP plies his or her healthcare trade. One practice will never be exactly the same as another.
In the case of GPs who work in rural and remote Australia, the scope of patient populations often takes in entire communities and the differences between locations can be stark.
Rural GPs thus require advanced abilities that can easily be adapted to different settings.
‘Rural general practice has its differences – not good or bad – from other general practice for which you need a certain level of skill,’ Dr Ken Wanguhu, an experienced rural GP, told Good Practice. ‘As you grow in rural general practice you get to appreciate just how much
the community that you are working in actually shapes your practice.
‘I you go into a small community and they need obstetric services, for example, then that sort of procedural stuff is important as a GP. Or if it’s an older population, then skills in internal medicine, geriatrics, palliative care, etc become a really big part of it.’
The RACGP’s Fellowship in Advanced Rural General Practice (FARGP) qualification, which is available to general practice registrars as well as experienced GPs, aims to develop advanced rural skills and increase options for safe, accessible and comprehensive care in rural, remote and very remote communities throughout Australia.
‘If you want to work in rural and remote areas and have that credibility as a GP, then you need to show a lifelong commitment to enhancing your skills and your qualifications.
The FARGP is a great way to do that,’ Assoc Prof Brad Murphy, an experienced rural GP who recently completed the FARGP, told Good Practice.
‘The wonderful thing about the FARGP is that it has so many opportunities – you’re not necessarily committed to obstetrics, anaesthetics, surgery, or anything else. There is acknowledgement that there is a whole range of other areas of special interest.
‘The FARGP identifies that and gives you an opportunity to be formally recognised for your expertise and qualifications.’
Never stop learningMany practising GPs undertake the FARGP throughout their careers, and Assoc Prof Murphy and Dr Wanguhu represent a significant level of experience in a wide range of areas within general practice.
Advancing rural skills
RURAL HEALTHCARE
PAUL HAYES

15Reprinted from Good Practice Issue 1–2, January–February 2017
Assoc Prof Murphy, a long-time GP throughout Queensland, has held roles such as Chair of RACGP Aboriginal and Torres Strait Islander Health and Services Director – Clinical/Medical at the Indigenous Wellbeing Centre in Bundaberg. He is also on the RACGP Council and a founding member of the Jimmy Little Foundation.
Dr Wanguhu, who was born in Kenya and worked as a doctor in Kenya, Somalia and South Africa before coming to Australia in 2001, has practised in the South Australian Riverland town of Waikerie for more than a decade. He is also RACGP Rural Censor and received the faculty’s Brian Williams Award in 2015.
Regardless of their experience, both doctors are aware of the value in continuing their learning. One of the most valuable opportunities the FARGP offers experienced GPs is the chance to take a closer look at their careers and, as such, their abilities.
‘It’s nice to step back on reflect on your skills,’ Dr Wanguhu, who recently completed the FARGP, said. ‘That is what the FARGP gives you a chance to do; to reflect and ask, “What else do I need? What else does my community need?”
Dr Ken Wanguhu appreciates the recognition of a rural-specific qualification such as the FARGP.
‘The FARGP then gives you an opportunity to address any of the areas that you identify.’
Given their extensive backgrounds in general practice, Assoc Prof Murphy and Dr Wanguhu were eligible for the FARGP’s recognition of prior learning (RPL). This pathway recognises the experience, skills and qualifications of experienced rural GPs, offering the opportunity to submit evidence that demonstrates how they meet the specific criteria of the FARGP.
The FARGP gives you a chance to reflect and ask, "What else does my community need?"
‘Even with the RPL process, there is still a chance to reflect,’ Assoc Murphy said. ‘I found that really useful because I had to go back through a whole lot of stuff that I had done in the past in order to be able to justify to those who were doing the assessment that I had actually met the necessary criteria. >>
The FARGP allowed Assoc Prof Brad Murphy to reflect on his non-clinical skills.

16
RURAL HEALTHCARE
Reprinted from Good Practice Issue 1–2, January–February 2017
Fellowship of Advanced Rural General Practice
The RACGP’s Fellowship in Advanced Rural General Practice (FARGP) has pathways designed for general practice registrars and experienced GPs. The FARGP aims to develop advanced rural skills and broaden options for safe, accessible and comprehensive care for Australia’s rural, remote and very remote communities.
The FARGP is completed on an interactive learning program that is delivered via the RACGP’s gplearning education platform. The FARGP online learning platform allows registrars and practising GPs to access course materials, upload certificates and other relevant documents, receive ongoing feedback from their medical educator or mentor and submit work for assessment.
The FARGP qualification is awarded in addition to vocational Fellowship (FRACGP) and cannot be undertaken as a stand-alone qualification.
Visit www.racgp.org.au/education/fellowship/ruraladvantage or email [email protected] for more information.
>> ‘It was a useful journey for me to have a look at the things I had completed, both in my medical career at the coalface and in terms of what I had been involved in at a national level. For example, setting up RACGP Aboriginal and Torres Strait Islander Health.
‘That journey can blur over time … so the FARGP gave me a chance to reflect upon that and what I have been able to achieve.’
Advancing skillsWhen Dr Wanguhu took a step back and looked at his existing practice and abilities, he was struck by a specific area in which he had definite room for improvement.
‘I found there was one thing I hadn’t done much in my community … and that was men’s health,’ he said. ‘And rural men often have bad health – they smoke, they have a high suicide rate. They don’t do as much with their health.
‘I thought we were doing better, but when a patient pointed it out I realised it was perfect for me within the FARGP.
‘I was able to develop a learning plan and do some education. From that I developed a series of talks for men in my community.’
The FARGP provided Assoc Prof Murphy the chance to examine his abilities in Aboriginal and Torres Strait Islander health – a prominent area of his career – and develop more advanced non-clinical skills.
‘I think it’s an understanding of some of the differences that can often be associated with Aboriginal and Torres Strait Islander health,’ he said. ‘The interpersonal skills, the relationships you have with the patient and the wider family and community are often so important.
‘Aboriginal and Torres Strait Islander people – as a gross generalisation – tend to be very family-oriented, so it’s really important to collaborate with communities, and with individuals and families in order to get the right outcomes.
‘Because if you have the relationship with the community then the person with the problem, who you may never see because they would never walk through your door, will be brought to you by the community if they know you are trustworthy, reliable and competent.
‘That is just imperative, otherwise these people won’t even come to you. They will stay away and suffer in silence.
‘Understanding the resources that are available to you [is also vital]. Being up to date with what’s available and collaborating with the RACGP, being involved in the [Aboriginal and Torres Strait Islander Health] faculty and those sorts of things so that you get that information on a regular basis can be really important.’
Confident in practiceWhile the ability for individuals to independently provide competent primary healthcare lies as the foundation of high-quality general practice, a greater level of isolation means that independence is inevitably heightened for GPs in rural and remote areas of Australia.
‘[Rural healthcare] uses all of the skills you get as an urban GP, but it is quite challenging because the referral opportunities you have in the more urban areas aren’t always available to you,’ Assoc Prof Murphy said.
‘You are much more reliant on the use of technology, such as emails, photos, the internet and the phone. But you really need to develop the confidence to be able to practise in those areas.
‘You also need to acknowledge your own skills and be comfortable with your own skills so you can practise [remote medicine] with some confidence. It takes a lot of confidence to be able to look after someone with major chest trauma from a road accident at two o’clock in the morning when you only do it once every two years.
‘That is a different sort of medicine. The journey you undertake through the FARGP … is about acknowledging those differences and that we can always work towards improving and enhancing. That we maintain that qualification, that skill, to be the very best for the patients we look after.’
Following his many years in rural general practice, both with patients and other healthcare professionals, Dr Wanguhu appreciates the fact the FARGP offers a certain level of appreciation for the work that is required.
‘We know so much and we are so experienced at general practice that we can be on auto-pilot. We are unconsciously competent: we don’t think, we just do,’ he said. ‘We work in rural general practice
but don’t always get that recognition, so it’s actually nice to have a qualification that recognises what you have done for your community and what you do every day.’
Regardless of their considerable service to rural general practice, each GP found undertaking the FARGP to be an especially beneficial journey, both for their own practice and in terms of what they can pass on to other GPs and registrars.
‘It’s certainly an advertisement to registrars who might want to go and undertake their training,’ Assoc Prof Murphy said. ‘They can say, “This guy has obviously ticked the boxes and sees this journey as being important enough for him”.’

17Reprinted from Good Practice Issue 1–2, January–February 2017
ETHICS IN GENERAL PRACTICE
SARA BIRD
Drugs of dependence
Legislation and regulation.
In his weekly address on 14 May 2016, Barack Obama said, ‘Addiction doesn’t always start in some dark alley. It often starts in the medicine cabinet’.
Harm related to the use of opioid therapy has emerged as a major threat to public health in the US and there is growing evidence of harm caused by prescribed drugs of dependence in Australia. Not only are there risks to the health of patients and the community, but there can also be significant medico-legal consequences for GPs who do not comply with the law when prescribing drugs of dependence.
This column focuses on the state-based legislative requirements for prescribing Schedule 8 drugs, such as alprazolam, opiates and amphetamines.
The prescription of Schedule 8 drugs throughout Australia is closely regulated due to the risk of addiction, and the prevalence of misuse and trafficking of these medications.
Before prescribing a drug of dependence, a GP must take all reasonable steps to ensure a therapeutic need exists. Once a therapeutic need is established, GPs are required to comply with state-specific legislation and, where necessary, obtain an authority/permit/approval from the relevant health department unit before writing a prescription for these medications.
It is important for GPs to be aware that the legislative requirements for prescribing Schedule 8 drugs are different for drug-dependent patients and non-drug-dependent patients.
Drug-dependent patientsThe legal definition of a drug-dependent person varies in each state and territory. In general terms, a drug-dependent person is someone who, as a result of the repeated consumption of a drug of addiction/
dependence, acquires an overpowering desire for the continued consumption of such a drug, and is likely to suffer mental or physical distress upon ceasing the drug.
In all states and territories, it is a mandatory requirement for GPs to seek an authority/permit/approval from the appropriate health department unit to prescribe a Schedule 8 drug to a drug-dependent person. These health department units include: • Pharmaceutical Services (ACT, NSW,
WA and Tasmania)• Drugs of Dependence Unit (SA) • Medicines and Poisons Control (NT)• Medicines Regulation and Quality
(Queensland)• Drugs and Poisons Regulation (Victoria).The health department unit authority/permit/approval is required regardless of whether the prescription is written on the Pharmaceutical Benefits Scheme (PBS), and this process is quite distinct from (and in addition to) any authority to prescribe under the PBS.
The Pharmaceutical Services Branches in Tasmania and WA also require GPs to provide consultant support with an application for the proposed treatment of a drug-dependent person with Schedule 8 drugs.
Non-drug-dependent patients If the patient is not drug-dependent, there are strict limits on the length of time that drugs of dependence can be prescribed before an authority/permit/approval is required.
In general terms, GPs prescribing Schedule 8 drugs and other restricted drugs of dependence for more than two months will need to obtain approval from the relevant health department unit. In most states and territories, the two-month period includes prior treatment by other prescribers.
Of note, in NSW an authority is required for only a very limited list of Schedule 8 drugs, including alprazolam, but not for commonly prescribed oral opiates such as oxycodone. In other states and territories, most Schedule 8 drugs are included and, in some states, benzodiazepines are also included in the restricted drugs for which an authority/permit/approval is required.
GPs should familiarise themselves with the specified drugs in their jurisdiction. Up-to-date information is available on the website of the relevant health department unit.1
Recognising and managing inappropriate requests for drugs of dependenceIdentifying drug-dependent patients is not always straightforward. Dependency on Schedule 8 drugs can occur at any age and across all socioeconomic groups and professions. Some patients may exhibit drug-seeking behaviours, but this is not invariable.
Useful tools to assist in identifying drug-dependent patients include the Prescription Shopping Information Service and real-time prescription monitoring. The latter is currently only available in Tasmania, although there are plans to introduce it in other states and territories.
GPs will benefit from developing strategies to manage patients’ inappropriate requests for drugs of dependence. Having some verbal scripts can be useful. For example:• ‘We don’t prescribe this medication. Let’s
talk about how I can help you with your pain problems.’
• ‘Under the state law, it is illegal for me to prescribe those medications to you.’
• ‘The level of care you need is not within my expertise. I am happy to refer you to our local drug and alcohol service to ensure you get the care you need and there is no long-term harm to your health.’2
References 1. The Royal Australian College of General Practitioners.
Prescribing Drugs of Dependence in General Practice, Part A. East Melbourne, Vic: RACGP, 2015. Available at www.racgp.org.au/your-practice/guidelines/drugs-of-dependence-a/appendix-c-state-and-territory-legislation- and-contacts/c2-stateterritory-contacts [Accessed 30 November 2016].
2. Royal Australian College of General Practitioners. Prescribing Drugs of Dependence in General Practice, Part B. East Melbourne, Vic: RACGP, 2015. Available at www.racgp.org.au/your-practice/guidelines/drugs-of-dependence-b/resource-a-examples-of-responses-to-patient-requests-for-benzodiazepines/resource-a-examples-of-responses-to-patient-requests-for-benzodiazepines [Accessed 30 November 2016].
This article is provided by MDA National. They recommend that you contact your indemnity provider if you need specific advice in relation to your insurance policy.

18 Reprinted from Good Practice Issue 1–2, January–February 2017
DATA BACKUP
Imag
es iS
tock
; Oliv
er F
rank
, Chr
is H
ogan
; Chr
is M
itche
ll
Implementing an effective system for data backup and recovery is an essential preventive activity for the health of a general practice.
Information lockdown
AMANDA LYONS
It is no exaggeration to say that data is the lifeblood of the modern general practice.
‘If there’s any interruption to the medical record, it can be financially, medically, professionally and personally devastating,’ Assoc Prof Chris Hogan, GP and Associate Professor of General Practice at the University of Melbourne, told Good Practice.
The importance of data itself is not new; patient information has always been vital to the running of a practice. As technology has developed, however, so have methods of data storage, creating new efficiencies and possibilities – and vulnerabilities.
Dr Chris Mitchell, GP and member of the RACGP Expert Committee – eHealth and Practice Systems (REC–eHPS) and the General Practice Data Governance Council, learnt the consequences of these vulnerabilities the hard way.
‘My first experience of data loss was right in the beginning of my career,’ he told Good Practice. ‘[Our practice] had a computer that wasn’t connected to the internet, so I thought, “Oh well, we won’t need any anti-viral protection”.
‘Then one of the administrative staff brought in something to look at on the computer – this was in the days of floppy discs. Everything crashed and was unrestorable. Since then, I’ve learnt my lesson.’
Digital benefitsThe advent of digital data has brought with it clear advantages, including the fact this type of storage is more robust and less likely to be misplaced than paper records.
‘Anybody who has used paper systems would know that they are not that reliable,’ Dr Mitchell said. ‘They get taken out on a home visit and never come back. They get misfiled and are never found.’
Paper also has obvious vulnerability to disasters such as fire or flood, with little recourse in the event it is lost.
‘Paper records are not backed up. If the practice burns down, or even if one patient’s paper record is misplaced, it’s gone forever,’ Dr Oliver Frank, GP, member of the REC–eHPS and University Senior Research Fellow at the University of Adelaide, told Good Practice.
But while digital data offers many advantages, it is not infallible.
‘There are only two kinds of computer users: those who have lost data and those who are going to lose data,’ Dr Frank said, quoting a general practice colleague.
Digital data can be threatened by the same naturally occurring scourges as its paper counterpart, but its very medium exposes it to new types of threats.
‘You need to consider how you’re going to manage fire and floods, but also how you’re going to manage prolonged power outages,’ Dr Mitchell said. ‘At one point in the past, our practice lost power for three days when there was a terrible accident that took out basically all of the electricity coming into our rural town.
‘We were very fortunate that we had a generator that we could pull out, but even so it’s a challenge.
‘We have since had to make changes to the way we operate with the generator going. For example, we can’t use our laser printers because the laser drags too much power. We have got to have some inkjet printers in the practice.’

19Reprinted from Good Practice Issue 1–2, January–February 2017
From top: Assoc Prof Chris Hogan, Dr Oliver Frank and Dr Chris Mitchell all believe high-quality data backup systems in general practice are worth the financial investment.
There are also the modern digital problems of computer hacking and the introduction of malware, such as viruses and worms.
‘Before, we had to worry about mischance and misadventure, but now we also have to worry about mischief and mayhem,’ Assoc Prof Hogan said.
There can be various motivations behind attacks on software and systems. For example, practices can be faced with ‘ransomware’, where a computer system is essentially blocked and won’t be restored until a sum of money is paid to those who implemented the software. The desirability of medical data on the internet’s black market is another security issue.
‘Medical data has a high level of value among hackers because it contains sufficient demographic details to enable identity fraud,’ Assoc Prof Hogan said.
Protecting patient data is a fundamental issue of patient and practice safety.
‘Data security is key,’ Dr Mitchell said. ‘It’s really important that that information is maintained securely; for the reputation of your practice and for the protection of your patients’ personal health information.’
Although ensuring data backup and security comes with a financial price tag, Dr Frank cautioned that not doing so carries a much more significant expense.
‘To some extent, it’s a question of cost versus how much data you’re prepared to lose,’ he said. ‘The more you spend, the more likely you’ll lose less data and be able to recover your data sooner and more easily. So there is a balance in that.’
Tricks and trapsWhile the technology involved can be complex, the ultimate goal of data backup systems is fairly straightforward.
‘The aim is to have all the information available at any time you might need it, and to be able to restore it quickly and efficiently,’ Dr Frank said.
There is a range of methods and systems available and a practice needs to decide what is best for its needs (refer to breakout on page 20 for more information). According to Assoc Prof Hogan, however, there is one consideration that should be common to all practices: the need for offsite storage in order to be prepared for several disaster-type scenarios. >>

20 Reprinted from Good Practice Issue 1–2, January–February 2017
RACGP resource
The RACGP released its Guide to information backup in general practice in 2016. The document is designed to assist general practices in selecting and implementing secure and reliable information backup and data recovery processes.
The guide provides details of backup procedures, case studies and checklists, and should be used in conjunction with advice from an IT professional.
Visit www.racgp.org.au/your-practice/ehealth/protecting-information/guide-to-information-backup-in-general-practice to access Guide to information backup in general practice.
DATA BACKUP
>> ‘First of all, [be prepared for] the destruction of your general system. For example, your office burning down,’ he said. ‘The next thing is when there has been an incident whereby the whole building is inaccessible, usually due to extensive flooding.’
There are many types of backup, including local, in which practices back up data to a physical storage device onsite or at a nearby location. There are also options in which data is stored offsite, either physically or online. Finally, there is the option of storing data in the ‘cloud’.1
Each of these options contains its own benefits and drawbacks: physical onsite storage remains vulnerable to theft and natural disaster, online storage is dependent on internet access,1 and use of third-party storage companies can expose practices to external risk.
‘It’s tempting to think that one could outsource all of this and let someone else manage the data,’ Dr Frank said. ‘But then you’re very dependent on the organisation maintaining it. Even if they are doing the right thing but then go out of business, there’s potentially a problem.
‘And, of course, there are questions about the data being hosted in Australia, and even about your connection to where your backup is working.
‘There’s quite a few steps along the way.’Once the practice backup system has been
selected and implemented, it is important to ensure it is operating as it should.
‘The area where I see practices getting into strife is thinking that they’ve got an automated backup process when they don’t,’ Dr Mitchell said. ‘They’ve set up, or their IT [information technology] manager has set up, a process of automated backups that has fallen over for whatever reason, and nobody knows that it’s fallen over.
‘The other problem I often see is backups occurring, but the data is not readable. The key is to ensure that backups are occurring every day, at least, and that they are checked and you can restore from them.’
There are also more technological concerns to consider, such as compatibility between systems.
‘When your system goes down, how do you collect the information?’ Assoc Prof
Hogan said. ‘It needs to have a computer that’s compatible with the data-retrieval system. The technology you use has to be robust and able to do the job that you are asking it to do. For instance, USB sticks are useful for intermittent backup, but not for doing it regularly.
‘The other thing is that once you’ve got your backup system, the computer you are using must be able to read and cope with the backup and not corrupt the data.
‘And when you are using the system away from the practice, you need to make sure that the information you collect can be integrated back into your main system.
‘We have had issues after a bushfire where people collect all of the data and then realise they have to manually re-enter it because they’ve used a manual system.’
System educationIt is not just data backup technology that requires attention, but also the people who are using it.
‘Even with the best IT system in the world, people have to be aware of the risks,’ Dr Mitchell said. ‘So it’s not just about investment in infrastructure, but also about investment in training.’
Effective training is vital to ensure that practice staff members understand the correct procedures to safeguard the security of their IT system.
‘A chain is only as strong as its weakest link, and the person who has the passwords on sticky notes on their computer isn’t what you would call the strongest link,’ Assoc Prof Hogan said.
In addition to day-to-day use, it is also important to have dedicated staff members who have detailed background knowledge of the practice system.
‘You’ve got to have at least one person, ideally two people, who understand the backup process and who are involved with checking it over,’ Dr Mitchell said. ‘Because it isn’t just IT systems that fall over, [human] systems fall over as well, and it’s pretty awkward if the only person who knows how that system works leaves the practice for sickness or any other reason.
‘So you’ve really got to have some allowance for redundancy in terms of your staff knowledge of the system.’
Given the technical knowledge needed to understand and run these systems is so specialised, it is also important for GPs seek professional assistance and advice.
‘GPs are not computer technicians,’ Dr Frank said. ‘Some of us have a bit of an interest in these things, but even then it’s probably dangerous to think we can actually manage it ourselves. It’s too technical.’
Assoc Prof Hogan emphasised that it is important to expect the unexpected when it comes to system failure.
‘We always used to say that we believe in Mrs Murphy’s law: that Mr Murphy was an optimist, because even things that couldn’t go wrong, would go wrong,’ he said.
With this principle in mind, Dr Mitchell recommends ensuring a practice has a comprehensive system manual on the premises.
‘Unfortunately, disaster won’t always strike when your most senior practice manager is available, or when the person with the IT responsibilities is there,’ he said. ‘So you need to make sure that your training and manuals are sufficient for people to understand what they need to do.
‘That first step might be calling in your practice manager. But often there are steps that can be taken and [in our practice] we’ve tried to outline those in the manual to show exactly what to do.’
References1. The Royal Australian College of General Practitioners.
Guide to information backup in general practice. East Melbourne, Vic: RACGP, 2016.


22 Reprinted from Good Practice Issue 1–2, January–February 2017
Patient connections
Imag
es R
AC
GP
GP PROFILE
AMANDA LYONS
Dr Wence Vahala continues a family legacy of dedication to general practice.
Western Australian GP Dr Wence Vahala belongs to a family with a strong tradition in medicine in Perth, with his father having practised as a GP in the suburb of Bayswater from the 1950s.
Prior to Bayswater, however, the Vahala legacy began in Europe. The family fled political turmoil in what was then Czechoslovakia in the middle of the 20th century, driving across the border to live as refugees in Germany for a year before being accepted into the UK. On their arrival, Dr Vahala Sr had to undergo a rigorous process in order to be recognised as a doctor in his new country.
‘Dad had to study fourth-, fifth- and sixth-year exams, but not at university – he did it from home with books,’ Dr Vahala said. ‘Then he had to sit the exams before he could be recognised as a doctor, and after that he worked for a couple of years in hospitals in the UK.
‘One of the registrars he worked with in Guildford, near London, was an Australian surgeon and he recommended Dad be a GP in Perth.
‘So that’s how we got to Perth and to Bayswater. That was 1956, so I was not yet 13 years old when we got here.’
It wasn’t long after the family’s arrival in Australia that Dr Vahala began his own medical training, starting his degree at the University of Western Australia at the age of 16.
‘In the transition from school in the UK to Australia, Mum was keen for me to be stretched academically,’ he said.
Following graduation at the age of 22, Dr Vahala entered hospital training as a registrar at Fremantle Hospital, but left halfway through his second year to assist his father at his single-GP practice in Bayswater.
‘Dad was getting fatigued and it wasn’t easy to get locums or partners in those days,’ Dr Vahala said.
Dr Vahala found that once he began working in general practice, he didn’t want to leave, and he credits his father for his subsequent career as a GP.
‘Dad somehow made me feel as if I knew a lot when I didn’t, and he was able to teach me in a way where I didn’t feel like I was being lectured to,’ he said. ‘It’s a skill that I guess not many dads have with their kids: to look on them as professional equals – even though I wasn’t an equal and didn’t have his sort of experience – and make them feel valued.
‘Otherwise, I’m sure I would have gone back to hospital and probably been a physician.’
The Vahalas also found they were important to patients from the local Czech community, who maintained loyalty to their care, in some cases for generations.
‘We had a fairly large Czech population in the practice. I could speak Czech and Dad could speak Czech better than he could speak English,’ Dr Vahala said. ‘When I retired [from full-time practice] I had a patient who was 80-odd years old who used to drive [300 km] from Three Springs to see us, and bring his 45-year-old daughter. And they were Dad’s patients before they were mine.’
Present-day practiceThe semi-retired Dr Vahala is now able to reflect on a general practice career of nearly 50 years, but that doesn’t mean he is resting on his laurels. In fact, he has maintained a busy schedule into his 70s.

23Reprinted from Good Practice Issue 1–2, January–February 2017
After 46 years in practice, Dr Vahala went to work for Western Australia General Practice Education and Training (WAGPET) just over two years ago.
‘What really appeals to me in general practice education is small-group learning, where you get problem-based learning situations and work with registrars in coming to solutions and working out how to do things,’ he said.
As much as he enjoyed this type of education, Dr Vahala found that he missed face-to-face interaction with patients. After two years with WAGPET, he returned to general practice work with a variety of organisations.
‘I work for Street Doctor a couple of days a week, where I look after homeless and Aboriginal [patients],’ he said.
‘One day [a week] … I look after people with mental health issues for their comorbidities. And I do some GP after-hours work at Midland Royal Perth [Hospital], which works out to about one day a week.’
Dr Vahala has also continued to work with WAGPET on a part-time basis,
carrying out workshops and external clinical teacher visits. He also assists the RACGP with exams and the selection of new registrars.
The common thread through all of Dr Vahala’s work is a continuing love of his chosen profession.
‘I think general practice is the best job. I still enjoy getting up for work the three to four days a week, and I really value that,’ he said.
Dr Vahala has seen a great deal of change in general practice over the course of his career.
While he finds that the advent of larger practices and relatively shorter working hours can mean less face-to-face interaction with patients, Dr Vahala does appreciate the subsequent improvement to work–life balance this provides GPs.
‘It’s a far better lifestyle now in terms of your home and private life than it was,’ he said.
But whether he is reflecting on his past or enthusing about his current work in general practice, it is the profession’s connection to
people that makes Dr Vahala grateful for his career choice.
‘What I love about [general practice] is that you’ve got continuity of care,’ he said. ‘You see patients, you deliver babies, then you end up looking after the babies you delivered during their pregnancies.
‘That concept, where you look after people for up to 46 years, can’t be experienced anywhere else.’
I’m a member because …
Being at the frontline of patient management, GPs are best placed to deliver quality healthcare. I feel assured the RACGP is advocating on my behalf to the government to ensure a financially secure profession and fair working standards in the years to come.
– Dr Wence Vahala, RACGP member since 1973.

24 Reprinted from Good Practice Issue 1–2, January–February 2017
IN MY PRACTICE
Imag
es A
dela
ide
Hea
lth C
are
AMANDA LYONS
City care
Adelaide Health Care is a big city practice with an eclectic patient demographic and special skills to match.
The large and bustling Adelaide Health Care – winner of the RACGP’s 2016 South Australia and Northern Territory Practice of the Year Award – came from relatively humble beginnings when it opened in 1999. Originally named Franklin Street General Practice after its location in central Adelaide, the practice was first in a small building with four consulting rooms.
‘Five of us established the practice at that time,’ Dr Moira McCaul, GP and
practice principal, told Good Practice. ‘Four women and one man.’
Four of the original practice owners remain (the fifth, Dr Lesley Shorne, has sadly since passed away). As the city of Adelaide has grown around them, so has their practice.
‘When we moved into our little bluestone building in Franklin Street, we never anticipated we would require anything more than that,’ Dr McCaul said.
But, as patient demand grew, Adelaide Health Care moved to a bigger building in 2006 to host a larger staff (and also changed its name, due to the move from Franklin Street). These premises feature 12 consulting rooms, two treatment rooms, a nurse’s room and a clinical pathology room.
‘We now have four nurses, a midwife who works one day a week and another RN [registered nurse] who does our aged care home health assessments,’ Dr McCaul said.
‘We have two co-located mental health workers – one psychologist and one mental health social worker. We’ve also got a dietitian and an exercise physiologist.
‘Our physio practice has sadly just moved out around the corner – they’re still very close – but we’ve got podiatrists coming on board this year.’Increasing patient numbers saw Adelaide Health Care expand to larger premises in 2006.

25Reprinted from Good Practice Issue 1–2, January–February 2017
A changing demographicThe patients of Adelaide Health Care have evolved along with the city.
‘Over the time that we have been in the city, the actual residential population has increased quite dramatically and there has been a bit of a generational shift,’ Dr McCaul explained. ‘We are the genuine local practice for a lot of people; they walk around with their prams, they live in surrounding streets. Not what you would necessarily imagine for a city practice.
‘We also see a lot of city workers, a lot of local students, and a lot of international students and refugees. It’s a very eclectic mix, which is great.’
Adelaide Health Care’s focus on preventive healthcare has remained the same since its inception. Dr McCaul believes this can be traced from four of the founders’ backgrounds in women’s and community health centres.
‘We came with a very population-based, primary healthcare focus and we feel as though general practice has actually moved in that direction over the last 20 years,’ Dr McCaul said.
People might come in to talk about an ingrown toenail, but we’ll assess where they’re up to with lifestyle and exercise
‘Also, we’ve got a younger-than-average patient demographic, so that really makes it possible for us to talk to people about how to stay well.
‘I often say to people that they have got more than they bargained for because they might come in to talk about an ingrown toenail, but we’ll assess where they’re up to with their screening and their lifestyle and exercise, emphasising the importance of diet, stress levels and self-care.
‘We do a lot of talking about those things, with a real focus on managing your own health.’
The practice’s 17 doctors also demonstrate a wide range of special interests, from paediatrics to asthma management.
‘One of our doctors works at SHine SA [Sexual Health Information Networking
and Education], another is the state IUD [intrauterine device] trainer, another one works at a rape and sexual assault centre,’ Dr McCaul said.
‘We’ve got researchers and GPs who have further qualifications in paediatrics or a variety of different interests.’
Dr McCaul believes this diverse range of knowledge attracts patients from further afield than the practice’s immediate surrounds.
‘Because our GPs have a lot of specialty skills and interests, we also draw people from country areas and from all over the state,’ she said.
Passing on expertiseGiven Adelaide Health Care has been a teaching practice for more than 10 years, registrars and medical and nursing students also benefit from its GPs’ expanse of specialty skills.
‘Every registrar has their nominated supervisor who does the bulk of their teaching,’ Dr McCaul explained. ‘But other people put their hand up to be involved in the formal teaching roster.
‘There are certain people registrars and students might have mental health sessions with because we know it’s that doctor’s real skill set and expertise. There are other doctors with which they do women’s health, and others for men’s health issues or
adolescent health. So we really share out the formal teaching.’
In addition, the practice undertakes in-house training from which all can benefit.
‘We do case discussion once a week, and anyone can bring cases to that,’ Dr McCaul said. ‘We bring in speakers once a month, and that gets organised according to who needs in-servicing on what.’
Although she can occasionally be somewhat in awe of the practice’s growth, Dr McCaul is proud of what she and her fellow GPs have built.
‘There are some days when I look around and think, “How did this happen?”,’ she said. ‘I’ve got this really big practice that’s very busy with lots of things happening. But it’s all really good.
‘I think everybody who works here loves and values it. We’ve got a great team of nurses, great team of administrative staff, and a really good group of doctors.’
For Dr McCaul and her colleagues at Adelaide Health Care, winning the RACGP’s 2016 SA&NT Practice of the Year Award has added another layer of pride to their work.
‘It felt like a great acknowledgement of all our hard work. It’s lifted people’s spirits,’ Dr McCaul said. ‘I think the other doctors and nurses and everybody who works here has thought, “Yeah, great, we deserve this.” They’re really happy.’
Dr Moira McCaul (right) was one of five GPs who opened Adelaide Health Care – originally known as Franklin Street General Practice – in 1999.

26 Reprinted from Good Practice Issue 1–2, January–February 2017
RACGP SPECIFIC INTERESTS
AMANDA LYONS
Disaster management
The RACGP’s Disaster Management network works hard to ensure GPs are included in disaster planning throughout Australia.
As a central part of Australia’s health service infrastructure, GPs often provide vital assistance during disaster situations. Their role in disaster planning processes, however, is often relatively minor,1 a situation the RACGP’s Disaster Management specific interests network is working to change.
‘The aim of the network is to promote, in every way we can, opportunities for improving the integration between primary care, general practice and established [disaster management] systems,’ Dr Glynn Kelly, GP and Chair of the Disaster Management network, told Good Practice.
Dr Kelly believes that GPs are essential to disaster response efforts, and he has practical experience to back up his assertion: while President of the Australian Capital Territory (ACT) Division of General Practice, Dr Kelly developed and completed a general practice disaster management plan a few weeks before the ACT bushfires of 2003.
‘We’ve got more than 33,000 GPs2 in Australia, and that’s a valuable resource to assist [in a disaster],’ he said.
But Dr Kelly also emphasises that GPs must receive appropriate training and support in order for them to provide the best assistance as safely as possible.
‘My mantra has always been: GPs will respond,’ he said. ‘But if we’re going to respond, we need to respond as effectively and safely as possible. Because responders die in disasters and we need some training and resourcing to minimise that.’
ResourcesOne of the Disaster Management network’s most significant undertakings since its 2012 inception has been its work with the RACGP in developing Managing emergencies and pandemics in general practice: A guide for preparation, response and recovery, which was released in 2013.
This resource was funded by the Department of Health and Ageing and is freely available on the RACGP website (refer to breakout for more information).
‘There are no new lessons in disaster emergency management, just old lessons,’ Dr Kelly said. ‘We just have to always use those lessons for forward planning.’
In addition, members of the Disaster Management network work hard to develop communication channels between GPs and other health service providers in the community, both in Australia and internationally. Dr Kelly also advises GPs on how to cultivate their own connections in advance of a possible disaster.
‘[The network] encourages general practices to develop local networks with their pharmacists, ambulance workers and community nurses,’ he said. ‘Because when a disaster hits, those networks will work much better and much earlier if they are pre-established.’
According to Dr Kelly, it is important to note that GPs’ response in a disaster situation does not necessarily mean working on the frontlines of the event.
‘Response means making sure your practice can stay running to look after your normal patients,’ Dr Kelly said. ‘So if the practice down the road has closed because it burnt down or whatever else, you can take some of their overflow if need be.’
Another concern for general practice is that the effects of disaster do not necessarily subside once the event itself is over.
‘In primary care you’re often helping, treating and assisting people months and even years after the event, because they may have significant trauma or injuries,’ Dr Kelly said.
‘So our involvement doesn’t stop when the disaster ends, it often goes on for a long time. And that’s what we do. That’s our job.’
Dr Kelly is also determined that doing their job should not come at the expense of GPs’ own health, which is why the network is keen to develop a training course for working in disaster management.
‘We want to promote awareness of self-care for GPs during disasters,’ he said.
References1. The Royal Australian College of General Practitioners.
Managing emergencies and pandemics in general practice. East Melbourne, Vic: RACGP, 2013. Available at www.racgp.org.au/download/Documents/Disaster/mepsguide.pdf [accessed 14 November 2016].
2. The Department of Health. GP workforce statistics. Canberra: DOH, 2015. Available at www.health.gov.au/internet/main/publishing.nsf/content/F210D973E08C0193CA257BF0001B5F1F/$File/GPWorkforceStatistics.pdf [accessed 14 November 2016].
About the network
The Disaster Management network was endorsed in 2012. Its aims are to act as a resource for other bodies involved in disaster management, facilitate integration between general practice and established disaster response agencies, promote the need for awareness of disasters and emergencies in general practice, and develop international connections.
The network worked with the RACGP to develop Managing emergencies and pandemics in general practice: A guide for preparation, response and recovery in 2013 after receiving funding from the Department of Health and Ageing. This guide is freely available on the RACGP website (www.racgp.org.au/your-practice/business/tools/disaster/emergencies).
The network also plans to develop a course in disaster management for interested GPs.
Visit www.racgp.org.au/yourracgp/faculties/specific-interests or contact [email protected] for more information or to join the network.