The Official Magazine of the Alzheimer’s Foundation of …...Alzheimer’s Foundation of America...
Transcript of The Official Magazine of the Alzheimer’s Foundation of …...Alzheimer’s Foundation of America...

Alzheimer’sTODAY
The Official Magazine of the Alzheimer’s Foundation of America
VOLUME 14, NUMBER 3
'69 Mets Supporting Teammates with Dementia
Amazin’ Bond

MISSION: TO PROVIDE SUPPORT, SERVICES AND EDUCATION TO INDIVIDUALS, FAMILIES
AND CAREGIVERS AFFECTED BY ALZHEIMER’S DISEASE AND RELATED DEMENTIAS NATIONWIDE,
AND FUND RESEARCH FOR BETTER TREATMENT AND A CURE.
FEATURES
The content of this magazine is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of a physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this magazine. The Alzheimer’s Foundation of America makes no representations as to the accuracy, completeness, suitability or validity of any of the content included in this magazine, which is provided on an “as is” basis. The Alzheimer’s Foundation of America does not recommend or endorse any specific tests, physicians, products, procedures, opinions or other information that may be mentioned in this magazine. Articles are provided for information purposes only and the views and opinions expressed in those articles are those of the respective authors and do not necessarily reflect those of the Alzheimer’s Foundation of America. Reliance on any information provided in this magazine is solely at your own risk.
The inclusion of advertisements in Alzheimer’s TODAY is not an endorsement of the advertiser or its products or services. The Alzheimer’s Foundation of America does not investigate advertisers’ claims and is not responsible for these claims.
All rights reserved. This publication may not be reproduced in whole or in part without permission from the Alzheimer’s Foundation of America.
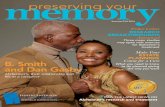
Cover image: Mets greats Tom Seaver (L) and Ed Kranepool (R). © Jerry Coli | Dreamstime.com
PAGE 4Hello Out There, I Have Dementia
PAGE 22What Families Should Know: Planning for Long-term Care
PAGE 19Simple Act, Potentially Big Impact
PAGE 6Amazin’ Bond: ’69 Miracle Mets Supporting Teammates with Dementia
PAGE 16What Alzheimer’s Taught Me: Teens Share Their Stories
CONTACT INFORMATIONAlzheimer’s Foundation of America322 Eighth Ave., 16th Fl.New York, NY 10001
National Toll-Free [email protected] and www.alzfdn.org
Alzheimer’s TODAY is published quarterly by AFA.
Volume 14, Number 3 • Alzheimer’s TODAY 1
PAGE 8Join the Movement: Opening UP Communication with Dance/Movement Therapy
Congratulations! Teens for Alzheimer’s Awareness Scholarship Essay Contest Winners
A Record-Breaking 36 Winners Received Nearly $35,000 in Scholarships!
A big THANK YOU to all our participants for sharing your stories.
Mark Your CalendarsFor students who will be high school seniors this fall 2019, the deadline to enter AFA’s 2020 Teens for Alzheimer’s Awareness Scholarship Essay Contest is Friday, January 17, 2020. Go to www.alzfdn.org for more information about applying.
$1000 WinnersAisho Ali, Columbus, OHChristopher Bi, McLean, VAJaden Carrier, Dayton Beach Shores, FLHunter Daniels, Clark Hills, SCAlexa Gallo, Newton Square, PACaitlin Gurley, Pensacola, FLLindsey Hicks, Spotsylvania, VAJulia Mazzucato, Tustin, CARyan McCue, Fort Lauderdale, FLMorgan Phillips, Hollenburg, KS Sabrina Piccirillo-Stosser, Ossining, NYLacey Sanguinito, Little Meadows, PALillian Segert, Grant Park, IL
$750 WinnersMason Cavalier, New Orleans, LAAndrea Gehling, Breda, IAAnna Gleason, Gross Point Park, MICaroline Howard, Harwich Port, MAAnnika Phillips, Portland, ORAshlee Phillips, Blakely, GAAmanda Porter, Ashburnham, MAMia Quinlan, Marion, MAVarsha Vedapudi, Tory, MI
$500 WinnersMonique Ades, Coarsegold, CAQuinn Collier, Brunswick, GAAshlyn Kelly, Dudley, MAXavier King, Pueblo, COEmma Marrs, Brentwood, TNJoseph McInvale, West Point, NYKaitlyn Pendergrast, Galesburg, ILEmily Pettesch, Hillsborough, NJMyka Savage, Chicago, ILGina Vitacco, Carpentersville, ILErica Wattenmaker, Southhampton, PA
Grand Prize Winner $5,000 Jason Sitt, Lynbrook, NY Second-Place Winner $2,500 Abigail Ransom, Ambler, PA Third-Place Winner $1,500 Corynne Emmerson, Salem, VA
Read their winning stories on pp. 16-17!
©2019 Alzheimer’s Foundation of AmericaVOLUME 14, NUMBER 3
Chairman of the Board Bert E. Brodsky Board of TrusteesGerald (Jerry) Angowitz, Esq.Barry Berg, CPALuisa EchevarriaSteve IsraelArthur Laitman, Esq.Edward D. Miller Associate Board MembersMatthew Didora, Esq.Judi Marcus President & Chief Executive OfficerCharles J. Fuschillo, Jr. Medical, Scientific & Memory Screening Advisory BoardJ. Wesson Ashford, M.D., Ph.D.Peter Bayley, Ph.D.Soo Borson, M.D.Herman Buschke, M.D.Donna Cohen, Ph.D.Jeffrey Cummings, M.D., Sc.D.Peter Davies, Ph.D.Margaret Dean, R.N., C.S.-B.C., N.P.-C., F.A.A.N.P.Sanford I. Finkel, M.D.Lori Frank, Ph.D.Lee Hyer, Ph.D.George Perry, Ph.D.Richard E. Powers, M.D.Frederick Schmitt, Ph.D.
PublisherAlzheimer’s Foundation of America EditorsChris SchneiderKaren Mazzotta DesignThe Monk Design Group

A MESSAGE FROM OUR PRESIDENT & CEO TEAL TAKE - EDITORIAL
2 Volume 14, Number 3 • Alzheimer’s TODAY Volume 14, Number 3 • Alzheimer’s TODAY 3
phot
o cr
edit:
©Li
ghtfi
eld
Stud
io P
rod
I Dre
amst
ime.
com
With every issue of Alzheimer’s TODAY, we bring you a community of people who have your back. We know helping someone live with dementia, or personally living with it yourself, isn’t easy.
We want to empower you every day to make the most of each moment with solutions you can use, a plan you can make, and a smile you can take. Inside this issue:
• Check out our cover story, “Amazin’ Bond” on p. 6. There’s an amazin’ feature about the 1969 Miracle Mets in honor of their 50th anniversary that brings to life their longstanding commitment to each other, especially now as two of them face dementia. So honored to share this photo with “Miracle Met” Bud Harrelson at Stew Leonard’s in East Meadow, NY (right).
• Don’t miss this year’s Teens for Alzheimer’s Awareness Scholarship Essay Contest winners on our opening page. Congratulations to our top three placing winners: Jason Sitt of Lynbrook, NY; Abigail Ransom of Ambler, PA; and Corynne Emmerson of Salem, VA. Their heartwarming stories are on pp. 16-17.
• Despite the hyperpartisan political environment we live in these days, I’m proud to tell you that hands crossed the aisle in the fight against Alzheimer’s disease. We were able to introduce legislation that would enable taxpayers to donate money to research and care through their annual income tax returns, thanks to the leadership of Rep. Tom Suozzi (D) and Rep. Peter King (R). Check out our Capitol Report update on p. 19 which describes the Alzheimer’s Research and Caregiving (ARC) Trust Fund and how you can help make it a reality.
• Meet Mike Oliver on p. 4, Birmingham News and AL.com/Advance Local reporter and human being extraordinaire. He shares his personal story of living with Lewy body dementia (LBD) and how you can connect better with someone who is living with a dementia.
• Bring dance and movement into the lives of persons with Alzheimer’s and dementia to connect and communicate. Go to p. 8 to learn how it works.
• And if you are unsure of how or when to move forward with long-term care for a loved one, Julian Gray, Certified Elder Law Attorney (CELA) and a member of the National Elder Law Foundation offers his suggestions on p. 22.
Interested in getting on our mailing list for Alzheimer’s TODAY? Go to our website at Alzfdn.org to the Media Center tab; then click on Alzheimer’s TODAY to sign up. You can sign up using the subscription card inside this issue, too.
Don’t forget we always love hearing from you. Send us feedback and story ideas to [email protected].
Take good care,
Charles J. Fuschillo, Jr. President & CEO Alzheimer’s Foundation of America
I f you’re reading this magazine, chances are pretty strong you know someone affected by Alzheimer’s disease. And by the time you are done reading it,
someone new will be diagnosed.
Despite numerous experimental cures and treatments reaching phase III of clinical trials, the fail rate is 99%. While a handful of FDA-approved medications can potentially slow the progression of the disease for a period of time, they cannot reverse the damage. Unless a cure or disease-modifying treatment is found, the Centers for Disease Control and Prevention (CDC) projects the number of Americans with the disease will nearly triple to 14 million by 2060. Alzheimer’s disease is currently ranked as the sixth leading cause of death in the United States, but recent estimates indicate that it may rank third, just behind heart disease and cancer, as a cause of death for older people, says the National Institute on Aging.
When it comes to Alzheimer’s, the status quo can never be acceptable. So while federal funding for Alzheimer’s research has reached historic levels—$2.34 billion in fiscal year 2019, finally reaching the annual dollar amount scientists say is needed to find a cure or disease modifying treatment by
2025, more absolutely needs to be done. Fortunately, there is continued movement forward.
New bipartisan legislation has been introduced in Congress to create an additional revenue source for Alzheimer’s research and caregiver support programs (you can read more details on p. 19). If enacted into law, taxpayers would be able to make voluntary contributions to a new Alzheimer’s Research and Caregiving Trust Fund by simply checking off a box on their federal income tax returns. An existing checkoff box on federal income tax returns for the Presidential Election Campaign Fund raised over $47 million from January 2018 to May 2019. If that’s what can be raised for political campaigns, imagine what could be raised for Alzheimer’s research and support services?
The article also tells how you can help build momentum for this proposal. It’s quick, easy and impactful. We hope you’ll take a minute to join the effort to get this bill passed and signed into law.
Alzheimer’s is relentless. We must, and will, ensure that efforts to help those affected by this disease are relentless, too.
Greater Need, Greater Response Needed

dementia symptoms appear later by definition than Lewy body dementia.
Alzheimer’s is linked to another kind of misfolding protein.
Not long after my first diagnosis of Parkinson’s, I told my boss.
Eventually, I told the newsroom in a meeting. For me, I didn’t want to sit on this secret. I can talk about it freely, answer questions and have incorporated it into my job as a journalist with support from my company: AL.com under the Advance Local organization umbrella.
I’ve written about living with the disease from various angles. I am the “poster child” of a successful annual fund-raising event, Mike Madness, a basketball tournament seeking to raise awareness and money for research.
I realize everybody has different thresholds for privacy and many may not want to talk about some-thing that can be overwhelmingly difficult.
It is important to know about the disease, whether it’s Alzheimer’s, Parkinson’s or Lewy body dementia. I’ve talked to readers who say how frustrating it can be because their loved one has been diagnosed but won’t accept
the diagnosis and refuses to talk about it.
My main caregiver or care partner, if you will, is Catherine, my wife. This illness of mine has hit her hard, but as a Presbyterian pastor and registered nurse and someone who loves me, she couldn’t be more qualified.
We talk about the future, the implications of early retirement, downsizing, and how to handle those times in the future when I may be confused or physically hurt from falling. We are together developing a mindset. Our biggest lifestyle change I made so far is to quit driving.
So what do you say to a person with dementia? As someone who has it, I say, don’t be afraid to ask anything. Think of open-ended questions that allow the person with dementia to answer. Sometimes I lose my train of thought and ramble a bit. I am thankful I can still write and provide a window into the world of someone living with dementia.
I don’t know how long I have with this level of cognition. I think of a big house with dozens of lighted windows; every day one of them turns off. I’m hoping, for metaphorical reasons, that I have lots of windows.
I believe even when we lose our words, we can still understand the world. So talk, ask questions, tell stories and look into our eyes, the window of the soul.
Mike Oliver is an award-winning journalist with 30 years in the business in AL, FL and CA. He writes about living with Lewy body dementia and other end-of-life issues.
MY STORY
Volume 14, Number 3 • Alzheimer’s TODAY 5
Mike with wife, Catherine.
Hello Out There, I Have Dementia
No. This is not how I introduce myself to people I meet and greet.
But with the awareness that this can be uncomfortable subject matter for some, I choose on a case-by-case basis what to say, if anything, about my disease.
Hi,
my name is Mike Oliver and I have a degenerative brain disease.
Since I was diagnosed with Lewy body dementia more than three years ago, I have had to recalibrate who I am in terms of the words used to describe one’s identity: Who are you?
For me it would be: husband, father, journalist, amateur basketball player, and 59-year-old male human.
Now, I add something quite significant to this thumbnail autobiography: person with dementia.
That’s one part of the resumé some folks want to keep quiet or even ignore or disbelieve. I described Lewy body disease
once: “Live like you are expecting the best, but be prepared to deal with the worst.” If you are in denial, you will not be prepared.
At first, I was diagnosed with Parkinson’s then Lewy body dementia, a common occurrence because the diseases are so similar. Both Parkinson’s and Lewy body involve what I call “rogue” proteins which are misfolded. The difference between the two diseases is that Lewy body attacks the cognitive function of the brain—words, math, judgment—in addition to the motor skills. People living with Parkinson’s also often develop dementia, but
MIKE’S TIPSn WHAT TO SAY: The most common reaction Mike gets when he tells people that one of his key symptoms is forgetfulness and losing things is: “I lose my stuff all the time.” “That’s fine to say, but it doesn’t really engage me or help,” says Mike. “A better response would be: ‘Oh no, are you coming up with any tricks to remember things?’” He would be delighted to talk about how Catherine is helping him take inventory of the things he needs to bring to work. They are also working on double-checking his phone (or his wallet) which he has left numerous times at restaurants.
n GET YOUR SUPPORT SYSTEM READIED: If you or a loved one have been diagnosed with dementia, be it Alzheimer’s, Parkinson’s, Lewy body or other types, Mike wants to encourage you to talk openly with close friends and family. “You are building the foundation for a support system that you will likely need to call on in the future,” he says.
n GET COUNSELING: “This is hard stuff,” says Mike. “Dementia can bring family systems together and it can blow them apart. Let a trained professional help you find the sunshine again.”
n GET FINANICAL HELP: “You’re going to need a good assessment of how much your expenses will be and how much income you will have. You’ll need to look at 401(k)s, pensions, Social Security, and disability options. Strongly consider seeking a professional advisor,” says Mike.
4 Volume 14, Number 3 • Alzheimer’s TODAY

COVER STORY had told him that he would no longer be traveling. So Shamsky decided to bring the celebration to Seaver’s Calistoga, CA, home. The reunion “idea” kicks off Shamsky’s book After the Miracle: The Lasting Brotherhood of the ’69 Mets, which he co-wrote with veteran sportswriter Erik Sherman, published this past spring.
Shamsky organized the group trip in 2017 with former teammates Harrelson, pitcher Jerry Koosman and outfielder Ron Swoboda. “It really could have been any combination of players,” Shamsky told AFA, but Harrelson was particularly important. With his Alzheimer’s and as a best friend to Seaver, Shamsky knew it would be “therapeutic” for both of them.
The actual meeting up with Seaver was never a “done deal” though. After five months of planning and coordination with the guys and their families, Shamsky came to the realization that their only chance to rendezvous with Seaver for their early golden jubilee reunion was going to be a single Saturday that might not happen.
Seaver’s wife, Nancy, had warned him that Tom wasn’t always up for visitors: “I think it’s a wonderful idea and will really be great for Tom—and Buddy, too—but just understand that some days are good and some days are not too good,” she told him. “Every day is different. It’s really a roll of the dice.”
Luckily, “somebody was watching over us,” said Shamsky. They were able to share eight or nine hours together. “We just had a glorious time.”
It was definitely a bit of a miracle to Shamsky who described filling the hours with a walk along the hills of Seaver’s three-and-a-half acre vineyard as he clipped and pruned, a drive into town for lunch and continuous banter and reminiscing about their baseball days: the clubhouse kid Jimmy, favorite Yogi Berra anecdotes, manager Gil Hodges not making the Baseball Hall of Fame and his special love for his wife.
During their talks, Seaver even shared the story behind why he left broadcasting years ago. His mother, during a phone call, had asked him what city he was in. “And you know what?” he said. “I didn’t remember! I couldn’t tell her. It was the Lyme disease, you know. That was another reason I knew it was time to move on.” The city was Pittsburgh.
That reunion was the just the beginning of the celebration. The official Mets 50th anniversary ceremony came to Citi Field this past June, an event-full weekend honoring the ’69 Miracle Mets. Fifteen players were able to attend, including the four who were at the California mini reunion, without Seaver, of course. The teammates reenacted the 1969 World Series parade, with players riding in vintage convertible cars, and received the keys to New York City. Citi Field’s address was renamed 41 Seaver Way.
“It’s hard to explain the adulation, and I know for Buddy [Harrelson] it was great,” said Shamsky, describing the Citi Field
events. “I had the honor to ride out with him in a golf cart. I just put my arm around him….I wanted to make sure he had a sense of how important he was to the team and how important that day was.”
About missing Seaver that weekend, Shamsky commented, “He was the star of the team. It was a shame that he wasn’t there, but
he was there in a form, as all the players are who are not around anymore. There was a sadness about that. But I’m happy that I got a chance to see the guys and glad they got a chance to see the love that is still around for everybody on that team.” In that sense, they are still making miracles.
And they’re not done.
“I think with the Seaver situation and with Buddy, it’s just natural that [Alzheimer’s and dementia] are going to come up; and whatever I can do on a personal level, I’m willing to do to help,” Shamsky said. “In some ways the fact that these two well-known people are involved in this kind of horrible situation I think it makes more awareness, and whatever we can do collectively as a team I’m sure we are going to do….These things hit home and so all of us feel close to this situation and whatever we can do, we will do. I promise you that.”
6 Volume 14, Number 3 • Alzheimer’s TODAY Volume 14, Number 3 • Alzheimer’s TODAY 7
The impossible dream came true in 1969. What was unfathomable only a few years earlier suddenly became reality. And 50 years later, it’s still celebrated
and revered. Not the moon landing (though it too certainly fits that criteria). Something far closer to home: The 1969 New York Mets winning the World Series.
A team that was born just seven years earlier—setting the modern-era, Major League Baseball record for most single season losses—rose up to complete one of the most improbable championship runs in sports history. In the midst of some of America’s most turbulent times, notably, the Vietnam War, their victory was a golden moment, a miracle, a blessing, an underdog triumph that continues to inspire to this day.
So it was no surprise that crowds formed lines out the doors at three Stew Leonard’s locations when the east coast supermarket chain hosted special events with seven of the ‘69 Mets this past spring. In celebration of their joint 50th anniversary, Stew Leonard, Jr., welcomed the magical players who brought wide smiles and signed memorabilia for fans, old and young.
But the baseball brothers were doing something much more with Leonard: They were also raising awareness about Alzheimer’s disease. Stew Leonard’s in-store Wishing Well accepted donations to fight Alzheimer’s for an entire month.
Mets teammates were honored to come together for these special occasions to create new memories, understanding too well that not all of their teammates could do the same.
“These memories are treasures for me,” said former outfielder Ron Swoboda at a Stew Leonard’s event. “…[Y]ou start hearing about your former teammates, some of them aren’t here anymore. And some of them are here, but their memories are fading because of Alzheimer’s and dementia of various sorts. For [Stew Leonard’s] to bring us here and to raise money and try to come up with some sort of a solution is incredible work.”
Some of the teammates Swoboda was referring to are Hall of Fame pitcher Tom Seaver, who did not attend the event, and his former road roommate and close friend, shortstop Bud Harrelson, who, fortunately, did. For many years, Seaver had lived with the effects of Lyme disease, which can cause fatigue and cognitive issues. Just this May, Seaver’s family announced he would no longer make public appearances due to his dementia diagnosis. Harrelson was already in the early stages of Alzheimer’s, and, luckily for his fans, continues to make public appearances.
Outfielder Art Shamsky, too, bemoaned the changes that were occurring for Seaver and Harrelson, and knew as the 50th anniversary of the 1969 World Series was approaching, no celebration would be complete without “Tom Terrific,” who
Amazin’ Bond1969 Miracle Mets Supporting Teammates with Dementia
’69 Miracle Mets at Stew Leonard’s in East Meadow, NY.
At the pre-50th anniversary reunion with Tom Seaver, eating lunch from L. to R., Buddy Harrelson, Jerry Koosman, Erik Sherman, Art Shamsky, Ron Swoboda, and Seaver.
phot
o co
urte
sy o
f Erik
She
rman
Col
lect
ion

For those of us who can walk to a train station, unpack a bag of groceries or do “The Macarena” at a wedding reception, movement is an automatic, easy response
to something we want or need to do. But to a person who is living with a cognitive impairment, movement can serve as their communication. That is the theory behind dance/movement therapy and why it can be so important to the quality of life for a person living with Alzheimer’s or other dementia.
“Dance/movement therapy gives individuals the opportunity to express their true selves, be who they are without judgement, and find that self-confidence that lives deep within,” says Jackie Gatto, MS, R-DMT, AFA’s Recreational Therapist and Registered Dance/Movement Therapist. “To witness the transition from living in a world of isolation into the world of socialization and self-expression is heartwarming.”
Gatto leads “Dance with Jackie,”“Movin’ & Groovin’” and other programs in AFA’s Education and Resource Center in New York City. She does not follow specific choreography, and the program looks different every session. Gatto often uses a variety of colorful props to encourage movement and engagement, including scarves, parachutes, and, one of her favorites, The Octaband®. The main activity goals are self-expression, socialization, body awareness and, of course, FUN!
AFA member Rhythm Break Cares, founded by Nathan Hescock, also uses the restorative power of music and ballroom dance to support older adults with a dementia. Rhythm Break Cares’ professionally trained ballroom dancers host AFA Teal Rooms at senior and memory centers.
Says Hescock, “We love going to the centers every week to dance with the seniors and have seen noticeable
improvements from week to week. We’ve even witnessed small miracles of wheelchair-bound seniors, who after a few months with us, gained just enough strength and courage to try standing and moving (with a smile!). This is our great joy to work toward and be a part of, to restore life. It is incredibly moving
to see that spark come back to people when we dance together. For a moment they can be who they were before Alzheimer’s.”
“When a person can no longer function as they once did, dance/movement therapy builds on what a person can still do,” says Donna Newman-Bluestein, M.Ed., BC-DMT, CMA, LMHC, a Board Certified Dance/Movement Therapist and creator of The
Octaband®. “We pay honor when we dance and move with people with dementia, when we
relate to them in an embodied way, when we attempt to understand their nonverbal communication. In our everyday lives, not a lot of attention is paid to this social-emotional environment, but people with diminishing cognitive abilities are dependent on this environment to feel safe. In fact, people with dementia can be quite expert at tuning into feelings. Our job, as caregivers, is to create loving, caring environments, and we do that with our
nonverbal communications through our bodies.” Newman-Bluestein was awarded an AFA Anne & Irving Brodsky Innovation Grant through the Marian Chace Foundation in 2010 for her groundbreaking work in this area.
While the functions of dance/movement therapy may look like all fun and games, it can be much more. It’s a form of evidence-based therapy that uses movement to connect the mind and body, while improving emotional, physical, and mental well-being. Under the umbrella of creative arts therapy, dance/movement therapy promotes healing through self-expression—and often lots of smiles.
FEATURE
Join the
8 Volume 14, Number 3 • Alzheimer’s TODAY Volume 14, Number 3 • Alzheimer’s TODAY 9
Movement:Opening UP Communication withDance/Movement Therapy
Gatto leading a session with The Octaband® at AFA’s Education and Resource Center in New York City.
Bringing Movement Home“Movement can and should be incorporated into the home setting every day,” says Gatto. “Whether movement is as small as batting eyelashes or as large as a jump in the air, moving the body in ways that feel good will help create a healthy quality of life.”
Keep walking. No matter what the level of capability, or what adaptive equipment is needed, a few steps every day can do a world of good. The simplest and most basic type of movement, walking is an excellent source of gentle exercise. At an individual’s own pace, walking allows for blood flow and healthy circulation throughout the body as well as cognitive stimulation especially if able to do it in different locations—even moving into a hallway or looking out a window will help. Walking alongside another person encourages needed socialization and can be used as motivation to keep going.
Try dancing. Whether in a chair, bed or standing, encouraging movement of the body to a rhythm or tune can be enjoyable and engaging. “Put on music that is irresistible. Then just move and be silly,” recommends Newman-Bluestein. Know the person and their likes, and find the music that moves them! Dance is a fun way to express yourself. It encourages body awareness, creates emotional connections and can help with balance and circulation.
Lifting weights, using resistance bands and fabric. Remember to always talk with a doctor regarding any use of props. If cleared, a light dumbbell (.5lb – 2lb) can be a great tool for gaining strength and endurance. If the individual you are working with has limitations in their hands, other objects can be used instead (e.g., weighted beanbags, wrist weights, balloons filled with dry beans). Another option are resistance bands, available in varying levels. For a more relaxed approach, use an old tie, ribbon, cloth or a t-shirt to encourage movement—play a gentle “tug of war.” Turn on fun, uplifting music to help with motivation.
Ball toss. Whether it’s a balloon, squishy ball or beach ball, tossing a ball back-and-forth is a great way to help with coordination and alertness. Writing jokes or questions on the ball can add a layer of cognitive fun into this game, too.
Rhythm Break Cares instructors Dariusz Horvath (front) and Dylan Cary (back) at a monthly Tea Dance Social in their Herald Square, NY, studio.

10 Volume 14, Number 3 • Alzheimer’s TODAY Volume 14, Number 3 • Alzheimer’s TODAY 11
phot
o cr
edit:
©To
a551
l | D
ream
stim
e.co
m
A s we all age, we are at a greater risk of falling and getting hurt. Falls are the second leading cause of accidental or unintentional injury deaths worldwide,
with adults over 65 years of age suffering the greatest number of fatal falls, according to the World Health Organization.
Falling can stem from a variety of circumstances involving medical conditions, medication, balance difficulties, visual-cognitive impairment, and environmental factors. Not only can falls cause serious injuries, they can negatively impact one’s sense of self. Preventing falls can be particularly challenging for someone living with Alzheimer’s disease or other dementia-related illnesses.
Here are five tips for caregivers to help reduce the risk of falls:
Be aware of the surroundings outside and inside the home.Make sure all pathways of the house are clear of clutter and other obstacles. Indoors, secure or remove all area rugs, ensure that all electrical cords are neatly kept and tucked away behind furniture and that everyday items such as food and personal care products are stored away neatly within reach. Outdoors, it is crucial to be aware of the daily weather conditions. Remove/limit the buildup of natural obstacles like snow in the winter or leaves in the fall.
Make sure that the home is easily accessible. Install handrails in areas such as stairways, bathrooms, and bedrooms, and ensure that they are securely attached. Mark
all rooms with signs to avoid wandering and confusion. Utilize nightlights throughout the house, so it is easier to see the surroundings in the dark. Minimize the glares that come from windows and mirrors to avoid direct light to the eyes.
Be mindful of the impact that medications can have.Some medications can cause dizziness, which increases the risk of falls. Always ask the individual’s doctor or pharmacist about prescription and non-prescription medication side effects. Take the time to educate yourself about what to expect.
Be aware of the individual and their personal needs. Keep the individual comfortable. For example, evaluate the feet for pain and always check to see that they are wearing comfortable and well-fit shoes with non-skid soles. Ensure the individual wears eyeglasses and hearing devices, if needed, as sensory issues can contribute to falls. Consult with a physical therapist about assistive devices such as walkers and canes.
Maintain a healthy lifestyle.A healthy diet can help build bone strength. Exercises, such as chair rises and tai chi, may help strengthen leg muscles and improve balance, minimizing falls. Don’t forget to consult with a physician about appropriate diet and exercise selections.
While these tips can be helpful, an individual with Alzheimer’s disease or other dementia-related illnesses can still be at risk of having a fall. If an individual falls and appears to be injured, contact emergency services immediately.
5 Tips to Prevent FallsMild cognitive impairment (MCI) is a disorder involving
problems with memory and other mental functions that are greater than normal age-related changes
but not as significant as the decline seen with a dementia. Symptoms are noticeable, and, in many cases, similar to those of a dementia-related illness.
What are some of the common signs of MCI?
• forgetting things more often
• frequently losing train of thought in a conversation
• difficulty remembering scheduled appointments and/or events
• challenges with navigating familiar locations or environments
• increased difficulty or anxiety with making decisions, planning or following instructions
What’s the difference between mild cognitive impairment and dementia?Unlike dementia, mild cognitive impairment does not interfere with the person’s daily life. Someone living with MCI will still be able to take part in many day-to-day activities. While dementia-related illnesses like Alzheimer’s are progressive brain disorders, meaning that symptoms worsen over time as the brain deteriorates, mild cognitive impairment symptoms can remain the same or even improve.
Some problems commonly associated with MCI may be caused by certain medications, cerebrovascular disease (which impacts blood vessels that supply the brain), and other factors—and may even be reversible. That’s why it’s crucial to be aware of the differences.
Some additional contributing factors to MCI include: • sleep apnea• stroke• fatigue• urinary tract infection (UTI)• thyroid imbalances • chemotherapy• depressed mood, anxiety and stress
Does MCI guarantee dementia?Individuals with mild cognitive impairment are at a greater risk of developing a dementia-related illness, but it’s important to note that not everyone who has MCI will develop dementia.
Lifestyle changes and choices commonly suggested to reduce the risk of developing a dementia-related illness, or help slow the progression of the disease, can also help lessen the chances of developing mild cognitive impairment. These include a good diet, proper sleep, regular mental and physical exercise, and social interaction.
MCI is not a normal part of aging, and it does impact one’s ability to think. Consult your doctor if you notice changes in thinking and memory to determine a plan for care.
Have questions about mild cognitive impairment?
Call AFA’s National Toll-Free Helpline at 866-232-8484 and speak with a licensed social worker.
phot
o cr
edit:
Nor
iko
Coop
er |
Drea
mst
ime.
com
What to Know About Mild Cognitive Impairment

12 Volume 14, Number 3 • Alzheimer’s TODAY Volume 14, Number 3 • Alzheimer’s TODAY 13
RECIPE FOR YOUR HEALTH
INGREDIENTS 4 tablespoons extra-virgin olive oil
3 tablespoons red wine vinegar
Juice from half a lemon
1½ cups cooked chickpeas, drained and rinsed
5 ounces skipjack* or chunk light tuna, packed in water, drained
1 large cucumber, diced
½ cup radishes, thinly sliced (optional)
½ medium red onion, sliced
1.5 pounds tomatoes, sliced
1/3 cup pitted Kalamata olives or capers
¼ teaspoon sea salt (optional)
Freshly ground black pepper to taste
½ bunch fresh basil leaves, chopped
3 ounces mixed baby greens of your choice
*skipjack (chunk light) tuna is low in mercury compared to albacore (chunk white) tuna
DIRECTIONSIn a large salad bowl, whisk together olive oil, vinegar and lemon. Add chickpeas, tuna, cucumber, radishes, onion, cherry tomatoes, olives or capers, salt and pepper. Stir to combine and use a fork to flake the tuna. Set aside.
Just before serving, add basil, and mix well. Allow to stand for 15 minutes for flavors to blend and serve over mixed baby greens. Serve with hearty whole-wheat sourdough bread or top with homemade croutons.
Serves 4
This healthy Mediterranean salad can be used as a template for one-bowl dishes by varying seasonal veggies and lean protein. For vegetarian alternatives swap out the tuna for diced tofu, sliced hard-boiled egg or fresh mozzarella cheese. One-bowl salads offer an all-in-one balanced meal and are a casual option for easy entertaining.
MEDITERRANEAN SALAD WITH TUNA, TOMATOES AND CHICKPEAS
Self-care is crucial.Prioritizing the well-being of the person you are caring for while sacrificing your own is noble but can be detrimental. Failing to care for yourself increases risk of caregiver burnout, which compromises your ability to provide quality care and negatively impacts the person for whom you are caring. Self-care is critically important. Find ways to reduce stress: Working out and breathing exercises are helpful. Make time for yourself, too. Even short breaks go a long way to help recharge your mind and your body.
Ask for help.Support is vital. Family, friends, community and professional caregivers can all lend a helping hand in different ways, but only if you ask. Don’t be hesitant to ask someone to assist with errands, help with transportation to medical appointments or spend time with the person you are caring for, so that you have a break. Distance isn’t always an obstacle either. Family, friends and people in your community can assist with coordinating appointments and making phone calls—all you need to do is ask! Of course, AFA’s Helpline (866-232-8484) is here for you, too.
Prepare as much as possible.Caring for someone with dementia often involves a complex array of long-term medical, legal and financial issues. Deal with these decisions as early as possible, with strong consideration for personal wishes, to help reduce stress later. Addressing these matters early also gives the individual the opportunity to have a more active role in their care and the decision-making process.
Build your skills.Key skills for any care partner include communication, understanding safety considerations, recognizing behaviors as a form of communication, and managing activities of daily living. Get to know doctors and other care team members. Ask questions, express concerns and be involved.
Be flexible.While you can’t control every situation, you can work to better manage your reactions. While it may seem impossible at times, try to have a positive and accepting attitude; be flexible and understand the need to adapt. Take things one day at a time and handle challenges as best you can. Don’t feel that you have to deal with everything at once.
Connect with others. Hugs, gentle touch and compassion help you and the person you are caring for feel connected and loved. Kindness, humor and creativity are essential. Manage your expectations and remain patient. Find your support network and surround yourself with positive connections, both old and new!
Build empathy.Building empathy and maintaining compassion is essential for both you and the person you care for. Try to comprehend what it is to have this type of illness. Putting yourself in their shoes, while also recognizing your own losses, can help place things in perspective and alleviate stress.
Feeling stressed? We’re here to help. Contact AFA’s Helpline at 866-232-8484 to speak with a licensed social worker.
Recipe and photo by Layne Lieberman, MS, RD, CDN, culinary nutritionist and award-winning author of Beyond the Mediterranean Diet: European Secrets of the Super-Healthy. For more information and recipes, visit www.WorldRD.com
Caring for a family member with dementia may involve a lot of “juggling” to manage the demands
of caregiving as well as your personal responsibilities. Feeling stress is natural, but if left unchecked, continuous stress can negatively impact your physical and mental health and hinder your ability to provide proper care.
Here are some tips to help manage the stress associated with caregiving:
7 Ways to Manage Caregiver Stress
phot
o cr
edit:
©Al
eksa
ndra
Suz
i | D
ream
stim
e.co
m

14 Volume 14, Number 3 • Alzheimer’s TODAY Volume 14, Number 3 • Alzheimer’s TODAY 15
dementiaAlzheimer’s disease and other forms of dementia
a form of dementiasymptoms of dementia
a person/people living with dementia
changed behavior(s)expressions of unmet need
psychological symptoms of dementia
change in life expectationsstressful
dementing illnessdemented
senile dementiasicknesssufferer
patient or resident (when used outside of medical field)
challengingattention seeker
aggressor
hopelesstragic
Word choices matter when talking about dementia. Knowing which words are appropriate and inappropriate when talking to someone about Alzheimer’s or other dementia-related illnesses is crucial. Using words with negative meaning,
even unintentionally, can profoundly impact the person with dementia as well as their family and friends.
DOs and DON’Ts of Discussing Dementia
WHEN TALKING ABOUT DEMENTIA WHEN TALKING ABOUT DEMENTIA
WHEN DISCUSSING BEHAVIORS AS FORMS OF COMMUNICATION
WHEN DISCUSSING BEHAVIORS AS FORMS OF COMMUNICATION
WHEN DESCRIBING THE IMPACT OF DEMENTIA WHEN DESCRIBING THE IMPACT OF DEMENTIA
USE THIS TYPE OF LANGUAGE AVOID THIS TYPE OF LANGUAGE
We’re Always Here to Help!¡Siempre Estamos Aquí
Para Ayudar!Spanish-language resources are available
on AFA’s website, www.alzfdn.org.(Click on Español in the lower right-hand corner of the website.)
LEARN ABOUT Alzheimer’s disease signs and symptoms
dementia caregiving memory screening
healthy aging
Spanish-language brochures on dementia care are also available by calling our licensed social workers on our National Toll-Free Helpline, 866-232-8484.
Many people with late-stage dementia forget how to swallow properly, which can lead to weight loss, malnutrition and aspiration pneumonia (when a person inhales food, stomach acid or saliva into the lungs). Remember that the trachea, which leads to the lungs, is in front of the esophagus, which leads to the stomach. To swallow, the trachea needs to close properly. When we consider that just swallowing uses some 50 pairs of muscles, some voluntary and some involuntary, you can begin to understand how complicated it is. A speech pathologist can evaluate these problems, help initiate swallowing studies at bedside and using x-rays, and may find safer food and liquid solutions (see p. 24 for more information about how speech pathologists help).
“When someone has a late-state dementia, it’s important to allow them to eat what they are willing to eat,” says Dr. Weintraub.
A preference for sweets is often maintained. So you may find yourself using a lot of pudding, but try any of their known favorite foods as well as new foods—tastes will definitely change.
What about straws? “You’ll notice straws are everywhere in hospital settings, but for a person with swallowing difficulty, straws are not your friend,” says Dr. Weintraub. “Sucking from a straw shoots droplets all over your mouth that are hard to collect, making it easy to aspirate liquid.”
Maintaining a person’s independence and preferences for as long as possible is important to quality of life. So adjusting food textures and liquid consistencies and providing feeding gadgets are important steps for caregivers to take on this journey. Some changes that may be recommended by a speech therapist or doctor follow.
Eating & Drinking in Later-Stage DementiaA s a person living with a dementia and Alzheimer’s progresses
through its many phases, the loss of various skills, unfortunately, is predictable. Eating and drinking can become challenging and
maintaining proper nutrition a major concern. “Feeding problems afflict 86% of people with an advanced dementia,” says Nancy Weintraub, MD, Clinical Professor of Medicine, UCLA, and Director, UCLA Geriatric Medicine Fellowship. “The ability to feed oneself is usually the last independent skill that a person with dementia loses.”
Adapted from an AFA CARE CONNECTION educational webinar series. To learn more about upcoming opportunities, go to the Caregiving Resources tab on our website, www.alzfdn.org.
FOOD TEXTURES
Puree (smooth-pudding consistency) Pudding, yogurt, cottage cheese, cream soups, fruits/vegetables, pureed and thickened
Ground (may need gravy or sauces to make moist) Canned tuna, soft ground meats and vegetables
Soft foods (that “stay together”) Macaroni and cheese, scrambled eggs, pancakes with jam or syrup, soft casseroles, meatloaf, egg/tuna/chicken salad with mayo
Complex Pasta, soft cheeses, cold cereal in milk, chopped or steamed vegetables (green beans, carrots)
LIQUID CONSISTENCIES Honey-thick (i.e., the consistency of honey) Nectar-thick (i.e., the consistency of pear/apricot/peach nectar or tomato soup)
FEEDING GADGETS
Weighted utensils Good for a person with tremors; keeps food from falling as easily.
Bowls with lips & rubber bottoms Keeps food/plate in place when pressed or leaned against.
Universal cuff A wrist cuff, with an attached utensil, for someone who can no longer use their hand.
Long-handled baby spoons Ideal for a person who needs to be fed a small amount of food; discourages rushing.
FOOD TEXTURES HARDER TO SWALLOW SAFELY
Stringy or hard to eat foods Celery, fresh fruit, corn, crunchy peanut butter, brown/wild rice
Flaky foods Toast, crackers, popcorn, nuts
Foods that melt Ice cream, milkshakes, chocolate, sherbet, gelatin (Jell-O)
Sticky or bulky foods White bread, mashed potatoes, potato salad, refried beans
phot
o cr
edit:
@Ch
erne
tska
ya I
Drea
mst
ime.
com

Volume 14, Number 3 • Alzheimer’s TODAY 1716 Volume 14, Number 3 • Alzheimer’s TODAY
T here’s a misconception that Alzheimer’s disease and other dementia-related illnesses only impact older individuals. In reality, they affect people of all ages,
including teens and children, who can sometimes be just as involved in caregiving as adults.
Each year, AFA’s Teens for Alzheimer’s Awareness Scholarship Essay Contest gives high school seniors an outlet to share their stories about how Alzheimer’s has impacted their lives, with the chance to earn money for college. Nearly 3,000 students entered our 2019 competition, sharing their personal experiences to raise awareness, with 36 winners receiving nearly $35,000 in scholarships, the largest single-year total since the program’s inception.
Jason Sitt of Lynbrook, NY, our grand prize winner and recipient of our $5,000 scholarship, shared memories of his grandfather, who is living with Alzheimer’s. Jason described his grandfather as a loving family man with a strong work ethic who immigrated to the United States from China. Jason fondly remembers his grandfather proudly teaching him about his Chinese heritage, encouraging him to do well in school, taking him on walks in the park to feed fish in the pond, and cooking family dinners every Saturday.
When Jason’s grandfather began to exhibit the symptoms of Alzheimer’s disease, he had a positive outlook. Despite the
impact of the disease, including several incidents in which his grandfather wandered miles away from safety, Jason embraced a “silver lining” in his grandfather’s diagnosis. It allowed Jason to “treasure his presence and recognize the simple gifts he has given [him].”
“Maybe I’m not sad because Grandpa isn’t completely gone; I have found him within myself—his persistence, his culture, his legacy. Yes, I will miss Grandpa’s cooking, and I will miss those Saturdays at the dinner table with all the family. But, when I look into the peaceful surface of the pond, I see my reflection; and in my own reflection, I see Grandpa and he’s smiling,” says Jason in his essay.
The experience also inspired Jason to get involved in scientific research. Last summer, he was a researcher at Columbia University, where he conducted projects that take steps in developing treatments to halt the progression of Alzheimer’s. In the fall, Jason will be attending the University of Virginia, where he has plans to become a science educator and bring light to the disease, as well as share his experience with others.
Second-place winner Abigail Ransom of Ambler, PA, who received the $2,500 scholarship, described a different way Alzheimer’s changed her life while working at a retirement home. Although Alzheimer’s did not impact anyone in her immediate family, Abigail’s experiences were still life-changing.
What Alzheimer’s Taught MeTeens Share Their Stories
Grand prize winner Jason Sitt
at high school graduation with his
grandparents.
After beginning work at the Spring House Estates retirement home, Abigail instantly developed relationships with the residents living with dementia-related illnesses. She enjoyed listening to their stories, hearing about their pasts, developing more empathy and appreciation as each day went by.
“I knew that the residents still had the ability to feel and love,” she wrote. “I would want the people that were being paid to take care of me to take a few extra moments to show me patience and compassion. I would want them to have empathy towards me. And most of all, I would want them to understand my struggles. After all, I would not be able to express them myself.”
These experiences inspired her to enroll in the biology program at the Eberly College of Science at Pennsylvania State University. Following her undergraduate stint, she plans to go to medical school to become a psychiatrist.
Corynne Emmerson of Salem, VA, who was the third-place winner and recipient of a $1,500 scholarship, had a similar life-changing experience while volunteering at an assisted living facility near her home.
The summer before her junior year of high school, Corynne was searching for something to fill her life with more passion. After being introduced to the Joseph C. Thomas Assisted Living Center, she found the change in her life that she was looking for.
“The Joseph C. Thomas Center has my heart,” she wrote, adding that the memory care residents are her favorite. “Even though their minds can’t always keep up with their bodies, their hearts still do. There is so much love coming from these people and sitting and talking to them always puts me in a good mood.”
Corynne has been touched by all of her residents’ stories and formed very strong bonds with each of them. She even brings her youth group and her friends from home to meet and spend time with them. Through her high school’s Pathway Project, she also set up students as pen pals with some of the residents.
“It’s hard to watch people progress through the stages before my eyes, but that doesn’t scare me away. It motivates me to love harder,” she wrote, “I want to help those affected by diseases like Alzheimer’s stay connected to others as long as possible and live a life worth living.”
This fall, Corynne will be attending Virginia Tech, where she plans to learn more about aging, so she can better serve individuals and raise awareness. Her experiences inspired her pursuit of a career in the geriatrics field and fueled her desire to make an everlasting impact on those affected by Alzheimer’s and other dementia-related illnesses.
Jason, Abigail and Corynne’s experiences with Alzheimer’s disease have changed them forever. All will likely go on to continue to impact the lives of others as well.
Interested in reading these three essays in their entirety and learning more about AFA’s Teens for Alzheimer’s Awareness Scholarship Essay Contest? Visit our website at Alzfdn.org and go to the “Teen Scholarship Essay Contest” tab located on the top menu bar!
Abigail Ransom, second-place winner.
Corynne Emmerson, third-place winner.

ASK AN AFA SOCIAL WORKER
T here’s never a “right” time to decide that your mother should no longer live at home with the person she trusts the most, in the environment where she feels the most
comfortable. However, there may come a point when you are noticing that it is becoming increasingly difficult to provide good care for mom, as well as yourself.
Two things to think about to help you decide: burnout (yours) and socialization (hers).
Caring for your mother can be a lot of work. Making sure she is eating and swallowing properly, ensuring that she is getting around her home safely and dressed properly is akin to a full-time job. Working two jobs with no break can breed exhaustion and can impact the care that you are providing. Having professional staff who are required to take a break allows the space for you to support your mother as her daughter, restoring that relationship. You will have a chance to rest and be a pair of fresh eyes to help guide the care team to best support her.
The second thing to think about is your mother’s socialization. For individuals who have Alzheimer’s, socialization is important because it provides a sense of connectedness to others and the outside world and can have a positive impact on the quality of her life.
Here are some suggestions to guide your decision on transitioning your mother’s care from home to a facility:
Talk to your mother. Have conversations about care and course of care early, and, if possible, as the disease progresses. Have a good understanding of how this illness can progress and the care needs that might arise, including placement in a different
setting. Engage with a care team, perhaps a doctor or social worker, to gain a sense of options and what may be best for mom. The goal here is quality of life and meaningful living.
Work with an interdisciplinary team next (i.e., social worker, geriatrician, case manager, financial advisor, and/or elder law attorney) to explore options available. Care can be expensive and it is important to know what options may be available for you (see “What Families Should Know: Long-term Care” on p. 22 of this issue).
Be flexible. The symptoms of Alzheimer’s can ebb and flow like the tide, so we need to be flexible about plans as this disease progresses. It’s perfectly okay to go back to the drawing board a few times. Work with your care team to assess when a higher level of care is needed.
After gathering all the facts, it’s time to make a decision. Remember, there’s no “perfect” answer or “perfect” time. Your plan will be right for you and your mother because it will be yours. Seek support groups or AFA’s National Toll-Free Helpline (866-232-8484) for ongoing assistance. These decisions may not seem easy, but when we focus on the goal of quality of life for you and mom, you’ll be able to find some clarity.
Acanthus Fairley, LCSW, answers your question.
QuestionI am the primary caregiver for my mother, who has Alzheimer’s disease, and have been so for the past three years. My father and my siblings have passed away and
I am the only family member left to care for her. She is getting increasingly dependent on me for support with eating, transferring her, and dressing. The only break I have is when I go to work during the day because I moved in with her. When do I know it’s time to start looking for a nursing home for my mother?
Volume 14, Number 3 • Alzheimer’s TODAY 1918 Volume 14, Number 3 • Alzheimer’s TODAY
Contact our social workers seven days a week through AFA’s National Toll-Free Helpline at 866-232-8484 or through our website, www.alzfdn.org.
Here’s how you can help! Contact your federal representatives and ask for their support!
To find your Congressperson Visit www.house.gov or call the Capitol switchboard at 202-224-3121 to connect with your Congressperson and urge them to support HR 3453, the legislation creating the ARC Trust Fund (or thank them if they are already a bill sponsor).
To find your Senators Visit www.senate.gov or call the Capitol switchboard at 202-224-3121 to connect with the two Senators from your state and urge them to introduce companion legislation to HR 3453 in the Senate.
W ashington has prioritized progress in the fight against Alzheimer’s over the last several years. Democrats and Republicans are working together
on another step forward to further increase federal funding to fight Alzheimer’s through a very simple act: letting people check off a box on their federal income tax returns.
Alzheimer’s Research and Caregiving (ARC) Trust Fund Under the proposed legislation, taxpayers could make a voluntary contribution to a new Alzheimer’s Research and Caregiving (ARC) Trust Fund through a checkoff on their income tax form. The amount of the voluntary contribution will be deducted from the taxpayer’s refund or added to their tax liability. Of the funds raised, half will be provided to the National Institutes of Health (NIH) for clinical research into a cure or modifying treatment for Alzheimer’s disease; half will be used by the Administration for Community Living (ACL) to fund dementia caregiver services and supports.
Working together with AFA, Rep. Tom Suozzi (D-NY3), Rep. Peter King (R-NY2), Rep. Maxine Waters (D-CA43), Rep. Christopher Smith (R-NJ4) and Rep. Brian Fitzpatrick (R-PA1) introduced the legislation.
It is important to note that the funds collected for the ARC Trust Fund would supplement, not supplant, existing federal appropriations to NIH and ACL to fight Alzheimer’s. Washington provided record-level funding for Alzheimer’s research in fiscal year 2019 ($2.34 billion), finally topping the $2 billion a year minimum scientists say is required to meet the National Plan to Address Alzheimer’s Disease goal of finding
a cure or disease-modifying treatment by 2025. But the need is steep: The failure rate for experimental cures or treatments reaching phase III clinical trials is 99%.
Thirty states have similar laws allowing taxpayers to make voluntary contributions to different causes through their state income tax returns. Since 1976, taxpayers can voluntarily contribute to the Presidential Election Campaign Fund through their income taxes to help finance political campaigns. From
January 2018 through May 2019, that fund received over $47 million in voluntary contributions, according to the Federal Election Commission (FEC).
With more than 154 million individual federal tax returns filed in 2018 alone, this simple checkoff could potentially have a big impact in delivering additional dollars for Alzheimer’s disease research and caregiver support.
“This is a responsibility we all share and something that folks on both sides of the aisle should get behind,” said Rep. Tom Suozzi (pictured above, center) announcing the bipartisan legislation with Rep. Peter King (above, right) and AFA President and CEO Charles J. Fuschillo, Jr. (above, left) on June 24.
CAPITOL REPORT
Proposed Income Tax Checkoff Would Increase Federal Funding to Fight Alzheimer’s
Simple Act, Potentially Big Impact

Once-daily NAMZARIC [nam-ZAIR-ick] is a prescription medicine approved to treat moderate to severe Alzheimer’s disease in patients who are taking donepezil HCl 10 mg, the active ingredient in Aricept®.
There is no evidence that NAMZARIC prevents or slows the underlying disease process in patients with Alzheimer’s disease.
IMPORTANT RISK INFORMATION NAMZARIC should not be taken by anyone who: · has an allergy to memantine HCl, donepezil HCl, medicines that
contain piperidines, or any of the ingredients in NAMZARIC.
Before taking NAMZARIC, tell the doctor about all of the patient’s medical conditions, including: · heart problems including an irregular, slow, or fast heartbeat· asthma or lung problems· seizures· stomach ulcers· bladder, kidney, or liver problems· any surgical, dental, or other medical procedures scheduled
when anesthesia may be usedTell the doctor about all the medicines the patient takes, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Please see Brief Summary of Patient Information for NAMZARIC on adjacent page.
What are the possible side effects of NAMZARIC?NAMZARIC may cause serious side effects, including: · muscle problems in patients given anesthesia· slow heartbeat and fainting. This happens more often in people with
heart problems. Call the doctor right away if the patient faints while taking NAMZARIC.
· more stomach acid. This raises the chance of ulcers and bleeding especially when taking NAMZARIC. The risk is higher for patients who have had ulcers, or take aspirin or other NSAIDs.
· nausea and vomiting· diffi culty passing urine· seizures· worsening of lung problems in people with asthma or other
lung diseaseThe most common side effects of memantine HCl include: headache, diarrhea, and dizziness.The most common side effects of donepezil HCl include: diarrhea, not wanting to eat (anorexia), and bruising. These are not all the possible side effects of NAMZARIC.You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.FDA.gov/medwatch or call 1.800.FDA.1088.
NAMZARIC.COM | Allergan® and its design are trademarks of Allergan, Inc. | NAMZARIC® and its design are trademarks of Merz Pharma GmbH & Co. KGaA. | © 2017 Allergan. All rights reserved. | NMZ111784 | 11/17
Aricept® is a trademark used by Eisai Inc. under license from Eisai R&D Management Co., Ltd.
IMPROVE COGNITION, also known as mental function
IMPROVE OVERALL FUNCTION
SLOW DOWN the worsening of SYMPTOMS for a while
30
*Restrictions apply.
Take a photo of this ad and ask their healthcare provider about NAMZARIC today.
NAMZARIC works in 2 ways. Data has shown that NAMZARIC may:
Visit NAMZARIC.com and download a free 30-day trial offer.*
I amFor my loved one with moderate Alzheimer’s
and I am asking about
I amstepping up®
Once-daily NAMZARIC [nam-ZAIR-ick] is a prescription medicine approved to treat moderate to severe Alzheimer’s disease in patients who are taking donepezil HCl 10 mg, the active ingredient in Aricept®.
There is no evidence that NAMZARIC prevents or slows the underlying disease process in patients with Alzheimer’s disease.
IMPORTANT RISK INFORMATION NAMZARIC should not be taken by anyone who: · has an allergy to memantine HCl, donepezil HCl, medicines that
contain piperidines, or any of the ingredients in NAMZARIC.
Before taking NAMZARIC, tell the doctor about all of the patient’s medical conditions, including: · heart problems including an irregular, slow, or fast heartbeat· asthma or lung problems· seizures· stomach ulcers· bladder, kidney, or liver problems· any surgical, dental, or other medical procedures scheduled
when anesthesia may be usedTell the doctor about all the medicines the patient takes, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Please see Brief Summary of Patient Information for NAMZARIC on adjacent page.
What are the possible side effects of NAMZARIC?NAMZARIC may cause serious side effects, including: · muscle problems in patients given anesthesia· slow heartbeat and fainting. This happens more often in people with
heart problems. Call the doctor right away if the patient faints while taking NAMZARIC.
· more stomach acid. This raises the chance of ulcers and bleeding especially when taking NAMZARIC. The risk is higher for patients who have had ulcers, or take aspirin or other NSAIDs.
· nausea and vomiting· diffi culty passing urine· seizures· worsening of lung problems in people with asthma or other
lung diseaseThe most common side effects of memantine HCl include: headache, diarrhea, and dizziness.The most common side effects of donepezil HCl include: diarrhea, not wanting to eat (anorexia), and bruising. These are not all the possible side effects of NAMZARIC.You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.FDA.gov/medwatch or call 1.800.FDA.1088.
NAMZARIC.COM | Allergan® and its design are trademarks of Allergan, Inc. | NAMZARIC® and its design are trademarks of Merz Pharma GmbH & Co. KGaA. | © 2017 Allergan. All rights reserved. | NMZ111784 | 11/17
Aricept® is a trademark used by Eisai Inc. under license from Eisai R&D Management Co., Ltd.
IMPROVE COGNITION, also known as mental function
IMPROVE OVERALL FUNCTION
SLOW DOWN the worsening of SYMPTOMS for a while
30
*Restrictions apply.
Take a photo of this ad and ask their healthcare provider about NAMZARIC today.
NAMZARIC works in 2 ways. Data has shown that NAMZARIC may:
Visit NAMZARIC.com and download a free 30-day trial offer.*
I amFor my loved one with moderate Alzheimer’s
and I am asking about
I amstepping up®
Brief Summary of Important Risk Information NAMZARIC [nam-ZAIR-ick] (memantine hydrochloride and donepezil hydrochloride) extended-release capsules
This information does not take the place of talking to your doctor about your medical condition or your treatment.
What is NAMZARIC? NAMZARIC is a prescription medicine used to treat patients with moderate to severe Alzheimer’s disease. NAMZARIC contains 2 medicines, memantine hydrochloride (HCl), an NMDA receptor antagonist, and donepezil HCl, an acetylcholinesterase inhibitor. NAMZARIC is for people who are taking donepezil HCl 10 mg.
Who should not take NAMZARIC? Do not take NAMZARIC if you are allergic to memantine HCl, donepezil HCl, medicines that contain piperidines, or any of the ingredients in NAMZARIC.
What should I tell my doctor before taking NAMZARIC? Before taking NAMZARIC, tell your doctor about all of your past and present medical conditions, including if you have: • heart problems including an irregular, slow, or fast heartbeat • asthma or lung problems • seizures • stomach ulcers • liver, kidney, or bladder problems • surgical, dental, or other medical procedures scheduled
and anesthesia may be used
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
What are the possible side effects of NAMZARIC? NAMZARIC may cause serious side effects, including: • muscle problems if you need anesthesia • slow heartbeat and fainting. This happens more often in
people with heart problems. Call the doctor right away if the patient faints while taking NAMZARIC
• more stomach acid. This raises the chance of ulcers and bleeding especially when taking NAMZARIC. The risk is higher for patients who had ulcers, or take aspirin or other NSAIDs
• nausea and vomiting • difficulty passing urine • seizures • worsening of lung problems in people with asthma or
other lung disease
The most common side effects of memantine HCl include: headache, diarrhea, and dizziness. The most common side effects of donepezil HCl include: diarrhea, not wanting to eat (anorexia), and bruising. These are not all the possible side effects of NAMZARIC.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
How should I take NAMZARIC? • Take NAMZARIC exactly as your doctor tells you to take it • Do not change your dose or stop taking NAMZARIC without
talking to your doctor • Take NAMZARIC by mouth 1 time each evening before
going to bed, with or without food • NAMZARIC capsules may be opened and sprinkled on
applesauce before swallowing. Sprinkle all of the medicine in the capsule on the applesauce. Do not divide the dose
• If you do not open and sprinkle NAMZARIC capsules on applesauce, the NAMZARIC capsules must be swallowed whole. Do not divide, chew, or crush NAMZARIC capsules
• If you miss a dose take NAMZARIC at your next scheduled dose. Do not take 2 doses of NAMZARIC at the same time
• Do not use any NAMZARIC capsules that are damaged or show signs of tampering
What if I take more NAMZARIC capsules than I should? If you take too much NAMZARIC, call Poison Control at 1-800-222-1222, or go to the nearest hospital emergency room right away.
What other information should I be aware of? • The use of NAMZARIC in children is not recommended • You should not breast-feed during treatment with
NAMZARIC • Tell your healthcare provider if you are pregnant or
planning to become pregnant
Need more information?The risk information provided here is not complete. It summarizes the most important information about NAMZARIC. If you would like more information, talk to your doctor.
For the FDA approved product labeling or for more information go to NAMZARIC.com or call 1-800-678-1605.
Distributed by:Allergan USA, Inc.Irvine, CA 92612
Allergan® and its design are trademarks of Allergan, Inc.
NAMZARIC® and its design are trademarks of Merz Pharma GmbH & Co. KGaA.© 2016 Allergan. All rights reserved.
7/10 mg, 14/10 mg, 21/10 mg, 28/10 mg
(memantine HCl and donepezil HCl) extended-release capsules
NMZ92529 09/16

22 Volume 14, Number 3 • Alzheimer’s TODAY Volume 14, Number 3 • Alzheimer’s TODAY 23
As the saying goes, “We can do this the easy way or the hard way.” Thousands of families across the United States deal with long-term neurodegenerative diseases
on a daily basis. Alzheimer’s and dementia-related illness are particularly hard to address because the course of the diseases are different for each individual.
As a Certified Elder Law Attorney (CELA), I see the struggles that a person with Alzheimer’s and dementia faces along with the supporting cast of family, friends and other caregivers. Seniors, who rely on Medicare to cover most of their medical expenses, are often surprised to learn that it does not cover long-term care in a skilled nursing facility for more than a few weeks—and that’s only while making progress towards a recovery. “How are we going to pay for this?” is the question that keeps families up at night. The good news is, we can figure it out together and the outcome will be positive.
HOW ARE WE GOING TO PAY FOR THIS?Planning for long-term care as early as possible is vital to providing your loved one with the best quality of life. I always recommend starting with a Certified Elder Law Attorney (CELA).
These attorneys have passed a rigorous exam and are required to update their certifications on a regular basis, which is needed to keep up with the ever-changing rules and laws. The National Elder Law Foundation (NELF) has a referral service that can help you locate a CELA in your area. Pre-planning can be broken down into three main areas: medical, financial and legal. All three disciplines should be considered and integrated into a comprehensive plan.
MEDICALMost families have some type of medical coverage. This could be through an employer health insurance plan or retirees using Medicare or even Medicaid coverage. However, this coverage is meant to cover acute-care scenarios or catastrophic medical events, not a long-term disability. A long-term disability routinely involves the need for ongoing daily care for assistance with activities of daily living.
People who need ongoing custodial care must personally secure and pay for long-term disability services. While there is an entire industry dedicated to offering long-term care insurance, the overwhelming majority of us simply do not
purchase this coverage for one reason or another. When the average cost of this long-term care can be anywhere from $5,000 – $10,000 per month, you quickly realize that the next part of the equation—the financial element—becomes paramount to obtaining quality care.
FINANCIALOver the years, people accumulate a variety of assets. These commonly include a home, business interests, vehicles, bank accounts, investments, IRAs, life insurance, and many other types of valuable things. A good exercise is to prepare a list of all of your assets, how each asset is titled (i.e., who has legal ownership) and if a death beneficiary is named. These assets change over time and as a person’s life evolves, the title and beneficiary designations may need to change, too.
The high cost of long-term care drives the majority of Americans to seek Medicaid coverage. While Medicaid has become an important benefit that drives the middle class to obtain long-term care services at home or in a facility, Medicaid has stringent financial guidelines that can vary drastically from state to state. Determine your family’s total-asset value picture to see how it would be affected by long-term care costs as well as what steps can be taken either in advance, or at the eleventh hour, to conserve your assets. A family may or may not be able to secure Medicaid coverage depending on your total asset value.
LEGALThis is where it all comes together. The continuum of care can progress from healthy senior to long-term disability in a short or long timeframe. Your lawyer plays a critical role in assessing your family’s medical needs while integrating your financial picture into a sustainable care plan that may last for several years. Some of the planning involves preparing legal documents: powers of attorney, wills and trusts that are specific to long-term care planning. A simple estate plan comprised of a basic will is wholly inadequate to address the challenges of long-term care.
An initial assessment of a family’s situation early on can make an exponential difference in your ability to obtain quality care, and, more importantly, make choices about how and where that care is delivered, before those choices are lost by the simple passage of time.
All of us realize that as we age long-term care challenges will come, and the cost of care will only increase over time. Addressing these issues in advance provides the best chance for a more successful and acceptable outcome.
Julian E. Gray is a Certified Elder Law Attorney (CELA) and a member of the National Elder Law Foundation (NELF). He is the owner of Julian Gray Associates practicing in Pittsburgh, PA.
What Families Should Know: Planning for Long-term Care
phot
o cr
edit:
©TP
ikse
l | D
ream
stim
e.co
m
phot
o cr
edit:
©Zi
mm
ytw
s I D
ream
stim
e.co
m
Advance Directives 101What are Advance Directives?Legal documents stating your medical wishes, including treatment choices and life-prolonging procedures.
What is a Healthcare Agent?A healthcare agent is someone designated to make medical decisions for you when you are unable to make decisions for yourself.
How to Start Advance Directives• Choose a health care agent.• Request forms in a doctor’s office, hospital, law office, state or
local office for the aging, senior center or nursing home.• When completing each form, note some may require a
witness or notary present.• Give copies to your family, doctor, lawyer, and health care agent.• Keep the original form in a safe and accessible place. Let
your family and friends know where your forms are kept.
Types of Advance DirectivesHealth Care Proxy or Medical Power of Attorney: You appoint a trusted person who will make medical decisions on your behalf when/if you become incapacitated or unconscious.
Living Will: You provide the conditions for when you want life-sustaining treatment provided, withheld or withdrawn.
Do Not Resuscitate (DNR): Your preference to not receive cardiopulmonary resuscitation (CPR) when your heart stops or you stop breathing.
Do Not Intubate (DNI): Your preference to not have a breathing tube used in the event of breathing difficulty or respiratory arrest.
POLST (Physician Orders for Life-Sustaining Treatment): A request for specific medical treatments that you want during a medical emergency. This is called different things in different states (e.g., MOLST, MOST, POST).

24 Volume 14, Number 3 • Alzheimer’s TODAY
Speech-language pathologists (SLPs) play a central role in the assessment, diagnosis, and treatment of individuals with dementia and
collaborate with many other disciplines in caring for them. Individuals with dementia may develop aphasia, the inability to communicate effectively, or dysphagia, a swallowing disorder.
Signs of AphasiaA person with aphasia may:
• Speak in short or incomplete sentences that do not make sense
• Substitute one word for another or one sound for another
• Not understand other people’s conversation• Speak unrecognizable words
• Write sentences that do not make sense
Signs of Dysphagia*A person with dysphagia may:
• Cough during or right after eating or drinking• Need more effort and time to chew and swallow
• Have food or liquid leaking from the mouth• Experience weight loss and dehydration
• Regurgitate food and liquids
*It is crucial to recognize swallowing disorders because they can lead
to rapid weight loss, which further results in serious health issues.
Speech-language pathologists (SLPs) can provide specific types of support to manage these symptoms and ensure the best possible quality of life. Referral and collaboration between members of the care team, particularly during the early stages of assessment and treatment planning, are essential to help ensure quality care for individuals affected by communication and cognitive disorders.
Here are some ways SLPs can assist:
Provide strategies to preserve communication for as long as possible.Aiding the individual’s abilities to communicate and verbalize is essential. By implementing different speaking strategies, SLPs can preserve a person’s language, making it easier for them to converse and communicate with others, ultimately resulting in a happier life.
Speech pathologists can also teach families ways to communicate using different tools, such as a communication board, and refer the individual to other professionals to rule out other conditions and facilitate access to comprehensive services.
Assess and diagnose swallowing disorders associated with dementia.Once a person is assessed and diagnosed, the SLP will know the best treatments and therapies to further aid the person in recovering lost functions.
Ensure safe swallowing.SLPs will go through different exercises with a person to practice safe swallowing. Repetitively performing these exercises helps form safe eating and drinking habits. Muscles typically targeted during these exercises include the cheeks, tongue, and lips. For example, tongue-strengthening exercises can be beneficial toward moving food around the mouth and safely transferring it to the pharynx.
Los patólogos del habla y el lenguaje juegan un papel central en la evaluación, diagnóstico y tratamiento de personas con demencia y colaboran con muchas otras
disciplinas en el cuidado de ellos. Las personas con demencia pueden desarrollar afasia, la incapacidad para comunicarse de manera efectiva, o disfagia, trastorno de la deglución.
Signos de AfasiaUna persona con afasia puede:
• Hablar en oraciones cortas o incompletasque no tienen sentido
• Sustituir una palabra por otra oun sonido para otro
• No entiendo la conversación de otras personas• Hablar palabras irreconocibles
• Escribir oraciones que no tienen sentido
Signos de Disfagia*Una persona con disfagia puede:
• Tener tos durante o justo después de comer o beber• Necesita más esfuerzo y tiempo para masticar y tragar
• Se le escapa comida o líquido de la boca• Experimente la pérdida de peso y la deshidratación.
• Regurgitar alimentos y líquidos.
* Es crucial reconocer los trastornos de la deglución porque pueden
provocar a la rápida pérdida de peso, lo que resulta en graves
problemas de salud.
Los patólogos del habla y lenguaje pueden proporcionar información y apoyo específico para manejar estos síntomas y garantizar la mejor calidad de vida posible. Referencia y colaboración entre miembros del equipo de atención, particularmente durante las primeras etapas de evaluación y planificación del tratamiento, son esenciales para ayudar a garantizar una atención de calidad para las personas afectado por trastornos de la comunicación y cognitivos.
Aquí hay algunas formas en que los patólogos del habla y lenguaje pueden ayudar:
Proporcionar estrategias para preservar comunicación por el mayor tiempo posible. Ayudar a las habilidades del individuo para comunicarse y verbalizar es esencial. Al implementar diferentes estrategias de comunícacion, los patólogos del habla pueden preservar el lenguaje de una persona, haciendolo más fácil para conversar y comunicarse con otros, dando como resultado una vida más feliz. Los patólogos del habla también pueden enseñar a las familias formas para comunicarse utilizando diferentes herramientas, como un tablero de comunicación, y referir al individuo a otro profesionales para descartar otras condiciones y facilitar acceso a servicios integrales.
Evaluar y diagnosticar los trastornos de la deglución asociado con la demencia.Cuando una persona es evaluada y diagnosticada, los patólogos del habla sabrá los mejores tratamientos y terapias para ayudar aún más a la persona en recuperación.
Asegure una deglución segura.Los patólogos del habla pasarán por diferentes ejercicios con una persona para practicar la deglución segura. Realizar repetitivamente estos los ejercicios ayudan a formar hábitos seguros de alimentación y bebida. Músculos típicamente dirigido durante estos ejercicios incluyen las mejillas, lengua y labios. Por ejemplo, ejercicios para fortalecer la lengua puede ser beneficioso para mover alimentos alrededor de la boca y transfiriéndolo de manera segura a la faringe.
Have questions about how a speech-language pathologist can help someone with a dementia-related illness? Call AFA’s Helpline at 866-232-8484 and speak with a licensed social worker.
¿Tiene preguntas sobre cómo un patólogo de lenguaje puede ayudar a alguien con una enfermedad relacionada con la demencia? Llame a la línea de ayuda de AFA al 866-232-8484 y hable con un trabajador social licenciado.
How Speech Pathologists Can Help Someone with Alzheimer’s
Cómo los Patólogos del Lenguaje Pueden Ayudar a Alguien con Alzheimer’sph
oto
cred
it: ©
Sha
o-ch
un W
ang
| Dre
amst
ime.
com
phot
o cr
edit:
© S
hao-
chun
Wan
g | D
ream
stim
e.co
m
Volume 14, Number 3 • Alzheimer’s TODAY 25

322 Eighth Avenue, 16th Fl. New York, NY 10001
Call AFA’s National Toll-Free Helpline 866-232-8484www.alzfdn.org
IF YOU HAVE QUESTIONS, WE’RE HERE TO HELP.
Connect with our licensed social workers and a community
who cares.