The Prognostic Value of Electroneurography of … · The Prognostic Value of Electroneurography of...
Click here to load reader
-
Upload
duonghuong -
Category
Documents
-
view
212 -
download
0
Transcript of The Prognostic Value of Electroneurography of … · The Prognostic Value of Electroneurography of...

The LaryngoscopeVC 2015 The American Laryngological,Rhinological and Otological Society, Inc.
The Prognostic Value of Electroneurography of Bell’s Palsy at the
Orbicularis Oculi Versus Nasolabial Fold
Sang Hoon Kim, MD; Eun Woong Ryu, MD; Chul Won Yang, MD; Seung Geun Yeo, MD, PhD;
Moon Suh Park, MD, PhD; Jae Yong Byun, MD, PhD
Objectives/Hypothesis: We compared the prognostic value of different placements measured by electroneurography(ENoG) in Bell’s palsy, especially among patients with poor results on ENoG.
Study Design: Retrospective study using electrodiagnostic data and medical chart review from August 2006 to June2013 was performed of patients who were diagnosed with Bell’s palsy.
Methods: We included 81 patients treated from August 2006 to June 2013. Initial and final facial function was estab-lished clinically by the House-Brackmann scale. Final state of facial palsy was estimated after 6 months from onset of facialpalsy. Patients with less than 10% of ENoG response (more than 90% degeneration) were divided into three groups accord-ing to ENoG response by electrode placement as follows: group A, ENoG for orbicularis oculi (oculi) � 10% and ENoG fornasolabial fold (NLF) < 10%; group B, ENoG (oculi) < 10% and ENoG (NLF) � 10%; and group C, ENoG (oculi) < 10% andENoG (NLF) < 10%.
Results: There were no differences in demographic data among the three groups in terms of age, gender, initial paraly-sis, and days from the onset to ENoG. The complete/nearly complete recovery rates were the following: group A, 49.9%;group B, 75%; group C, 32%. The overall incomplete recovery rate in groups A and C was significantly worse than group B,and group C was the worst (P < 0.05).
Conclusion: The results suggest that ENoG of the NLF has more prognostic value in the outcomes of Bell’s palsy thanENoG of the oculi, with poorest results in patients with the NLF < 10%.
Key Words: Facial palsy, electroneurography (ENoG), facial nerve, outcome.Level of Evidence: 4.
Laryngoscope, 126:1644–1648, 2016
INTRODUCTIONBell’s palsy is unilateral weakness or paralysis of
the face due to acute peripheral facial nerve dysfunction,although the pathophysiologic mechanism of impairednerve function is still being disputed.1 The annual inci-dence of Bell’s palsy is 20 to 30 per 100,000 people, andfacial weakness generally resolves in 6 months, eitherwith medical treatment or with observation alone.2 How-ever, a small subset of affected individuals (10%–29%)displays persistent facial nerve dysfunction.2 Mostpatients with acute peripheral facial palsy are concernedabout the possibility of developing a permanent facialdeformity. Therefore, patients want to know the proba-bility and duration of recovery.3
Various objective electrophysiologic examinations offacial paralysis have been used to estimate the prognosis
of facial palsy. These have provided helpful information,which allowed the clinician to select treatment and alsohelped reduce anxiety for patients and their families.Prognostic procedures in objective electrophysiologicexaminations include scoring facial movements, the nerveexcitability test (NET), electroneurography (ENoG), elec-tromyography (EMG), and stapedial reflex measure-ments. Each of these has advantages and limitations, butNET and ENoG are the most widely used.
Electroneurography was first described by Esslenand is used to evaluate the degree of facial nerve degen-eration and predict the prognosis of patients with facialnerve palsy.4 It uses a maximal electrically evoked stim-ulus paradigm and recording technique to objectivelymeasure the amplitude of the facial compound muscleaction potential (CMAP).5 The ENoG value, which is theratio of the CMAP on the paralyzed side to the healthyside, multiplied by 100, reflects the percentage of facialnerve degeneration of the paralyzed side.6 The minimumcritical value suggesting unfavorable prognosis is 90%,above which recovery is incomplete and development ofsynkinesis secondary to aberrant regeneration is highlypossible.4
Facial palsy generally has a poor prognosis ifdegeneration measured by ENoG is greater than 90%, orif a patient has complete facial palsy within 14 days ofonset.7,8 Gantz’s study confirmed Fisch’s proposed 90%degeneration within 14 days as a cutoff for surgical
From the Department of Otolaryngology–Head and Neck Surgery,School of Medicine, Kyung Hee University (S.H.K., E.W.R., C.W.Y., S.G.Y.,M.S.P., J.Y.B.), Seoul, Republic of Korea.
Editor’s Note: This Manuscript was accepted for publicationSeptember 9, 2015.
The authors have no funding, financial relationships, or conflictsof interest to disclose.
Send correspondence to Jae Yong Byun, MD, PhD, Department ofOtolaryngology, School of Medicine, KyungHee University, 149 SangiI-Dong, Gangdong-Gu, Seoul 134-890, Republic of Korea.E-mail: [email protected]
DOI: 10.1002/lary.25709
Laryngoscope 126: July 2016 Kim et al.: Electroneurography in Facial Palsy
1644

facial nerve decompression.7 In patients with an ENoGresult exceeding 90% degeneration who show no volun-tary EMG motor unit potentials, surgical decompressionby a qualified surgeon likely offers improved functionaloutcomes.7,9
Electroneurography is usually measured in the orbi-cularis oculi muscle (oculi), and in the nasolabial fold(NLF).6 However, ENoG response can differ based onthe branch of the facial nerve and electrode placementin patients with Bell’s palsy, even within the samepatient. If ENoG results differ at each electrode position,it can be difficult to determine the prognosis of patientswith Bell’s palsy.
Therefore, our study aimed to investigate whetherENoG results can provide further prognostic informationaccording to measured placement, especially amongpatients with poor results (< 10%).
MATERIALS AND METHODS
Study DesignA retrospective review of inpatient and outpatient medical
records from August 2006 to June 2013 of patients with acuteperipheral facial palsy was performed at the Department ofOtolaryngology–Head and Neck Surgery in Kyung Hee Univer-sity Hospital at Gangdong, Seoul, Korea.
PatientsThe diagnosis of Bell’s palsy was made when patients with
peripheral facial paralysis had no obvious cause based on his-tory, physical examination, or serologic or radiologic studies.Serologic tests about varicella zoster virus; Ebstein-Barr virus;cytomegalovirus; Toxoplasmosis; hepatitis B and C; syphilis,and human immunodeficiency virus were performed. Addition-ally, serum immunoglobulin G, A, and M were checked toexclude autoimmune disease. The results of patients included inthis study were within normal range. X-rays of the mastoid andskull were reviewed to exclude patients with otitis media, frac-ture of temporal bone, and skull (Table I). Also excluded werepatients with central facial palsy, congenital palsy, and surgicalreconstruction of the facial nerve, as well as patients with dis-eases such as hypertension and diabetes mellitus becauseunderlying disease could impact recovery of facial palsy. Addi-tionally, patients who received another treatment for the sameepisode were excluded. Demographic and follow-up clinicalinformation was obtained from the patients’ medical historiesand the electrodiagnostic recording in our department’s data-base. We selected patients with less than 10% response onENoG to predict unfavorable outcomes of facial palsy. Thepatients were divided into three groups according to ENoGresults: group A, result of ENoG (oculi) � 10% and ENoG (NLF)< 10%; group B, ENoG (oculi) < 10% and ENoG (NLF) � 10%;and group C, ENoG (oculi) < 10% and ENoG (NLF) < 10%.
Clinical Evaluation of Facial Nerve FunctionThe initial and final facial nerve function after 6 months
was reported using the House-Brackmann (HB) facial nervegrading system. The HB grading system judges facial functionin six categories, ranging from grade I as normal function in allfacial areas to grade VI as complete paralysis with gross asym-metry at rest. Patients who improved to I or II on the HB grad-ing system after 6 months were considered to have a completerecovery. We defined an incomplete recovery as a score greater
than HB grade III. Follow-up was completed a minimum of 6
months from the onset of facial paralysis, or until complete
recovery.
Electroneurography Evaluation of Facial NerveFunction
Electroneurography was performed between 5 and 14 days
from the onset of facial weakness by a single highly experienced
examiner using a Nicolet Viking Select device (Madison, WI). It
was performed first on the healthy side and then repeated on
the affected side. Supramaximal stimulation of 0.2-ms duration
at a rate of 1 Hz was provided through bipolar surface electro-
des. A bipolar stimulator was placed over the truncal region of
the facial nerve on the skin over the stylomastoid foramen and
then manually adjusted to determine the best position to gener-
ate the compound action potential. For recording, the surface
electrodes were placed at the lateral third of the lower eyelid,
referred to the oculi, and just lateral to the NLF. Skin was pre-
pared with abrasive conductive paste to reduce skin impedance.
The ground electrode was placed around the patient’s wrist.
The percentage of peak-to-peak amplitudes of the ENoG
response on the affected side to those on the unaffected side
was designated as the ENoG value for the patient.
TreatmentAll patients who meet the inclusion criteria were treated
with oral corticosteroids (1mg/kg/day for 7 days, followed by 4
days of tapering), an oral antiviral agent (acyclovir or famciclo-
vir for 1 week), and protective eye care (artificial eye drops,
ointment, taping of the paralyzed eyelid during nights, and
education).
TABLE I.Serologic and Radiologic Tests.
Serologic Tests
Complete blood cell count/differential count
Erythrocyte sedimentation rate measurement
Thyroid function studies
Free T4, T3, thyroglobulin
Serum glucose level
Rapid plasma reagin and/or venereal disease research laboratoryor fluorescent treponemal antibody absorption test
HIV screening by means of enzyme-linked immunosorbent assayand/or Western blot
Immunoglobulin G, A, M
Viral antigen-antibody test
Varicella zoster virus IgG, IgM; Ebstein-Barr virus;cytomegalovirus; Toxoplasmosis
Hepatitis A, B, C antigen-antibody test
Liver function tests
AST, ALT, r-GT
Radiologic Test
Mastoid X-ray
Skull X-ray
Chest X-ray
Ig 5 immunoglobulin.
Laryngoscope 126: July 2016 Kim et al.: Electroneurography in Facial Palsy
1645

Statistical AnalysesData were analyzed with SPSS 19.0 (IBM Corp., NY).
Demographic data among groups were compared with one-wayanalysis of variance or the chi-square test at an alpha level of
5%. Comparison of recovery rate in the different ENoG groupswas conducted by Fisher’s exact test. P values of less than 0.05
indicated statistical significance.
RESULTSThis study included 45 male and 46 female
patients. Group A included 13 male and 9 femalepatients. Groups B and C included 19 and 13 malepatients, respectively, and 13 and 12 female patients,respectively. The median age was 48 years (range 15–75years; standard deviation, 17.6 years). The median ageof group A was 46 (45 6 19.2) years, and of groups Band C was 48 (47 6 17.9) and 51 (51 6 15.6) years,respectively. Forty-eight patients had a right-sided palsy,and 43 had a left-sided palsy. Ten patients in group Ahad right facial palsy, and 23 and 15 patients in groupsB and C were affected at the right side. None had bilat-eral palsy or a previous history of facial palsy. Baselinedemographic data contained days from onset to treat-ment start, the time after paralysis onset that ENoGwas performed, and the initial HB grade for each group.The median date of performed ENoG test was 7 daysfrom onset of facial palsy in all patients. The date ingroups A, B, and C was 7, 8, and 7 days from onset,respectively. Seven patients in group A had initial HBgrade IV. Ten and five patients had initial HB grade Vand VI. Twelve, 22, and 10 patients in group B had ini-tial HB grade IV, V, and VI, respectively. Five, 13, andseven patients in group C showed initial HB grade IV, V,and VI, respectively. There were no differences in base-line characteristics among the three groups in terms ofage, gender, initial paralysis, and days from onset to theENoG test. There were no differences in the differencein amplitude among groups in the ENoG results. Therewere also no differences in the percentage of peak-to-peak amplitudes of the ENoG response on the affectedside to the unaffected side among groups (Table II).
Over 6 months after treatment, 11 of 22 patients(50.0%) in group A showed a complete/nearly completerecovery; 33 of 44 patients (75.0%) in group B showed acomplete/nearly complete recovery; and eight of 25
patients (32.0%) in group C showed a complete/nearlycomplete recovery. The final recovery outcome was sig-nificantly better in group B than in groups A and C (P <
0.05) (Table III).Of the 11 (50.0%) patients with incomplete recovery
in group A, three (13.6%) had a grade III recovery out-come; six (27.2%) had a grade IV recovery outcome; andtwo (9.1%) had a grade V recovery outcome. In group B,nine (20.5%) of 44 patients showed a grade III recoveryoutcome; one (2.3%) of 44 showed a grade IV recovery out-come; and one (2.3%) of 44 showed a grade V recovery out-come. Of the 19 (76.0%) patients with incompleterecovery in group C, eight (32.0%) had a grade III recov-ery outcome; nine (36.1%) had a grade IV recovery out-come, and two (8%) had a grade V recovery outcome.There were no differences among groups in the incom-plete recovery rate in grades III or V, but group B showedan overall better recovery rate compared with groups Aand C. However, the overall incomplete recovery rate ingroups A and C was significantly worse than group B,and group C was the worst (P < 0.05) (Table IV).
DISCUSSIONThe reactivation of virus that remained dormant in
the axon and nerve endings, outbreak of inflammationand infection of cells due to external injury, exposure topoor environment, effects of metabolism, and emotionaleffects have been reported to cause nerve damage, lead-ing to Bell’s palsy.10 Recovery of approximately 70% of
TABLE II.Electrophysiologic Test.
Group A Group B Group C P Value
Diff-Amp (mV) Oculi 0.69 6 0.65 1.07 6 0.84 0.73 6 0.64 0.127
NLF 1.27 6 0.81 1.38 6 0.92 1.47 6 0.77 0.214
Diff-Amp (%) Oculi 68.9 6 32.1 70.5 6 38.3 74.3 6 43.2 0.253
NLF 69.1 6 35.4 69.8 6 31.2 72.4 6 29.8 0.345
Group A: ENoG (oculi) � 10% and ENoG (NLF) < 10%Group B: ENoG (oculi) < 10% and ENoG (NLF) � 10%.Group C: ENoG (oculi) < 10% and ENoG (NLF) < 10%Diff-AMP: amplitude of unaffected side amplitude of affected side.Diff-AMP (%): 100 (amplitude of affected side/amplitude of unaffected side) 3100(%).Diff-AMP 5 difference of amplitude, mV; ENoG 5 electroneurography; NLF 5 nasolabial fold; oculi 5 orbicularis oculi muscle.
TABLE III.Relationships of Complete/Near-Complete Recovery Rate to the
Different ENoG Groups.
Group A(n 5 22)
Group B(n 5 44)
Group C(n 5 25) P Value
Grade I 6 (27.2%) 20 (45.5%) 4 (16.0%) 0.037*
Grade II 5 (22.7%) 13 (29.5%) 4 (16.0%) 0.358
Total 11 (49.9%) 33 (75.0%) 8 (32%) 0.025*
*P < 0.05Group A: ENoG (oculi) � 10% and ENoG (NLF) < 10%.Group B: ENoG (oculi) < 10% and ENoG (NLF) � 10%.Group C: ENoG (oculi) < 10% and ENoG (NLF) < 10%.ENoG 5 electroneurography; NLF 5 nasolabial fold; oculi 5 orbicu-
laris oculi muscle.
Laryngoscope 126: July 2016 Kim et al.: Electroneurography in Facial Palsy
1646

patients with Bell’s palsy up to grade I in the HB grad-ing system has been reported, and approximately 83% ofpatients with Bell’s palsy up to grade II.11 A total of75.0% of patients with less than 10% on ENoG in theoculi showed complete recovery in our study. This is sim-ilar to the overall complete recovery rate of Bell’s palsyin past studies, although the ENoG response is less than10% in the oculi. This suggests that ENoG results meas-ured only at the orbicularis oculi cannot reliably predictunfavorable outcomes for patients with Bell’s palsy.
Facial ENoG is the objective electrophysiologic mea-surement of a muscle compound action potential used toassess nerve degeneration. The ENoG value is the ratioof facial nerve degeneration on the paralyzed side tothat of the healthy side.6 Because the technique wasdeveloped and introduced to otolaryngology by Esslenand Fisch, a number of studies have evaluated the prog-nostic value of ENoG.4,6 The degree of nerve fiber degen-eration can be found by comparison between theparalyzed and normal sides, which can forecast the prog-nosis of Bell’s palsy and help clinicians plan for propertreatment.12 May et al. showed that ENoG amplitudereductions to less than 10% on the unaffected side werehighly associated with incomplete recovery.13 Gantzet al. showed that subjects who reached 90% degenera-tion on ENoG within 14 days of paralysis returned toHB grade 1 or 2 within 7 months of onset of paralysis.9
Fisch reported recovery in 50% of patients with 90% ormore ENoG degeneration and 80% recovery in patientswith less than 90% degeneration.10 Mantsopoulos et al.also showed that patients with 90% or more ENoGdegeneration had 7.5 times the probability of an unsatis-factory long-term result.14 We observed similar recoveryrates for patients with less than 10% ENoG in the NLFelectrode on our study. Therefore, ENoG results meas-ured at the NLF may reliably predict unfavorable out-comes in patients with Bell’s palsy. Most of the reportscalculated ENoG results from one subsite or the meanvalue of two subsites (oculi and NLF) for use in theiranalysis. ENoG is a useful and important tool to evalu-ate facial palsy at a early stage of Bell’s palsy; at thistime, we can determine whether the facial nerve shouldbe decompressed. This determination is important toimprove the final state of facial palsy. ENoG is more reli-
able to estimate facial palsy at early stage than othertools, electromyography, maximal stimulation test, nerveexcitability test. So we used ENoG result to predictrecovery of facial palsy in our study.
The timing of Wallerian degeneration is an addi-tional feature of electrodiagnosis that provides importantprognostic information. Injuries that induce only a con-duction block within the nerve (neuropraxia) do not dis-rupt axoplasmic continuity and therefore can conduct aneural discharge if an electrically evoked stimulus ispresented distal to the conduction block. More severeinjuries such as axoplasmic disruption (axonotmesis) orneural tubule disruption (neurotmesis) result in Waller-ian degeneration distal to the site of the injury. Waller-ian degeneration in the peripheral facial nerve usuallytakes about 72 hours to become apparent after onset ofthe lesion, so it is recommended that ENoG not be per-formed until at least 3 days after onset.7 In this study,we performed ENoG between 5 and 14 days after theonset of facial weakness.
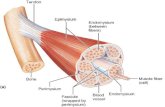
The facial nerve exits from the stylomastoid fora-men and enters into the parotid gland. The nerve travelsanteriorly and divides into a few branches. The five ter-minal branches of the facial nerve are the temporal,zygomatic, buccal, marginal mandibular, and cervicalbranches.
These branches communicate with each other inthe gland and distribute radially to the facial mimeticmuscle. According to most literature and anatomy books,the temporal branch and zygomatic branch innervatethe orbicularis oculi muscle, and the buccal branch andmarginal mandibular branch or the buccal branch aloneinnervate the orbicularis oris muscle.10,11 Other litera-ture reported that the temporal branch innervates theforehead muscles and the superior part of the orbicularisoculi; the zygomatic branch innervates the muscles ofthe NLF; and the buccal branch innervates the buccina-tors and orbicularis oris.15 A weakened orbicularis oculiwill cause lagophthalmos, and in severe cases will causeparalytic ectropion.
The NLFs are maintained by the orbicularis oris,zygomaticus major, zygomaticus minor, levator labiisuperioris, and levator labii superioris alaeque nasimuscles. These muscles are tested as a group by askingthe patients to smile, show their teeth, or pull back thecorners of their mouth. The amplitude of the CMAP,measured from the movement of the facial muscles witha surface electrode, was proportional to the number ofblocked nerve fibers that could be stimulated. By com-paring the paralyzed side of the face with the normalside, an estimate of the amount of the nerve that haddegenerated could be determined. Dividing the responseof the paralyzed side by the normal side and subtractingfrom 100% estimates the percentage of fibers that havedegenerated. Supramaximal strength was used to ensurethat all nerve fibers were stimulated.16 The recordingwas accepted only when the shape of the obtained signalwas consistent at two consecutive stimulations to ensurerelative response stability.17
In our study, one highly experienced examinerrepetitively conducted ENoG to eliminate error between
TABLE IV.Relationships of Incomplete Recovery Rate to the Different ENoG
Groups.
Group A(n 5 22)
Group B(n 5 44)
Group C(n 5 25) P Value
Grade III 3 (13.6%) 9 (20.5%) 8 (32.0%) 0.243
Grade IV 6 (27.2%) 1 (2.3%) 9 (36.1%) 0.015*
Grade V 2 (9.1%) 1 (2.3%) 2 (8%) 0.324
Total 11 (50.0%) 11 (25.0%) 19 (76.0%) 0.028*
*P < 0.05.Group A: ENoG (oculi) � 10% and ENoG (NLF) < 10%.Group B: ENoG (oculi) < 10% and ENoG (NLF) � 10%.Group C: ENoG (oculi) < 10% and ENoG (NLF) < 10%.ENoG 5 electroneurography; NLF 5 nasolabial fold; oculi 5 orbicu-
laris oculi muscle.
Laryngoscope 126: July 2016 Kim et al.: Electroneurography in Facial Palsy
1647

results. ENoG measures the amplitude of wave formsappearing while contracting all muscles that areinvolved by providing a supramaximal threshold stimu-lus. The amplitude of these wave forms is stimulatedand is proportional to the number of nerve fibers thatreact and their synchronicity.18 It seems that differencein prognosis among groups is related to the amount ofmuscle that affects nerve conduction. The NLF has moremuscles dominated by the facial nerve than the oculi.Therefore the result of ENoG on NLF is more significantin predicting recovery from facial palsy than the oculi.
In the event of facial nerve palsy after proximalnerve injury, the degree of degeneration is different ineach nerve branch, which might relate to the thicknessand lengths of each branch. Engstrom et al. reportedthat the nasalis and/or mentalis initial ENoGs were thebest single recordings in predicting favorable outcomes,and additional muscle registrations may improve theirprognostic accuracy in Bell’s palsy.19 Our findings thatENoG results at the NLF more precisely reflect facialnerve function and recovery of facial palsy are in agree-ment with these results. The recovery rate of patientswith poor results at both the oculi and the NLF onENoG is lower than that of patients who only have oneaffected.
Our study focused on ENoG results < 10% to pre-dict unfavorable outcomes. Therefore, we selectedpatients with ENoG results < 10% and analyzed ENoGresults and electrode placement data to determine theability to predict the recovery rate of facial palsy by theHB grading system. Patient recovery was estimateduntil 6 months after onset of Bell’s palsy different,unlike Engstrom’s study, which used a 3-month cutoff.The final follow-up period to estimate facial palsy isimportant in determining the recovery rate because it ispossible to improve facial palsy.
Study LimitationsThere are potential limitations of this work. First,
this study was limited by the small number of patients.To improve our understanding, further research shouldverify these findings with more patients. Second, weonly used ENoG to evaluate facial palsy. Finally, weused the oculi and NLF, which are commonly used asplacement for ENoG, but other electrode placements forENoG can be used to study the facial nerve branch. Wewill study the prognosis of Bell’s palsy with result of
other electrodiagnostic tools and electrode placements ofENoG in future research.
CONCLUSIONThis study showed that degeneration of the facial
nerve branch in Bell’s palsy patients can be variable.The results suggest that ENoG of the NLF has moreprognostic value in the outcomes of Bell’s palsy thanENoG of the oculi, with poorest results in patients withthe NLF < 10%.
AcknowledgmentS.H.K. and E.W.R. are co-first authors of this article.
BIBLIOGRAPHY
1. May M, Hughes GB. Facial nerve disorders: update 1987. Am J Otol 1987;8:167–180.
2. Adour KK. Combination treatment with acyclovir and prednisone for Bellpalsy. Arch Otolaryngol Head Neck Surg 1998;124:824.
3. Sittel C, Stennert E. Prognostic value of electromyography in acute periph-eral facial nerve palsy. Otol Neurotol 2001;22:100–104.
4. Esslen E. The acute facial palsies: investigations on the localization andpathogenesis of meato-labyrinthine facial palsies. Schriftenr Neurol1977;18:1–164.
5. Gantz BJ, Gmuer AA, Holliday M, Fisch U. Electroneurographic evalua-tion of the facial nerve. Method and technical problems. Ann Otol Rhi-nol Laryngol 1984;93:394–398.
6. Fisch U. Maximal nerve excitability testing vs electroneuronography. ArchOtolaryngol 1980;106:352–357.
7. Fisch U. Prognostic value of electrical tests in acute facial paralysis. Am JOtol 1984;5:494–498.
8. Sillman JS, Niparko JK, Lee SS, Kileny PR. Prognostic value of evokedand standard electromyography in acute facial paralysis. OtolaryngolHead Neck Surg 1992;107:377–381.
9. Fisch U. Surgery for Bell’s palsy. Arch Otolaryngol 1981;107:1–11.10. Furuta Y, Fukuda S, Chida E, et al. Reactivation of herpes simplex virus
type I in patients with Bell’s palsy. J Med Virol 1998;54:162–166.11. Peitersen E. The natural history of Bell’s palsy. Am J Otol 1982;4:107–111.12. Thomander L, Stalberg E. Electroneurography in the prognostication of
Bell’s palsy. Acta Otolaryngol 1981;92:221–237.13. May M, Blumenthal F, Klein SR, et al. Acute Bell’s palsy: prognostic value
of evoked electromyography, maximal stimulation, and other electricaltests. Am J Otol 1983;5:1–7.
14. Mantsopoulos K, Psillas G, Psychogios G, Brase C, Iro H, ConstantinidisJ. Predicting the long-term outcome after idiopathic facial nerve paraly-sis. Otol Neurotol 2011;32:848–851.
15. Walker K, Hall W, Husrt J, eds. Cranial nerve VII: the facial nerve andtaste. In: Clinical Methods: The History, Physical, and LaboratoryExaminations 3rd ed. Boston, MA: Butterworths; 1990:322–326.
16. Kartush JM, Lilly DJ, Kemink JL. Facial electroneurography: clinical andexperimental investigations. Otolaryngol Head Neck Surg 1985;93:516–523.
17. Hughes GB, Josey AF, Glasscock ME, Jackson CG, Ray WA, Sismanis A.Clinical electroneurography: statistical analysis of controlled measuresin twenty-two normal subjects. Laryngoscope 1981;91:1834–1846.
18. Redhead J, Mugliston T. Facial electroneuronography: action potentialamplitude and latency studies in 50 normal subjects. J Laryngol Otol1985;99:369–372.
19. Engstrom M, Jonsson L, Grindlund M, Stalberg E. Electroneurographicfacial muscle pattern in Bell’s palsy. Otolaryngol Head Neck Surg 2000;122:290–297.
Laryngoscope 126: July 2016 Kim et al.: Electroneurography in Facial Palsy
1648