The Pa Tho Physiology of Acute Coronary Syndromes
-
Upload
anelita123 -
Category
Documents
-
view
219 -
download
0
Transcript of The Pa Tho Physiology of Acute Coronary Syndromes
8/3/2019 The Pa Tho Physiology of Acute Coronary Syndromes
http://slidepdf.com/reader/full/the-pa-tho-physiology-of-acute-coronary-syndromes 1/6
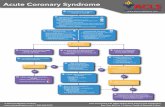
Virtually all regional acute myocardialinfarcts are caused by thrombosis devel-oping on a culprit coronary atheroscle-
rotic plaque. The very rare exceptions to thisare spontaneous coronary artery dissection,coronary arteritis, coronary emboli, coronaryspasm, and compression by myocardialbridges. Thrombosis is also the major initiatingfactor in unstable angina, particularly whenrest pain is recent and increasing in severity.Necropsy studies suggest that a new throm-botic coronary event underlies 50–70% of sud-den deaths caused by ischaemic heart disease.
The culprit plaque
Given the importance of thrombosis as the
trigger for acute myocardial ischaemia, it is
necessary to know something about the
structure of plaques before thrombotic events
occur and why there should be a sudden
change from a stable state (no thrombus) to an
unstable state (thrombus).The fully developed human fibrolipid
plaque, designated by the American Heart
Association (AHA) as type IV or type Va,1 has
a core of lipid surrounded by a capsule of con-
nective tissue (fig 1). The core is an extracellu-
lar mass of lipid containing cholesterol and its
esters, some of which is in a crystalline form.
The core is surrounded by numerous macro-
phages, many of which contain abundant
intracytoplasmic droplets of cholesterol (foamcells). These macrophages are derived frommonocytes which crossed the endotheliumfrom the arterial lumen. They are not inert orend stage cells, but are highly activated,producing procoagulant tissue factor and ahost of inflammatory cell mediators such astumour necrosis factor (TNF ), inter-leukins, and metalloproteinases. The connec-tive tissue capsule which surrounds this
inflammatory mass is predominantly collagensynthesised by smooth muscle cells. Theportion of the capsule separating the core fromthe arterial lumen itself is the plaque cap.
The early stages of plaque development(AHA types I–III) are not associated with evi-dence of structural damage to the endothe-lium. Once plaque formation has progressed tostage IV, however, structural changes in theendothelium become almost universal.2 Theendothelium over and between plaques showsenhanced replication compared to normalarteries, implying a degree of endothelial cellimmaturity and abnormal physiological func-tion. Focal areas of endothelial denudation
occur over the plaque, exposing the underlyingconnective tissue matrix and allowing amonolayer of platelets to adhere at the site.Such ultramicroscopic thrombi are far toosmall to be visible on angiography or to impedeflow, but may contribute to plaque smoothmuscle cell growth by release of plateletderived growth factor.
Mechanisms of thrombosis
Thrombosis over plaques occurs because of two somewhat diV erent processes. One iscaused by an extension of the process of
endothelial denudation so that large areas of the surface of the subendothelial connectivetissue of the plaque are exposed. Thrombusforms which is adherent to the plaque surface(fig 2). This process has become known asendothelial erosion. Observational studies havelinked endothelial cell loss to the proximity of macrophages. These macrophages are highlyactivated and cause endothelial cell death byapoptosis, and also by the production of proteases which cut loose the endothelial cellsfrom their adhesion to the vessel wall.
The second mechanism for thrombus forma-tion is plaque disruption (synonyms rupture,fissuring) (fig 3). Here the plaque cap tears to
expose the lipid core to blood in the arteriallumen. The core area is highly thrombogenic,containing tissue factor, fragments of collagen,and crystalline surfaces to accelerate coagula-tion. Thrombus forms initially in the plaqueitself which is expanded and distorted fromwithin; thrombus may then extend into thearterial lumen (fig 4).
Plaque disruption,like endothelial erosion, isa reflection of enhanced inflammatory activitywithin the plaque.3 The cap is a dynamic struc-ture within which the connective tissue matrix,upon which its tensile strength depends, isconstantly being replaced and maintained by
CORONARY DISEASE
The pathophysiology of acute coronarysyndromes
Michael J Davies
St George’s Hospital Medical School, Histopathology Department,
London, UK
Figure 1: The established stable plaque. In this cross section of a humancoronary artery there is an established fibrolipid plaque with a core of lipid. Thelipid core is separated from the lumen by the plaque cap. The plaque onlyoccupies part of the circumference of the artery, leaving a segment of normalarterial wall.
Heart 2000;83:361–366
36
Correspondence to:
Professor M J Davies,St George’s HospitalMedical School,Histopathology
Department, CranmerTerrace, London SW170RE, UK
8/3/2019 The Pa Tho Physiology of Acute Coronary Syndromes
http://slidepdf.com/reader/full/the-pa-tho-physiology-of-acute-coronary-syndromes 2/6
the smooth muscle cell. The inflammatoryprocess both reduces collagen synthesis byinhibiting the smooth muscle cell and causes itsdeath by apoptosis. Macrophages also producea wide range of metalloproteinases capable of degrading all the components of the connectivetissue matrix, including collagen. These metal-loproteinases are secreted into the tissues in aninactive form and then activated by plasmin.Metalloproteinase production by macrophages
is upregulated by inflammatory cytokines suchas TNF. Plaque disruption is therefore nowseen as an auto-destruct phenomenon associ-ated with an enhanced inflammatory activation.
The relative importance of disruption anderosion as triggers of thrombosis may varybetween diV erent patient groups. Disruption isthe predominant cause (> 85%) of majorcoronary thrombi in white males with highplasma concentrations of low density lipopro-tein (LDL), and low concentrations of highdensity lipoprotein (HDL). In contrast, inwomen endothelial erosion is responsible foraround 50% of major thrombi.4–6 The distinc-tion between erosion and disruption is not
necessarily of major clinical importance. Bothprocesses depend on enhanced inflammatoryactivity within the plaque and appear equallyresponsive to lipid lowering. Disruption has anintraplaque component more resistant to fibri-nolytic treatment, while in erosion the throm-bus is more accessible. This potential advan-tage is, however, oV set by erosion relatedthrombi tending to occur at sites where thepre-existing stenosis was more severe. Inwomen there is also a form of thrombosiscaused by endothelial erosion over plaqueswhich do not contain lipid or have a majorinflammatory component.6 This type of diseaseis rare and arguably distinct from conventionalatherosclerosis, and may be smoking related.
The vulnerable plaque concept
Analysis of plaques which have undergone dis-ruption has been used to determine character-istics which may indicate currently stableplaques whose structure and cell contentmakes them likely to undergo an episode of thrombosis in the future (vulnerable plaques).
There is widespread unanimity7 in the belief that these features are:+ a large lipid core occupying at least 50% of
the overall plaque volume+
a high density of macrophages+ a low density of smooth muscle cells in thecap
+ a high tissue factor content+ a thin plaque cap in which the collagen
structure is disorganised.All of these markers of plaques at future risk
are likely to be the direct result of macrophageactivity, which enlarges the core and thins thecap.
The risk of any subject with coronary arterydisease having a future acute event will dependon the number of these vulnerable plaqueswhich are present rather than on the total
number of plaques. Patients, however, vary inthe number of vulnerable plaques which arepresent in the coronary arteries—this variationexplains why one individual has a series of inf-arcts at regular intervals while another indi-vidual has an infarct without further events for10 or even 20 years.
The sequence of thrombotic events
The thrombi which occur either in disruptionor erosion circumstances are dynamic andevolve in stages. In disruption the initial stageoccurs within the lipid core itself and ispredominantly formed of platelets. As throm-bus begins to protrude into the lumen thefibrin component increases, but any surfaceexposed to the blood in the lumen will be cov-ered by activated platelets. While antegradeflow continues over this exposed thrombus,clumps of activated platelets are swept downinto the distal intramyocardial arteries asmicroemboli (fig 5). Thrombus may grow to
Figure 2: Thrombosis caused by erosion. This human coronary artery is largelyoccluded by a mass of thrombus which is adherent to the surface of a plaque.The plaque itself is intact.
Figure 3: Thrombosis caused by disruption. The cap of a plaque has torn andprojects up into the lumen. Thrombus has formed within the original lipid corefrom where it projects into, but does not totally occlude, the lumen. This is thetypical lesion of unstable angina.
Education in Heart
362
8/3/2019 The Pa Tho Physiology of Acute Coronary Syndromes
http://slidepdf.com/reader/full/the-pa-tho-physiology-of-acute-coronary-syndromes 3/6
occlude the artery, leading to a final stage inwhich there is a loose network of fibrincontaining large numbers of entrapped redcells. This third and final stage thrombus maypropagate distally after the onset of myocardialinfarction. The final stage of occlusive throm-bus has a structure making it very susceptibleto either natural or therapeutic lysis, but thiswill expose the deeper and earlier thrombuswhich is more resistant to lysis.
Symptomology in relation to coronary
thrombi
Episodes of plaque disruption which are almostentirely associated with intraplaque thrombusare associated with the onset or exacerbation of stable angina caused by a sudden increase inplaque volume.
Thrombi which project into but do notocclude the lumen (mural thrombi) are thebasis of unstable angina. The intermittentattacks of myocardial ischaemia at rest arecaused by several potential mechanisms.+ The thrombus may intermittently wax and
wane in size and become occlusive for rela-tively short periods of time.
+
There may be intense local vasoconstriction.Many disrupted plaques are eccentric, withthe retention of an arc of normal vessel wallin which constriction can reduce blood flow.
+ Platelet deposition is a known potent stimu-lus for local smooth muscle constriction.
+ Embolisation of platelet aggregates into theintramyocardial vascular bed both blocksmaller arteries in the size range of 50−100 µm external diameter and causevasoconstriction within the myocardium.Necropsy studies show a strong correlationbetween such platelet thrombi and micro-scopic foci of myocyte necrosis.8 9
Clinical correlations
Much of the work described so far is based onnecropsy observations but these have beenextended and amplified by observations madein life to give the dynamic dimension.
Acute myocardial infarction
It is diY
cult now to perceive why coronarythrombosis was regarded 25 years ago as aninconstant and irrelevant consequence of acuteinfarction rather than its prime cause. Onceangiography was carried out soon after theonset of infarction, and it was realised that thesubtending artery was totally blocked butspontaneously reopened with time in manycases (and that this reopening was acceleratedby fibrinolytic treatment), thrombosis was seenas a major causal factor in occlusion. Suddenlythe clinical world found thrombi to be bothdynamic and important. Pathologists hadthought thrombi were important but did notrealise how dynamic they could be. Sequentialangiograms taken over some years in patients
with chronic ischaemic heart disease alsochanged perceptions. It was realised that a sig-nificant proportion of the thrombotic occlu-sions causing infarction did not develop at siteswhere there was pre-existing high grade steno-sis, or even a plaque identified at all. Sixty eightper cent of the occlusions leading to acute inf-arction were judged to have caused less than50% diameter stenosis previously, while only14% developed on high grade stenoses of morethan 70% diameter in a recent review of theliterature.10
The advent of intravascular ultrasound hasconfirmed that many stable coronary plaquesare angiographically invisible because of arte-
rial remodelling. In this process, described sowell by Glagov,11 the artery is seen to respondto plaque growth by increasing its crosssectional area while retaining normal lumendimensions. Angiography cannot and does notpredict the sites and risk of future infarction. Itis true that chronic high grade stenoses doprogress to occlude, but this is a slow processand is often caused by erosion type thrombosis,and is not associated with acute infarction dueto collateral flow. For example, 24% of lesionsoccluding more than 80% by diameter willprogress to chronic total occlusion by fiveyears.
Figure 4: Thrombosis caused by disruption. The capof the plaque has torn and thrombus within the lipidcore extends into and occludes the lumen. This isthe typical lesion of acute myocardial infarction.
Figure 5: Platelet embolisation. Any thrombus (red)
which protrudes into the arterial lumen but does notocclude has the surface covered by a layer ofactivated platelets strongly expressing the IIb/IIIareceptor. Clumps of these platelets are swept downinto the myocardium vascular bed.
Education in Heart
363
8/3/2019 The Pa Tho Physiology of Acute Coronary Syndromes
http://slidepdf.com/reader/full/the-pa-tho-physiology-of-acute-coronary-syndromes 4/6
The magnitude of episodes of disruptionvaries widely. At one extreme the plaque has acrack or fissure only, and the large thromboticresponse appears out of proportion to thestimulus. Such events are easily treated by lysisto give a lumen size which is little diV erentfrom the previous state or event taken to be anormal artery. At the other extreme a plaqueundergoes complete disintegration, occludingthe lumen with a mixture of plaque content
and thrombus. Another form is where theartery is occluded by the thrombus expandingthe plaque from within. These more complextypes of disruption occlusion will be morelikely to respond to primary angioplasty. Theexact morphology of disrupted plaques causingocclusion cannot, however, be determined invivo by any current methodology.
Transmural regional acute myocardial inf-arction is caused by a coronary artery occlusionwhich develops over a relatively short timeframe of a few hours and persists for at least6–8 hours. The infarcted tissue is structurallysuggestive of a homogenous entity—that is, allthe myocardium involved died at around the
same time. Non-transmural regional infarcts(non-Q wave) have a diV erent structure whichis built up by the coalescence of many smallareas of necrosis of very diV erent ages. Thispattern of necrosis characteristically followscrescendo unstable angina and appears to becaused by repetitive episodes of short livedocclusion or platelet embolisation, or both. Afurther factor in limiting the spread of necrosisand preserving the subpericardial zone is theexistence of prior collateral flow in the aV ectedartery.
Unstable anginaThe challenge of understanding the patho-physiology of unstable angina is the wide spec-
trum of clinical severity.12 Necropsy studies areinevitably biased toward the worst outcome,but within this limitation show unstable anginato be caused by disrupted plaques withexposed mural thrombus and retention of antegrade flow in the artery. This feature of some persistent antegrade flow is all that sepa-rates the vascular lesion of unstable anginafrom that of acute infarction. The persistenceof the thrombotic process so that it neitherprogresses to occlude nor resolves to heal rep-resents a balance between prothrombotic andantithrombotic factors. Confirmation of plaquedisruption and thrombosis as the basis forsevere unstable angina has come from angio-
graphy in vivo where type II lesions withirregular overhanging edges and intraluminalfilling defects (fig 6) representing thrombus arefound.13 These angiographic appearances arerare in stable angina. Type II lesions have beenshown to be disrupted plaques by pathologystudies. Angioscopy has directly observed tornplaque caps in vivo and intravascular ultra-sound has also identified disrupted plaques invivo. Atherectomy studies comparing tissuefrom plaques thought to be responsible forstable and unstable angina have shown veryconsistent results. A significant proportion, butnot all, of samples from unstable angina
contain thrombus, while most samples fromstable angina, but not all, do not containthrombus. The absence of thrombus in unsta-ble angina is in part related to the time delaybetween acute symptoms and atherectomy.14
Samples taken some weeks after the last epi-sode of rest pain often show acceleratedsmooth muscle proliferation—that is, the heal-ing process rather than the acute thromboticprocess. The presence of thrombus in plaquecausing stable angina highlights the role of subclinical disruption or erosion in plaquegrowth. The pathological changes in plaquescausing unstable angina expose thrombus in anartery in which antegrade flow continues.Platelet emboli into the myocardium causemicroscopic foci of necrosis which are the basisof the increased concentrations of troponin T
found in the blood in a proportion of cases of unstable angina.
The problem of the pathophysiology of unstable angina lies in patients who havemilder and persistent rest pain over months oreven years. The perception is that these casesare related to vasomotor tonal abnormalitiesoften occurring at specific sites in the coronaryartery tree. Why one such plaque should leadto local spasm is unclear—one suggestion isthat there is local endothelial damage andrepetitive ultramicroscopic thrombosis. Thepreponderance of literature reports of suchvasospastic angina from Japan suggests theremay be racial or geographic diV erences in thepathogenesis of this form of unstable angina.
Plaque disruption: the healing process
The great majority of episodes of plaquedisruption do not cause a major event such asinfarction or death. Minor episodes of erosionor disruption are often clinically silent but docontribute to the episodic progression of coronary artery disease seen on sequentialangiography.
Thrombus will be removed by natural lysis tosome extent and is also associated with “passi-
Figure 6: Angiogram of plaque disruption. In thispostmortem angiogram there is a typical type IIeccentric ragged stenosis with an overlyingintraluminal filling defect indicating thrombus over theplaque.
Education in Heart
364
8/3/2019 The Pa Tho Physiology of Acute Coronary Syndromes
http://slidepdf.com/reader/full/the-pa-tho-physiology-of-acute-coronary-syndromes 5/6
fication”, a term implying that the exposed col-lagen becomes less active in causing plateletadhesion probably due to being coated bynatural heparinoids. Any residual thrombuswhich is still present after 36 hours will provokesmooth muscle cell migration into the area,with the production of new connective tissuewhich smooths out the surface and restoresplaque integrity. The final result will be a stablelesion which may cause anything from chronictotal occlusion to only a minor increase fromthe pre-existing degree of stenosis. The proc-ess, however, takes weeks and residual thrombiin the base of the exposed lipid core act as anidus for a further thrombotic event at thesame site for up to six months.
The risk of progressing to complete occlu-sion on angiography within a year of an episodeof unstable angina, or after lysis for acute myo-cardial infarction, is far higher if the culpritlesion has an irregular outline on the initialangiogram taken immediately after the acuteevent.15
Inflammation and coronaryatherosclerosis
Atherosclerotic plaques are the site of aninflammatory reaction which is of equal inten-sity to that found in the synovium in acuterheumatoid arthritis. The volume of anyindividual plaque in the coronary arteries issmall, but most individuals have many plaquesin the carotid artery and aorta which can be upto 2 cm in length. It is therefore not surprisingthat there may be elevation in systemic markersof inflammation such as fibrinogen and C reac-tive protein in subjects with chronic coronaryatherosclerosis. The physicians health studyshows that the diV erence between the lowestand highest quartiles of C reactive protein con-centration is a threefold increase in the risk of afuture acute event.16 The actual concentrations
of C reactive protein are not, however, high andsuch estimates give assessment of group rather
than individual risk. One explanation is that thesubjects with the highest concentrations of Creactive protein have the largest plaque mass.The link between systemic markers of chronicinflammation and acute coronary events may,however, be more complex. There is experi-mental evidence that upregulation of systemicinflammation will have a secondary aV ect of enhancing inflammatory activity in theplaque.17 18 On this basis any factor which
increases systemic inflammation would poten-tially trigger plaque instability and increase therisk of unstable angina. Causes of suchsystemic low grade inflammation includeinfection by chlamydia or helicobacter, diseasessuch as rheumatoid arthritis, and chronicdental sepsis.
Lipid lowering, infection, and acutecoronary events
The current view of atherosclerosis is that theprime stimulus for plaque inflammation is thereaction between oxidised LDL and the
macrophage. Significant reduction of plasmalipids in animal models of atherosclerosis has aprofound eV ect on the plaque morphology,with a reduction in both macrophage numbersand activation products including metallopro-teinases. The resultant plaque will be lessinflammatory, and smooth muscle cell num-bers and the collagen content rise. Althoughnot reduced greatly in size, the plaque would beat far less risk of thrombosis. Similar changes inhuman plaques would explain the consistentbenefit observed in a reduction of acute eventsin all the statin based trials.
Even allowing for poor patient compliance,the need for at least 18 months for the benefitto appear, and inadequate lipid lowering, acute
ischaemic events still occur in treated patients.This suggests there may be non-lipid depend-ent factors enhancing plaque inflammation.One such factor is direct invasion of the plaqueby chlamydia. These organisms exist withinmacrophages and potentially could upregulatethe production of inflammatory mediatorswithin the plaque.18 Therapeutic trials of antichlamydial drugs to reduce acute coronaryevent rates are currently underway but resultsso far are contradictory. It seems likely thatthere are many other factors which enhance theinflammatory activity of the plaque, but theprimary stimulus remains the conversion of plasma LDL in the intima to a proinflamma-
tory product.
19
In keeping with this view is theconsistent message from animal models of atherosclerosis that reducing plasma lipid con-centrations strikingly reduces all the inflamma-tory processes in the plaque.20
1. Stary H, Chandler A, Dinsmore R, et al . A definition ofadvanced types of atherosclerotic lesions and a histologicalclassification of atherosclerosis. A report from the committeeon vascular lesions of the council on atherosclerosis,American Heart Association. Circulation 1995;92:1355–74.• Atherosclerotic plaques are morphologically diverse. This
AHA committee report is the best nomenclature so far produced to describe the different forms and highlights the importance of a lipid core and fibrous cap in plaques at risk of thrombotic compliations.
Mechanisms of myocardial ischaemia in
non-occluding coronary thrombosis
x Distal embolisation of aggregates of platelets
x Intermittent total occlusion
x Spasm at thrombus site
Plaques at risk of future thrombotic events are characterised by:
x Large lipid cores (> 50% overall plaque volume)
x Thin caps
x High densities of macrophages and high levels of expression of tissuefactor and metalloproteinases
x Low densities of smooth muscle cells
Education in Heart
365
8/3/2019 The Pa Tho Physiology of Acute Coronary Syndromes
http://slidepdf.com/reader/full/the-pa-tho-physiology-of-acute-coronary-syndromes 6/6
2. Davies M, Woolf N, Rowles P, et al . Morphology of theendothelium over atherosclerotic plaques in human coronaryarteries. Br Heart J 1988;60:459–64.
3. Ross R. Atherosclerosis—an inflammatory disease.N Engl J Med 1999;340:115–26.
4. Burke A, Farb A, Malcom G, et al . Coronary risk factorsand plaque morphology in men with coronary disease whodied suddenly. N Engl J Med 1997;336:1276–82.
5. Davies M. The composition of coronary artery plaques.N Engl J Med 1997;336:1312–13.
6. Arbustini E, Dal Bello P, Morbini P, et al . Plaqueerosion is a major substrate for coronary thrombosis in acutemyocardial infarction. Heart 1999;82:269–72.• Thrombosis over a plaque is either caused by erosion or
disruption. This paper illustrates endothelial erosion and highlights its contribution to acute myocardial infarction.
7. Davies M. Stability and instability: two faces of coronaryatherosclerosis. The Paul Dudley White Lecture 1995.Circulation 1996;94:2013–20.• A review of the concept of plaque thrombosis being
caused by erosion or disruption and highlighting the role that plaque inflammation plays. The concept that collagen production and smooth muscle proliferation are essential in maintaining plaque stability (resistance to thrombosis) is described.
8. Davies M, Thomas A, Knapman P, et al . Intramyocardialplatelet aggregation in patients with unstable anginasuffering sudden ischaemic cardiac death. Circulation 1986;73:418–27.
9. Falk E. Unstable angina with fatal outcome: dynamiccoronary thrombosis leading to infarction and/or suddendeath. Circulation 1985;71:699–708.• This paper describes the characteristic non-occluding
thrombi that cause unstable angina and explains that distal
embolisation of platelets is an important mechanism for intermittent myocardial ischaemia.
10. Falk E, Shah P, Fuster V. Coronary plaque disruption.Circulation 1995;92:656–71.
11. Glagov S, Weisenberd E, Zarins C, et al .Compensatory enlargement of human atheroscleroticcoronary arteries. N Engl J Med 1987;316:1371–5.• This article should be compulsory reading for everyone
who carries out coronary angiography. It explains that the usual response of a coronary artery to the formation of a plque is to increase its cross sectional area to preserve lumen size. Most plaques therefore remain angiographically occult. Stenosis occurs when this compensatory mechanism fails.
12. Braunwald E. Unstable angina. An etiologic approach tomanagement. Circulation 1998;98:2219–22.
13. Ambrose J, Winters S, Stern A, et al . Angiographic
morphology and the pathogenesis of unstable angina. J Am Coll Cardiol 1985;5:609–16.
14. Mann J, Kaski J, Pereira W, et al . Histological patternsof atherosclerotic plaques in unstable angina patients varyaccording to clinical presentation. Heart 1998;80:19–22.
15. Chen L, Chester M, Redwood S, et al . Angiographicstenosis progression and coronary events in patients with“stabilised” unstable angina. Circulation 1995;91:2319–24.
16. Ridker P, Cushman M, Stampfer M. Inflammationaspirin and the risk of cardiovascular disease in apparentlyhealthy men. N Engl J Med 1997;336:973–9.
17. Libby P, Egan D, Skarlatos S. Roles of infectiousagents in atherosclerosis and restenosis: an assessment ofthe evidence and need for future research. Circulation 1997;96:4095–103.
18. Libby P, Ridker PM. Novel inflammatory markers ofcoronary risk, theory and practice. Circulation 1999;100:1148–50.
19. Witztum J. The oxidation hypothesis of atherosclerosis.
Lancet 1994;344:793–5.20. Aikawa M, Voglic SJ, Sugiyama S, et al . Dietary lipidlowering tissue factor expression in rabbit atheroma.Circulation 1999;100:1215–22.
Education in Heart
366