Systemic lupus erythematosus
-
Upload
buddhika-illeperuma -
Category
Health & Medicine
-
view
294 -
download
0
Transcript of Systemic lupus erythematosus

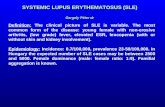
SYSTEMIC LUPUS ERYTHEMATOSUSAn overview of the diagnosis & management
Dr. Buddhika Illeperuma

Bit of history▪ The word ‘lupus’ (Latin for
‘wolf’) is attributed to the thirteenth century physician Rogerius who used it to describe erosive facial lesions that were reminiscent of a wolf's bite.

Bit of history▪ Robert Willan (1757-1808), a British dermatologist, described
destructive lesions of the face and nose under the heading of lupus. Cutaneous tuberculosis or lupus vulgaris was included under this.
▪ In 1872, Kaposi first described the systemic signs of the disorder. These included fever, weight loss, lymphadenopathy, anemia, and arthritis.
▪ The name discoidal lupus, as pertaining to the exclusively cutaneous form of the disease, is credited to Kaposi.
▪ Kaposi and Cazenave clearly distinguished lupus erythematosus from lupus vulgaris or cutaneous tuberculosis, although there was a lot of confusion around that time due to the coexistence of both diseases in patients.

1997 Update of the 1982 American College of Rheumatology Revised Criteria for
Classification of Systemic Lupus Erythematosus1. Malar (butterfly) rash2. Discoid lesions3. Photosensitivity4. Oral or nasopharyngeal ulcers5. Non-deforming arthritis in two or more joints6. Serositis: pleuropericarditis, aseptic peritonitis7. Renal: persistent proteinuria › 0.5 g/d or ›3+
or cellular casts Definite SLE = 4 or more positive criteria

1997 Update of the 1982 American College of Rheumatology Revised Criteria for
Classification of Systemic Lupus Erythematosus
8. Neurologic disorders: seizures, psychosis9. Heme: hemolytic anemia; leucopenia, lymphopenia, thrombocytepenia10.Immune: anti-DNA, or anti-Sm, or APS (ACA IgG, IgM), or lupus anticoagulant (standard) or false + VDRL11.Positive ANA
Definite SLE = 4 or more positive criteria

New SLICC* Revision of the ACRClassification Criteria - Clinical
1. Acute/subacute cutaneous lupus2. Chronic cutaneous lupus3. Oral/Nasal ulcers4. Nonscarring alopecia5. Inflammatory synovitis with physician-observed swelling
of two or more joints OR tender joints with morning stiffness
6. Serositis
*Systemic Lupus International Collaborating Clinics (SLICC)

New SLICC Revision of the ACRClassification Criteria - Clinical
7.Renal: Urine protein/creatinine (or 24 hr urine protein) representing at least 500 mg of protein/24 hours or red blood cell casts
8.Neurologic: seizures, psychosis, mononeuritis multiplex, myelitis, peripheral or cranial neuropathy, cerebritis (acute confusional state)
9. Hemolytic anemia10.Leukopenia (< 4000/mm3 at least once) OR
Lymphopenia (< 1000/mm3 at least once)11. Thrombocytopenia (<100,000/mm3) at least once

SLICC Revision of the ACRClassification Criteria – Immunologic
1. ANA (antinuclear antibody) 2. Anti-dsDNA3. Anti-Sm (anti-Smith) antibody4. APS abs: Lupus anticoagulant , false-positive
test for syphilis, anticardiolipin IgG, IgM, or IgA 5. Low complement: low C3, low C4, low CH506. Direct Coombs test in the absence of
hemolytic anemia

Lupus – SLICC New Classification Criteria: 4 needed
▪ At least 1 clinical plus at least 1 immunologic criteria (for a total of 4)
or▪ Lupus nephritis by biopsy as the
sole clinical criterion plus SLE autoantibodies: (+) ANA or (+) anti-dsDNA

Acute/subacute cutaneous lupus
1) Lupus Malar rash (do not count if malar discoid)

Acute/subacute cutaneous lupus
2) Bullous lupus

Acute/subacute cutaneous lupus
3) Toxic epidermal necrolysis variant of SLE

Acute/subacute cutaneous lupus
4) Maculopapular lupus rash

Acute/subacute cutaneous lupus
5) Photosensitive lupus rash

Acute/subacute cutaneous lupus6) Subacute cutaneous lupus Nonindurated psoriaform and/or annular polycyclic lesions that resolve without scarring

Chronic cutaneous lupus1. Classic discoid rash Localized (above the neck) Generalized (above and below the neck)

Chronic cutaneous lupus
2. Hypertrophic (verrucous) lupus

Chronic cutaneous lupus3. Lupus panniculitis (profundus)

Chronic cutaneous lupus4. Mucosal lupus

Chronic cutaneous lupus5. Lupus erythematosus tumidusErythematous, succulent, edematous, nonscarring plaques in sun-exposed areas

Chronic cutaneous lupus6. Chillblains lupusPainful inflammation of small blood vessels

Chronic cutaneous lupus7. Discoid lupus/lichen planus overlap

Oral/Nasal ulcers
▪ In the absence of other causes, such as vasculitis, Behcet’s disease, infection (herpesvirus), inflammatory bowel disease, reactive arthritis, and acidic foods

Nonscarring alopecia ▪ In the absence of other causes such as alopecia areata, drugs, iron
deficiency, and androgenic alopecia.

Arthritis▪ Arthritis of the proximal interphalangeal (PIP)
and metacarpophalangeal (MCP) joints of the hands, as well as the wrists
▪ Synovitis involving 2 or more joints, characterized by swelling or effusion OR tenderness in 2 or more joints and at least 30 minutes of morning stiffness
▪ Tenderness, edema, and effusions accompany a polyarthritis that is symmetric, nonerosive, and usually nondeforming
▪ Jaccoud arthropathy is the term used to describe the nonerosive hand deformities due to chronic arthritis and tendonitis that develop in 10% of patients with SLE.
Jaccoud arthropathy

Serositis▪ Typical pleurisy for more than 1 day OR pleural effusions OR pleural rub▪ Typical pericardial pain (pain with recumbency improved by sitting forward)
for more than 1 day OR pericardial effusion OR pericardial rub OR pericarditis by electrocardiographyIn the absence of other causes, such as infection, uremia, and Dressler’s pericarditis

Renal Manifestations ▪ Urine protein–to-creatinine ratio (or 24-hour urine protein)
representing 500 mg protein/24 hours▪ Red blood cell casts

Neurologic Manifestations1. Seizures2. Psychosis3. Mononeuritis multiplex - In the absence of other known causes such
as primary vasculitis4. Myelitis5. Peripheral or cranial neuropathy - In the absence of other known
causes such as primary vasculitis, infection, and diabetes mellitus6. Acute confusional state - In the absence of other causes, including
toxic/metabolic, uremia, drugs

Haematological Manifestations 1) Hemolytic anemia2) Leucopenia (4,000/mm3 at least once)In the absence of other known causes such as Felty’s syndrome, drugs, and portal hypertension
OR Lymphopenia (1,000/mm3 at least once)In the absence of other known causes such as corticosteroids, drugs, and infection
3) Thrombocytopenia (100,000/mm3 ) At least once in the absence of other known causes such as drugs, portal hypertension, and thrombotic thrombocytopenic purpura

Immunologic criteria1. ANA level above laboratory reference range2. Anti-dsDNA antibody level above laboratory reference range (or 2-fold the reference range if tested by ELISA)3. Anti-Sm: presence of antibody to Sm nuclear antigen4. Antiphospholipid antibody positivity as determined by any of the following: Positive test result for lupus anticoagulant False-positive test result for rapid plasma reagin Medium- or high-titer anticardiolipin antibody level (IgA, IgG, or IgM) Positive test result for anti–B2-glycoprotein I (IgA, IgG, or IgM)5. Low complement - Low C3, Low C4, Low CH506. Direct Coombs’ test in the absence of hemolytic anemia

The Use of ANA for Screening Immunofluorescence ANA assay (IF) remains the gold standard for detection of ANA
Many laboratories perform immunoassays (such as the multiplexed immunobead assay), for the detection of ANA as it is less labor-intensive
Data suggest that screening with an immunoassay would result in misclassification and potential delay or missed diagnoses
Immunofluorescence (IF) should remain the preferred assay for ANA testing - Endorsed by the American College of Rheumatology (ACR)

SLE – Management ▪ EULAR recommendations for the management of systemic lupus
erythematosus. Report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics - July 2007
▪ Joint European League Against Rheumatism and European Renal Association–European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis - July 31, 2012
▪ American College of Rheumatology Guidelines for Screening, Case Definition, Treatment and Management of Lupus Nephritis - 2012 June

Treatment of non-major organ involvement
▪ Glucocorticoids, Antimalarials, Non-steroid anti-inflammatory drugs (NSAIDs) and, in severe, refractory cases immunosuppressive agents are used in the treatment of SLE patients without major-organ involvement.
▪ Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used for the symptomatic management of arthralgia, mild arthritis, myalgia, serositis and fever in patients with SLE.
▪ They do not have any immunosuppressive properties and despite their widespread use in the lupus population there is little trial evidence for safety or efficacy.
▪ They should be used for short periods of time and with caution especially in patients with renal involvement, hypertension and established heart disease.

Treatment of non-major organ involvement
Hydroxychloroquine
▪ Hydroxychloroquine has emerged as the drug of choice and some experts advocate its use in all patients provided that there are no contraindications.
▪ Owing to its anti-inflammatory and immunomodulatory properties, it has a significant impact on the long-term outcome by modifying the course of illness through reduction of low-grade flares and hence slows progression to severe disease requiring more intense treatment.
▪ Hydroxychloroquine is most useful in the management of mucocutaneous, musculoskeletal and constitutional symptoms such as fatigue and fever.
▪ Recently, hydroxychloroquine has been shown to have cardioprotective properties in several studies, by reducing total cholesterol, low-density lipoprotein (LDL) cholesterol and triglycerides (TG) and increasing high-density lipoprotein (HDL) cholesterol levels

Treatment of non-major organ involvement
Hydroxychloroquine
▪ Hydroxychloroquine has a good safety profile and toxicity is infrequent, mild and largely reversible.
▪ In pregnancy, it is safe with noticeable reduction in SLE activity and no adverse effects on the child
▪ Retinal toxicity and macular damage are rare with hydroxychloroquine.
▪ Owing to the remote risk of hydroxychloroquine-related maculopathy, guidance from the Royal College of Ophthalmology, UK, states that doses should not exceed 6.5 mg/kg/day and patients should have yearly visual acuity monitoring.

Treatment of non-major organ involvement
Corticosteroids
▪ Several studies have shown that a short course of moderate-dose corticosteroids can not only treat active disease but can also help prevent flares in clinically stable but serologically active patients.
▪ In mild disease, prednisolone is given in doses starting at 0.1–0.3 mg/kg/day followed by a gradual tapering dose regimen according to clinical response.
▪ The dose rises to 0.4–0.6 mg/kg/day in moderate disease and as high as 0.7–1.5 mg/kg/day in very severe disease.
▪ At such high doses, pulse therapy with intravenous (IV) methylprednisolone (MP; 500–1000 mg on one to three occasions) is deemed by many physicians to be safer with fewer associated side effects.
▪ Prednisolone is safe in pregnancy as they are inactivated by 11 β-hydroxysteroid dehydrogenase, so that less than 10% crosses the placenta

Treatment of non-major organ involvement - Immunosuppressive therapies
▪ In patients with moderate-to-severe disease who require 10mg prednisolone/day or more to manage their disease, other immunosuppressive agents should be added to reduce the steroid requirements.
Azathioprine
▪ Azathioprine is commonly used for the induction of remission and as a steroid-sparing agent in mild-to-moderate disease.
▪ In severe disease, it is used as maintenance therapy and data from lupus nephritis trials show significant improvement in disease activity following induction therapy with cyclophosphamide or mycophenolate mofetil (MMF)
▪ It is safe in pregnancy, as the foetal liver cannot metabolize azathioprine to the active metabolites

Lupus nephritis: treatment▪ The treatment of lupus nephritis often consists of a period of intensive
immunosuppressive therapy (induction therapy) followed by a longer period of less intensive maintenance therapy.
▪ Class I and Class II generally does not require immunosuppressive treatment
▪ In general, patients with Class III, IV and V require aggressive therapy with glucocorticoids and immunosuppressive agents.
▪ Class VI (sclerosis of ≥90% of glomeruli) generally requires preparation for renal replacement therapy rather than immunosuppression.
▪ Options for induction therapy are either IV Cyclophosphamide or MMF in combination with pulse Methylprednisolone (Methylprednisolone alone in pregnancy)
▪ Options for maintenance therapy are azathioprine (AZA), MMF or Prednisone up to 10 mg daily

Lupus nephritis: Adjunctive Treatments
▪ The Task Force Panel recommended that all SLE patients with nephritis be treated with a background of hydroxychloroquine (HCQ) (level C), unless there is a contra-indication.
▪ All lupus nephritis patients with proteinuria ≥ 0.5 g per 24 hours should have blockade of the renin-angiotensin system
▪ Treatment with either ACEi or ARBs reduces proteinuria approximately 30%, and significantly delays doubling of serum creatinine and progression to end stage renal disease
▪ The use of combination ACEi/ARB therapies is controversial.▪ Careful attention should be paid to control of hypertension, with a
target of ≤ 130/80.▪ Statin therapy be introduced in patients with LDL cholesterol >100
mg/dL

Lupus nephritis: Treatment goals▪ Complete renal response, defined as urine protein:creatinine ratio
(UPCR) <50 mg/mmol (roughly equivalent to proteinuria <0.5 g/24 h) and normal or near normal(within 10% of normal) GFR.
▪ Partial renal response, defined as ≥50% reduction in proteinuria to subnephrotic levels and normal or near-normal GFR, should be achieved preferably by 6 months and no later than 12 months following treatment initiation.

Treatment of severe neuropsychiatric lupus
▪ Seizure, peripheral neuropathy, optic neuritis, transverse myelitis, brainstem disease, coma and internuclear ophthalmoplegia
▪ Induction therapy with intravenous methylprednisolone (MP) was followed by either intravenous monthly cyclophosphamide (CY) versus intravenous MP every 4 months for 1 year and then intravenous CY or intravenous MP every 3 months for another year.

THANK YOU