Systemic lupus
-
Upload
siva-nanda-reddy -
Category
Health & Medicine
-
view
207 -
download
0
Transcript of Systemic lupus

Systemic Lupus Erythematosus (SLE)
By:Mr. M. Sivananda Reddy


Incidence• About 90% of all cases occur in women• Most cases occur in women of
childbearing years• At the age of 30 years the ratio of
women to men is 10:1• African, Asian, Hispanic, and Native
Americans three times more likely to develop than whites

Etiology• Auto immune• Etiology is unknown• Most probable causes:– Genetic influence– Hormones– Environmental factors- UV B rays,
infections with CMV, HCV, smoking– Certain medications- Trimethoprim,
Sulphamethaxozole

Pathophysiology• Autoimmune reactions directed against
constituents of cell nucleus, DNA• Antibody response related to B and
T cell hyperactivity which is stimulated by the Estrogen
• The antigen antibody complexes that are developed will be in the circulation and blocks the microvasculature and the spaces

Clinical Manifestations• Ranges from a relatively mild disorder
to rapidly progressing, affecting many body systems
• Most commonly affects the skin/muscles, lining of lungs, heart, nervous tissue, and kidneys


• Dermatologic:– Cutaneous vascular lesions– Butterfly rash– Oral/nasopharyngeal ulcers– Alopecia

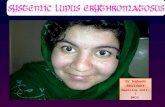
Butterfly Rash / Malar Rash

• Musculoskeletal–Polyarthralgia with morning
stiffness–Arthritis• Swan neck fingers• Ulnar deviation• Subluxation with hyperlaxity of joints

Swan Neck Deformity

Ulnar deviation:

• Cardiopulmonary– Tachypnea– Pleuritis– Dysrhythmias– Accelerated CAD– Pericarditis

• Renal– Lupus nephritis• Ranging from mild proteinuria to
glomerulonephritis

• Nervous system– Generalized/focal seizures– Peripheral neuropathy– Cognitive dysfunction• Disorientation• Memory deficits• Psychiatric symptoms

• Hematologic– Formation of antibodies against blood cells– Anemia– Leukopenia– Thrombocytopenia– Coagulopathy– Anti-phospholipid antibody syndrome

• Infection– Increased susceptibility to infections– Fever should be considered serious– Infections such as pneumonia are a
common cause of death

Diagnostic Studies

• Antinuclear antibodies– ANA and other antibodies indicate
autoimmune disease– Anti-DNA and anti-Smith antibody tests
most specific for SLE– ESR & CRP are indicative of
inflammatory activity.

• CBC for hematologic problems• Ultrasound Abdomen for lupus
nephritis• X-rays of affected joints• Chest x-ray for pulmonary problems• ECG for cardiac problems

Treatment• Drug therapy–NSAIDs- Acetaminophen–Antimalarial drugs-
Hydroxychloroquine–Corticosteroids- Prednisone– Immunosuppressive drugs

Nursing ManagementNursing Diagnoses
• Fatigue• Acute pain• Impaired skin integrity• Ineffective therapeutic regimen
management• Body image disturbance

Nursing Interventions–Observe for• Fever pattern• Joint inflammation• Limitation of motion• Location and degree of discomfort• Fatigability

–Monitor weight and I&O– Collect 24-hour urine sample– Assess neurological status– Explain nature of disease– Provide support

• Ambulatory and home care– Reiterate that adherence to treatment
does not necessarily halt progression–Minimize exposure to precipitating factors
– fatigue, sun, stress, infection, drugs– Teach energy conservation and relaxation
exercises– Teach regarding ROM to prevent
contractures

• Psychosocial issues– Counsel patient and family that SLE has
good prognosis– Physical effects can lead to isolation,
self-esteem, and body image disturbances
– Assist patient in developing goals