Tangents ONLY for Sentinel Lymph Node Positive Breast ...
Transcript of Tangents ONLY for Sentinel Lymph Node Positive Breast ...
Tangents ONLY for Sentinel Lymph Node Positive Breast Cancer
(Skip the RNI)
Henry Kuerer, MD,PhD,FACSDepartment of Surgical Oncology
University of Texas MD Anderson Cancer Center
Disclosures• Employment/Compensation
– MD Anderson Cancer Center; Editor, McGraw‐Hill
• Research funding support– Genomic Health, Inc.
• Scientific advisory board– Lightpoint Medical, Inc.
Outline• Focus breast conserving surgery, SLN
positive disease in one or two nodes, whole-breast radiotherapy
• Clinical trials in relation to MA.20– IBCSG 23-01– ACOSOG Z11– AMAROS
• 42% SLNB vs 29% ALND (p<0.03)
• Micrometastases– 16% SLNB vs
3% ALND (p<0.0005)
• SLN era of detection more like historical node-negative disease
SLN Era: significantly higher axillary metastatic node detection
Giuliano et al Ann Surg, 1995
Decreasing nodal burden: stage migration• MD Anderson Cancer Center• Number positive nodes, axillary dissection• 1978 – 1997
– 1 + 45%– 2 + 32%– 3 + 23%
• 2000 – 2007– 1 + 55%– 2 + 30%– 3 + 15%
McBride et al, Int J Radiation Oncol Biol Phys, 2014
Risk of additional positive nodes after positive SLN whole-breast radiation trials
• Randomized trials that included ALND after (+) SLN: Additional (+) nodes 13 to 27% (before administration of systemic therapy)
• Axillary nodal recurrence in SLN surgery alone arms <1%
• IBCSG 23-01, ACOSOG Z11
Tangential Fields: Design Determines Axillary Nodal Coverage
High TangentsStandard Tangents
Incidentally includes level I part II Deliberately includes level I-II higher and deeper borders
What is Regional Node Irradiation?• Many definitions, may
be unspecified• Can include:
– Supraclavicular– Internal mammary– Level III– Axillary fields (level I/II)
MA.20
Why consider RNI for Early Breast Cancer?
• Node negative and 1 to 3 positive lymph nodes
• L III, SC, IM may serve as occult reservoir for disease, never clinically apparent, but source for distant disease– Unpublished; NCIC MA.20 and EORTC 22922
MA.20:2000-2007
A Phase III Study of Regional Radiation Therapy
in Early Breast Cancer Whelan et al ASCO 2011
®Stratification Axillary nodes removed (<10, >10) Positive axillary nodes (0, 1-3, >3) Chemotherapy (anthracycline, other, none) Endocrine therapy (yes, no)
MA.20 StudyNode positive or high risk
node negativeafter BCS
Whelan et al ASCO 2011
WBI
WBI + RNI
n=916
n=916
MA.20 PopulationEligibility Criteria: Treated with BCS and sentinel node biopsy
(39%) or axillary node dissectionNOTE: all node +ve patients treated with a level 1 and 2 axillary dissection; 85% of patients in study 1-3 node positive Treated with adjuvant chemotherapy and/or
endocrine therapy
Whelan et al ASCO 2011
Isolated Locoregional DFS
* 67% of regional recurrences were in the axilla
Any First Local or Regional Recurrence WBI WBI + RNI
N of Patients 916 916Events 48 29
Local only 25 25Regional only* 21 4Local + Regional 2 0
5-Yr LR DFS 94.5% 96.8%2.3%
Whelan et al ASCO 2011
HR=0.64 (95% CI 0.47 to 0.85)P=0.002 (Stratified)
−WBI −WBI + RNI
Distant DFSPe
rcenta
ge
0
20
40
60
80
100
Years
0 1 2 3 4 5 6 7 8 9 10
92.4%87%
Whelan et al ASCO 2011
HR=0.76 (95% CI 0.56 to 1.03)P=0.07 (Stratified)
−WBI −WBI + RNI
Overall Survival
Perce
ntage
0
20
40
60
80
100
Years0 1 2 3 4 5 6 7 8 9 10
92.3%90.7%
Whelan et al ASCO 2011
Why not consider RNI for Early Breast Cancer?
• Long term survival > 80%• Potential long term toxicity becomes real
concern– Heart, lung, esophagus– Lymphedema– Arm mobility– Cosmesis, malignancy
EORTC phase III trial 22922/10925 SC-IMEarly reported toxicity up to 3 years
• Cardiac disease–1.4% IM-MS vs. 1.6% none; p=0.64
• Lung toxicity–4.3% IM-MS vs. 1.3% none; p<0.0001–(fibrosis, dyspnea, pneumonitis)
Matzinger et al., Acta Oncologica, 2010
WBIn=927
WBI + RNIn=893
PValueGrade 2 3 4/5 Any 2 3 4/5 Any
AcuteRadiationDermatitis 349 23 - 40% 397 45 - 50% <0.001
Pneumonitis 2 - - 0.2% 12 - - 1.3% 0.01
DelayedLymphedema 34 3 1 4% 61 4 - 7% 0.004
*NCI Common Toxicity Criteria v.2 1998
MA.20 Adverse Events*Grade ≥ 2
Whelan et al ASCO 2011
WBI WBI + RNI P Value
Baseline 187 / 910 (21%) 197 / 876 (22%) 0.33
At 3 years 177 / 679 (26%) 195 / 670 (29%) 0.22
At 5 years 111 / 381 (29%) 142 / 396 (36%) 0.047
* Number (%) of Patients with fair or poor global assessment of cosmetic outcome using the EORTC cosmetic rating system
MA.20 Adverse Cosmetic Outcome*
Whelan et al ASCO 2011
International Breast Cancer Study Group (IBCSG) Trial 23-01: N1mi, N=931
Galimberti, et al. Lancet Oncol 2013
• Phase III randomized trial of ALND vs SLND only• cT1-2 N0 patients with micromets (≤ 2mm) in ≥ 1 SLN• In ALND group, 59 (13%) had additional positive nodes• 9% of patients in each arm underwent mastectomy
Median f/u 5 years ALNDN=464
SLND onlyN=467
Local recurrence 10 (2%) 8 (2%)
Regional recurrence 1 (<1%) 5 (1%)
Distant recurrence 34 (7%) 25 (5%)
Radiation Fields IBCSG 2301• Unknown, ‘extent of incidental axillary
radiation is not ascertainable’• 22% no WBXRT (none or ELIOT PBI)• Authors suggest that low rate of nodal
recurrence could be immunosurveilance
IBCSG 23-01 Survival Endpoint
Galimberti, et al. Lancet Oncol 2013
ALNDN=464
SLND onlyN=467
HR(95% CI) P value
5 yr DFS 84% 88% 0.78 (0.55 – 1.11) 0.16
5 yr OS 98% 98% 0.89 (0.52-1.54) 0.73
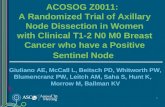
ACOSOG Z0011: All patients node positive detected by SLN biopsy
Primary Objective: To assess whether OS after SLND alone was not inferior to that for patients who
underwent completion ALND for a positive SLN
Patient and tumor characteristics
Giuliano, et al. Ann Surg, 2010
ALNDN=420
SLNDN=436
Median age 56 (24-92) 54 (25-90)
Clinical T1 68% 71%
Ductal histology 83% 84%
ER+ 83% 83%
GradeIIIIII
22%49%29%
26%47%28%
LVI 41% 35%
Adjuvant systemic therapy
ALNDN=420
SLNDN=436
Chemotherapy 57.9% 58.0%
Hormonal therapy 46.4% 46.6%
Either/Both 96.0% 97.0%
Giuliano, et al. Ann Surg, 2010
Size of SLN metastasis
0
10
20
30
40
50
60
70
Micrometastasis(<2.0mm)
Macrometastasis
Perc
ent o
f Pat
ient
s
ALND
SLN
37.5%44.8%
62.5%
55.2%
P=0.05
Giuliano A, et al. JAMA, 2011
Additional positive LNs
106 (27.3%) of patients treated with ALND had
additional positive nodes removed beyond the SLN
Giuliano, et al. Ann Surg, 2010
Z0011:Local-regional recurrence
ALNDN=420
SLNDN=436
Local 15 (3.6%) 8 (1.8%)
Regional 2 (0.5%) 4 (0.9%)
Total 17 (4.1%) 12 (2.8%)
Node-positive Disease
Giuliano, et al. Ann Surg, 2010
Z0011:Overall survival
Giuliano, et al. JAMA, 2011 Median follow-up: 6.3 yr
0
10
20
30
40
50
60
70
80
90
100
0 1 2 3 4 5 6 7 8
Time (Years)
% A
live
ALNDNo ALND
P-value = 0.25
93%92%
Z0011:Disease-free survival
Giuliano, et al. JAMA, 2011 Median follow-up: 6.3 yr
0
10
20
30
40
50
60
70
80
90
100
0 1 2 3 4 5 6 7 8
Time (Years)
% R
ecur
renc
e-Fr
ee and
Aliv
e
ALNDNo ALND
P-value = 0.14
84%82%
Z0011:Conclusions
• For patients with cT1-2 N0 breast cancer and 1-2+ SLN undergoing BCS with whole breast RT:– No improvement in regional control with ALND– No impact on survival
• Does not apply to:– Clinically node positive– Patients receiving neoadjuvant chemotherapy– Patients undergoing mastectomy
Z0011:Conclusions• For patients with cT1-2 N0 breast cancer and 1-2+ SLN
undergoing BCS with whole breast RT:– No improvement in regional control with ALND– No impact on survival
• Does not apply to:– Clinically node positive– Patients receiving neoadjuvant chemotherapy– Patients undergoing mastectomy– Patients receiving partial breast irradiation
Radiation Fields and RNI ACOSOG Z11(Alliance) Trial
• Case report forms: 605 patients• 89% WB; 11% NO RADIOTHERAPY• 15% supraclavicular field
• 228 detailed RT records• 81.1% tangents only, 18.9% ≥ 3 fields, more common
with greater nodal involvement (p<0.001)• High-tangents used 50% of patients each arm
Jagsi et al, J Clin Onc, 2014
Radiation Fields and RNI ACOSOG Z11(Alliance) Trial
• No significant difference in RNI in SLN only versus ALND groups
• The primary finding – that routine ALND is not necessary after +SLNB in one or two nodes–stands
Jagsi et al, J Clin Onc, 2014
Can axillary radiotherapy substitute for axillary dissection?
Is it actually necessary after a positive SLN?
AMAROS:EORTC 10981-22023• After mapping axilla: radiation or surgery?• Hypothesis: AxRT provides comparable local control and survival as ALND with
fewer side effects• cT1b-2 N0• BCT or mastectomy
• Pos SLN randomized to ALND or AxRT
cT1-2N0 R SNB
ALND
AxRT
AxSN+
AxSN-Rutgers E, ASCO 2013
N=1,425
• Extent:level I + II + III + medial SC
• Dose & schedule:25 x 2 Gy or equivalent
• Quality control:dummy run
Hurkmans et al, Radiother Oncol 2003; Rutgers, ASCO 2013
AMAROS Radiation Fields
AMAROS Nodal Recurrence• In ALND group, 244 (32.8%) patients had additional
positive nodes• Median follow-up = 6.1 years
ALNDN=744
AxRTN=681
Axillary recurrence 0.43% 1.19%
Axillary recurrence in SLN negative patients = 0.72%
Rutgers E, ASCO 2013
AMAROS• No difference in DFS or OS
HR:1.17; 95CI: 0.85-1.62HR:1.18; 95CI: 0.93-1.15
Rutgers E, ASCO 2013
AMAROS Lymphedema• Decreased lymphedema with AxRT
Rutgers E, ASCO 2013
0
5
10
15
20
25
30
35
40
1 3 5
ALND
AxRT
28.0%
40.0%
29.8%
21.7%
16.7%13.6%
Years after randomization
P < 0.0001 P < 0.0001P < 0.0001
Perc
enta
ge
*lymphedema observed or treated
Z0011/AMAROS
• Lymphedema rates• ALND 28%• AxRT 14%• SLND 5%
• Based on Z0011, 82% of patients enrolled on AMAROS could have avoided both ALND and AxRT
AMAROS/Z11 Conclusions
• Ax radiotherapy and ALND provide effective local regional control in SLN + patients
• Additional benefit of Level III and SC radiotherapy fields not clear
• Long term lymphedema rate significant concern
Individualization: Patient Selection• Nomograms to predict risk of >4 positive
nodes in non-dissected axilla?– “If greater than 30% strongly consider L III/SC”
• Will performing axillary dissection change field selection? 1/14; 2/20; 3+– What nodal fields will you treat?
Katz et al J Clin Oncol, 2008Haffty, Hunt, Harris, Buchholz, J Clin Onc, 2011
De‐escalating therapy: NSABP B‐51/RTOG1304
Primary aim: Evaluate whether the addition of PMRT and regional nodal irradiation will improve invasive DFS rates
Clinical T1‐T3, N1 Breast Cancer
Neoadjuvant Chemotherapy
Pathologically negative lymph nodes (either by SLND or ALND)
No PMRT or regional nodal XRT
Regional nodal XRT
Stratification Factors:• Surgery type (lumpectomy, mastectomy• Hormone receptor status• HER2 status• Adjuvant chemotherapy (yes/no)• pCR in breast (yes/no)
Randomization
N=1,636
Summary• Local regional control and survival excellent among
patients with SLN + disease receiving WBXRT and systemic therapy
• Use of RNI is associated with significant additional toxicity
• Results for RNI in earlier stage breast cancer (1-3+ and node negative)– Potentially profound and practice changing
Conclusion: Tailoring Local Therapy
• Breast Cancer is a heterogeneous disease• Many groups do extremely well focus on omission, cost, convenience focus on toxicity avoidance
• Selected groups need improvements focus on new therapeutic approaches
AcknowledgementsSurgical Oncology
Kelly K. Hunt, MDGildy V. Babiera, MDIsabelle Bedrosian, MDShon Black, MDAbigail S. Caudle, MDSarah M. DeSnyder, MDBarry W. Feig, MDRosa F. Hwang, MDAnthony Lucci, MDFunda Meric-Bernstam, MDMediget Teshome, MD
Breast Medical OncologyBanu Arun, MDMariana Chazez, MD Gabriel N. Hortobagyi, MD Jennifer K. Litton, MDVicente Valero, MD
PathologyAysegul A. Sahin, MDMichael Gilcrease, MDSavitri Krishnamurthy, MD
Radiation OncologyThomas A. Buchholz, MDWelela Tereffe, MDEric Strom, MDSimona Shaitelman, MDBen Smith, MDMichael Stauder, MDGeorge Perkins, MDWendy Woodward, MD, PhD