The Grog, Issue 43 2015
-
Upload
the-grog-ration -
Category
Documents
-
view
222 -
download
2
description
Transcript of The Grog, Issue 43 2015

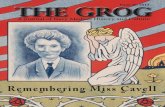
A Journal of Navy Medical History and Culture
Issue 43, 2015
T he Sitka Chronicles 1867-1912

THE GROGA Journal of Navy Medical History and CultureIssue 43, 2015
Office of Medical HistoryCommunications DirectorateBureau of Medicine & Surgery7700 Arlington BlvdFalls Church, VA 22042
Editor and Historian:André B. Sobocinski
Archivist:Mike Rhode
Oral History Editor:COL Dick Ginn, MSC, USA (Ret.)
Introduction
2 Issue 43, 2015
The Last Frontier. Land of the Mid-night Sun. Seward's Folly. Since 1867 when it was purchased from
Tsar Alexander II for a meager $7.2 million, Alaska has been known by many names. Throughout it all, it has held our fascination as a land of beauty, ancient traditions, natu-ral resources and, more recently, as a reality TV show dynamo. Although unconfirmed, it is believed by some that everytime a bell rings Alaska gets a new reality show. Long before it became the 49th U.S. State in 1959, and even before it was granted ter-ritory status in 1906, Alaska was a "U.S. Department." From 1867 to 1884, when its first civilian governor was appointed, the Department of Alaska was governed by a succession of Army, Cutter Service (Coast Guard) and Navy personnel from the vil-lage of Sitka. Located on Alaska's south-eastern coast, Sitka was an ancestral home of the Tlingit people and capital of Russian-America. Until 1906, when Juneau became the territorial capital, Sitka was Alaska's cultural and political center. Today, Sitka may best be known for its Russian roots, its totem poles, as home to the oldest national park in the state and being the largest city by area in the United States (some 4,811 sq. miles!) In this edition of THE GROG, we look back at the Navy's unique history in Sitka—from the arrival of USS Jamestown and Cdr. Beardslee's "commandership" of Alaska to the establishment of the little-known U.S. Naval Hospital Sitka. We follow this with a bountiful array of original articles. As always, we hope you enjoy this tour on the high seas of Navy Medicine’s past!
Images of Cmdr. Lester Beardslee (center), officers and crew of USS Pinta at Sitka (top left and bottom right), USS James-town (bottom left) and Tlingit tribesmen in Sitka (top right).Photos courtesy of NHHC and National Park Service

THE GROG is a free publication of the Communications Directorate dedicated to the promotion and preservation of the history and culture of the Navy Medical Department. Articles and information published in THE GROG are historical and are not meant to reflect the present-day policy of the Navy Medical Department, U.S. Navy, and/or the Department of Defense.
page 4...The Navy in Sitka
page 14...Battle for the Aleutians
THE GROGA JOURNAL OF NAVY MEDICAL HISTORY AND CULTURE
page 22...Capt. Mary Keating
THE GROG 3
Features
The Sitka Chronicles, U.S. Navy in Sitka, Alaska, 1867-1912.............................................
Looking Back on the Career of Capt. Mary Keener, Aviation Physiologist....................................
Showcase
The Ballad of a Dog Named "Jack"by Dr. Nelson M. Ferebee..............................................................
The Whale, Wolf, Raven and Dog; or the Legend of Mount Edgecumbeby Dr. Nelson M. Ferebee...............................................................
Navy Medicine in Alaska..............................................................
Navy Medicine in the Aleutian Campaign...................................
Oral Histories: "Most Legacies are Not Legacies"An Excerpt of an Oral History with Rear Adm. Rowley..............
The Curious Tale of Naval Hospital Dublin, Ga.,.......................
The Navy Medical Laboratory School, 1878-79: A Culture Grows in Brooklyn.......................................................
page 4
page 22
page 6
page 11
page 12
page 14
page 26
page 30
page 34

The Sitka Chronicles
4 Issue 43, 2015

THE GROG 5
The U.S. Navy in Sitka,
Ala ska ,1867 -1912“The town is beautifully situated on comparatively flat land on one of the finest harbors in Alaska. The bay is surrounded by snow-capped mountains from which streams flow through the town and furnish ex-cellent drinking water.”
~Passed Assistant Surgeon Allan Stuart, USN1
When U.S. Secretary of State William Seward agreed to purchase Alaska from the
Russian Czar for $7.2 million dollars (roughly $114 million in today’s mon-ey), the American press lampooned the deal as “Seward’s Folly” and “Seward’s Icebox.” The first U.S. first territorial ex-pansion since the end of the Civil War was considered a mixed bag at best and its distance from the contiguous states “impractical” for some prospective set-tlers. But in time, the discovery of gold, oil and its inherent arctic beauty would thaw the cold rhetoric and mispercep-tions of the Alaskan territory. On October 18, 1867, the U.S. Army raised the (then) 37-star U.S. flag above the old Russian Governor’s house in Sit-ka, Alaska in a ceremony marking the transfer. For the next 17 years—until a civilian government could be estab-lished—Alaska (sometimes referred to as the “Department of Alaska”) would be governed by a succession of Army, Cutter Service and finally Navy officers. The military's mission in this new land was clear and distinct: maintain order and survey the new territory.
Until 1906, when Juneau became the Alaskan capital, Sitka was its unequivo-cal cultural and civic center. Located on Baranof Island along the southeastern coast, Sitka is in a region as wealthy in its history as its traditions. Its name is a corruption of “Shee At’ika,” a refer-ence to the clan of Tlingit Kiks.adi who “lived outside the village of Shee.” The area’s cedar forests, rivers and snow-capped mountains have been home to the Tlingit people for thousands of years. To this day, totem poles—one of Tlingit’s cultural symbols—still punc-tuate the landscape in and around Sitka. The island’s namesake, "Baranof," is a vestige of Sitka’s more recent European past. As far back as the late eighteenth century, Sitka was the center of the Rus-sian fur trade, whaling industry and capital of Russian-America. In 1799, Alexander Baranof (or Baranov), the head of the Russian-American Compa-ny, helped establish a Slavic presence in Sitka—which the Russians called “New Archangel” (Novoarchhangelsk). Es-tablishing a presence in this new land did not come without some adversity. The early years of Russian-America
1. Stuart, A. "Report on Sanitary Conditions in Connection with the Naval Hospital Sitka, Alaska." Report of the Surgeon-General. Washington, DC: GPO. p183.

6 Issue 43, 2015
was marked by bloody battles with the native Tlingits. In 1804, Baranof and a force that included the Aleuts and other native tribes fought with and quelled Tlingit resistance in the Battle of Sitka. The battlefield, still in existence, is now part of Sitka National Park—Alaska’s oldest and smallest national park. When the Americans moved into Sit-ka they found a Western frontier town more than a little seasoned by Russian influence. To this day, the Russian Or-thodox Church, a replica of the original St. Michael's Church that burned down in 1966, is planted in the very center of the old town.2
THE NAVY ARRIVES IN SITKA During the transfer ceremonies in 1867 the sloop-of-war USS Jamestown was moored in Sitka’s harbor for the festivities. On June 14th, 1879 the ship returned under the command of Cmdr. Lester Beardslee (1836-1903), a 29-year veteran of the service who had served with Commodore Perry on his mission to Japan in 1853. Just as the Army and the Cutter Service had done over the previous twelve years, the Navy was there to maintain “harmonious rela-tions” amongst the polyglot of white settlers, Russians, native populations, and “creoles” (a term used by the Navy to describe locals of “mixed” heritage). The Jamestown’s medical officer—and for a time Sitka’s lone physician—Passed Assistant Surgeon Nelson Fere-bee (1849-1917) called Sitka a scenic, but “dead place.”3
“The town was built principally on one street which ran along the water front. The houses were small and low, the Russian houses being generally built of logs with double windows and heated with large ovens…Near the main land-ing was the house formerly occupied by the Russian governors. It was a large heavily built structure of wood and was perched on the top of a rock about 70 feet above the street. In our time it was much out of repair…From the platform around this castle a fine view was had on a summer day. At your left was the harbor studded with rocks and green is-lands, beyond and several miles away a long low island and to the right forming
the entrance to the sound was Mount Edgecombe [sic], an extinct volcano, snowcapped and closely resembling Fu-jiama in Japan.”4
During the Jamestown’s 26-month stay at Sitka, Beardslee acted as the De-partment of Alaska’s “Commander” and supreme authority. Years later, Beard-slee would remember that the Navy’s presence may have been the result of false information created by some lo-cals. “White men began to come to this country, among them both good and bad men; the last, seeing riches in the country wished to keep it for them-selves, so they wrote false letters and
2. Sitka National Park Unigrid Brochure. National Park Service. Department of the Interior.3. Nelson M. Ferebee Papers, Collection No. 404. East Carolina Manuscript Collection, J.Y. Joyner Library, East Carolina University, Greenville, NC. The term "Passed Assistant Surgeon" denotes that physician has passed his examination boards to be a Surgeon but is awaiting for a billet.
USS Jamestown arrived in Sitka in 1879 commencing the town's naval period. From 1879 to 1884, captains of the ships Jamestown, Adams, and Pinta would serve as "Commanders of the Alaskan Department."Courtesy of the Navy Art Collection

THE GROG 7
5. Beardslee, Lester. "Operations of the Navy." Papers relating to the American Occupation. Alaska Boundary Tribunal: The Case of the United States before the Tribunal Convened at London Under the Provisions of the Treaty between the United States of America and Great Britain Concluded January 24, 1903. Washington, DC: Government Printing Office, 1903. p372.
the white men read that the country of Alaska was [a] ‘bad land’ and the Indi-ans a dangerous, treacherous lot of men, and the whites could not stay unless the Government sent a warship or soldiers to protect them. Some of these reports were true, for the white men and Indi-ans did not understand each other, nor how to get along together. “The Government sent the warship asked for, and selected me to command it, and it told me to protect the whites, and Indians who desired it, from the Indians….At first my work was very hard. Bad Indians and bad white men gave me much trouble, and the good men would not assist me, but stood and looked on, because they did not know me; but as time passed and they saw that the war ship was the enemy of the bad men only, and a friend of the good ones, these [good men]…began to help me.”5 After several months, Beardslee and the Navy contingent would establish control over community affairs. The Navy took a census, appointed an In-dian police force, established a Marine Guard House and Barracks, helped in-stitute better sanitary conditions, im-plemented a period of prohibition and made school attendance mandatory for the town’s children. The Navy numbered the houses and compelled the local children to attend a new mission school operated by a Miss Olinda Austin in April 1880. According to Dr. Ferebee the Navy had tin badges placed outside of each home bearing
Like many Navy ships the Jamestown had its own animal shipmate onboard, in this case a dog named “Jack.” The ship’s doctor, Passed Assistant Surgeon Nelson Ferebee would serve as one of the dog’s handlers. Years later he would remember ol' Sitka Jack.
***
Jack had been a pack dog and, as his face showed, the veteran of many battles. Ordinarily, he would remain quietly on
board. But there would come times when Jack would go to the gangway and after looking over at the village for a while, jump into the first boat going ashore. Soon you would see Jack coming through the stockade down the beach. Jack would take no notice of a single dog, but make his way to where a half a dozen or more were lying asleep in the sunshine. Then he would go and begin making insult-ing remarks. In a few minutes he would be in the midst of a fight which delighted the Irish heart. After a while some boat would bring Jack back to the ship to be cured of his wounds and for a month or so Jack would be peaceable. He always left a number of wound-ed behind. •
The Ballad of a Dog Named "Jack"

8 Issue 43, 2015
6. Ferebee Papers7. Andrews, C.L. The Historical Outpost of the Northwest Coast. (originally published in 1922);Timeless Classic Books, 2010.8. Ferebee Papers9. Ibid.10. During the naval adminsitration of Alaska, Future Marine Commodant George Barnett and Navy Lt. George Thorton Emmons, served in Sitka and both expressed a lively interest in local customs. Emmons a draftsman would later become a noted collector, ethnog-rapher and expert of Tlingit culture.
the house number, the number of chil-dren within, their gender and the order of birth. “Then with the assistance of the In-dian police, we went among them and arranged the ... children of school age in regular order, putting a tag around each one’s neck. These [tags] were re-quired ...[to be worn] at all times. To encourage the children to take care of the tags, a reward was promised to those who kept them on for six months. The school teachers were given a list arranged so that they could detect ab-sentees very quickly…the seats in the school house were arranged so that the children of each house sat together in regular order.” The heads of families were held responsible for absenteeism, but Ferebee does not mention what the repercussions were, if any.6
In April 1880, the population of Sit-ka numbered 444—92 by birth, 123 by naturalization, and 229 by treaty.7 Sitka’s census would swell to as much as 1,500 in the colder months as native tribes, prospectors and others would winter in town. As one can imagine, with the larger population came the increased risk of conflict Like any other frontier town at the time, fights and shooting brawls would increase exponentially with the presence of alcohol. Even though it was illegal to import alcohol into the territory, locals would concoct their own noxious brews like “Hooch-enoo” or “Hooch” out of coarse sugar,
molasses and other materials available to them. In 1879, the Navy destroyed 38 stills, and 150 gallons of liquor. The Navy was responsible for keep-ing order and adjudicating when nec-essary. In one case when a man was shot and killed breaking into another man’s house the Navy’s verdict was “justifiable homicide.”8
During the naval period, officers would occasionally hold masquerade parties with local women, and sponsor lectures and theatricals in the old Rus-sian Governor’s house. In the winter months, recreational activities includ-ed ice skating and something called “snow tramping.” As the temperatures rose, fishing, hunting and canoeing proved popular among Sailors and Ma-rines alike. The Navy’s diet in Sitka consisted of a local bounty of fish, venison, grouse and ducks. As one can expect salmon would become a staple food as well. Dr. Ferebee later recollected, “During the salmon season our men salted down a large quantity of fish. Smoked salmon bellies were highly esteemed. I know nothing which goes so well with a glass of beer, ... salmon creates a taste for a glass of beer and a glass of beer brings a wish for a bit salmon.”9
Jamestown departed Alaskan wa-ters for the last time in 1881 only to be relieved by the screw sloop Adams (1881-1883), and the screw tug USS Pinta (1883-1897).10 Six naval offi-
cers would follow Beardslee’s stead as governor through 1884. On May 17, 1884, the Department of Alaska was reorganized as the “District of Alaska” and the Pinta’s commanding officer, Lt. Cmdr. Henry Nicohls relinquished his "commandership" duties. On July 4, 1884, Joseph Henry Kinkaid, a former Postmaster General under President Andrew Johnson, took office as the first civilian governor of Alaska. Twenty-two years later the District of Alaska was redesignated as a “U.S. Territory” and granted a Congressional Delega-tion. On January 3, 1959, Alaska be-came the 49th state in the Union.
NAVY MEDICINE IN SITKA Even after the Navy’s governorship ceased, the Navy and Marine Corps re-mained a dominant presence in Sitka into the twentieth century. In addi-tion to the Marine Barracks, the Navy maintained a medical presence cater-ing to the military and, at times, the civilian population. In his memoir, Navy physician Nel-son Ferebee makes reference to the existence of a naval dispensary being established in Sitka with the arrival of Jamestown in 1879. Certainly, from 1879 through the early twentieth cen-tury Navy physicians attached to the ships Adams, Pinta and later the Naval Hospital Sitka would be called to not only take care of military and govern-ment personnel, but also locals.

THE GROG 9
11. Willson W,G.G. "Sanitary Report Upon the USS Pinta: Summary of Cruise and General Hygiene." Report of the Surgeon-General of the U.S. Navy. Washington, DC: GPO. 1885. pp290-295.12. Fitts, Herbert A. "Sanitary Report USS Pinta (Fourth Rate), Sitka Alaska." Annual Report of the Surgeon General of the U.S. Navy. Washington, DC: GPO. 1890. pp96-97.13. Ibid.14. Braisted, William, Memorandum for the Assistant Secretary of the Navy, December 7, 1907. RG52, 114074. NARA, Wash., DC.15. Barnett, George to Bureau of Supplies and Accounts. Expenditures made by Quartermaster's Department. Marine Corps, in Territory of Alaska. May 25, 1916. RG52. 125670. NARA, Wash., DC.16. Report of the Surgeon-General of the U.S. Navy. Washington, DC: GPO. 1904. p23.
For a time, the Pinta's physician op-erated a dispensary ashore in the sec-ond floor of a building belonging to the U.S. Treasury Department. In his med-ical report from Sitka dated 1884-1885, USS Pinta’s physician W.G.G. Wilson wrote, “During the supremacy of the Navy in Alaska [1879-1884] it seems to have been the custom with various ships, from time to time in charge of the station, to furnish attendance and medicines, as far as practicable.” Wil-son continued this practice for the first month after Pinta’s arrival but after civil authority was established in 1884,
the Navy medicine would be the "last resort.”11
Wilson reported that common ail-ments suffered by the locals included pulmonary diseases like tuberculosis, and, as one would expect of any fron-tier town of the time, syphilis. Several decades before the discovery of penicil-lin, and even before the arsenic-based Salvarsan therapy, mercury-based Cal-omel ointment, pills and steam baths were still the go-to treatments for vene-real diseases. Catarrh (catarrhus epidemicus) was most common among the children of Sitka and one Navy physician noted that it was so severe that it almost resembled the influenza. Rheumatism was also listed as being common among locals.12
Whatever medical facility the Navy operated in the early years at Sitka was certainly temporary and negligible at best. In 1890, Passed Assistant Surgeon Henry Fitts of USS Pinta suggested that a permanent facility should be main-tained in Sitka for any “real and perma-nent good to be done.” He stated that the physician in charge should have authority to compel native populations, especially children, to visit. Fitts also stated that the hospital would require a nurse or medical assistant who could go to the Indian village to teach hygiene. As for who would provide these servic-es, Fitts contended that as long as a na-val vessel was stationed in Alaskan wa-
ters a naval surgeon would be naturally looked upon for assistance. It did not hurt that the naval physician in charge of the hospital was typically the only medical professional in Sitka.13
The Naval Hospital Sitka was of-ficially established by the Navy Depart-ment letter No. 5569 dated November 12, 1895. Intially, the hospital occupied the third floor of the old Russian Store-house that stood "on a pile of rocks" some 125 feet above above the water. The hospital consisted of three rooms used for a medical ward, kitchen and a dispensary/office/operating room. The Storehouse served as the Naval Hospi-tal until 1903 when the building was deemed unsafe.14 In 1903, the hospi-tal relocated to a small frame house. Four years later, by Executive Order dated January 16, 1907, the hospital relocated to the old Russian Governor’s House.15
In addition to duties with the Marine Guard, the attending Navy doctor was frequently called upon for emergency surgical work by civilians.16 The an-nual sanitation reports from the Naval Hospital Sitka lists sprains, contusions, influenza, catharrh, as well as chronic dysentery, syphilis, tuberculosis, and alcoholism as problems among the military population. In 1909, a Navy physician with the unfortunate sur-name "Grieve" reported a case of a fish-erman being admitted to the hospital
PAS Nelson M. Ferebee, USN (1849-1917) would serve as the Navy's first attending physician in Sitka.Courtesy of the Navy History and Heritage Command

10 Issue 43, 2015
with "bear bites." In his medical report, later published in the Naval Medical Bulletin (with pictures of the grisly wounds), Grieve states that the man spent 37 days at the hospital before being released. He noted that the case serves to “disprove the time-honored fallacy originating in the claim of old hunters that bears never bite man.”17
One of the additional duties of the naval hospital physician was to oversee the military cemetery nearby. The cem-etery contained the dead of generations of Soldiers, Sailors and Marines who lived and died on the Alaskan frontier
before statehood. The graves would later become part of a National Cem-etery which today holds the distinction as the oldest National Cemetery west of the Mississippi. For its entire existence, medical per-sonnel stationed at Naval Hospital Sit-ka had to contend with questions sur-rounding the facility's future. In 1902, the medical officer on duty wrote, “If it be determined to continue the present naval station, a small hospital favor-ably situated within easy reach of the barracks should be provided and is ur-gently needed. The present hospital can
Officers of USS Pinta in Sitka, 1889. Standing on the far left is Passed As-sistant Surgeon Herbert Fitts who would later serve at the helm of the Naval Hospital Sitka, Alaska.Courtesy of the Navy History and Heritage Command
17. "Bitten by a Bear." Forest and Stream: A Journal of Outdoor Life, Travel, Nature Study, Shooting, Fishing, Yachting. May 15, 1909; LXXII. p77618. Report of the Surgeon-General of the U.S. Navy. Washington, DC: GPO. 1902. p15.19. Barnett, George. Expenditures. 1916.
hardly be said to deserve the dignity of that name.”18 The Naval Station at Sitka closed in March 23, 1912. The hospital and Marine Corps Guard House prop-erty was turned over to the Depart-ment of Interior and used, for a time, as a home for “indigent pros-pectors.”19
Although the Navy would operate coaling stations in Alaska until the 1920s, it was not until the late thir-ties and early forties that it returned in full force. •

THE GROG 11
The Story about the Whale, Dog, Wolf, Raven; or the Legend of Mount EdgecumbeAs told by Passed Assistant Surgeon Nelson McPherson Ferebee
The crater [of Mount Edgecumbe] is bowl-shaped and in summer is fre-quently free of snow. The deer seem to like to go there. The Indian leg-end is that in days long ago there was an Indian who had a very beautiful
wife of whom he was very jealous, so much so that he would not let her be seen by man or beast. One day he saw his children peeping at her and at once killed them. The sorrowing mother wandered to the shore and while standing there was seen by a whale, who asked the cause of her grief. Being told that she was now childless, the whale told her to swallow a small pebble which he threw upon the beach with his tail. She did so and in time was delivered a son. The father repenting him of his hasty act became very fond of this boy and allowed him to live. He was called the "Son of the Whale." After long years this boy, now man, found a beautiful maiden, whose father kept locked in three chests-the Sun, Moon and Stars. The chests were guarded by a dog. The legend was that should these chests be opened by any descendant [sic] of the father, the father would at once die. The dog had been so trained that he would not allow the daughter to approach the chests. To prevent desecendents [sic] [from opening up the draw-ers] the father would not allow his daughter to go out of his sight. The maiden saw the young man and loved him. A wolf told her to eat the blades of certain grass and she would be invisible. She did so and there was born to them a son and a daughter. The grandfather became very fond of his grandson and gave him all he asked. The dog also became his friend allowing the child to play with the chests as he wished, yet he was not allowed to open them. One day a raven said to the boy that he should try to see inside the boxes. He did so, but was refused. The boy began to cry, so at last to please him one of the boxes was given to him. He carried it out and when he opened it the Star appeared in the sky, then to get another he pretended sickness, from this box came the Moon. Now the old man put the dog to watch the last box, but the raven coming near dropped a fish which the dog ran to eat, the boy at once opened the box and lo, the Sun was in the sky and the old grandfather, Darkness, was dead. So came the four totems of the Tlinkets [sic], whale, wolf, dog, and raven. After a time there came a deluge and all were destroyed but a few on a raft. The raft broke in halves leaving the sister alone on one half. She, taking the form of a raven, flew to the top of Mount Edgecombe[sic] and went down into the crater, so that now she bears up the earth there. The Indians say, when the raven calls around the summit of the mountain and the wolf howls, it is the brother and sister calling each other. •
SourceNelson M. Ferebee Papers, Collection No. 404. East Carolina Manuscript Col-lection, J.Y. Joyner Library, East Carolina University, Greenville, NC.Raven Totem, Sitka, Alaska.
Courtesy of National Park Service

12 Issue 43, 2015
Aerial Naval Clinic, Adak, Alaska in 194309-5000-3All photos from the BUMED Archives
"Navy Medical Battalion," Adak, March 28, 194409-5000-2

THE GROG 13
A Look Back: Navy Medicine in Alaska:
The Navy returned to Alaska in full-force during World War II establishing operating stations in Dutch Harbor, and Adak in the Aleutian Islands. Adak was a key supply and logistical location for the U.S. military during operations against Japanese forces. The Navy Medical Department first established a clinic in Adak in 1943 which closed at the end of the war. In 1950s, a Naval Air Station and Naval Hospital were established on Adak. These facili-ties were disestablished on March 31, 1997.
Navy nurses standing outside the Nurse Corps Quarters in Adak, ca. 194309-5000-7
Navy nurses hiking in extinct volcanoes in the Aleutian Islands, December 7, 194309-5000-4

14 Issue 43, 2015
Navy Medicine in the Aleutian Campaign,
1942-1943
In World War II, Alaska faced its greatest military threat in what has been called the Battle of the Aleutians (June 1942 to August 1943). The Aleutians are a chain of volcanic islands that jut out from Alaska into the North Pacific. In June 1942, Japanese Imperial forces
advanced on the Aleutians, bombing the naval operating base at Dutch Harbor and landing forces in the western islands of Attu and Kiska. Following U.S. and Canadian counterattacks on Japanese positions, Allied forces recaptured Attu in May 1943; and in August 1943, retook Kiska. Throughout the campaign, Navy medical personnel served aboard ships patrolling the Alas-kan waterways and at the operating bases in Adak and Dutch Harbor. The following is an ex-cerpt on the medical presence in the Aleutian campaign from the unpublished Administrative History of the Navy Medical Department in World War II (1946).
Ice Floes, Kodiak (1943)By Edward T. GrigwarePainting, Oil on BoardAll artwork courtesy of Navy Art Collection

THE GROG 15
Paralleling the South Pacific Solomons campaigns was an-other American offensive far
to the North. In the summer of 1942 the Japanese had occupied several of the islands in the Aleutian group, the most important of which were Attu and Kiska. By May 1943, [the] United States forces were ready to attempt the reconquest of these Japanese outposts. D-day for the capture of Attu ("Opera-tion Landcrab") was set for May 11th
1943.
ATTU On the morning ... [the] May 11th
landings were made on the north coast of Attu, the American forces proceed-ed inland. In the afternoon other land-ings were made at Massacre Bay,1 and also at Holtz Bay.2 These landings were covered by American naval forces, and in the bitter fighting which followed, various naval units assisted Army troops by furnishing fire support and air cover. Enemy attacks on American naval forces were ineffective. The story of naval medicine at Attu was largely the story of the work of the medical staff aboard the individual ships. There was the attack transport, USS J. Franklin Bell [APA-16], which received her first experience against the enemy at Attu. The J. Franklin Bell participated in the landings on the northern sector. Between May 11 and 16, the beach party of this ship was called upon to evacuate 80 casualties. Torpedoes were fires by the Japanese at the vessel, and the necessity for haste during one torpedo alarm resulted in one man being fatally crushed by
the falling of a landing boat. This and other shipboard and boat casualties raised the total to 100. Exposure to foul weather complicated battle wounds and in many cases was the only dis-abling factor. This situation was aggra-vated by time-consuming difficulties in getting casualties to the beach for transportation to the ship. All casual-ties were transferred at Adak. At Attu, 260 cases of immersion foot were treated aboard the USS Heywood (AP-12). This condition was a result of cold, constriction from all-leather boots, and moisture. The patients came aboard within 36 hours after they had been in fox holes on the snow-covered slopes of the mountains from four to seven days. All the men were placed in a single troop compartment space where the unheated atmosphere remained at about 50 degrees F. Here the men were given routine nursing care and their feet were exposed to the compartment temperature. Over a period of several days the temperature was elevated to comfortable room temperature. Dur-ing the first day they all experienced a great deal of pain, which in most cases was controlled with codeine and aspi-rin. After about a week, the swelling commenced to subside and devitalized tissue began demarcating as a dry gan-grene. Cases in which evidence of gan-grene appeared usually involved one or several toes. There were three cases in all observed which were delimited at about the head of the malleoli. There was one case of particular in-terest which involved a man who had been shot through the ankle. Shortly after the injury, his boot was removed
from the injured foot. The boot on the other foot was not removed. [He was evacuated three days later]. The foot which was injured and from which the boot had been moved showed no evidence of immersion foot, while the other foot showed extensive damage typical of immersion foot. As compared with the patients ar-riving on board the Heywood at subse-quent operations, there were very few cases of initial shock seen at Attu and the infection rate was extremely low. However, the casualties at Attu were shivering and complaining of the cold. The USS Indianapolis (CA-35), al-though neither hit nor damaged by the enemy, was struck by another Ameri-can vessel, and part of the hull in the operating room was ripped away. On the same evening that this accident oc-curred, a surgical emergency arose and the operating room, with canvas cover-ing the hole in the hull, had to be used. It was the experience of the officers and men of the Indianapolis that no more arduous activity could be devised than patrol and blockade duty in the Aleu-tians. Physiologically and psychologi-cally it was found to be more wearing than actual combat. The medical officer found that the almost complete absence of respiratory infections in the Aleu-tians area is medically its only desirable feature. Another unfortunate accident which befell the Indianapolis was being struck with an abnormally high wave which washed nine men overboard. Two of the men were recovered, suffer-ing from temporary exhaustion only. The medical organization of the USS Raleigh (CL-7) could be considered
Ice Floes, Kodiak (1943)By Edward T. GrigwarePainting, Oil on BoardAll artwork courtesy of Navy Art Collection
1. Southeastern coast of Attu, Aleutian Islands.2. Inlet on northeast coast of Attu.

16 Issue 43, 2015
typical of the cruisers participating in this operation and although this ship was not engaged by any enemy forces, its medical organization proves of in-terest. There were three-battle dressing stations aboard, the forward battle-dressing station being located in the officers’ ward room on the main deck. The after battle-dressing station was located on the main deck between the crew’s wash rooms. The captain’s cabin on the weather deck was converted into an auxiliary battle-dressing station. In the forward or main battle-dressing station, an additional surgical light was installed and a permanent metal bat-tle-dressing locker was placed behind the tripod on the port side. A similar locker was located on the starboard, to be available in the event of an emer-gency. The facilities for handling casu-alties, surgical and medical equipment, lights and water were adequate in all battle-dressing stations. Because of pilfering, the morphine was removed from all first-aid boxes and the syrettes were given to responsible personnel in anticipation of an emergency. By the time of the Attu campaign, tannic acid jelly had likewise been removed and replaced with petrolatum, which was then being used on all burn cases on the USS Raleigh. Constant and ad-equate first-aid instruction was given systematically to officers and crew, casualty drill problems having been exercised during general quarters and damage control drills. First-aid in-structions were clearly augmented by slides and movies which were supple-mented by practical demonstrations. Generally speaking, the morbidity from any source was at a new low in the Aleutians area. It has been suggest-
ed that the confinement to ship and lack of contact with civilization, except with the armed forces in the area, was good preventive medicine. Aboard the USS Spica (AK-16) there were no fatalities or serious injuries—in spite of the loading and unloading of dangerous cargo in foul weather and rough seas, the use of various types of landing craft, and help that was often inexperienced. Credit for these successful operations was due to the efficient officers’ handling. On the Spica, besides a sick bay containing six permanent berths and a small operat-ing dispensary, there was an excellent operating room containing adequate sterilizing equipment and surgical in-struments to perform the necessary major operations. As a result, the Spica was able to give necessary aid to ships and small craft unable to reach shore in
severe weather, besides giving proper care to the war casualties placed aboard and the casualties and surgical cases oc-curring in personnel who had recently been placed ashore and were temporari-ly with sick bay facilities. For those days, during the period of May 21 to June 5, 1943, the medical officer of the Spica, together with the Hospital Corpsmen and Hospital Strikers, had to assist war casualties aboard the Heywood. This medical officer and the Corpsmen also assisted aboard the [U.S. Army Trans-port Ship] David W. Branch. Aboard the latter, a soldier who had suffered a bayonet wound of the lower abdomen and had part of his omentum protrud-ing was operated upon successfully in an operating room so small it was diffi-cult to stand around the operating room table.
Fireworks (The First Japanese Raid on the Island) (1942)By William F. DraperPainting, Oil on Board

THE GROG 17
Preventive medicine was practiced extensively aboard these vessels. Typi-cal was the experience on the Spica where there were lectures and motion pictures on first aid, stressing preven-tion and treatment of burns, wounds, fractures, hemorrhages, shock, sun-stroke, heatstroke, heat exhaustion and venereal disease; frequent instruction of stretcher bearers and Corpsmen in the proper technique of handling the injured—particularly those with the head injuries and fractures—and in ar-tificial respiration, constant inspection of cooks and mess attendants; inspec-tion of all food stores placed aboard ship; and careful observation of all per-sonnel in regard to their inoculations for typhoid, tetanus, yellow fever, and their booster shots. As evidenced by the work of the medical department at Attu, medical science, aided by its life-saving drugs, plasma, etc. and rapid transportation from distant battlefields to base hos-pitals had reduced mortality but will make World War II noteworthy as “A war of cripples.” An enlightening picture of the treat-ment of the Japanese wounded was given by the medical officer of the Spica. The doctrines of Shintoism, pro-mulgating the practice of hara-kiri, prevented the capture of Japanese pris-oners. Notwithstanding their sincere and stubborn resistance to capture, a Nipponese prisoner, who survived the explosion of his companion’s hand gre-nade, was borne by litter to the USS Spica. Our men watched the prisoner with resentment plainly evident on their faces. Fortunately a doctor is able to treat enemy patients unaffected by personal feelings. The patient was re-
moved to the sick bay. The lower right leg was dangling, swollen, gangrenous mess that required immediate amputa-tion. During the procedure, the patient obviously didn’t know whether he was going to be helped or killed, but noth-ing betrayed his emotions. The leg was amputated about two inches above the right knee. Later in the afternoon, the doctor returned to the patient’s cell. Here was a son of Nippon devoutly praying in gratitude for the kindly deed that had saved his life. The day of his transfer to a base hospital he seemed somewhat saddened and insisted on shaking hands with the doctor before leaving the ship. In the handling of large scale casual-ties from the beach, insofar as [attack
transports] APA’s are concerned, it was found that the establishment of a cen-tral casualty station through which all casualties passed and from where those cases needing singular care were trans-ferred to other specially set up dressing stations facilitated greatly the handling, care, and recording of the wounded. A suggestion was made that two respon-sible clerical technicians be assigned to the task of keeping records and ar-ranging and submitting the routine periodical dispatches required during the operations, thereby relieving the medical officer to carry on with treat-ment Hospital Corpsmen with greater adeptness and higher rates should be assigned to the dressing stations and those with lower ratings and less expe-
Ships and Shapes (1942)By William F. DraperPainting, Oil on Board

18 Issue 43, 2015
rience assigned to routine care of casu-alties in the hospital established in the troop compartment. The USS Hatfield (APA-6) found that none of the usual communicable dis-ease—other than catarrhal fever—were encountered, all of which responded very rapidly to systematic treatment. Because of the short period of time spent in ports of the mainland of Alaska, no venereal disease were encountered, al-though it was reported that many of the native women were infected by syphilis and tuberculosis. Despite the intense cold weather which caused the ship to be covered with a heavy coating of ice, there were no colds among the mem-bers of the crew until the Hatfield put into port in the United States. The crew were all given vitamin tablets, together with an adequate diet. It was noted that after a time without multiple vitamin tablets finger nails had a tendency to grow brittle; the hair grow dry and un-ruly; and pimples and boils, to appear on many—particularly on the younger men. Recommendation was made that a sunlamp should be allowed for all types of ships. A great deal of difficulty was experienced in preserving medi-cal supplies in gun bags in the exposed portions of the guns, as rain and snow quickly soaked through the gun bags and destroyed the contents. This was remedied by the simple process of plac-ing the material first in a 30 inch rubber target balloon and placing the balloons in the gun bags. After weeks of contin-ual use, the contents were found to be dry and ready for instant use.
KISKA In the battle for Kiska, Task Unit 16.2.2 was the Navy’s invasion force.
It consisted of the invasion fleet and a small group of men who were to from the nucleus of a planned naval station at Kiska. The largest portion of the men were members of the Amphibious units which operated the various types of small landing craft—LCT’s, LCM’s, LCV’s. The USS New Mexico [BB-40] also took part in the night engagement which became known variously as the “Battle of the Gremlins” and “Battle of the Pips.” It was not known definitely who were the opponents on this occa-sion, but it was thought quite possible that they were Japanese submarines engaged in evacuating the enemy from Kiska. Successful landings were made at Kernal Cove on August 15, 1943 at 1330 and the "Operation Cottage" (Kiska) could be said to be successful before it started—inasmuch as there was no Jap-anese opposition. The medical section was established and set to function im-mediately at 1600 the beach party was secured and told to return to its parent ship. As at Attu, it was found on Kiska that immersion foot and catarrhal fever were the primary medical problems. It was recommended that all ships pres-ent at any amphibious operation feed any and all personnel on the beach ir-respective of the branch of service to which they belong. Aboard the USS Doyen (APA-1) sea-men of the boat crews and men of the beach party were especially trained in first aid. Officers were given specific first-aid instructions and issued mor-phine syrettes and taught their use. Numerous drills were held at practice of general quarters, during which stew-
ard’s mates assigned to stretcher bearing were taught to handle and transport pa-tients. It was found that they made poor students and poorer stretcher bearers. Repeated surgical drills were held in the operating room until many combi-nations of Corpsmen were capable of setting up the operating room and as-sisting in surgical procedures. Constant repetition of drills dealing with intra-venous procedures were held. Corps-men practiced venipuncture upon one another until they were proficient and, therefore, competent, after learning the mechanical phase of the equipment, and how to administer plasma, draw and infuse blood and prepare intrave-nous medications. The techniques of the administration of various anesthetic agents were taught the Corpsmen—special emphasis being placed upon the use of sodium pento-thal. All first-aid boxes were checked on D minus 7 days and again on D minus 1 day, with any deficiencies being cor-rected at once. Sixty-five army litters equipped with units containing a blan-ket, four bunk straps and six large safety pins were in readiness. The J. Franklin Bell handled 32 casual-ties at Kiska even though there were no Japanese on the Island. Accidental and “trigger happy” wounds occurred and there were a few booby trap accidents. A big factor in the accidental wounds was the careless handling of grenades, the release pins of which had in many cases been loosened before landing in order to have them in a greater state of readiness. Inasmuch as the weather conditions were quite good for the Aleutians, exposure was a minor factor. There was one notable unfortunate occurrence which happened to the USS

THE GROG 19
Abner Read (DD-526). The stern of this destroyer apparently came in con-tact with a floating mine while on anti-submarine patrol off Kiska the night of August 17-18, 1943. On hearing the ex-plosion, the medical officer proceeded to his battle station in the wardroom. Casualties were brought to this place until it was filled, following which they were placed in the captain’s cabin and the division commander’s cabin. Most of the casualties were covered with fuel oil and most of those who had been exposed to the smoke escaping from ruptured smoke screen genera-tors were having difficulty in breath-ing and were coughing up moderate
amounts of whitish sputum. As each casualty arrived, the nature of his injury was quickly determined and those who were suffering from smoke inhalation only were carried below to the CPO quarters or “officers’ country.” Here, the wet clothing was removed and the pa-tients were placed in bunks and covered with blankets. The more serious cases, and those with lacerated wounds, were retained in the wardroom. All the lac-erated wounds were cleansed with soap and water, sprinkled with sulfonamide, and covered with dressings. Only two cases were in shock—one an
extensive burn case and the other a sus-pected abdominal injury. The burn case was given morphine (grains ¼) and two units of plasma intravenously. Both re-sponded satisfactorily. One deceased patient was brought in about 30 min-utes after the explosion and, although apparently dead, was given artificial respiration for an hour. At the end of this time it was seen that treatment was of no avail and the body was removed to the torpedo deck. By 0800, August 18, all casualties were free from shock and in bunks, and those who were able to take food received coffee and toast.
Fighter and Freighter -Kodiak, Alaska (1942)By William F. DraperPainting, Oil on Board

20 Issue 43, 2015
At this time each casualty was re-exam-ined and classified according to injury. Sixteen patients with lacerated wounds and burns were brought one by one to the sick bay, where definitive treat-ment was given. All lacerated wounds were thoroughly cleansed with saline solution, then sprinkled with sulfan-amide powder and covered with sterile dressings. All burns were cleansed with soap and water and dressed with heavy dressings of boric acid ointment gauze.While this treatment was being given in the sick bay, the chief pharmacist’s mate supervised the cleansing and re-distribution of the smoke exposure cases. These cases had previously been separated by the medical officer who had indicated the men well enough to take showers. While the showers were being taken and the cases with burns and wounds were being treated in the sick bay, bunks in the officers’ country and crews’ quarters were being pre-pared so that each patient when treated could return to a clean bunk. By 0700, August 19, 1943, each patient had been examined for the third time and notes made for the health records. The total number of casualties was 48, with one dead—of these, 34 were transferred to a naval dispensary at Adak, Alaska.
CONCLUSION It was observed that men over 35 years of age and men with arthritis, myalgic, or neuralgic pain history, in-cluding men with history of injury to major joints and the back, should not be sent into the Alaskan-Aleutian area. Moreover, additional vitamins should be provided in this area and overcrowd-ing in quarters and barracks should be foreseen and remedied.
A study of Japanese medical facilities was conducted and the medical officer concluded that their medical facili-ties, camp sanitation, general messing accommodations, and living quarters were inadequate by occidental stan-dards. The Japanese water supply was con-stantly open to contamination and the water systems for the main camp area were inadequate. The Japanese clothing was considered to be inferior to that furnished to the Americans, with the exception of the felt mitt which hangs from the shoul-der by a string and has a wide opening at the wrist and shooting fingers on the palm surface. The American mitt is leather, has a cumbersome finger ar-rangement and an elastic wrist.
Japanese dispensaries were given the best available protection from bombs, shells, and staffing. In one instance the entire unit was underground, except for galleys and a few attendants living ra-vines consisting of deeply reveted [sic] huts with nearby caves for shelters. A detailed survey of the Alaskan sec-tor of the 13th Naval District subsequent to the campaign of the Aleutians was conducted and a number of significant findings were made. It was determined that, in general, the morale of the per-sonnel in the Aleutian area was good, with a small percentage of men devel-oping situational neuroses of various degrees. It was suggested that a mere liberal policy of evacuation of border-line cases before complete breakdown be adopted. As a rule, the only indi-
Dutch Harbor, Alaska (1942)By William F. DraperPainting, Oil on Board

THE GROG 21
viduals in the construction battalions who were unable to withstand the stress of duty were the men past 40, who, in a sudden flash of patriotism, volunteered and then founds that they could not keep up with the younger men in the rigorous climate and terrain doing the hardest type of work. It was also a fact that many of these were married men with children, and were dissatisfied in the possession of the knowledge that many individuals in the continental United States were at that time receiv-ing inflated wages under the stress of a war economy. It was found, as is true throughout the service—whether it be in Panama, aboard ship, or the Alaskan sector—that medical officers are happy when they are busy and are fretful when they are not. Because of the organizational knots that were in the process of being untied by the medical officer in charge, there were some stations in the Alaskan sec-tor that were overstaffed with medical officers. This surplus had been main-tained in view of the operations which were projected at Kiska but which failed to be productive of casualties. The morale of the Navy nurses was reputed to be high, although a more suitable type of uniform should have been authorized. It was reported that the advent of the Navy nurses made a marked change in hospitals. There was one patient with a fractured pelvis who protested having to take a daily bath, giving as the reason therefore the fact that he had been in the hospital for nine weeks and had improved satisfactorily. There were several other hardy individ-uals who objected to the compulsory use of sheets as such articles were not supposed to be required on the rugged
frontier. The experienced chief nurse at the hospital involved, literally and figura-tively cleaned up the situation with gusto in a few days. The government-issue clothing for officers and enlisted help was found to fall short of adequate protective needs. Shoes were not rugged enough to with-stand the terrain. The practice of obtain-
ing and using Army waterproof soles was common. All naval personnel were found to prefer Army woolen shirts and woolen trousers for working dress in cold weather. The possible development of protective head gear or transparent eye covering as a medium of protection against foreign bodies of the eye and sandstorms was suggested. •
Transport Quarter Aboard Ship (1943)By William F. DraperPainting, Oil on Board

Capt. Mary Keener,
A Pioneering Physiologist
Capt. Keener at promotion ceremony receiving congratulations from Vice Adm. Robert Brown, Surgeon General of the Navy, March 1968BUMED Archives, 09-9054-2
22 Issue 43, 2015

THE GROG 23
"Do not compete with other people. Compete with yourself. Try to do better each day than you did yesterday. Remember, anyone can be mediocre. We were meant to excel."~Capt. Mary Keener, Medical Service Corps, USN
***
In 1965, Aviation Physiologist Mary Keener was promoted to Captain, becoming the first woman in the
Navy's Medical Service Corps to achieve this rank. At the time of her promotion, Keener purportedly had trained more aviation personnel in night vision, ejec-tor seat procedures, and low-pressure chambers than any other aviation phys-iologist in naval history Keener grew up in Attalla, Ala. with a dream of becoming a physician. She at-tended the University of Alabama ma-joring in zoology graduating in Octo-ber 1942. World War II would alter the career paths of many students, Keener included. Like other recent graduates, Keener wanted to do her part in the war effort. As a graduation present Keener’s mother bought her a ticket to New Or-leans so that she could take the Navy entrance exam. With the introduction of the WAVES (Women Accepted for Volunteer Emer-gency Service) program in 1942, wom-en were once again allowed to serve in non-nursing roles in the Navy, both as enlisted and officers. Keener was one of 15 women from Alabama selected for service as a WAVES officer and sent to Smith College in Northampton, Mass. for indoctrination and training in com-munications. In January 1943, Mary Keener was as-signed to work the “Secret Code” room of the Chief of Naval Operations, Adm.
Ernest King. She would later recall, “We were essentially cryptographers, breaking various codes, some of which Eleanor Roosevelt used to communi-cate to President Roosevelt when she travelled. When we decoded a mes-sage that started out ‘For the eyes of the President only,’ we were not allowed to read the message, but had to call a se-nior officer to stand over us as we typed out the code.” Over the summer of 1944, a family friend stationed at the Bureau of Per-sonnel offered Keener a chance to go to Pensacola where the Hospital Corps was opening a new field for WAVES officers—aviation physiology. Keener jumped at the opportunity and report-ed to the School of Aviation Medicine at the Naval Air Station Pensacola, Fla. There she would spend the remainder of the war serving as an “oxygen offi-cer.” Throughout World War II, Pensacola was where new recruits learned how to fly. Ostensibly, the job of aviation phys-iologists stationed there was to run pro-spective aviators (i.e., aviation cadets) through a gauntlet of tests to ensure that they could withstand the condi-tions of flying and aerial combat. Avia-tion cadets were required to take “alti-tude runs” in low pressure chambers to test their ability to withstand pressure changes to the body. Many WAVES of-ficers like Keener would be placed in
Capt. Mary Keener,
A Pioneering Physiologist

24 Issue 43, 2015
charge of the low pressure chambers that would simulate high altitudes. As an “oxygen officer,” Keener’s responsi-bilities included giving lectures on the pressure changes to the body, the dan-gers of high altitude, accompanying them on “oxygen flights” aboard PBYs, and demonstrating the effects of hy-poxia. (Note. The term "oxygen officer" was later changed to “aviation equip-ment and survival officer.”) After the war, Keener briefly served at the Naval Medical Research Institute (NMRI) in Bethesda, Md., where she assisted in the development of “ideal cockpit configuration.” She briefly left the Navy and then returned as a com-munications officer working at Naval Air Station Memphis, Tenn. The Women’s Armed Services Inte-gration Act of 1948 opened doors and new career paths for women in the military allowing them to enlist and be commissioned in the regular Navy. A year earlier, in August 4, 1947, Public
Law 80-337 had established the Medi-cal Service Corps creating new op-portunities within the Navy Medical Department. The Navy’s newest staff corps consisted of four specialty sec-tions: Supply and Administration, Op-tometry, Pharmacy and Allied Scienc-es (including aviation physiology). On September 20, 1948, Keener applied for and was one of 21 women selected for a regular commission in the Medical Service Corps. With the advent of jet aircraft in 1949, Keener would help develop programs for higher altitude training. Along with the first jets came the introduc-tion of ejection seats and the need for training. Per Flight Safety Council of the Chief of Naval Operations, all avia-tors were required to be indoctrinated in ejection seat training. The Navy Medical Department assumed the lead
for ejection training and beginning in 1951 established portable ejection seat towers at naval air stations across the United States. On March 12, 1951, BUMED installed the first mobile ejec-tion seat trainer at North Island, Calif. Others were soon installed at Marine Air Station Moffett Field, El Toro and Naval Air Station (NAS) Alameda. While stationed as NAS Norfolk in the 1950s, Keener would help train the aircrew of the Navy’s newest seaplane, the Martin P6M-1 Seamaster. The Seamaster was equipped with multiple ejection seats, but it also was an aircraft plagued by series of mechanical prob-lems. During the prototype’s inaugu-ral flight it disintegrated killing all four crew members. On November 9, 1956, the Navy tested the plane again and due to a mechanical failure it crashed, but not before the entire crew ejected
Martin P6M-1 SeamasterCourtesy of the Navy History and Heritage Command
Capt. Mary Keener

THE GROG 25
to safety. Later the crew sent a letter to Keener’s commanding officer thank-ing her training and crediting her with instilling them with the knowledge to save their lives. The Martin P6M Fly-ing boat program would be cancelled in 1959. Over the next two decades, Keener would have a front row seat to the his-torical developments in aviation and aerospace. Because of her experience
in physiological training, Keener was selected to serve as one of the Navy’s experts in the development of the pres-sure suit. “Navy pilots refused to accept full pressure suits and after many years of trying to sell them, they were finally dropped from our training programs,” Keener later related. "Some of our flight surgeons and some younger aviation physiologists went to NASA and were involved in the space program.”
Keener later served at NAS Barbers Point, Hawaii and then reassigned to BUMED. Since there was not yet an aviation physiology billet at the Bureau of Medicine and Surgery (BUMED) at the time, Keener was technically as-signed to NMRI. As she later remem-bered, “When I was first assigned to BUMED, I had no desk, no telephone and no parking place. I was assigned to the Aviation Medicine Operations Divi-sion and was the first woman officer to be assigned there.” At BUMED, Keener was tasked with recruiting new physiology candidates, supervising the making of training films, reviewing aircraft handbooks, writing policy, inspecting the 19 differ-ent training activities, approving train-ing aids and overseeing maintenance of training devices. Keener helped insti-tute an annual inspection program of training devices like ejection seats and low pressure chambers to ensure safety. In 1966, her aviation medicine billet went from being “ADDU” to full-time and moved to BUMED. A year later, in April 1967, the U.S. Navy Uniform Regulations granted "designated naval aviation physiologists" the permission to wear aviation wings. Keener would be among the first to adorn this crest. In 1967, Keener was elected Vice President of the Aerospace Medical As-sociation, the first woman to hold this office. Later in 1969, she was elected as the first fellow of the Aerospace Medi-cal Association. Keener retired from service in 1970. She died in November 2004. •
Martin-Ejection Seat Trainer in Port Magu, Calif., 1964BUMED Archives, 12-1002-001

26 Issue 43, 2015
"Most Legacies are not Legacies":An excerpt of an oral history with Rear Adm. William R. Rowley
Over the course of his 29 year career (1971-2000), Rear Adm. (ret.) William Rowley established a reputation as one of Navy Medicine’s most innovative and well-respected leaders. His vast resume includes tours as Dep-uty Commander, National Naval Medical Center, Bethesda, MD; Commanding Officer, Naval Hospital, Camp Pendleton, CA; Deputy Assistant Chief for Health Care Operations, BUMED, Washington, D.C.; Assistant Chief for Plans, Analysis and Evaluation, BUMED, Washington, D.C.; and Commanding Officer, Naval Medical Cen-ter, Portsmouth, Va. Since retirement in 2000, Dr. Rowley has been affiliated with the Institute for Alternative Futures, Alexandria, Va, most recently as a Senior Fellow. In June 2014, the BUMED History Office had the op-portunity to sit down with Dr. Rowley to look back on his career, his life after retirement and to capture some of his philosophies. The following is an excerpt of this session. It has been lightly edited for this publication.
***
Q: What legacies are you most proud of in your career? A: Most legacies are not legacies; they’re things you did, but they are not permanent. For example, the old Fort Belvoir hospital is gone, and now they’ve got their own “Gucci” hospital. By its very nature it is one of the best hospitals the military has ever built. But the culture waxes and wanes. The [Naval Hospital] Pendleton didn’t stay the way I made it; it kept changing over time. Of course most of the patients I operated on long ago are now dead. But for the people I taught and the people that were in my commands, whatever I did to help them as a role model:, if as a result they cared a little more about patients, if they took more risks, and if they saw things differently; then every time something like that happened, it changeds a little bit of the future. If it made a difference for them, that means the patients they took care of got better care.
One of the things I see in high- level politicians and sports figures is a desire for a legacy. There are people who look for that kind of fame and permanence. Admiral James Zimble [Surgeon Gen-eral of the Navy, 1987-1991] had a li-brary named after him, and Admiral Don Sturtz has a general surgery teach-ing award in his name at San Diego. He was another fabulous role model. I don’t know if you ever heard of him, but he was a true renaissance man. He was going to be a preacher, but ended up becoming a Navy pilot and then a general surgeon. He is about 6’4” tall (somehow he fit in a small fighter jet), the most mild-mannered, politically correct, precise person you can imag-ine; he really cared, listened, and always talked to you (“So how is your family doing?”). He could make decisions and he turned out to be a wonderful father figure for the surgery department. He did a great job, with quality and com-passion, and became one of the few
“clinical admirals” recognized for his medical accomplishments. I watched many officers retire from the military and try to keep their title – colonel or whatever. When I retired I dropped my rank and most of the time my title of doctor. Just “Bill” is fine with me. I still do leadership teaching for Navy Medicine. I teach medical stu-dents at USUHS (Unifomed Services University of the Health Sciences) and work on some projects for the Military Health System. These are opportunities to contribute my wisdom and biases, and stimulate others to provide great patient care, explore the future and practice good leadership. I go to Medi-cal Corps balls and occasional flag offi-cer get-togethers. And I get my medical care at Walter Reed, so in some ways I stay immersed in military medicine. When I teach leadership to senior of-ficers I run into people who remember me from when they were as new naval officers at my commands, and their

THE GROG 27
comments and praise help me remem-ber the good old days. The best memo-ries are of providing good patient care, being friendly with all the staff and making a difference in helping resi-dents become great doctors. I think my only important legacy is every once in a while I look back and say, “Yes, I did some good things.” My plaques are ei-ther gone or in a box somewhere, and my formal uniform doesn’t fit. But I keep the pictures of me with four presidents in the basement so I can say, “Gee, think of all the experiences I had.” I guess everybody is different; I mean there are so many people (especially in the political world) worried about how history is going to see them, and if they’re always going to be respected. And that’s why the titles and the belief something will be named after them is so critically important and influences everything they do. So there are a couple of things I do now. I stay very active. Yesterday I rode on a 38 mile bike ride with a bunch of seniors, and I’ll do that again tomor-row. I still do some research. I keep abreast of what’s going on in medicine so I can keep my presentations cur-rent. I’m lucky that I’ve had the op-portunity to figure out what’s going on in military medicine through my work on two DoD independent review panels, and I am still teaching medical officer leadership courses. I know one of these days soon I’ll just have to say,
“You know, thank you very much, but I shouldn’t be doing this anymore.” For now, I stay part of the military medical family once in a while, and of course I go to Walter Reed for my medical care. That’s it. To review real quickly what I say in my presentations to medical officers.First there’s leadership. As you move further up in rank, according to Colin Powell’s book,1 you really cannot just focus on what’s going on inside your organization; you’ve got to know what’s going on in the bigger world. You can’t only think about tomorrow, you’ve got to think about what’s going to happen thirty years from now. Senior leaders need to have the big picture because the military is directly affected by what will happen in the future, and must prepare now for making the needed changes in time. American healthcare is changing very fast and it will profoundly affect military medicine. Here’s the secret of the future—and this is really important: Nobody knows exactly what is going to happen, be-cause the future consists of many po-tential possibilities and no one knows which ones society will pursue. You can invent the future, but you can’t in-vent the future without a vision. Most people say, “I don’t know what’s go-ing to happen, so I’ll just go with the flow. I’ll keep doing what I’m doing and when the world changes I’ll go with it.” At Camp Pendleton we chose to create the future.
[A Tricorder] is a device used by Dr. McCoy on Star Trek.2 It is the thing you wave over the patient to make a diag-nosis and maybe provide some therapy. It is an analogy for where medicine is heading. Today, there is a ten million dollar prize for the team that creates the first functioning Tricorder-type device that can diagnose fifteen major diseas-es.3 It is anticipated that the maker of the first functional prototype will re-ceive the award by the end of 2016. To give an example of what will prob-ably be available soon: you’re at home. You have chest pain, so you consult your cell phone that suggests doing an EKG by the cell phone. The EKG con-firms a heart attack so the hospital ER is wirelessly notified. Your cell phone informs you, “Your EKG is of concern so an ambulance will arrive in about five minutes to take you to the emer-
Rear Adm. William Rowley
1. Powell, Colin L., GEN, USA, Ret.: Chairman, Joint Chiefs of Staff, 1989-1993; Secretary of State, 2001-5; author, It Worked for Me; N.Y., HarperCollins, 2012.2. Star Trek, a science fiction series developed by CBS and Paramount Pictures; the original series was broadcast in 1966-69, and was followed by other productions.3. The Tricorder X Prize, a competition sponsored by Qualcomm, in 2016 will award a $7 million first prize, $2 million 2d price, and $1 million 3d prize, to the developers of a portable devise weighing five pounds or less that is able to diagnose fifteen medical conditions.

28 Issue 43, 2015
gency room for further evaluation. In the meantime please take two aspirins, lie down and relax.” Of course, the next step (which is not going to be too many years from now) is your cell phone is going to do some kind of a finger prick or non-invasive test to see if you have markers sugges-tive of progressive arteriosclerosis with significant risk of a heart attack. The cell phone informs you of the sched-uled doctor’s appointment to address the problem and treat you prophylac-tically to prevent a future heart attack. So I talk about that, and where war-fighting is going with information tech-nology, and then the interesting trend as to where health care is going to be delivered. It’s going to be at home and in cyberspace, and most hospitals are going to be without inpatient beds. Now let’s talk about the Quadruple Aim.4 The first thing is population health. Presently, your kids have about a fifty percent chance of becoming obese and one-third will develop dia-betes during their lifetime, based on current lifestyles. We’re already seeing life expectancy decline in America; in other words we’re not a very healthy society. Here are some recent statistics about what’s going on with our kids: 23 per-cent have pre-diabetes or diabetes, fifty percent have at least three out of seven major cardiac risk factors, and seventeen percent are obese. There was an important survey of 174,000 adults who answered four questions: (1) Are
you not smoking? (2) Are you main-taining a normal body weight? (3) Are you eating five fruits and vegetables a day? (4) Are you getting thirty minutes of some kind of physical activity five days a week?” Only three percent said “yes” to all four. So why is this important? Seventy percent of premature deaths are the re-sult of lifestyle. There is a 35-year dif-ference in life expectancy depending upon what county you live in and that’s basically related to lifestyle. Comparing the group that said “yes” to those four questions to the group that said “no,” the difference is a 36 percent reduction in cancer, 81 percent reduction in heart disease, and a 93 percent reduction in diabetes. In other words, if we get peo-ple to quit smoking and start moving and eating fruits and vegetables, and a few other things, we could make a huge difference in health. Here’s another number. We’re spending almost three trillion dollars annually, mostly for treating chronic diseases that we cre-ate due to the way we live in America: No exercise, eating sugar, salt and fat, stress, not enough sleep, not brushing your teeth, not having relationships—it goes on. Another aim I focus on is lower cost. We don’t realize that the cost of military medicine is almost twice the operating budget of the Marine Corps, and it is growing faster than the overall defense budget. Most are unclear about the cen-tral aim: improved readiness. Medical personnel must be ready so we need
GME training programs, busy MTFs for skills maintenance, operational medical platforms and research and development. It would be ideal if Con-gress would change the TRICARE ben-efit to incentivize beneficiaries to re-turn to MTFs for their care. Obviously our warfighters must be healthy and re-silient to withstand the stresses of com-bat. Admiral [Michael] Mullen, when he was Chairman of the Joint Chiefs, said it was essential that we also have family readiness to support returning injured warriors into society again.
Q: Ten, fifteen years from now, how will we look back at the current years of Military Medicine? A: Some people say it’s the beginning of fundamental change in health, health care, and society. It’s like we don’t real-ize it until hundreds of years later, but we finally left the dark ages and entered a new era.
Q: “The awakening”?A: Yes, “the awakening” would be a pretty good term. The interesting thing about the future is we can show you a world of possibilities, but the question is: do you want to go there? There will be resistance to embracing many of the possibilities on the part of institutions (government, military, medicine and society), and change is a slow process when everybody wants to go there. But I think what happens is we reach tip-ping points. Many things are reaching a tipping point now. We’ve got more
4. Quadruple Aim: In 2009 the Military Healthcare System adopted the Triple Aim that had been formulated the Institute of Healthcare Improvement, a not-for profit organization located in Cambridge, Mass., of three components necessary to improve American medicine: improving the patient experience, including quality and satisfaction; improving the health of the population; and reducing the per-capita cost of healthcare. The Quadruple Aim included an additional component – readiness.

THE GROG 29
transparency so the truth is more in the open if people want to see. We can’t survive without our cell phones, and “Why in the world can’t I do that with a cell phone?” is clearly changing every-thing we do and empowering people. One of the things about the future is disruptive innovation. For example we used to live in the world of mainframe computers. IBM made million dollar computers that were run by powerful “geeks” who mysteriously took control of our lives in banking, airline tickets, etc. Well the world has changed since IBM did something unbelievably radi-cal when they decided that they were going to build the PC, this little desktop computer they could sell to consumers. So what did they do? They built a new plant in Boca Raton, Fla., and brought in a new set of people who were sepa-rated from the rest of the company. They leveraged new technology—the micro-chip and the floppy disk drive—the technology enablers. They convert-ed to a business model of selling PCs through stores to ordinary humans for $2,500 starting in 1981.5 In 1977, Computer Sciences Corporation’s net-work was selected by the Bell System to support its units in the U.S. The IBM PC [personal computer] came out in ’81. The PC was seen as a child’s toy so it was not a threat to geeks and their mainframes, and nobody could imag-ine what was coming next. But the PC fundamentally changed the planet and everything we do. So, on the one hand we see the mili-tary culture and health care industry
that are incredibly resistant to change, and on the other hand, we see how dis-ruptive innovations are so powerful that they can change everything in so-ciety. It’s possible that if you took a time machine thirty years into the future, you would not recognize or understand most of what you saw. However it doesn’t get there just like that; there’s a lot of starts and stops along the way. There might soon be a cancer that we essentially cure every time, but another that we are still trying to find a cure for thirty years from now. We’ll find some things that the public embraces immediately, but other things we still can’t wrap our minds around. Even though we can be in denial and strongly resist change there is ultimate-ly no choice but to adapt and eventually embrace change. Anyway, this gives you an idea of what I discuss in a military leadership class. I then divide the students into dialogue groups and challenge them to solve tough issues facing Navy Medi-cine. What would you do? I want you to create a better future for Navy Medi-cine ten years from now. The only way you’re going to get there in ten years is if you have a compelling vision now of a future worth creating stimulated by the future possibilities we talked about. Here’s the last thing worth mention-ing that changed over my career. When I was a resident in surgery, we would get to the hospital very early every morning, go down to the cafeteria, and sit down with a few others for a good 45 cent (1970’s price) breakfast (even cus-
tom-made omelets). It was a wonderful and important experience. At the table we could have a couple Medical Ser-vice Corps officers, a nurse, maybe an internist and a vascular surgeon; we’d be talking and we’d build relationships. I’d understand what it was like from their perspective, how they were do-ing things, what their challenges were, what their opinions were. We learned everything that was going on, and we started supporting each other in get-ting the job done because we built trust between us. Then citizens started complaining to Congress that we were getting inappro-priately subsidized meals and a major surcharge was added, so the breakfast price went up to a couple dollars and everyone stopped eating in the cafete-ria. Unfortunately, this fundamentally changed the culture for the worst be-cause the different perspectives, ex-planations, trusting relationships and opportunities to cooperate went away. Now with constant emails, cellphone calls, long commutes, and job complex-ity there is not time for people to have a dialogue, reflect on complex issues or to build understanding and trusting re-lationships—we just chase our tails try-ing to get through the day. •
5. CSC was founded in 1959. In 1978 it was awarded the system support contract for California MEDICAID, at that point the largest contract California had awarded.

The Curious Story of Naval Hospital Dublin and the Rheumatic Fever Scourge
“[Rheumatic Fever] is not numbered among the—shall I say?—spectacular maladies. You don’t hear much about it. Someone has characterized it as a condition ‘which licks the joints but bites the heart.’ It is one of the most dangerous, disabling afflictions known to mankind. It claims thousands of new victims each year yet its cause remains unknown and we are still groping in the dark as to its treatment and cure.”
~Rep. Carl Vinson (D-Georgia), May 1946
30 Issue 43, 2015

THE GROG 31
Rheumatic fever is a debilitat-ing disease caused by A strep-tococcus (Streptococcus pyo-
genes), the same bacteria responsible for strep throat and scarlet fever. Usu-ally manifesting two to three weeks af-ter a throat infection, the condition can lead to severe joint pain, involuntary muscle movements, fever, and irrepa-rable damage to heart valves and even heart failure (rheumatic heart disease). Owing to the advance of antibiotics, rheumatic fever is largely a forgotten threat in developed nations today, but it was not that long ago that the ailment resulted in one of the leading causes of valvular heart disease in the United States and the very reason for establish-ing a naval hospital and research labo-ratory in Dublin, Ga. Between 1900 and 1930, rheumatic fever related valvular disease (cor-dis valvulrum morbis) accounted for 156,120 sick days and invalided 2,871 from service in the Navy. During World War II, with the Navy and Ma-rine Corps populations peaking at the largest levels in history, the impact of infectious diseases like rheumatic fever posed a very serious threat to readi-ness. In 1943, more than 3,000 Navy Sailors developed rheumatic fever. On average rheumatic fever cost each pa-tient about 60 days on the sick list and, according to one Navy report, “break the morale of the patient.” Beginning in 1943, the Bureau of Medicine and Surgery (BUMED) sought to establish “special purpose” hospitals as well as a research labora-tory dedicated to acute rheumatic fe-ver. At the time, the Naval Hospital in Corona, Calif. had been used for this purpose, but with increased demands
for the hospital’s other services, the fa-cility no longer proved adequate. Early proposals called for establishment of rheumatic fever hospitals in Florida and southern California, each offering warm locales deemed ideal for treating patients. West Palm Beach, Clearwa-ter, and Daytona, Fl. and Beverly Hills and Palm Springs, Calif. were each proposed as prospective homes for the new facilities.
In 1943, under the guidance of Lt. Cmdr Alvin Coburn, MC-V(S), US-NR—a pioneer in the field of rheumatic carditis—the Navy Medical Depart-ment outlined a new treatment plan for all rheumatic fever cases. All acute pa-tients would be treated promptly with salicylate, a non-steroidal anti-inflam-matory drug, and then placed in a re-stricted ward dedicated for rheumatic fever patients. After blood sedimenta-
Dr. James Paullin, Atlanta-based cardiologist and consultant to NavalHospital Dublin and NAMRU-4. National Library of Medicine

32 Issue 43, 2015
tion rates were deemed normal, pa-tients would be transferred to a special convalescent hospital where they would continue to be treated with salicylate and mandatory bed rest. As patients showed fewer clinical symptoms and inflammation subsided, their activity levels would be increased until eventu-ally they were returned back to duty. Coburn asserted that the Navy’s execu-tion of this plan would be “regarded by American Medicine as a great advance in the solution of the clinical problem of an important disease.” The next step would be to in the fight against the disease was to establish the special convalescent facility. As a result of the increased demand
for hospitalization and treatment of rheumatic fever, and support by and in-fluence of powerful Georgia Represen-tative, and the Chairman of the Naval Affairs Committee, Carl Vinson, the Navy constructed its newest hospital on the outskirts of Dublin, Ga in 1944. Located on 232 acres, “Naval Hospital Dublin” could accommodate up to 900 patients at its peak and offered many of the “modern” services available at naval hospitals at the time. One of Dublin’s characteristics (and chief complaints by personnel stationed there) was its isolation. The closest “big” city, Macon, was located 55 miles away. The local train from Macon, which would breeze through Dublin
once daily, and intermittent commer-cial bus service did little to make the hospital feel any less isolated from the rest of the world. Most patients arrived via a four-engine R4D or R5D trans-port planes which landed in an airfield 2.8 miles from the hospital and then be bussed in. Unlike other naval hospitals in op-eration, Dublin was conjoined with a clinical research laboratory with the strict purpose of studying rheumatic fever. Although subject to administra-tive orders of the hospital, the laborato-ry would develop into an independent unit, eventually garnering distinction as Naval Medical Research Unit No. 4 (NAMRU-4), at least ostensibly. On August 8, 1946, Rear Adm. William Agnew, then acting Chief of BUMED, issued a memorandum to Navy Medi-cal Corps Chiefs stating: “The research group and research facilities at Dublin may…be known as NAMRU-4, but the designation will be used only as a term of convenience on Medical Depart-ment correspondence without im-plying independence of the hospi-tal command.” At its peak, NAMRU-4 com-prised a staff of research direc-tor, assistant research director, a personnel/property officer, enlisted technicians, two secre-taries, and a number of civilian-scientists working as virologists, bacteriologists, immunologists, histopathologists, microbiolo-gists, physiologist, and chemico-physicologists. At the end of 1945, the Dublin re-search unit embarked on its first ma-jor project: a basic study of rheumatic state in post-streptococcal infections
Representative Carl Vinson of Georgia (on right) would ulti-mately decide the future home of the Navy's rheumatic fever hospital. Library of Congress

THE GROG 33
at the Naval Training Center in Great Lakes, Ill. Working in accordance with the Rockefeller Institute and BUMED, NAMRU-4 sent researchers to Great Lakes to screen recruits showing af-ter effects of streptococcus infections (Project X-702A). The project set out to study the bacteriology of the disease from infection to convalescence, and to collect information on clinical and sub-clinical rheumatic fever or carditis
in 400 cases of scarlet fever. Despite both being in operation (in some form) since the end of 1944, and the hospital was only placed in com-mission on January 22, 1945 and the laboratory in May 1946. The ceremony featured remarks by Vice Adm. Ben Moreell (Chief, Civil Engineer Corp), Vice Adm. Ross McIntire (Surgeon General), Congressman Carl Vinson, music by both the Marine Corps and
Army Bands and a special address by Atlanta-based heart specialist and phy-sician to President Roosevelt, Dr. James E. Paullin. Paullin, then a civilian con-sultant to Surgeon General McIntire, would take special interest in the de-velopment of the hospital and research unit. Both the Navy’s increased access to penicillin and massive demobilization following World War II helped reduce the need for a special rheumatic fever hospital and laboratory. In 1947, the Naval Hospital Dublin was transferred to the Veterans Administration where it was scheduled be converted into a neu-ropsychiatric hospital. Today the facil-ity is still in operation and known as the Carl Vinson Veterans Affairs Medical Center. When Naval Hospital Dublin closed down in 1947, NAMRU-4 relocated to the Naval Training Center, Great Lakes, Ill. where it set forth on an ambi-tious course of investigating additional problems affecting Navy recruits—i.e., influenza, pneumonia, respiratory in-fections, the common cold, and Menin-gococcal Infections. The Research Unit was disestablished in 1974. •
“[The] capacity of 500 beds is estimated to be inadequate for the purpose intended dur-ing the next nine to twelve months, but ultimately it will be too small for the anticipated number of patients suffering from acute rheumatic fever. The duration of stay of such patients is considerably longer than the average stay of all patients in United States Naval Hospitals.”
~Frank Hines, Chairman of Federal Board of Hospitalization, December 1944
Streptococcus pyogenes bacteria. Rheumatic Fever is caused by the
same bacteria responsible for strep throat and scarlet fever.

The Navy Laboratory School, 1878-1879: A Culture Grows in Brooklyn
The development of bacteriology and the birth of public health movements in the late nineteenth century would go far to reshape our understanding of disease and the means of disease prevention. This new age of medicine would also help remold the role of the
Navy physician. The Surgeon-Physician travelling the oceans in age of sail was now the “Scientist-Physician” charting the unexplored territories of sanitary science through chemical, bacteriologi-cal, and microscopic investigations. By the 1870s, physicians seeking commissions in the Navy, and those seeking promotion within service, had to show an aptitude in laboratory science before the Navy’s Medical Examining Board. On February 1, 1878, in order to better prepare candi-dates for this examination, Navy Surgeon General William Grier authorized the formation of the “Laboratory School of Instruction” (sometimes called the Department of Instruction) at Naval Hospital Brooklyn, N.Y. Naval Hospital Brooklyn was every bit a forebear of today’s multifunctional medical centers.
In addition to being one of the largest hospitals in the Navy at the time, it served as the home to the Medical Examin-
ing Board and the Naval Laboratory—an in-house pharmaceutical/medical supply depot that both
manufactured and supplied the Navy with all of its medicines and surgical equipment. Stu-
dents at the new school would have access to all of the hospital’s resources, including quarters and mess. And upon graduation, they would stand before the board for ex-amination. The hospital’s commanding officer, Medical Director Samuel F. Coues, USN—
a physician of “well-known ability, acquire-ments, and zeal”—was placed in charge of
34 Issue 43, 2015
Dr. William GrierSurgeon General of the Navy

developing the school’s curriculum and served as the principal instructor. Under his guidance students were required to go through an intensive regimen of lectures and laboratory work (see figure 1) covering fields of recruit medicine, optics and microscopy, chemistry and chemical anal-yses, Navy regulations and procedures, and “naval hygiene” (a catch-all term covering everything from occupational medicine/public health to food science and nutrition). Students were offered an opportunity to inspect naval vessels at the nearby shipyard for cleanliness, and ventilation and be encouraged to attend clinics at local civilian hospitals to improve their knowledge of anato-my and dissection. Classes were held Monday through Saturday and each session lasted three months. Sessions were offered in September 1878, November 1878, February 1879, June 1879, and September 1879. With Surgeon General Grier’s retirement at the end of 1878 and Medical Director Coues trans-fer to Boston for “special duty” at the end of 1879, the school lost its two founders and ultimately ceased operation. The effort was rekindled briefly in the 1890s as the “Navy Laboratory and Department of Instruction” (1893-1898). In May 1902, it was formally re-established at Naval Museum of Hygiene in Washington, D.C. as the Naval Medical School. •
THE GROG 35
Fig. 1. Laboratory School of Instruction Curriculum Partial Schedule of Second Class, Sep 2-Nov 2, 1878The Second class convened on 2 September 1878 and consisted of nine assistant surgeons. Schedule of course work included: “microscopial manipulation” (4-14 September), “History and construction of the microscope” (16 Sep and 3 Oct), microm-etry (17 and 23-34 Sep), chemistry (18-20 Sep), physical ex-aminations and recruiting (21 and 28 Sep), chemical analy-sis (25-26 and 30 Sep-1Oct), sphygmography (27 Sep), food science (2 Oct), recruit medicine/myopia and color blindness (5 Oct), analysis of air (7-9 Oct), section cutting (10 Oct), examination of sputum (11 Oct), temperature, thermometer, & humidity (12 Oct), ventilation of hospital (16 Oct), micro-scopic examination of water (16-17 Oct), antiseptic dressing (18 Oct), disinfection, bilges and timber (19 Oct), Optics (21-22 and 29-30 Oct), larynyopscopy (23 Oct), Physical Diagno-sis of Diseases of the Chest (24 Oct), Navy medical forms and regulations (25 Oct), disinfectants, cleanliness, ventilation of ships/punishment, prison, and prisoners (26 Oct), medical surveys and pensions (28 Oct), temperature (31 Oct), oto-scope (1 Nov), quarantine, and sanitary regulations (2 Nov).
Medical Director Samuel Coues

A product of theCommunications Directorate
Bureau of Medicine and Surgery