Systemic lupus erythymatosus
-
Upload
gayathiri-govindaraju -
Category
Education
-
view
60 -
download
2
Transcript of Systemic lupus erythymatosus
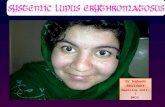
*A rash across the bridge of the
nose and the upper cheek bone.
*Systemic- Can affect any
organ or tissue in body.
*Lupus- Wolf
*Erythymatosus- Colour of the
rash.
*SLE- systemic autoimmune disease or
auto immune connective tissue disease.
*Can affect any part of the body.
*Characterised by acute or chronic
inflammation in various tissues of the
body.
*Type III hypersensitivity reactions in
which Ab immune complexes
precipitate and cause further immune
response.
*Skin manifestation- Butterfly eruption
on face and photosensitivity.
*SLE most commonly harms heart,
kidney, joints, lungs, blood vessels,
liver and nervous system
EPIDEMIOLOGY
*Women are more affected, especially women in
child bearing age are more affected. Because
XX chromosomes in females, X carries
immunological related genes which can mutate.
*Common in Canada and Europe.
*Children about 3 years are affected, majority in the
age of 15-44 years.
ETIOLOGY
*Environmental factors- cold, fatigue, stress,
sunlight. Sunlight contain UV rays- UVA and
UVB(Shorter wavelength causes more harm).
*Genetic factors – not caused by a single gene, but
multiple gene appear to influence chance of
develop lupus. HLA region on chromosome 6
where mutation occur randomly.
*Virus- Epstein bar virus.
*Chemicals- silica, mercury.
*Drug reactions- occur in people treated for
long term infections.
Eg. Procainamide
Hydrolazine
phenytoin.
PATHOPHYSIOLOGY
It is mainly related to
The deposition of immune complexes in
various organs which trigger complement and
other mediator of inflammation.
Auto-antibodies in SLE are directed against
wide variety of self antigens, most commonly
against Nuclear self antigen(ANA).
Deactivate the bacteria, virus and allergen.
APC’s activate the immune system
NORMAL MECHANISM
Bacteria, virus, allergens enter the body
Aggrevatedby env.
stimulantants
UV light or drug rxn
Destruct other cells in the body and
exposure of DNA histones
& other proteins mainly
a part of cell nucleus
Body’s sensitised B-cells produce Ab
against nuclear reacted proteins
Abnormalities in apoptosis
Ab-protein complex
Which will stick to surface of blood
vessel
Deficiency in clearance
Deposition of dead cells and other cellular waste
SLE
TYPES
Discoid lupus- A form of lupus that can be
isolated only to skin without affecting
internal organs is called discoid lupus
When internal organs are involved it is
called SLE.
COMPLICATIONS
*Anaemia- Haemolytic and iron deficiency.
*Antiphospholipid syndrome:
• disorder of blood coagulation related to
the presence of auto antibodies called
lupus anticoagulation and anti cardiolipin.
•APS causes blood clot in deep veins.
*Vasculitis- inflammation of blood vessel.
*Thrombocytopenia- Ab attack platelets and
cause their destruction- causes bleeding
from nose, gums and intestine.
*Blood cancer
*Heart complications- myocarditis, heart
attack, stroke, endocarditis, plaque build
up in arteries.
*Lung complications: chest pain, coughing,
pain in breathing, pulmonary hypertension.
*Kidney : early fluid build up which causes
overall weight gain, kidney failure.
*CNS complications: psychologic and
neurological disorder, anxiety, depression,
amnesia and migrane.
*Infection: fungal and parasitic infection, people
with weak immune system have increased risk
of UTI and yeast infection.
*GI complications: nausea, diarrhoea, weight
loss, heart burn(GERD).
*Joint, muscle and bone marrow complications:
osteoporosis, muscle ache, swelling of joints.
DIAGNOSIS
*SLE affects various organs, so they have wide
variety of symptoms and different combination of
organ involved.
There are 11 criteria mainly determined as
diagnosis…..
Butterfly rash.
Discoid skin rash/patchy redness with
hypo/hyper pigmentation that causes scarring.
*Photo sensitivity.
*Mucous membrane ulcers- nose mouth or
throat.
*Arthritis- 2 or more joints.
*Kidney abnormalities- abnormal amounts of
urine protein, casts are detectable.
*Anti- nuclear antibodies(ANA antibody)
*Antiphospholipid syndrome.
*Lungs – inflammation of lining around
the lungs.
*Brain irritation- by seizures,
convulsions- reffered as lupus
cerebritis.
*Low blood count abnormalities-
reduced WBC/RBC/Platelets.
TREATMENT
Management aims:
* To reduce inflammation.
*To reduce pain.
*To prevent organ damage.
*To improve the quality of life.
PHARMACOLOGICAL
TREATMENTCATEGORY EXAMPLES
SALICYLATES IBUPROFEN, NAPROXEN,
ASPIRIN
ANTIMALARIALS HYDROXYCHLOROQUINE,
CHLOROQUINE, QUINACRINE
TOPICAL CORTICOSTEROIDS BETAMETHASONE,
DIPROPIONATE,
CYCLOPHOSPHAMIDE,
METHYL PREDNISOLONE
IMMUNOSUPPRESANTS CYCLOPHOSPHAMIDE,
AZATHIOPRINE,
MYCOPHENOLATE MOFETIL,
DHEA
INTRAVENOUS
IMMUNOGLOBULINS
BELIMUMAB
SALICYLATES
*Indication: To treat arthritis.
*Dose : 400-800 mg 3-4 times/day
initial dose- 2.4-3.6 g/day in divided doses
maintainence dose – 3.6-5.6 g/day.
*ADR: Intolerance,
salicylism (HA, dizziness, vertigo, difficulty in
hearing).
ANTIMALARIALS
*Indication: To treat flares,
To protect blood clot in people with anti-
phospholipid syndrome.
*Dose : initial dose-400 mg OD
Maintainence dose: 200-400 mg
*ADR: GI problems, HA, hair loss, yellow
colour skin(Quinacrine), retinal damage.
TOPICAL CORTICOSTEROIDS
*INDICATION: Reduce inflammatory process,
symptoms involving anaemia and kidney. IV
methyl prednisolone can reduce flares in 3
days.
*Mechanism : acts as alkylating agents, it acts
by adding an alkyl group to base of DNA which
reduces immune system response to various
diseaes(AID’s)
*Dose : mild potency for face
mid potency for other areas
Apply thin films to affected areas once or twice
daily.
Maximum dose 45 g / week
Prednisolone, methyl prednisolone given as IV
in a dose of < 1 mg/kg/day.
*ADR: Osteoporosis, weight loss, excess hair
growth, insomnia, irritability, infertility.
IMMUNOSUPPRESSANTS
*Indication: to treat kidney disease.
*Mechanism: acts by blocking an early stage in
activation of cytotoxic T-lymphocytes after the
recepient is exposed to Ag.
*Dose: initial dose- 2-3 g/day
Maintainence dose- 0.5-3 g/day
Azathioprim: 1 mg/kg/day for 6-8 weeks
increases by 0.5 mg/kg every 4 weeks.
*Methotrexate- 7.5-15 mg / week with folic
acid.
*Mycofenolate mofetil: It inhibits an enzyma
neede for the growth of B & T cells.
*ADR: nausea, vommiting, hair loss,
infertility, diarrhoea(mycofenolate mofetil)
INTRAVENOUS IMMUNGLOBULINS
*Indication: In pain & fever , to reduce Ab
production, promote clearance of immune
complexes.
*It is a biological monoclonal antibody which
inhibits a protein called B- lymphocyte stimulator
protein and reduces the production of B - cells
and thereby reduces the immune response.
LIFE STYLE MODIFICATIONS
• Use topical sunscreens.
• Avoid triggers
- Exposure to sunlight.
- Avoid UV rays
- Use hypo-allergic cosmetics and hair
products.
- Don’t smoke or avoid exposure to passive
smoking.
Prevent infections:
-Reduce exposure to crowds.
-Reduce exposure to people with contagious
illness.
-Proper hygiene.