The Lymphoid System / and Breathing
-
Upload
arun-kumar -
Category
Documents
-
view
42 -
download
0
description
Transcript of The Lymphoid System / and Breathing
Chest (Thoracic) Breathing: Effects, Tests and SolutionsChest (or thoracic) breathing is very common in modern people. More than 50% of adults have predominantly chest breathing at rest. More than 90% of sick people have upper chest breathing with increased minute ventilation, respiratory rates, and minute volume (i.e., automatic deep breathing at rest or taking too much air per one breath). Chest breathing causes three fundamental health effects that promote chronic diseases and lead to low body oxygen levels.This is due to the misbelieve that taking deep breath helps body to not only get more oxygen but makes one healthy. Let us see what happens when we breathe through chest.1. Chest breathing reduces blood oxygenationThe textbook, Respiratory Physiology (West, 2000), suggests that the lower 10% of the lungs transports more than 40 ml of oxygen per minute, while the upper 10% of the lungs transports less than 6 ml of oxygen per minute. Hence, the lower parts of the lungs are about 6-7 times more effective in oxygen transport than the top of the lungs due to richer blood supply mostly caused by gravity.During thoracic breathing, lower layers of the lungs, which are most valuable in oxygen transport, get much less, if any, fresh air (less oxygen supply). This causes reduced oxygenation of arterial blood in the lungs and can lead to so called "ventilation-perfusion" mismatch (as in COPD or emphysema). Normal breathing is diaphragmatic and slow, allowing homogeneous inflation of both lungs with fresh air, similar to what happens in the cylinder of a car engine due to the movement of the piston. Hence, during diaphragmatic breathing, all alveoli are homogeneously stretched vertically and get fresh air supply with higher O2 concentration for superior arterial blood oxygenation. In contrast, chest breathing creates problems with blood oxygenation. This leads to reduced cell oxygenation: the driving force of all chronic diseases.2. Chest breathing causes lymphatic stagnationDr. Shields, in his study, "Lymph, lymph glands, and homeostasis" (Shields, 1992) reported that diaphragmatic breathing stimulates the cleansing work of the lymph system by creating a negative pressure pulling the lymph through the lymph system. This increases the rate of elimination of toxins from visceral organs by about 15 times. Why is this so?The lymph system, unlike the cardiovascular system with the heart, has no pump. Lymph nodes are located in parts of the human body that get naturally compressed (squeezing) due to movements of body parts. for example, lymph nodes are located around the neck, above arm pits and groin area. Hence, when we move, stretch or turn the head, arms and legs, these lymph nodes get mechanical stimulation to push the lymph through valves. This is how the lymphatic system works. However, the lymph nodes connected to the stomach, kidneys, liver, pancreas, spleen, large and small colons, and other vital organs are located just under the diaphragm - over 60% of all lymph nodes in total! Hence, nature expects us to use the diaphragm in order to remove waste products from these vital organs all the time - literally with each breath, 24/7. Hence, another problem with thoracic or chest breathing is stagnation in the lymph system and accumulation of waste products in vital organs located under the diaphragm.3. Thoracic breathing means hyperventilation and low oxygen levels in cellsPeople who are chest breathers virtually always have deep breathing (large breaths) at rest or sleep and suffer from hyperventilation (breathing more than the norm). When we breathe more air, we get less oxygen in body cells. In fact, the slower your automatic breathing pattern at rest (down to only 3 breaths/min), the larger the amount of oxygen delivered to cells.Keep in mind that, while healthy normal breathing is abdominal or diaphragmatic. It is very small in amount (only 500 ml of air per one breath at rest) so that healthy people usually do not feel their breath.Diaphragmatic breathing 24/7 is absolutely necessary for nearly maximum oxygenation of the arterial blood (98-99%) and efficient lymphatic drainage of abdominal organs (up to 60% of all lymph nodes are located just under the diaphragm). Bear in mind that ideal or healthy automatic breathing at rest is very small in amount, but mainly abdominal. Once a person starts taking breathe through lungs he gets a habit of it and then it is very hard to get rid of it. Here are some methods of diaphragmatic breathing exercises and techniques to get rid of thoracic breathing habit.Abdominal (Diaphragmatic) Breathing Techniques and Instructions How to test your own breathing techniqueHow to check one's predominant automatic breathing technique? Do you usually breathe using the belly and diaphragm or chest at rest?Self-test or simple breathing exercise. Put one hand on your stomach (or abdomen) and the other one on your upper chest (see the picture on the right). Relax completely so that your breathing dynamic has little changes. (We want to know more about your usual unconscious breathing.) Pay attention to your breathing for about 20-30 seconds. Take 2-3 very slow but deep breaths to feel your breathing in more detail. Now you know about your usual breathing technique. In order to be certain, you can ask other people to observe how you breathe when you do not pay attention to your breathing (e.g., during sleep, while reading, studying, etc.).
Diaphragmatic breathing exercises and techniquesHere are three abdominal breathing exercises to test and develop belly breathing. Exercise 1. Diaphragmatic breathing exercise to check your ability to move the diaphragmDiaphragmatic breathing exercise 1: Check your ability to move the diaphragm.Put your hands on your body as in the picture above. Try to push out your lower hand (which is on the belly button or navel) with your abdominal muscles. Can you breathe using your belly only so that your rib cage and upper hand do not move?Warning. It is vital for your health, abdominal breathing, good blood oxygenation, and respiratory and GI health to have a straight spine 24/7. Correct posture encourages abdominal breathing, while slouching prevents belly breathing. Exercise 2. Abdominal respiratory exercises with booksTake 2-3 medium weight books or one large phone book and lie down on your back with the books on your tummy. Focus on your breathing and change the way you breathe so that1) you can lift the books up about 2-3 cm (1 inch) with each inhalation and then relax to exhale (the books will go down);2) your rib cage does not expand during inhalations.Repeat this abdominal breathing exercise for about 3-5 minutes before your main breathing exercises to reconnect your conscious brain with the diaphragm. You can practice this exercise for some days until you are sure that diaphragmatic breathing is the usual way to breathe during the breathing sessions.For some people with persistently tense diaphragms and big fatty belly, who in addition have problems with slouching and constipation, magnesium can be an additional assisting factor. (Lack of magnesium leads to spasm and tension in body muscles.) If the diaphragm is still not the main muscle for your automatic breathing, and/or you have doubts about your ability to keep your chest relaxed during breathing exercises, apply this ultimate solution.
Exercise 3. Diaphragmatic breathing technique with a beltYou can use a strong belt to restrict your rib cage and force the diaphragm to be the main breathing muscle using the following technique. Put a belt around your lower ribs (in the middle of the trunk) and buckle it tightly so that you cannot take a deep inhalation using your rib cage or chest. Now for slow deep inhalations your body needs to use your tummy (or abdomen). Try it. While leaving the belt in place for some minutes or even hours, you can acquire diaphragmatic breathing and corresponding sensations. This breathing retraining process will be faster, if you focus your attention on your breathing and try to practice Buteyko reduced breathing with very light air hunger (taking small inhalations using your diaphragm and then immediately relaxing it). The focus of attention makes nervous links between your conscious mind and the diaphragm reinforced so that you can regain control of this muscle. When you pay attention to your breathing, be careful not to hyperventilate. Breathe slowly and remain relaxed so that even if your inhalations deepen, your CO2 will not lessen.Important note. The diets of modern people are low in magnesium, which is a known relaxant of smooth muscles, the diaphragm included. The normal daily requirement for Mg is about 400-500 mg. Typical symptoms of magnesium deficiency include: a tendency to slouch (indicating muscular tension), predisposition to constipation (muscles of the bowel also get into a state of spasm; hence "Milk of magnesia" or magnesium oxide is a popular and safe remedy for constipation) and tense diaphragm causing chest breathing 24/7. Try taking a Mg supplement (about 400-500 mg daily plus calcium to maintain balance) for 3 days and monitor your symptoms and any effects on your posture, breathing mechanics and CP. You need to restore a light and easy automatic breathing pattern or normalize your breathing in order to have abdominal breathing 24/7. What are the most effective abdominal breathing techniques? Hatha yoga and the Buteyko breathing technique help to prevent chest breathing. There are even more effective ways. Advanced diaphragmatic breathing exercises for unblocking the diaphragm The easiest way, however, to increase the CP and release or unblock the diaphragm 24/7 is to use breathing devices, such as the Frolov breathing device and the Amazing DIY breathing deice. If one has problems with abdominal breathing when using these devices, it is smart to use the belt technique for breathwork. After a few days of such practice, most people can easily involve diaphragm for breathwork.
Let us see all in more detail, why modern people do not have diaphragmatic breathing Modern people breathe about 2 times more air than the medical norm. Hyperventilation causes alveolar hypocapnia (CO2 deficiency), which reduces blood flow and oxygenation of the diaphragm muscle, while arterial hypocapnia makes smooth and skeletal muscles tense, the diaphragm included. If you were to take a close look at some old movies, you would hardly see any chest breathing at all. This is because people in the past had only 4-5 L/min for minute ventilation at rest (modern numbers are about 12 L/min for normal subjects). Hyperventilation makes modern people oxygen deficient (see instructions for the body oxygen test below) and this makes them chest breathers. Abdominal Breathing vs. Chest Breathing and Body Oxygen ContentBody Oxygen ContentAutomatic breathing at rest: diaphragmatic or chest?
1-10 sVirtually always chest
11-20 sChest in over 90% of people
21-30 sMostly chest
31-40 sMostly belly
over 41 sVirtually always belly
As we see from this Table, diaphragmatic breathing usually becomes the norm (24/7), when the morning body oxygen level (CP) is over 30 s. It is logical then that people in the past (about 100 years ago or more) had abdominal breathing 24/7 because they had more than 40 s for the body oxygen test. Since relatively healthy people have only about 20-25 s CP these days, most of them are chest breathers. The abdominal exercises, methods, and techniques are useful to prevent problems with chest breathing and achieve higher body oxygen level (CP) sooner. The more you practice them, the faster you get there. For better understanding let us see in more detail how can it be achieved by simple change in breathing style. Firstly let us understand LymphoId System.
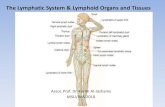
The Lymphoid SystemThe lymphoid system is the part of the immune system comprising a network of conduits called lymphatic vessels that carry a clear fluid called lymph (from Latin lympha "water) unidirectionally toward the heart. Lymphoid tissue is found in many organs, particularly the lymph nodes, and in the lymphoid follicles associated with the digestive system such as the tonsils. The system also includes all the structures dedicated to the circulation and production of lymphocytes, which includes the spleen, thymus, bone marrow and the lymphoid tissue associated with the digestive system.The blood does not directly come in contact with the parenchymal cells and tissues in the body, but constituents of the blood first exit the micro-vascular exchange blood vessels to become interstitial fluid, which comes into contact with the parenchymal cells of the body. Lymph is the fluid that is formed when interstitial fluid enters the initial lymphatic vessels of the lymphatic system. The lymph is then moved along the lymphatic vessel network by either intrinsic contractions of the lymphatic passages or by extrinsic compression of the lymphatic vessels via external tissue forces (e.g. the contractions of skeletal muscles).Functions of Lymphoid System The lymphoid system has multiple interrelated functions. it is responsible for the removal of interstitial fluid from tissues it absorbs and transports fatty acids and fats as chyle from the circulatory system it transports white blood cells to and from the lymph nodes into the bones The lymph transports antigen-presenting cells (APCs), such as dendritic cells, to the lymph nodes where an immune response is stimulated.Lymphatic tissue is a specialized connective tissue - reticular connective, that contains large quantities of lymphocytes.Clinical significanceThe study of lymphatic drainage of various organs is important in diagnosis, prognosis, and treatment of cancer. The lymphatic system, because of its physical proximity to many tissues of the body, is responsible for carrying cancerous cells between the various parts of the body in a process called metastasis. The intervening lymph nodes can trap the cancer cells. If they are not successful in destroying the cancer cells the nodes may become sites of secondary tumors.OrganizationThe lymphoid system can be broadly divided into the conducting system and the lymphoid tissue. The conducting system carries the lymph and consists of tubular vessels that include the lymph capillaries, the lymph vessels, and the right and left thoracic ducts. The lymphoid tissue is primarily involved in immune responses and consists of lymphocytes and other white blood cells enmeshed in connective tissue through which the lymph passes. Regions of the lymphoid tissue that are densely packed with lymphocytes are known as lymphoid follicles. Lymphoid tissue can either be structurally well organized as lymph nodes or may consist of loosely organized lymphoid follicles known as the mucosa-associated lymphoid tissue (MALT)Lymphoid tissueLymphoid tissue associated with the lymphatic system is concerned with immune functions in defending the body against the infections and spread of tumors. It consists of connective tissue with various types of white blood cells enmeshed in it, most numerous being the lymphocytes.The lymphoid tissue may be primary, secondary, or tertiary depending upon the stage of lymphocyte development and maturation it is involved in. (The tertiary lymphoid tissue typically contains far fewer lymphocytes, and assumes an immune role only when challenged with antigens that result in inflammation. It achieves this by importing the lymphocytes from blood and lymph.)Primary lymphoid organsThe central or primary lymphoid organs generate lymphocytes from immature progenitor cells.The thymus and the bone marrow constitute the primary lymphoid tissues involved in the production and early selection of lymphocytes.Secondary lymphoid organsSecondary or peripheral lymphoid organs maintain mature naive lymphocytes and initiate an adaptive immune response. The peripheral lymphoid organs are the sites of lymphocyte activation by antigen. Activation leads to clonal expansion and affinity maturation. Mature lymphocytes recirculate between the blood and the peripheral lymphoid organs until they encounter their specific antigen.Secondary lymphoid tissue provides the environment for the foreign or altered native molecules (antigens) to interact with the lymphocytes. It is exemplified by the lymph nodes, and the lymphoid follicles in tonsils, Peyer's patches, spleen, adenoids, skin, etc. that are associated with the mucosa-associated lymphoid tissue (MALT).Lymph nodesA lymph node showing afferent and efferent lymphatic vesselsA lymph node is an organized collection of lymphoid tissue, through which the lymph passes on its way to returning to the blood. Lymph nodes are located at intervals along the lymphatic system. Several afferent lymph vessels bring in lymph, which percolates through the substance of the lymph node, and is drained out by an efferent lymph vessel.The substance of a lymph node consists of lymphoid follicles in the outer portion called the "cortex", which contains the lymphoid follicles, and an inner portion called "medulla", which is surrounded by the cortex on all sides except for a portion known as the "hilum". The hilum presents as a depression on the surface of the lymph node, which makes the otherwise spherical or ovoid lymph node bean-shaped. The efferent lymph vessel directly emerges from the lymph node here. The arteries and veins supplying the lymph node with blood enter and exit through the hilum.Lymph follicles are a dense collection of lymphocytes, the number, size and configuration of which change in accordance with the functional state of the lymph node. For example, the follicles expand significantly upon encountering a foreign antigen. The selection of B cells occurs in the germinal center of the lymph nodes.Lymph nodes are particularly numerous in the mediastinum in the chest, neck, pelvis, axilla (armpit), inguinal (groin) region, and in association with the blood vessels of the intestines.LymphaticsTubular vessels transport back lymph to the blood ultimately replacing the volume lost from the blood during the formation of the interstitial fluid. These channels are the lymphatic channels or simply called lymphatics.Function of the fatty acid transport systemLymph vessels called lacteals are present in the lining of the gastrointestinal tract, predominantly in the small intestine. While most other nutrients absorbed by the small intestine are passed on to the portal venous system to drain via the portal vein into the liver for processing, fats (lipids) are passed on to the lymphatic system to be transported to the blood circulation via the thoracic duct. (There are exceptions, for example medium-chain triglycerides (MCTs) are fatty acid esters of glycerol that passively diffuse from the GI tract to the portal system.) The enriched lymph originating in the lymphatics of the small intestine is called chyle. As the blood circulates, fluid leaks out into the body tissues. This fluid is important because it carries food to the cells and waste back to the bloodstream. The nutrients that are released to the circulatory system are processed by the liver, having passed through the systemic circulation. The lymph system is a one-way system, transporting interstitial fluid back to blood.Diseases of the lymphatic systemLymphedema is the swelling caused by the accumulation of lymph fluid, which may occur if the lymphatic system is damaged or has malformations. It usually affects the limbs, though face, neck and abdomen may also be affected.Some common causes of swollen lymph nodes include infections, infectious mononucleosis, and cancer, e.g. Hodgkin's and non-Hodgkin lymphoma, and metastasis of cancerous cells via the lymphatic system. In elephantiasis, infection of the lymphatic vessels cause a thickening of the skin and enlargement of underlying tissues, especially in the legs and genitals. It is most commonly caused by a parasitic disease known as lymphatic filariasis. Lymphangiosarcoma is a malignant soft tissue tumor, whereas lymphangioma is a benign tumor occurring frequently in association with Turner syndrome. Lymphangioleiomyomatosis is a benign tumor of the smooth muscles of the lymphatics that occurs in the lungs.Development of lymphatic tissueLymphatic tissues begin to develop by the end of the fifth week of embryonic development. Lymphatic vessels develop from lymph sacs that arise from developing veins, which are derived from mesoderm.The first lymph sacs to appear are the paired jugular lymph sacs at the junction of the internal jugular and subclavian veins. From the jugular lymph sacs, lymphatic capillary plexuses spread to the thorax, upper limbs, neck and head. Some of the plexuses enlarge and form lymphatic vessels in their respective regions. Each jugular lymph sac retains at least one connection with its jugular vein, the left one developing into the superior portion of the thoracic duct.The next lymph sac to appear is the unpaired retroperitoneal lymph sac at the root of the mesentery of the intestine. It develops from the primitive vena cava and mesonephric veins. Capillary plexuses and lymphatic vessels spread from the retroperitoneal lymph sac to the abdominal viscera and diaphragm. The sac establishes connections with the cisterna chyli but loses its connections with neighboring veins.The last of the lymph sacs, the paired posterior lymph sacs, develop from the iliac veins. The posterior lymph sacs produce capillary plexuses and lymphatic vessels of the abdominal wall, pelvic region, and lower limbs. The posterior lymph sacs join the cisterna chyli and lose their connections with adjacent veins.With the exception of the anterior part of the sac from which the cisterna chyli develops, all lymph sacs become invaded by mesenchymal cells and are converted into groups of lymph nodes.The spleen develops from mesenchymal cells between layers of the dorsal mesentery of the stomach. The thymus arises as an outgrowth of the third pharyngeal pouch.Lymphatico-Venous CommunicationsPresent research has found cues about a lymphatico-venous communication. In mammals, lymphatico-venous communications other than those at the base of the neck are not easy to demonstrate, but described in some experiments.The specialists observed that the pulmonary complications following lymphangiography (a test which utilizes X ray technology, along with the injection of a contrast agent, to view lymphatic circulation and lymph nodes for diagnostic purposes) are more often severe in patients with lymphatic obstruction. In these cases, the contrast medium is thought to reach the vascular system via lymphovenous communications with shunt the material directly into the venous stream, bypassing those lymph nodes distal to the communications, Because less contrast agent is absorbed in lymph nodes, a greater portion of the injected volume passes into the vascular system. Since pulmonary complications are related to the amount of medium reaching the lungs area, the early recognition of lymphovenous communications is a great significance to the lymphangiographer. Another "hint" in proving a lymph-vein communication is offered by a Robert F Dunn experiment. The passage of radioactively tagged tracers, injected at elevated pressure, through the lymph node-venous communications coincides with the increased pressures of injection and subsequent nodal palpation in dogs. The passage of iodinated I 125 serum albumen (ISA) indicates that direct lymph node-venous communications are present, whereas passage of nucleated erythrocytes requires a communication structure the size of a capillary or larger. Moreover, the evidence suggest that in mammals under normal conditions, mostly of the lymph is returned to the blood stream through the lymphatico-venous communications at the base of the neck. When the thoracic duct-venous communication is blocked, however, the resultant raised intralymphatic pressure will usually cause other normal non-functioning communications to open and thereby allow the return of lymph to the blood stream.HistoryHippocrates was one of the first persons to mention the lymphatic system in 5th century BC. In his work "On Joints," he briefly mentioned the lymph nodes in one sentence. Rufus of Ephesus, a Roman physician, identified the axillary, inguinal and mesenteric lymph nodes as well as the thymus during the 1st to 2nd century AD. The first mention of lymphatic vessels was in 3rd century BC by Herophilos, a Greek anatomist living in Alexandria, who incorrectly concluded that the "absorptive veins of the lymphatics", by which he meant the lacteals (lymph vessels of the intestines), drained into the hepatic portal veins, and thus into the liver. Findings of Ruphus and Herophilos findings were further propagated by the Greek physician Galen, who described the lacteals and mesenteric lymph nodes which he observed in his dissection of apes and pigs in the 2nd century AD.Until the 17th century, ideas of Galen were most prevalent. Accordingly, it was believed that the blood was produced by the liver from chyle contaminated with ailments by the intestine and stomach, to which various spirits were added by other organs, and that this blood was consumed by all the organs of the body. This theory required that the blood be consumed and produced many times over. His ideas had remained unchallenged until the 17th century, and even then were defended by some physicians.In the mid 16th century Gabriele Falloppio (discoverer of the fallopian tubes) described what are now known as the lacteals as "coursing over the intestines full of yellow matter." In about 1563 Bartolomeo Eustachi, a professor of anatomy, described the thoracic duct in horses as vena alba thoracis. The next breakthrough came when in 1622 a physician, Gaspare Aselli, identified lymphatic vessels of the intestines in dogs and termed them venae alba et lacteae, which is now known as simply the lacteals. The lacteals were termed the fourth kind of vessels (the other three being the artery, vein and nerve, which was then believed to be a type of vessel), and disproved Galen's assertion that chyle was carried by the veins. But, he still believed that the lacteals carried the chyle to the liver (as taught by Galen). He also identified the thoracic duct but failed to notice its connection with the lacteals. This connection was established by Jean Pecquet in 1651, who found a white fluid mixing with blood in a dog's heart. He suspected that fluid to be chyle as its flow increased when abdominal pressure was applied. He traced this fluid to the thoracic duct, which he then followed to a chyle-filled sac he called the chyli receptaculum, which is now known as the cisternae chyli; further investigations led him to find that lacteals' contents enter the venous system via the thoracic duct. Thus, it was proven convincingly that the lacteals did not terminate in the liver, thus disproving Galen's second idea: that the chyle flowed to the liver. Johann Veslingius drew the earliest sketches of the lacteals in humans in 1647. The idea that blood recirculates through the body rather than being produced anew by the liver and the heart was first accepted as a result of works of William Harveya work he published in 1628. In 1652, Olaus Rudbeck (16301702), a Swede, discovered certain transparent vessels in the liver that contained clear fluid (and not white), and thus named them hepatico-aqueous vessels. He also learned that they emptied into the thoracic duct, and that they had valves. He announced his findings in the court of Queen Christina of Sweden, but did not publish his findings for a year, and in the interim similar findings were published by Thomas Bartholin, who additionally published that such vessels are present everywhere in the body, and not just the liver. He is also the one to have named them "lymphatic vessels". This had resulted in a bitter dispute between one of Bartholin's pupils, Martin Bogdan, and Rudbeck, whom he accused of plagiarism.
Breathing Problems: Foundation for Chronic DiseasesOver 90% of modern people suffer from breathing problems, such as chest breathing, mouth breathing, and hyperventilation (breathing more than the medical norm). All these abnormalities reduce oxygen levels in body cells and promote chronic diseases. Consider how sick people breathe.Myth #1. Breathing is regulated by want for oxygen.If you open any medical or physiological textbook with the description of the control of respiration, you will find that in normal conditions, breathing is regulated by the CO2 concentration in the arterial blood and the brain. Whatever we do (sit, walk, eat, run, sleep, etc.), CO2 concentration is kept within a narrow range (0.1% accuracy) by the breathing centre located in the medulla oblongata of the brain. Myth #2. CO2 is a poisonous or toxic waste gas and a waste product to get rid off. When a healthy person tries to hyperventilate or is forced to breathe deeply and fast, they experience hypocapnia (CO2 deficiency) in the blood and other fluids, tissues, and cells. The immediate effects are: constriction of blood vessels (CO2 is a powerful vasodilator) and reduced blood and oxygen supply to the brain, heart and all other vital organs. This is the reason why it is so easy to faint or pass out after 2-3 minutes of forceful hyperventilation. Another CO2 effect is the suppressed Bohr effect or diminished release of oxygen by the blood in the tissues due to the same hypocapnia. Apart from these phenomena, there are many other vital functions of CO2 in the human body (see links to medical studies below). Meanwhile, reduced tissue oxygenation is sufficient to promote cancer, heart disease, diabetes and many other chronic conditions.Myth #3. When a person is healthy, they can feel how they breathe.If people with normal breathing are asked what they feel about their breathing, they will say that they feel nothing at all (as if they are barely breathing). The perfect man breathes as if he is not breathing Lao-Tzu, circa 4th century BC. Indeed, if you have any healthy people around you and observe their breathing for 20-30 seconds, you will see and hear nothing. The medical norm for breathing is tiny. It is only 6 L/min or only 12 breaths/min with tiny 500 mL for one breath, while most modern people have about 700 mL. They are deep breathers.Myth #4. My breathing is OK and I know how to breathe.Less than 10% of people have normal breathing parameters and body oxygen stores these days. Check these 24 medical and physiological respiratory studies done on ordinary or normal subjects during last 80 years (Hyperventilation: Present in Over 90% of Normals). It is a fact that the medical norm established about a century ago is not a norm anymore. Modern people breathe about 2 times more air than we did 100 years ago. Hyperventilation results in tissue hypoxia and many other biochemical abnormalities. Your breathing is normal, if and only if you have normal body oxygenation. How can you check it? You should be able to easily hold your breath for at least 40 s after your usual exhalation and with no stress at the end of the test. This test is described in detail below.Myth #5. More breathing (deeper and/or greater volume) means better body oxygenation or even over oxygenation of the blood.During miniscule normal breathing, oxygenation of the arterial blood is about 98-99%. Note that normal breathing is invisible and inaudible. It is so light that most people do not feel it. As a result, breathing more air cannot get much more oxygen in the blood. It follows that, no matter how deep and fast one breathes, he or she cannot get over oxygenated blood using normal air, while pure oxygen is toxic for the lungs tissue.There is zero scientific evidence about this deep breathing myth, but hundreds of published studies have clearly shown that hyperventilation (or breathing more than the tiny medical norm) REDUCES oxygen supply to the brain, heart, liver, kidneys, and all other vital organs due to losses in CO2. (There are hundreds of studies presented on this website that proved this fact.) Nevertheless, on TV, radio, and in everyday life situations, people who have little knowledge of physiology say, Take a deep breath, get more oxygen, or Breathe deeper for better oxygenation, etc.Myth #6. Sick people notice when their breathing becomes abnormal.100% prevalence of hyperventilation at rest for the sick people is confirmed by over 40 published western studies on heart disease, cancer, asthma, COPD, diabetes, cystic fibrosis, epilepsy, panic attacks, chronic fatigue, and many other conditions. These sick patients breathe about 2-3 times more than the norm (see this Table with Minute Ventilation Rates for Chronic Diseases), and usually do not complain or even notice that their breathing is heavy or too deep. Why? This is because air is weightless and the main breathing muscles (diaphragm and chest) are very powerful: we can pump 25 times more air during maximum exercise (or about 150 liters of air in one minute), than we require for normal breathing at rest (only about 6 L/min). People may notice that their breathing is heavy during heart attacks, stroke, asthma attacks, or morning hyperventilation (between 4 and 7 am).
Minute ventilation rates (chronic diseases)ConditionMinute ventilation
Normal breathing6 L/min
Healthy Subjects6-7 L/min
Heart disease15 (4) L/min
Pulm hypertension12 (2) L/min
Cancer12 (2) L/min
Diabetes12-17 L/min
Asthma13 (2) L/min
COPD14 (2) L/min
Sleep apnea15 (3) L/min
Liver cirrhosis11-18 L/min
Hyperthyroidism15 (1) L/min
Cystic fibrosis15 L/min
CF and diabetes*10 L/min
Epilepsy13 L/min
CHV13 (2) L/min
Panic disorder12 (5) L/min
Bipolar disorder11 (2) L/min
Dystrophia myotonica16 (4) L/min
Yoga Breathing: Main Secret of Yoga's Super HealthMany people believe that yoga is about postures and maybe breathing exercises. Well, one may spend years practicing asanas and thousands of hours doing breathing exercises, but his or her health can get worse and worse. Instead of these silly ideas, it is smart to think about finding some criteria or measurements of super health. Then we can decide who is a real yoga master.Super health of real yoga masters is possible to measure. They should have the ideal automatic breathing pattern (with about 3 small breath per minute at rest or during sleep). This slow and relaxed breathing pattern provides the human body with superior body oxygenation: about 2-3 minutes for the DIY body oxygen test. Yoga masters should have only about 2 hours of natural sleep and do not require more. There are many other effects that corresponds to the ideal breathing pattern. You can find them on the web page Ideal Breathing Pattern.Indeed, the body and cells require oxygen 24/7. One can practice best yoga sessions, but if he or she sleeps on their back at night, or breathes through the mouth while sleeping, all positive effects of yoga practice will be demolished by tissue hypoxia and free radicals generated during sleep.According to ancient hatha yoga manuscripts, the goal of yoga breathing exercises is to "restrain", "hold", "suspend", and "calm" the breath 24/7. There are no any hints or quotes in these classical yoga texts about "breathing more" or "breathing deeper". According to these books, progress in pranayama (the main yoga breathing exercise) is measured in longer cycles for breath holds, inhalations, and exhalations. This is possible only if one's unconscious breathing becomes smaller and slower. When the diaphragmatic breathing pattern gradually becomes slower and lighter (breathing less air 24/7), blood supply, perfusion, abilities of the immune system, cells oxygen content, and many other key parameters of the human body are improved.
Buteyko Table of Health Zones (average parameters at rest)Health stateType of breathingDegreePulse,beats/minBreathing frequency/minCO2 inalveoli, %AP, sCP, sMP, s
Super-healthShallow54837.516180210
45047.412150190
35257.39120170
25567.17100150
15776.8580120
NormalNormal-6086.546090
DiseaseDeep-165106.035075
-270125.524060
-375155.0-3050
-480204.5-2040
-590264.0-1020
-6100303.5-510
Comments on Buteyko Table of Health Zones. Pulse heart rate or pulse rate in 1 minute; Breathing or Respiratory frequency in one minute (number of inhalations or exhalations); % CO2 - %CO2 in alveoli of the lungs (*or arterial blood if there is no mismatch); AP - the Automatic Pause or natural delay in breathing after exhalation (*during unconscious breathing); CP - the Control Pause (body oxygen test, breath holding time after usual exhalation and until first distress only); MP (the Maximum Pause, breath holding time after usual exhalation and as long as possible).This discovery is patented (see the bottom of this page) and the table is based on Buteyko KP, The method of volitional elimination of deep breathing [Translation of the Small Buteyko Manual], Voskresensk, 1994.* Note about pulse. Not all people with low CPs (less than 20 s) have a greatly increased heart rate, as is given by this table. Some categories of people with less than 20 s CP can have a resting pulse of around 60 70 beats per minute. However, increased heart rate for lower CPs is the feature of, for example, heart patients and patients with severe asthma. During the 1960's, when conducting his research, and later, Buteyko and his colleagues applied the Buteyko breathing retraining program mainly for heart and asthma patients, who were mostly hospitalized with frequent deficiencies in blood cortisol levels. This explains the increased heart rates provided by the Table.Buteyko normsDr. Buteyko suggested his own standards for health so that one can be free from about 200 chronic conditions. As we see in the Buteyko Table of Health Zones (the middle or central row), healthy people should have breathing frequency no more than 8 breaths per minute at rest, more than 60 s CP, over 6.5% CO2, less than 60 beats per min for heart rate, and at least 4 s for automatic pause.At this stage people enjoy and even crave physical activity. They are full of energy (when they have a normal blood glucose level). Standing throughout the day is easy and natural. Sleep is less than 5 hours and early morning parameters are not worse than evening ones.All tissues of the body are histologically normal (or in accordance with medical books), while chronic disorders are impossible.Steps of Buteyko Method1. Nasal breathingThe Buteyko method emphasizes the importance of nasal breathing, which protects the airways by humidifying, warming, and cleaning the air entering the lungs. A majority of asthmatics have problems sleeping at night, and this is thought to be linked with poor posture or unconscious mouth-breathing. By keeping the nose clear and encouraging nasal breathing during the day, night-time symptoms can also improve. Other methods of encouraging nasal breathing are full-face CPAP machines - commonly used to treat sleep apnea - or using a jaw-strap or paper-tape to keep the mouth closed during the night. Strictly nasal breathing during physical exercise is another key element of the Buteyko method.2. Reduced breathing exercisesThe core Buteyko exercises involve breath control; consciously reducing either breathing rate or breathing volume. Many teachers refer to Buteyko as 'breathing retraining' and compare the method to learning to ride a bicycle. Once time has been spent practicing, the techniques become instinctive and the exercises are gradually phased out as the condition improves.Rather than using traditional peak flow measurements to monitor the condition of asthmatics, Buteyko uses an exercise called the Control Pause (CP), defined as the amount of time that an individual can comfortably hold breath after a normal exhalation. According to Buteyko teachers, with regular Buteyko reduced-breathing practice, asthmatics are expected to find that their CP gradually increases and in parallel decreased asthma symptoms.3. RelaxationDealing with asthma attacks is an important factor of Buteyko practice. The first feeling of an asthma attack is unsettling and can result in a short period of rapid breathing. By controlling this initial over-breathing phase, asthmatics can prevent a "vicious circle of over-breathing" from developing and spiraling into an asthma attack. This means that asthma attacks may be averted simply by breathing less.
Yoga Pranayama: How to Get Pranayama BenefitsInstead of exploring the essence of yoga pranayama, most yoga teachers today are busy with dividing and sub-dividing this wise and exceptionally powerful breathing practice into various forms. Yes, there are many possible exercises in pranayama, but only one essential process: slowing down our automatic breathing. Indeed, when this main pranayama mechanism and its physiological effects are poorly understood, attention will be diverted from true progress in pranayama onto relatively meaningless topics and subjects. What is true progress in pranayama?
The Shiva Samhita(5) The Pranayama"22. Then let the wise practitioner close with his right thumb the pingala (right nostril), inspire air through the ida (the left nostril); and keep the air confined suspend his breathing as long as he can; and afterwards let him breathe out slowly, and not forcibly, through the right nostril.
23. Again, let him draw breath through the right nostril, and stop breathing as long as his strength permits; then let him expel the air through the left nostril, not forcibly, but slowly and gently.""39. When the Yogi can, of his will, regulate the air and stop the breath (whenever and how long) he likes, then certainly he gets success in kumbhaka, and from the success in kumbhaka only, what things cannot the Yogi commend here?""43. ... from the perfection of pranayama, follows decrease of sleep, excrements and urine."Increase of Duration"53. Then gradually he should make himself able to practice for three gharis (one hour and a half at a time, he should be able to restrain breath for that period). Through this, the Yogi undoubtedly obtains all the longed for powers.""57. When he gets the power of holding breath (i.e., to be in a trance) for three hours, then certainly the wonderful state of pratyahar is reached without fail."
Kussmaul breathingFrom Wikipedia, the free encyclopediaJump to: navigation, searchKussmaul breathing is a deep and labored breathing pattern often associated with severe metabolic acidosis, particularly diabetic ketoacidosis (DKA) but also renal failure. It is a form of hyperventilation, breathing which is increased above the required rate. Kussmaul breathing is characterized as rapid, deep breathing.In metabolic acidosis, breathing is first rapid and shallow[1] but as acidosis worsens, breathing gradually becomes deep, labored and gasping.Contents[hide] 1 Terminology 2 History 3 Mechanism 4 References
[edit] TerminologyKussmaul, who introduced the term, referred to breathing when metabolic acidosis was sufficiently severe for the respiratory rate to be normal or reduced.[2] This definition is also followed by several other sources,[3][4] including for instance Merriam-Webster, which defines Kussmaul breathing as "abnormally slow deep respiration characteristic of air hunger and occurring especially in acidotic states".[5] Other sources, however, use the term Kussmaul respiration also when acidosis is less severe, in which case breathing is rapid.[4][6]Note that Kussmaul breathing occurs only in advanced stages of acidosis, and is fairly rarely reached. In less severe cases of acidosis, rapid, shallow breathing is seen. Kussmaul breathing is a kind of very deep, gasping, desperate breathing. Occasionally, medical literature refers to any abnormal breathing pattern in acidosis as Kussmaul breathing; however, this is inaccurate.[edit] HistoryKussmaul breathing is named for Adolph Kussmaul,[2] the 19th century German doctor who first noted it among patients with advanced diabetes mellitus. Kussmaul's sign is also an eponymous finding attributable to Kussmaul, and should be distinguished from Kussmaul breathing.He published his finding in a classic 1874 paper.[7]MechanismKussmaul breathing is respiratory compensation for a metabolic acidosis, most commonly occurring in diabetics in diabetic ketoacidosis. Blood gases on a patient with Kussmaul breathing will show a low partial pressure of CO2 in conjunction with low bicarbonate because of a forced increased respiration (blowing off the carbon dioxide). Base excess is severely negative. The patient feels an urge to breathe deeply, an "air hunger", and it appears almost involuntary.A metabolic acidosis soon produces hyperventilation, but at first it will tend to be rapid and relatively shallow. Kussmaul breathing develops as the acidosis grows more severe. Indeed, Kussmaul originally identified this type of breathing as a sign of coma and imminent death in diabetic patients.Duration of fasting, presence or absence of hepatomegaly and Kussmaul breathing provide clues to the differential diagnosis of hyperglycemia in the inborn errors of metabolism.
Agonal respirationFrom Wikipedia, the free encyclopedia(Redirected from Agonal breathing)Jump to: navigation, searchThis article includes a list of references, related reading or external links, but its sources remain unclear because it lacks inline citations. Please improve this article by introducing more precise citations. (January 2011)
Agonal respiration is an abnormal pattern of breathing characterized by shallow, slow (3-4 per minute), irregular inspirations followed by irregular pauses. It may also be characterized by gasping, labored breathing, accompanied by strange vocalizations and myoclonus. Possible causes include cerebral ischemia, extreme hypoxia or even anoxia. Agonal breathing is an extremely serious medical sign requiring immediate medical attention, as the condition generally progresses to complete apnea and heralds death.The term is sometimes (inaccurately) used to refer to labored, gasping breathing patterns accompanying organ failure (e.g. liver failure and renal failure), SIRS, septic shock, and metabolic acidosis (see Kussmaul breathing, or in general any labored breathing, including Biot's respirations and ataxic respirations. Correct usage would restrict the term to the last breaths before death.Agonal respirations are also commonly seen in cases of cardiogenic shock or cardiac arrest where agonal respirations may persist for several minutes after cessation of heartbeat. The presence of agonal respirations in these cases indicates a more favorable prognosis than in cases of cardiac arrest without agonal respirations.A victim who has agonal gasps and does not respond and has no pulse is in cardiac arrest, agonal gasps are not effective breaths.Agonal respiration is not the same as, and is unrelated to, the phenomenon of death rattle.
Cheyne-Stokes respirationFrom Wikipedia, the free encyclopediaJump to: navigation, searchCheyne-Stokes respiration
ICD-10R06.3
ICD-9786.04
MeSHD002639
Graph showing the Cheyne-Stokes breathing pattern.Cheyne-Stokes respiration ( /tenstoks/) is an abnormal pattern of breathing characterized by progressively deeper and sometimes faster breathing, followed by a gradual decrease that results in a temporary stop in breathing called an apnea. The pattern repeats, with each cycle usually taking 30 seconds to 2 minutes.[1] It is an oscillation of ventilation between apnea and hyperpnea with a crescendo-diminuendo pattern, and is associated with changing serum partial pressures of oxygen and carbon dioxide.[2]Cheyne-Stokes respiration and periodic breathing are the two regions on a spectrum of severity of oscillatory tidal volume. The distinction lies in what we observe happening at the trough of ventilation: if there is apnea, we describe it as Cheyne-Stokes respiration (since apnea is a prominent feature in their original description); if there is only hypopnea (abnormally small but not absent breaths) then we call it periodic breathing. Physiologically and mathematically, the phenomena are less different than they appear, because breaths that are smaller than the anatomical dead space do not actually ventilate the lung and so - from the point of view of gas concentrations in an alveolus - the nadir of hypopnea in periodic breathing may be indistinguishable from apnea.These phenomena can occur during wakefulness or during sleep, where they are called the Central sleep apnea syndrome (CSAS).[3]It may be caused by damage to respiratory centers,[4] or by physiological abnormalities in chronic heart failure,[5] and is also seen in newborns with immature respiratory systems and in visitors new to high altitudes.Contents[hide] 1 History 2 Pathophysiology 3 Associated conditions 4 Related patterns 5 References
[edit] HistoryThe condition was named after John Cheyne and William Stokes, the physicians who first described it in the 19th century.[6][7][edit] PathophysiologyIn heart failure, the mechanism of the oscillation is unstable feedback in the respiratory control system. In normal respiratory control, negative feedback allows a steady level of alveolar gas concentrations to be maintained, and therefore stable tissue levels of oxygen and carbon dioxide (CO2). At the steady state, the rate of production of CO2 equals the net rate at which it is exhaled from the body, which (assuming no CO2 in the ambient air) is the product of the alveolar ventilation and the end-tidal CO2 concentration. Because of this interrelationship, the set of possible steady states forms a hyperbola:Alveolar ventilation = (body CO2 production)/end-tidal CO2 fraction.In the figure below, this relationship is the curve falling from the top left to the bottom right. Only positions along this curve permit the body's CO2 production to be exactly compensated for by exhalation of CO2. Meanwhile there is another curve, shown in the figure for simplicity as a straight line from bottom left to top right, which is the body's ventilatory response to different levels of CO2. Where the curves cross is the potential steady state (S).Through respiratory control reflexes, any small transient fall in ventilation (A) leads to a corresponding small rise (A') in alveolar CO2 concentration which is sensed by the respiratory control system so that there is a subsequent small compensatory rise in ventilation (B) above its steady state level (S) that helps restore CO2 back to its steady state value. In general, transient or persistent disturbances in ventilation, CO2 or oxygen levels can be counteracted by the respiratory control system in this way.
However, in some pathological states, the feedback is more powerful than is necessary to simply return the system towards its steady state. Instead, ventilation overshoots and can generate an opposite disturbance to the original disturbance. If this secondary disturbance is larger than the original, the next response will be even larger, and so on, until very large oscillations have developed, as shown in the figure below.
The cycle of enlargement of disturbances reaches a limit when successive disturbances are no longer larger, which occurs when physiological responses no longer increase linearly in relation to the size of the stimulus. The most obvious example of this is when ventilation falls to zero: it cannot be any lower. Thus Cheyne-Stokes respiration can be maintained over periods of many minutes or hours with a repetitive pattern of apneas and hyperpneas.The end of the linear decrease in ventilation in response to falls in CO2 is not, however, at apnea. It occurs when ventilation is so small that air being breathed in never reaches the alveolar space, because the inspired tidal volume is no larger than the volume of the large airways such as the trachea. Consequently, at the nadir of periodic breathing, ventilation of the alveolar space may be effectively zero; the easily-observable counterpart of this is failure at that time point of the end-tidal gas concentrations to resemble realistic alveolar concentrations.Many potential contributory factors have been identified by clinical observation, but unfortunately they are all interlinked and covary extensively. Widely accepted risk factors are hyperventilation, prolonged circulation time, and reduced blood gas buffering capacity.[8][9]They are physiologically interlinked in that (for any given patient) circulation time decreases as cardiac output increases. Likewise, for any given total body CO2 production rate, alveolar ventilation is inversely proportional to end-tidal CO2 concentration (since their mutual product must equal total body CO2 production rate). Chemoreflex sensitivity is closely linked to the position of the steady state, because if chemoreflex sensitivity increases (other things being equal) the steady-state ventilation will rise and the steady-state CO2 will fall. Because ventilation and CO2 are easily to observe because they are commonly-measured clinical variables which do not require any particular experiment to be conducted in order to observe them, abnormalities in these variables are more likely to be reported in the literature. However, other variables, such as chemoreflex sensitivity can only be measured by specific experiment, and therefore abnormalities will not in them will not be found in routine clinical data.[10] When measured in patients with Cheyne-Stokes respiration, hypercapnic ventilatory responsiveness may be elevated by 100% or more. When not measured, its consequences - such as a low mean PaCO2 and elevated mean ventilation - may sometimes appear to be the most prominent feature.[11][12][13]Circulatory delay may determine the length of the apnea-hyperpnea cycle although it is rarely sufficiently prolonged itself to be a major driving factor for instability.[14][15][edit] Associated conditionsThis abnormal pattern of breathing, in which breathing is absent for a period and then rapid for a period, can be seen in patients with heart failure,[16][17] strokes, traumatic brain injuries and brain tumors. In some instances, it can occur in otherwise healthy people during sleep at high altitudes. It can occur in all forms of toxic metabolic encephalopathy.[18] It is a symptom of carbon monoxide poisoning, along with syncope or coma. This type of respiration is also often seen after morphine administration.Hospice personnel sometimes document the presence of Cheyne-Stokes breathing as a patient nears death, and report that patients able to speak after such episodes do not report any distress associated with the breathing, although it is sometimes disturbing to the family.[edit] Related patternsCheyne-Stokes respirations are not the same as Biot's respirations ("cluster breathing"), in which groups of breaths tend to be similar in size.They differ from Kussmaul respirations in that the Kussmaul pattern is one of consistent very deep breathing at a normal or increased rate.
Biot's respirationFrom Wikipedia, the free encyclopediaJump to: navigation, searchBiot's respiration, sometimes also called ataxic respiration,[citation needed] is an abnormal pattern of breathing characterized by groups of quick, shallow inspirations followed by regular or irregular periods of apnea.[1]It generally indicates a poor prognosis.It is named for Camille Biot, who characterized it in 1876.[2][3]Contents[hide] 1 Causes 2 Related patterns 3 References 4 External links
[edit] CausesBiot's respiration is caused by damage to the medulla oblongata due to strokes or trauma or by pressure on the medulla due to uncal or tentorial herniation.It can be caused by opioid use.[4][edit] Related patternsIt is distinguished from ataxic respiration by having more regularity and similar-sized inspirations, whereas ataxic respirations are characterized by completely irregular breaths and pauses. As the breathing pattern deteriorates, it merges with ataxic respirations.In common medical practice, Biot's respiration is often clinically equivalent to Cheyne-Stokes respiration, although the two definitions are separated in some academic settings.
PneumaFrom Wikipedia, the free encyclopediaJump to: navigation, searchThis article is about the philosophical concept. For other uses, see Pneuma (disambiguation).Look up pneuma in Wiktionary, the free dictionary.
Pneuma () is an ancient Greek word for "breath," and is related, in theological and philosophical contexts, to psyche ( "spirit" or "soul"), as in the phrase "breath of life".[1] It is given various technical meanings by medical writers and philosophers of classical antiquity, and is also used in Greek translations of the Hebrew Bible and in the Greek New Testament.Contents[hide] 1 Classical antiquity 1.1 Ancient Greek medical theory 1.2 Aristotle 1.3 Stoic pneuma 2 Judaism and Christianity 3 See also 4 References
[edit] Classical antiquityPneuma, "air in motion, breath, wind," is equivalent in the material monism of Anaximenes to aer (, "air") as the element from which all else originated. This usage is the earliest extant occurrence of the term.[edit] Ancient Greek medical theorySee also: Pneumatic schoolIn ancient Greek medicine, pneuma is the form of circulating air necessary for the systemic functioning of vital organs. It is the material that sustains consciousness in a body. According to Diocles and Praxagoras, the psychic pneuma mediates between the heart, regarded as the seat of Mind in some physiological theories of ancient medicine, and the brain.[2]The disciples of Hippocrates explained the maintenance of vital heat to be the function of the breath within the organism. Around 300 BC, Praxagoras discovered the distinction between the arteries and the veins. In the corpse arteries are empty; hence, in the light of these preconceptions they were declared to be vessels for conveying pneuma to the different parts of the body. A generation afterwards, Erasistratus made this the basis of a new theory of diseases and their treatment. The pneuma, inhaled from the outside air, rushes through the arteries till it reaches the various centres, especially the brain and the heart, and there causes thought and organic movement.[3]AristotleThe "connate pneuma" of Aristotle is the warm mobile "air" that in the sperm transmits the capacity for locomotion and certain sensations to the offspring.Stoic pneumaIn Stoic philosophy, pneuma is the concept of the "breath of life," a mixture of the elements air (in motion) and fire (as warmth). For the Stoics, pneuma is the active, generative principle that organizes both the individual and the cosmos. In its highest form, the pneuma constitutes the human soul (psych), which is a fragment of the pneuma that is the soul of God (Zeus). As a force that structures matter, it exists even in inanimate objects.
PranaFrom Wikipedia, the free encyclopediaJump to: navigation, searchPrana (, pra) is the Sanskrit word for "vital life" (from the root pr "to fill", cognate to Latin plenus "full"). It is one of the five organs of vitality or sensation, viz. prana "breath", vac "speech", chakshus "sight", shrotra "hearing", and manas "thought" (nose, mouth, eyes, ears and mind; ChUp. 2.7.1).In Vedantic philosophy, prana is the notion of a vital, life-sustaining force of living beings and vital energy, comparable to the Chinese notion of Qi. Prana is a central concept in Ayurveda and Yoga, where it is believed to flow through a network of fine subtle channels called nadis. Its most subtle material form is the breath, but it is also to be found in the blood, and its most concentrated form is semen in men and vaginal fluid in women.[1] The Pranamaya-kosha is one of the five Koshas or "sheaths" of the Atman.Prana was first expounded in the Upanishads, where it is part of the worldly, physical realm, sustaining the body and the mother of thought and thus also of the mind. Prana suffuses all living forms but is not itself the Atman or individual soul. In the Ayurveda, the Sun and sunshine are held to be a source of prana.In the Hindu philosophy of Kashmir Shaivism, prana is regarded as an aspect of Shakti (cosmic energy).[citation needed]Contents[hide] 1 Nadis 2 The Five Pras 3 The Five Upa-Pranas 4 Pranayama 5 See also 6 References 7 External links
[edit] NadisFurther information: Nadi (yoga)In Yoga, the three main channels of prana are the Ida, the Pingala and the Sushumna. Ida relates to the right side of the brain, and the left side of the body, terminating at the left nostril and pingala to the left side of the brain and the right side of the body, terminating at the right nostril. In some practices, alternate nostril breathing balances the prana that flows within the body. In most ancient texts, the total number of nadis in the human body is stated to be 72,000. When prana enters a period of uplifted, intensified activity, the Yogic tradition refers to it as Pranotthana.[2][edit] The Five PrasIn Ayurveda, the Pra is further classified into subcategories, referred to as prana vayus. According to Hindu philosophy these are the vital principles of basic energy and subtle faculties of an individual that sustain physiological processes. There are five pranas or vital currents in the Hindu system:[3]1. Pra : Responsible for the beating of the heart and breathing. Prana enters the body through the breath and is sent to every cell through the circulatory system.2. Apna : Responsible for the elimination of waste products from the body through the lungs and excretory systems.3. Una : Responsible for producing sounds through the vocal apparatus, as in speaking, singing, laughing, and crying. Also it represents the conscious energy required to produce the vocal sounds corresponding to the intent of the being. Hence Samyama on udana gives the higher centers total control over the body.4. Samna : Responsible for the digestion of food and cell metabolism (i.e. the repair and manufacture of new cells and growth). Samana also includes the heat regulating processes of the body. Auras are projections of this current. By meditational practices one can see auras of light around every being. Yogis who do special practise on samana can produce a blazing aura at will.]]).[citation needed]5. Vyna : Responsible for the expansion and contraction processes of the body, e.g. the voluntary muscular system.[edit] The Five Upa-PranasIn Yoga the Prana is further classified into subcategory Upa-prana with following items:[4]1. Naga : Responsible for burping.2. Kurma : Responsible for blinking.3. Devadatta : Responsible for yawning.4. Krikala : Responsible for Sneezing.5. Dhananjaya : Responsible for opening and closing of heart valves.[edit] PranayamaPranayama is the practice in which the control of prana is achieved (initially) from the control of one's breathing. According to Yogic philosophy the breath, or air, is merely a gateway to the world of prana and its manifestation in the body.[citation needed] In yoga, pranayama techniques are used to control the movement of these vital energies within the body, which is said to lead to an increase in vitality in the practitioner.[citation needed] However, intensive practice [5] of these techniques is not trivial. Kason [6] describes situations where intensive pranayama techniques may have adverse effects on certain practitioners. According to kundalini yoga, intensive and systematic practice of pranayama can lead to the awakening of kundalini.[citation needed]
QiFrom Wikipedia, the free encyclopediaJump to: navigation, searchQi (Ch'i)
Chinese name
Traditional Chinese
Simplified Chinese
[show]Transcriptions
Mandarin
- Hanyu Pinyinq
- WadeGilesch'i4
Min
- Hokkien POJkh
Cantonese
- Jyutpinghei3
Japanese name
Hiragana
Kyjitai
Shinjitai
[show]Transcriptions
- Revised Hepburnki
Korean name
Hangul
Hanja
[show]Transcriptions
- RevisedRomanizationgi
- McCune-Reischauerki
Thai name
Thai
RTGSChi
Vietnamese name
Quc ngkh
This article contains Chinese text. Without proper rendering support, you may see question marks, boxes, or other symbols instead of Chinese characters.
For other uses, see Qi (disambiguation).In traditional Chinese culture, q (also chi or ch'i) is an active principle forming part of any living thing. Qi is frequently translated as "lifeforce" or "energy flow". Notions in the west of energeia, lan vital, or vitalism are purported[by whom?] to be similar. Qi is the central underlying principle in traditional Chinese medicine. The literal translation of "qi" is air, breath, or gas.Contents[hide] 1 Term and character 2 Definition 3 Pronunciation 4 Early philosophical texts 5 Traditional Chinese medicine 6 Scientific investigation 7 Feng shui 8 Martial arts 9 See also 10 References 11 Further reading 12 External links
[edit] Term and characterThe etymological explanation for the form of the qi logogram in the traditional form is steam () rising from rice () as it cooks. The earliest way of writing qi consisted of three wavy lines, used to represent one's breath seen on a cold day. A later version, , identical to the present-day simplified character, is a stylized version of those same three lines. For some reason, early writers of Chinese found it desirable to substitute for a cognate character that originally meant to feed other people in a social context such as providing food for guests.[citation needed] Appropriately, that character combined the three-line qi character with the character for rice. So plus formed , and that is the traditional character still used today (the oracle bone character, the seal script character and the modern "school standard" or Ki sh characters in the box at the right show three stages of the evolution of this character).[1]
Traditional Chinese character q, also used in Korean hanja. In Japanese kanji, this character was used until 1946, when it was changed to .[edit] DefinitionReferences to concepts analogous to the qi taken to be the life-process or flow of energy that sustains living beings are found in many belief systems, especially in Asia. Philosophical conceptions of qi from the earliest records of Chinese philosophy (5th century BC) correspond to Western notions of humours and the ancient Hindu yogic concept of prana, meaning "life force" in Sanskrit. The earliest description of qi in the current sense of vital energy is found in the Vedas of ancient India (circa 1500-1000BC) [2], and from the writings of the Chinese philosopher Mencius (4th century BC). Historically, it is the Huangdi Neijing translated as, The Yellow Emperor's Classic of Medicine (circa 2nd century BC) that is credited with first establishing the pathways through which qi circulates in the human body.[3]Within the framework of Chinese thought, no notion may attain such a degree of abstraction from empirical data as to correspond perfectly to one of our modern universal concepts. Nevertheless, the term qi comes as close as possible to constituting a generic designation equivalent to our word "energy". When Chinese thinkers are unwilling or unable to fix the quality of an energetic phenomenon, the character qi () inevitably flows from their brushes.[4]
Manfred Porkert
The ancient Chinese described it as "life-force". They believed qi permeated everything and linked their surroundings together. They likened it to the flow of energy around and through the body, forming a cohesive and functioning unit. By understanding its rhythm and flow they believed they could guide exercises and treatments to provide stability and longevity.Although the concept of qi has been important within many Chinese philosophies, over the centuries the descriptions of qi have varied and have sometimes been in conflict. Until China came into contact with Western scientific and philosophical ideas, they would not have categorized all things in terms of matter and energy. Qi and li (, li, pattern) were 'fundamental' categories similar to matter and energy.
Hand written calligraphic Qi.Fairly early on, some Chinese thinkers began to believe that there were different fractions of qi and that the coarsest and heaviest fractions of qi formed solids, lighter fractions formed liquids, and the most ethereal fractions were the "lifebreath" that animates living beings.[5]Yun q is a notion of innate or pre-natal qi to distinguish it from acquired qi that a person may develop over the course of their lifetime.[edit] PronunciationOther spellings include in simplified Chinese: ; traditional Chinese: ; Mandarin Pinyin: q; WadeGiles: ch'i; Jyutping: hei. Qi is pronounced /ti/ in English and [t] in Standard Chinese; Korean: gi; Japanese: ki; Vietnamese: kh, pronounced [x]) The approximate English pronunciation of qi, similar to "chee" in cheese, should also be distinguished from the pronunciation of the Greek letter chi, which has a hard c sound, like "c" in car, and a long i, similar to other Greek letters phi, psi, xi.[edit] Early philosophical textsTaoism
This article is part of a series on Taoism
Fundamentals
Dao (Tao) De (Te) Wuji Taiji Yin-Yang Wu Xing Qi Neidan Wu wei
Texts
Laozi (Tao Te Ching) Zhuangzi Liezi Daozang
Deities
Three Pure Ones Guan Shengdi Eight Immortals Yellow Emperor Xiwangmu Jade Emperor Chang'e Other deities
People
Laozi Zhuangzi Zhang Daoling Zhang Jue Ge Hong Chen Tuan
Schools
Tianshi Dao Shangqing Lingbao Quanzhen Dao Zhengyi Dao Wuliupai
Sacred sites
Grotto-heavens Mount Penglai
Taoism Portalv d e
The earliest texts that speak of qi give some indications of how the concept developed. The philosopher Mo Di used the word qi to refer to noxious vapors that would in due time arise from a corpse were it not buried at a sufficient depth.[6] He reported that early civilized humans learned how to live in houses to protect their qi from the moisture that had troubled them when they lived in caves.[7] He also associated maintaining one's qi with providing oneself adequate nutrition.[8] In regard to another kind of qi, he recorded how some people performed a kind of prognostication by observing the qi (clouds) in the sky.[9]In the Analects of Confucius, compiled from the notes of his students sometime after his death in 479 B.C., qi could mean breath,[10] and combining it with the Chinese word for blood (making , xue-qi, blood and breath), the concept could be used to account for motivational characteristics.The [morally] noble man guards himself against three things. When he is young, his xue-qi has not yet stabilized, so he guards himself against sexual passion. When he reaches his prime, his xue-qi is not easily subdued, so he guards himself against combativeness. When he reaches old age, his xue-qi is already depleted, so he guards himself against acquisitiveness.
Confucius, Analects, 16:7
Mencius described a kind of qi that might be characterized as an individual's vital energies. This qi was necessary to activity, and it could be controlled by a well-integrated willpower.[11] When properly nurtured, this qi was said to be capable of extending beyond the human body to reach throughout the universe.[11] It could also be augmented by means of careful exercise of one's moral capacities.[11] On the other hand, the qi of an individual could be degraded by averse external forces that succeed in operating on that individual.[12]Not only human beings and animals were believed to have qi. Zhuangzi indicated that wind is the qi of the Earth.[13] Moreover, cosmic yin and yang "are the greatest of qi."[14] He described qi as "issuing forth" and creating profound effects.[15] He said "Human beings are born [because of] the accumulation of qi. When it accumulates there is life. When it dissipates there is death... There is one qi that connects and pervades everything in the world."[16]Another passage traces life to intercourse between Heaven and Earth: "The highest Yin is the most restrained. The highest Yang is the most exuberant. The restrained comes forth from Heaven. The exuberant issues forth from Earth. The two intertwine and penetrate forming a harmony, and [as a result] things are born."[17]"The Guanzi essay 'Neiye' (Inward training) is the oldest received writing on the subject of the cultivation of vapor [qi] and meditation techniques. The essay was probably composed at the Jixia Academy in Qi in the late fourth century B.C."[18]Xun Zi, another Confucian scholar of the Jixia Academy, followed in later years. At 9:69/127, Xun Zi says, "Fire and water have qi but do not have life. Grasses and trees have life but do not have perceptivity. Fowl and beasts have perceptivity but do not have yi (sense of right and wrong, duty, justice). Men have qi, life, perceptivity, and yi." Chinese people at such an early time had no concept of radiant energy, but they were aware that one can be heated by a campfire from a distance away from the fire. They accounted for this phenomena by claiming "qi" radiated from fire. At 18:62/122, he too uses "qi" to refer to the vital forces of the body that decline with advanced age.Among the animals, the gibbon and the crane were considered experts in inhaling the qi. The Confucian scholar Dong Zhongshu (ca. 150 BC) wrote in Luxuriant Dew of the Spring and Autumn Annals:[19] "The gibbon resembles a macaque, but he is larger, and his color is black. His forearms being long, he lives eight hundred years, because he is expert in controlling his breathing." ("")Later, the syncretic text assembled under the direction of Liu An, the Huai Nan Zi, or "Masters of Huainan", has a passage that presages most of what is given greater detail by the Neo-Confucians:Heaven (seen here as the ultimate source of all being) falls (duo , i.e., descends into proto-immanence) as the formless. Fleeting, fluttering, penetrating, amorphous it is, and so it is called the Supreme Luminary. The dao begins in the Void Brightening. The Void Brightening produces the universe (yu-zhou ). The universe produces qi. Qi has bounds. The clear, yang [qi] was ethereal and so formed heaven. The heavy, turbid [qi] was congealed and impeded and so formed earth. The conjunction of the clear, yang [qi] was fluid and easy. The conjunction of the heavy, turbid [qi] was strained and difficult. So heaven was formed first and earth was made fast later. The pervading essence (xi-jing) of heaven and earth becomes yin and yang. The concentrated (zhuan) essences of yin and yang become the four seasons. The dispersed (san) essences of the four seasons become the myriad creatures. The hot qi of yang in accumulating produces fire. The essence (jing) of the fire-qi becomes the sun. The cold qi of yin in accumulating produces water. The essence of the water-qi becomes the moon. The essences produced by coitus (yin) of the sun and moon become the stars and celestial markpoints (chen, planets).Huai-nan-zi, 3:1a/19[edit] Traditional Chinese medicineFurther information: Traditional Chinese medicine and AcupunctureTraditional Chinese medicine (TCM) asserts that the body has natural patterns of qi that circulate in channels called meridians.[20] In TCM, symptoms of various illnesses are believed to be the product of disrupted, blocked, or unbalanced qi movement through the body's meridians, as well as deficiencies or imbalances of qi in the Zang Fu organs.[21] Traditional Chinese medicine often seeks to relieve these imbalances by adjusting the circulation of qi using a variety of techniques including herbology, food therapy, physical training regimens (qigong, tai chi chuan, and other martial arts training),[22] moxibustion, tui na, and acupuncture.[23][edit] Scientific investigationThere have been a number of studies of qi, especially in the sense used by traditional Chinese medicine and acupuncture. These studies have often been problematic, and are hard to compare to each other, as they lack a common nomenclature.[24] Some studies claim to have been able to measure qi, or the effects of manipulating qi, such as through acupuncture[citation needed], but the proposed existence of qi has been rejected by the scientific community.A United States National Institutes of Health consensus statement on acupuncture in 1997 noted that concepts such as qi "are difficult to reconcile with contemporary biomedical information."[25] In 2007 the MD Anderson Cancer Center at the University of Texas published an article [26] covering the concepts by which qi is believed to work and research into possible benefits for cancer patients. A review[27] of clinical trials investigating the use of internal qigong for pain management found no convincing evidence that it was effective.[edit] Feng shuiMain article: Feng shuiThe traditional Chinese art of geomancy, the placement and arrangement of space called feng shui, is based on calculating the balance of qi, interactions between the five elements, yin and yang and other factors. The retention or dissipation of qi is believed to affect the health, wealth, energy level, luck and many other aspects of the occupants of the space. Attributes of each item in a space affect the flow of qi by slowing it down, redirecting it or accelerating it, which is said to influence the energy level of the occupants.One use for a Luopan is to detect the flow of qi.[28] The quality of qi may rise and fall over time, feng shui with a compass might be considered a form of divination that assesses the quality of the local environment.[edit] Martial artsMain article: Nei JingIt has been suggested that Nei Jing be merged into this article or section. (Discuss) Proposed since January 2010.
Qi is a didactic concept in many Chinese, Korean and Japanese martial arts. Martial qigong is a feature of both internal and external training systems in China[29] and other East Asian cultures.[30] The most notable of the qi-focused "internal" force (jin) martial arts are Baguazhang, Xing Yi Quan, T'ai Chi Ch'uan, Snake Kung Fu, Dragon Kung Fu, Lion Kung Fu, Aikido, Aikijujutsu, Kyudo, Hapkido, jian and katana swordplay, Lohan Chuan, Shaolin Kung Fu, Liu He Ba Fa, Buddhist Fist, and some forms of Karate and Silat.Demonstrations of qi or ki power are popular in some martial arts and may include the immovable body, the unraisable body, the unbendable arm and other feats of power. All of these feats can alternatively be explained using biomechanics and physics.[31][32]
Respiratory rateFrom Wikipedia, the free encyclopediaJump to: navigation, searchThis article is about the measurement of breathing. For the parameter used in ecological and agronomical modelling, see respiration rate.Respiratory rate (Vf, Rf or RR) is also known by respiration rate, pulmonary ventilation rate, ventilation rate, or breathing frequency is the number of breaths taken within a set amount of time. Typically within 60 seconds.There is limited research on monitoring respiratory rate. However it is not yet proven whether or not this is due to age or environment and these studies have focused on such issues as the inaccuracy of respiratory rate measurement and respiratory rate as a marker for respiratory dysfunction.Contents[hide] 1 Measurement 2 Normal range 2.1 By Age 3 Minute volume 4 Diagnostic value 5 See also 6 References
[edit] MeasurementThe human respiration rate is usually measured when a person is at rest and simply involves counting the number of breaths for one minute by counting how many times the chest rises. Respiration rates may increase with fever, illness, OR other medical conditions. When checking respiration, it is important to also note whether a person has any difficulty breathing.Inaccuracies in respiratory measurement have been reported in the literature. One study compared respiratory rate counted using a 90 second count period, to a full minute, and found significant differences in the rates.[citation needed] Another study found that rapid respiratory rates in babies, counted using a stethoscope, were 6080% higher than those counted from beside the cot without the aid of the stethoscope.[citation needed] Similar results are seen with animals when they are being handled and not being handledthe invasiveness of touch apparently is enough to make significant changes in breathing.[edit] Normal rangeAverage respiratory rate reported in a healthy adult at rest is usually given as 12-18 breaths per minute (Vf) [1][2] but estimates do vary between sources, e.g., 1220 breaths per minute, 1014,[3] between 1618,[4] etc. With such a slow rate, more accurate readings are obtained by counting the number of breaths over a full minute.[edit] By AgeAverage Respiratory Rates (Vf) By Age: Newborns: 30-40 breaths per minute Less Than 1 Year: 30-40 breaths per minute 1-3 Years: 23-35 breaths per minute 3-6 Years: 20-30 breaths per minute 6-12 Years: 18-26 breaths per minute 12-17 Years: 12-20 breaths per minute Adults Over 18: 1220 breaths per minute.[edit] Minute volumeRespiratory minute volume is the volume of air which can be inhaled (inhaled minute volume) or exhaled (exhaled minute volume) from a person's lungs in one minute.[edit] Diagnostic valueThe value of respiratory rate as an indicator of potential respiratory dysfunction has been investigated but findings suggest it is of limited value.One study found that only 33% of people presenting to an emergency department with an oxygen saturation below 90% had an increased respiratory rate.[citation needed] An evaluation of respiratory rate for the differentiation of the severity of illness in babies under 6 months found it not to be very useful. Approximately half of the babies had a respiratory rate above 50 breaths per minute, thereby questioning the value of having a "cut-off" at 50 breaths per minute as the indicator of serious respiratory illness.It has also been reported that factors such as crying, sleeping, agitation and age have a significant influence on the respiratory rate.[citation needed] As a result of these and similar studies the value of respiratory rate as an indicator of serious illness is limited.
SpiritFrom Wikipedia, the free encyclopediaJump to: navigation, searchFor the alcoholic beverage or "spirits", see Distilled beverage. For other uses, see Spirit (disambiguation).This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. (June 2009)
Look up spirit in Wiktionary, the free dictionary.
The English word spirit (from Latin spiritus "breath") has many differing meanings and connotations, most of them relating to a non-corporeal substance contrasted with the material body.The spirit of a living thing usually refers to or explains its consciousness. The notions of a person's "spirit" and "soul" often also overlap, as both contrast with body and both are imagined as surviving the bodily death in religion and occultism,[1] and "spirit" can also have the sense of "ghost", i.e. a manifestation of the spirit of a deceased person.The term may also refer to any incorporeal or immaterial being, such as demons or deities, in Christianity specifically the Holy Spirit experienced by the disciples at Pentecost.Contents[hide] 1 Etymology 2 Metaphysical and metaphorical uses 2.1 Metaphysical contexts 2.2 Metaphorical usage 3 Related concepts in other languages 4 See also 5 References 6 Further reading
[edit] EtymologyThis section does not cite any references or sources. Please help improve this section by adding citations to reliable sources. Unsourced material may be challenged and removed. (November 2010)
The English word spirit comes from the Latin spiritus, meaning "breath", but also "spirit, soul, courage, vigor", ultimately from a Proto-Indo-European *(s)peis. It is distinguished from Latin anima, "soul." In Greek, this distinction exists between pneuma (), "breath, motile air, spirit," and psykh (), "soul."The word "spirit" came into Middle English via Old French. The distinction between soul and spirit also developed in the Abrahamic religions: Arabic nafs () opposite r (); Hebrew neshama ( nmh) or nephesh (in Hebrew neshama comes from the root NM or "breath") opposite ruach ( ra).[edit] Metaphysical and metaphorical usesEnglish-speakers use the word "spirit" in two related contexts, one metaphysical and the other metaphorical.[edit] Metaphysical contextsIn metaphysical terms, "spirit" has acquired a number of meanings: An incorporeal but ubiquitous, non-quantifiable substance or energy present individually in all living things. Unlike the concept of souls (often regarded as eternal and sometimes believed to pre-exist the body) a spirit develops and grows as an integral aspect of a living being.[citation needed] This concept of the individual spirit occurs commonly in animism. Note the distinction between this concept of spirit and that of the pre-existing or eternal soul: belief in souls occurs specifically and far less commonly, particularly in traditional societies. One might more properly term this type/aspect of spirit "life" (bios in Greek) or "aether" rather than "spirit" (pneuma in Greek). A daemon sprite, or especially a ghost. People usually conceive of a ghost as a wandering spirit from a being no longer living, having survived the death of the body yet maintaining at least vestiges of mind and of consciousness. In religion and spirituality, the respiration of a human has for obvious reasons become seen as strongly linked with the very occurrence of life. A similar significance has become attached to human blood. Spirit, in this sense, means the thing that separates a living body from a corpseand usually implies intelligence, consciousness, and sentience. Latter-day Saint prophet Joseph Smith Jr. taught that the concept of spirit as incorporeal or without substance was incorrect: "There is no such thing as immaterial matter. All spirit is matter, but it is more fine or pure, and can only be discerned by purer eyes."[2] In some Native American spiritual traditions, the Spirit, or 'Great Spirit', is a term for the Creator. Various forms of animism, such as Japan's Shinto and African traditional religion, focus on invisible beings that represent or connect with plants, animals (sometimes called "Animal Fathers)", or landforms (kami)[citation needed]: translators usually employ the English word "spirit" when trying to express the idea of such entities. Individual spirits envisaged as interconnected with all other spirits and with "The Spirit" (singular and capitalized). This concept relates to theories of a unified spirituality, to universal consciousness and to some concepts of Deity. In this scenario all separate "spirits", when connected, form a greater unity, the Spirit, which has an identity separate from its elements plus a consciousness and intellect greater than its elements; an ultimate, unified, non-dual awareness or force of life combining or transcending all individual units of consciousness. The experience of such a connection can become a primary basis for spiritual belief. The term spirit occurs in this sense in (to name but a few) Anthroposophy, Aurobindo, A Course In Miracles, Hegel, Ken Wilber, and Meher Baba (though in his teachings, "spirits" are only apparently separate from each other and from "The Spirit.")[3] In this use, the term seems conceptually identical to Plotinus's "The One" and Friedrich Schelling's "Absolute". Similarly, according to the panentheistic/pantheistic view, Spirit equates to essence that can manifest itself as mind/soul through any level in pantheistic hierarchy/holarchy, such as through a mind/soul of a single cell (with very primitive, elemental consciousness), or through a human or animal mind/soul (with consciousness on a level of organic synergy of an individual human/animal), or through a (superior) mind/soul with synergetically extremely complex/sophisticated consciousness of whole galaxies involving all sub-levels, all emanating (since the superior mind/soul operates non-dimensionally, or trans-dimensionally) from the one Spirit. Christian theology can use the term "Spirit" to describe God, or aspects of God as in the "Holy Spirit", referring to a Triune God (Trinity)(cf Gospel of Matthew 28:19). "Spirit" forms a central concept in pneumatology (note that pneumatology studies "pneuma" (Greek for "spirit") not "psyche" (Greek for "soul") as studied in psychology). Christian Science uses "Spirit" as one of the seven synonyms for God, as in: "Principle; Mind; Soul; Spirit; Life; Truth; Love"[4] Harmonism reserves the term "spirit" for those that collectively control and influence an individual from the realm of the mind.[edit] Metaphorical usageThe metaphorical use of the term likewise groups several related meanings: The loyalty and feeling of inclusion in the social history or collective essence of an institution or group, such as in school spirit or esprit de corps. A closely related meaning refers to the worldview of a person, place, or time, as in "The Declaration of Independence was written in the spirit of John Locke and his notions of liberty", or the term zeitgeist, meaning "spirit of the age". As a