system and pain being made. 0.04). that associ- · angiogram) with normal esophageal motility...
Transcript of system and pain being made. 0.04). that associ- · angiogram) with normal esophageal motility...

Psych
ologicaltraits
influen
ceau
tonomic
nervoussystem
reco
veryfollowingesophagealintubationin
healthan
dfunctional
chestpain
A.D.FARM
ER,*
S.J.
COEN,*,†
M.KANO,*,‡
S.F.W
ORTHEN,§
H.E.ROSSIT
ER,§
H.NAVQI,*
S.M
.SCOTT,*
P.L.FURLONG§&
Q.AZIZ*
*Cen
treforDigestiveDisea
ses,
Bliza
rdInstitute
ofCell&
Molecu
larScien
ce,W
inga
teInstitute
ofNeu
roga
stroen
terology
,
Barts
andtheLondonSch
oolofM
edicine&
Den
tistry,Quee
nM
aryUniversity
ofLondon,London,UK
†Dep
artm
entofNeu
roim
aging,
Institute
ofPsych
iatry,King’sColleg
eLondon,London,UK
‡Beh
aviouralM
edicine,
TohokuUniversity
GraduateSch
oolofM
edicine,
Sen
dai,Japan
§AstonBrain
Cen
tre,
Sch
oolofLifean
dHea
lthScien
ces,
AstonUniversity,Birmingh
am,UK
Key
Message
s
•Esophag
ealintubationis
widelyutilize
dbutac
tivates
aco
mplexphysiologica
lresponse.
•Herein,weco
mpared
anumber
ofvalidated
sympathetic
and
parasympathetic
nervoussystem
param
eters
inhea
lthysu
bjectsan
dpatients
withfunctional
chestpain.
•Oesophag
ealintubationac
tivates
afigh
torflightresponse.
•In
future,at
least10min
allowed
fortheau
tonomic
nervoussystem
toreco
verypriorto
mea
suremen
tsbeing
mad
e.
Abstract
Back
groundEsophage
alintubationisawidelyutilize
d
tech
niqueforadiverse
arrayofphysiologica
lstudies,
activatingaco
mplexphysiologica
lresponse
med
iated,
inpart,bytheautonomic
nervoussystem
(ANS).
In
order
todetermine
the
optimal
time
period
after
intubation
when
physiologica
lobservations
should
bereco
rded
,it
isim
portantto
know
thedurationof,
andfactors
thatinfluen
ce,this
ANSresponse,in
both
hea
lthanddisea
se.MethodsFifty
hea
lthysu
bjects(27
males,
med
ianage
31.9
yea
rs,range
20–5
3yea
rs)and
20patien
tswithRomeIIIdefi
nefunctionalch
estpain
(nine
male,
med
ian
age
of
38.7
yea
rs,
range
28–5
9yea
rs)had
personality
traitsand
anxiety
mea
-
sured.Subjectshad
hea
rtrate
(HR),
blood
pressure
(BP),
sympathetic
(cardiac
sympathetic
index
,CSI),
and
parasympathetic
nervoussystem
(cardiac
vaga
l
tone,
CVT)parametersmea
sured
atbaselineand
in
response
toper
nasu
mintubationwithanesophage
al
catheter.CSI/CVT
reco
very
wasmea
sured
following
esophage
alintubation.Key
Results
Inall
subjects,
esophage
alintubationca
usedanelev
ationin
HR,BP,
CSI,
and
skin
conductance
response
(SCR;
all
p<
0.0001)butco
nco
mitantCVT
and
cardiacsensi-
tivityto
thebaroreflex
(CSB)withdrawal(allp<
0.04).
Multiple
linea
rregressionanalysisdem
onstratedthat
longe
rCVTreco
verytimes
wereindep
enden
tlyassoci-
atedwithhigher
neu
roticism
(p<
0.001).Patien
tshad
prolonge
dCSIandCVTreco
verytimes
inco
mparison
tohea
lthysu
bjects(112.5
svs46.5
s,p=
0.0001and
549svs223.5
s,p=
0.0001,respec
tively).Conclusions
&Inference
sEsophage
alintubationactivatesaflight/
flightANSresponse.Future
studiessh
ould
allow
forat
least
10min
ofreco
verytime.Considerationsh
ould
be
given
topsych
ologica
ltraitsanddisea
sestatusasthese
caninfluen
cereco
very.
Address
forCorresponden
ceProfessorQasim
Aziz,
PhD,FRCP,TheW
inga
teInstitute
of
Neu
roga
stroen
terology
,Barts
andtheLondonSch
oolof
Med
icinean
dDen
tistry,26Ash
fieldStree
t,W
hitec
hap
el,
LondonE12AJ,UK.
Tel:+44(0)2078822630;fax:+44(0)2078825640;
e-mail:a.farm
.uk
Rec
eived
:26June2013
Acc
eptedforpublica
tion:13Augu
st2013
©2013JohnW
iley
&SonsLtd
1
Neu
roga
stroen
terolMotil(2013)
doi:10.1111/nmo.12231

Keywords anxiety, autonomic nervous system, esoph-
ageal intubation, functional chest pain, neuroticism.
INTRODUCTION
Abnormalities in esophageal sensorimotor function arecommon, exerting a worldwide burden.1 These abnor-malities may occur in both patients with provenorganic disease and also those without obvious struc-tural or biochemical abnormality such as in thefunctional gastrointestinal disorders (FGID). Theunderlying pathophysiology of FGID is incompletelyunderstood. Visceral hypersensitivity has been variablydemonstrated across a number of FGID, such asfunctional chest pain2–4 which is characterized byrecurrent unexplained midline chest pain.5
Methods used for measuring esophageal sensorimo-tor function face a number of cardinal limitations.Esophageal function may be influenced by a diversearray of factors including psychological factors andactivation of the stress-responsive systems such as theautonomic nervous system (ANS).6 Moreover,such limitations are compounded by the test techniqueitself, which invariably involves the per nasum
or per oral introduction of a catheter, of one kind oranother, with subsequent esophageal intubation. Thisprocess in itself activates a complex stress response,largely mediated by the ANS. Furthermore, manysubjects find this process very traumatic and indeed aproportion cannot tolerate this. Hitherto however, thedetailed interrogation of this ANS-mediated stressresponse to esophageal intubation has been hamperedby a lack of temporal resolution inmany of the surrogatemarkers of ANS tone, such as those conveyed by powerspectral analysis of heart rate variability. This paucity oftemporal resolution is further compounded in theliterature by significant controversy on the specificinterpretation of many proxy measures of ANS tone.7
Nevertheless, recent advances in autonomic neurosci-ence technology has led to considerable improvements,this temporal resolution such that validatedbeat-to-beatparameters of autonomic tone can now be measured.8
Using these novel measures, Paine et al. sought tofurther define theANS response to intubation, in a smallpreliminary group of healthy subjects, broadly demon-strating that sympathetic nervous system (SNS) activa-tion and parasympathetic nervous system (PNS)withdrawal over a total time epoch of 180 s, althoughthis study did not evaluate baseline recovery.9
Given that such techniques are so widely usedacross the study of esophageal sensorimotor function,particularly with the recent observation that auto-
nomic tone may also influence visceral and somaticpain sensitivity in health, a greater understanding ofthis stress response, and their recovery to baselineusing prolonged recordings, is warranted in both healthand disease.10 It is these knowledge gaps that our studyaimed to identify the factors that influence this stressresponse in healthy subjects and patients with func-tional chest pain. We therefore hypothesized thatesophageal intubation activates a fight or flightautonomic response and recovery to baseline maybedifferent in health and disease.
MATERIALS AND METHODS
Subjects
Twenty functional chest pain patients, defined according to theRome III criteria, and 50 healthy subjects took part in the study.5
Patients were identified from the gastrointestinal physiologydatabase at the Royal London Hospital and healthy subjects wererecruited from the residents of the surrounding geographical area.Within 12 months of the study, all patients had a negative cardiacevaluation (either a negative exercise tolerance test or coronaryangiogram) with normal esophageal motility demonstrated onhigh-resolution manometry, normal 24 h pH-metry and a normalesophago-gastro-duodenoscopy with normal biopsies from themid and distal esophagus. All subjects were na!ıve to theexperimental protocol but received written information before-hand and provided written informed consent. Females werestudied in the follicular phase of their menstrual cycle. Subjectswere excluded if they were taking any analgesics, centrally actingmedications or those influencing autonomic responses. Currentsmokers were asked not to smoke for 24 h before the study.Subjects were asked to refrain from alcohol consumption for 24 hprior to the study. All subjects were screened for sub-clinicalanxiety and depression using the validated Hospital Anxiety andDepression Scale and healthy subjects were excluded if theirscores exceeded 7 on either scale.11 All subjects were screened forco-morbid chronic pain disorders. As several measures in thestudy were questionnaire based, those who exceeded a self-deception score, as assessed by the Weinberger AdjustmentInventory, were excluded from the analysis thus ensuringresponse integrity.12 These studies were approved by the EastLondon and the City Ethics Committee 2 (Ref: 08/H0703/47,permission date February 2010). All subjects were na!ıve to thestudy protocol.
Personality & anxiety measures
The validated Big Five Inventory (BFI) was used to measure thepersonality traits of neuroticism (BFI-N) and extroversion (BFI-E).9
State (STAI-S) and trait (STAI-T) anxiety was assessed using thevalidated State-Trait Anxiety Inventory.13 These specific mea-sures were chosen based on our previous studies.9,14
Esophageal intubation & visceral pain induction
Subjects were intubated per nasum with an esophageal catheter(Sandhill Scientific, Oxford, UK), without local anesthetic, so thatits distal tip was positioned 34 cm ab nares. The catheter was
© 2013 John Wiley & Sons Ltd2
A. D. Farmer et al. Neurogastroenterology and Motility

secured using adhesive tape (Micropore, 3M; Healthcare, Brac-knell, UK) applied to the subject’s nose, upper lip, and face tominimize any displacement during the study.
Autonomic nervous system measures
The ANS measures used in this study are summarized in Fig. 1.
Blood pressure Digital arterial blood pressure (BP) was measurednon-invasively using the validated photoplethysmographic tech-nique (Portapres, Amsterdam, The Netherlands).15,16
Skin conductance responses Skin conductance is a putativesympathetic ‘emotional sudomotor’ measure responsive withinmilliseconds to threatening stimuli.17 Skin on the distal digit pulpof the right index and ring fingers was wiped with water andallowed to dry. In each subject, skin conductance electrodes werethen attached and the skin conductance level was zeroed using acommercially available bioamp (Powerlab, AdInstruments,Oxford, UK). The mean skin conductance response (SCR) wasextracted and analyzed off-line.
Heart rate, cardiac vagal tone, and cardiac sensitivity to thebaroreflex Skin was firstly prepared by light excoriation to reduceimpedance and improve signal (Nuprep, DO Weaver & Co,Aurora, CO, USA) in areas for standard three-lead electrocardio-gram (ECG) placement (right and left sub-clavicular and cardiacapex). Electrocardiogram electrodes (Ambu Blue Sensor P,Baltorpbakken, Denmark) were then placed in these areas.Electrocardiogram was acquired at 5 KHz using a commerciallyavailable biosignals acquisition system (NeuroscopeTM, MedifitInstruments, Enfield, UK). The R wave is the first upwarddeflection above the electrical baseline on the ECG and the partof the QRS complex that represents ventricular depolarization.The Neuroscope has an in-built R-wave detection algorithm,which features accuracy to the nearest millisecond, from whichthe R–R interval and heart rate are derived. The Neuroscope alsomeasures brainstem PNS efferent activity, known as cardiac vagaltone (CVT), in real time is measured on a validated linear vagalscale (LVS), where 0 represents full atropinization.8 The
Neuroscope also incorporates beat-to-beat R-R interval and meanBP into an algorithm on a 10-second cycle, calculating cardiacsensitivity to the baroreflex (CSB), an indirect measure ofparasympathetic afferent activity.18 These measures are describedin detail elsewhere,9,10 but in contrast to traditional measures,such as power spectral analysis of heart rate variability, arevalidated for time epochs of less than 1 min.9 It is well-documented that following a stressor, vagal tone plays a majorrole in restoring HR to baseline values.19
Cardiac sympathetic index R-R interval data were extracted fromthe Neuroscope recordings and was hand edited removing anymissed, or extra beats, as these can result in large artifacts.Following this, the R-R data were re-formatted and entered intothe Cardiac Metric program for the calculation of the validatedToichi’s Cardiac Sympathetic Index (CSI).20,21 CSI is a ratio of R-Rintervals and therefore has no units.
Autonomic nervous system recovery times Given that HR is amixed measure of ANS tone, we utilized CSI and CVT assurrogate markers of SNS and PNS recovery, which was definedby the point at which it returned to baseline for at least 30 s.Autonomic parameters were recorded according to internationallyagreed guidelines.22
Protocol
All subjects were studied in the afternoon (from 1400 to 1600 h) ina quiet, temperature controlled (20–22 °C) laboratory. Subjectscompleted the questionnaires and were reclined at 45° on a bed.After attachment of ANS recording equipment, baseline data wasacquired for 15 min. Baseline ANS data were derived from themiddle 5 min of the recording. Subjects were then intubated withthe esophageal catheter, allowed to rest for up to 30 min duringwhich they had continuous ANS monitoring.
Statistical analysis
Data distribution was analyzed using the D’Agostino–Pearsonomnibus K2 normality test.23 Results of quantitative data are
Figure 1 A schematic summary of theautonomic measures used in this study.
© 2013 John Wiley & Sons Ltd 3
Autonomic response to esophageal intubation

presented either as median with interquartile ranges (IRQ) fornon-normally distributed data, or mean ! SD and range forparametric data. For quantitative data, differences between thegroups were assessed using the Student’s t-test in case ofparametric data and using the Wilcoxon matched-pairs test incase of non-parametric data. Correlational analyses were performedusing Spearman’s (rs) coefficient. Multiple linear regression analy-sis was used to assess the association of CSI and CVT recovery timeas the dependent variable and age, gender, personality traits as theindependent variables. All tests were two-tailed, and p < 0.05 wasadopted as the statistical criterion. Analyses were performed usingproprietary software (GraphPad Prism 5, La Jolla, CA, USA andSPSS 18, IBM, New York, NY, USA).
RESULTS
Subjects characteristics
Twenty functional chest pain patients (nine male,median age of 38.7 years, range 28–59 years) and 50subjects (27 males, median age 31.9 years, range20–53 years) were recruited to the study. One patient(male, aged 28.4 years) did not complete the study, heexceeded the self-deception score. All subjects wereCaucasian. All other subjects completed and toleratedthe study well.
Psychological characteristics
In healthy subjects, themean personality scores were asfollows:- BFI-N - 3.6 (IRQ 2.1–4.7), BFI-E - 3.5 (IRQ 2.5–4.9), and the anxiety scores were STAI-S - 33 (IRQ 26.5–40) and STAI-T - 37 (IRQ 30.5–45). Big Five Inventory-Ncorrelated positively with STAI-S (rs = 0.79, p < 0.0001)and STAI-T (rs = 0.44, p < 0.0001) but negatively withBFI-E (rs = "0.5, p = 0.0001). Patients had higher BFI-N(4.8 [IRQ 4.2–4.9] vs 3.6 [IRQ 2.1–4.7], p < 0.0001),STAI- S (43 [IRQ 38–45) vs 33 [IRQ 26.5–40], p < 0.0001)
and STAI-T (45 [IRQ 40–47] vs 37 [IRQ 30.5–45],p = 0.003) in comparison to controls.
Autonomic parameters at baseline and inresponse to intubation
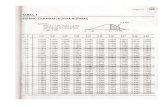
In all subjects, all autonomic parameters displayedsignificant changes in response to intubation. Esoph-ageal intubation resulted in an elevation of HR,systolic blood pressure (SBP), mean blood pressure(MBP), diastolic blood pressure (DBP), CSI, and SCRwith a concomitant decrease of CVT and CSB. Signif-icant differences in baseline heart rate, CVT, and CSIbetween patients and controls were noted. Similarly,differences were also observed in CVT and CSIbetween patients and controls in response to esopha-geal intubation, see Table 1.
Autonomic nervous system recovery times
The CSI median recovery time was 56 s (IRQ 36–81.5 s).The CVT median recovery time was 331 s (IRQ 170.5–544 s). Cardiac sympathetic index and CVT recoverytime positively correlated (rs = 0.81, p < 0.0001),see Fig. 2.
Sympathetic nervous system recovery times
Univariate correlational analysis demonstrated signif-icant associations with BFI-N and STAI-S (rs = 0.7,p < 0.0001 and rs = 0.68, p < 0.0001, respectively).Multiple linear regression analysis was used to assessthe association of CSI recovery time as the dependentvariable and age, gender and the personality traits ofBFI-N, BFI-E, STAI-S, and STAI-T as the independent
Table 1 Comparison of autonomic variables at baseline and in response to esophageal intubation
Autonomic parameters
Baseline Intubation
Controls Patients p-value Controls Patients p-value
Mixed ANS measures HR (bpm) 68.2 ! 11.5 74.2 ! 8.3 0.04* 77.7 ! 12.3 83.4 ! 11.9 0.08SBP (mmHg) 125.5 ! 18.7 123.7 ! 15.3 0.7 141.7 ! 18.7 146 ! 28.2 0.46MBP (mmHg) 80.9 ! 15 83.4 ! 13.8 0.52 93.4 ! 17.7 100.5 ! 20.7 0.15DBP (mmHg) 58.7 ! 14.5 63.3 ! 14.3 0.23 69.1 ! 15.3 77.3 ! 17.7 0.06
PNS measures CVT (LVS) 8.1 (5.7–11.3) 4.7 (3.3–6.8) 0.0002* 6.0 (4.3–7.2) 3.6 (2–4.4) 0.0008*CSB(DRR/DmmHg) 6.0 (4.5–8.3) 4.2 (3.6–6.2) 0.02* 3.0 (1.8–5.6) 2.5 (1.4–4.6) 0.25
SNS measures CSI 2 ! 0.9 2.7 ! 0.6 0.002* 2.4 ! 0.9 2.9 ! 0.5 0.02*SCR (lS) 3.1 ! 2.8 4.2 ! 1.4 0.1 13.9 ! 8.6 18.3 ! 10.8 0.07
HR, SBP, MBP, DBP, CSI, and SCR were parametrically distributed and thus data are expressed as mean ! SD. CVT and CSB were non-parametricand therefore data are expressed as median and IRQ.HR, heart rate; CSI, cardiac sympathetic index; SCR, skin conductance response; CVT, cardiac vagal tone; CSB, cardiac sensitivity to the baroreflex;IRQ, interquartile range; SNS, sympathetic nervous system; PNS, parasympathetic nervous system; ANS, autonomic nervous system.*Significant values.
© 2013 John Wiley & Sons Ltd4
A. D. Farmer et al. Neurogastroenterology and Motility

variables and did not demonstrate any significantindependent associations.
Parasympathetic nervous system recovery times
Univariate correlational analysis demonstrated signif-icant associations between CVT recovery with BFI-Nand STAI-S (rs = 0.87, p < 0.0001 and rs = 0.73,p < 0.0001, respectively). Multiple linear regressionanalysis was used to assess the association of CVTrecovery time as the dependent variablewith age, genderand the personality traits of BFI-N, BFI-E, STAI-S, andSTAI-T as the independent variables. The overall model
fit was R2 – 0.77. Only BFI-N was independentlyassociated with longer CVT recovery times followingesophageal intubation (b = 133.5, SE 17.6, t-7.6,p = 0.0001, 95% confidence interval 98.3–168.7).
Stratification of sympathetic andparasympathetic nervous system recovery timesby neuroticism
In order to dichotomize BFI-N into those with low andhigh scores, the raw scores were first converted into Z-scores and then into T-scores (mean 50, SD !10), amethod similar to that described by Zobel et al. andMcCleery et al.24,25 The mean and SD for the low BFI-N group was 40.9 ! 3.9 and 58.9 ! 4.9 for the highBFI-N group. From this dichotomization, Kaplan–Meier curves were constructed based on CSI and CVTrecovery times for each of the two groups of BFI-N, seeFig. 3. The mean CSI recovery time for the high BFI-Ngroup was 86.4 ! 39.8 s vs 42.7 ! 17.7 s in the lowBFI-N group (p < 0.0001). The mean CVT recoverytime for the high BFI-N group was 521.1 ! 145.3 s vs
196.1 ! 120.6 s in the low BFI-N group (p < 0.0001).
Stratification of sympathetic andparasympathetic nervous system recovery timesby health or disease status
Cardiac sympathetic index and CVT recovery werestratified according to health (n = 50) or functional
A B
Figure 3 Kaplan–Meier curves illustratingthe proportion of cardiac sympathetic index(CSI) recovery (A) and cardiac vagal tone(CVT) recovery (B) in high and lowneuroticism groups. Log rank (Mantel–Cox)tests for CSI (v2 31.6, df 1) and CVT (v2 55, df1) demonstrated statistical significance atp < 0.0001 (*).
Figure 2 The correlation between cardiac sympathetic index (CSI) andcardiac vagal tone (CVT) recovery demonstrating that whilst CSIrecovery times were shorter than CVT, there was a positive correlationbetween them – patients are denoted by circles and healthy subjects bydots (r = 0.81, p < 0.0001).
A B
Figure 4 Box & Whiskers plots (error barsindicating minimum and maximum values)of cardiac sympathetic index (A) and cardiacvagal tone (B) recovery times. *p < 0.0001.
© 2013 John Wiley & Sons Ltd 5
Autonomic response to esophageal intubation

chest pain (n = 19) with results shown in Fig. 4. Themedian CSI recovery time for healthy subjects was46.5 s (IRQ 29–63) vs 112.5 s (IRQ 63.7–165) forpatients, p = 0.0001. The median CVT recovery timefor healthy subjects was 223.5 s (IRQ 137–470.5) vs
549 s (IRQ 432–662) for patients, p = 0.0001.
DISCUSSION
In this study, we have demonstrated that esophagealintubation induces SNS activation and PNS with-drawal. The recovery of PNS tone to baseline waspreceded by that of the SNS tone. Interestingly, in theunivariate analysis both SNS and PNS recovery timeswere positively correlated with neuroticism and stateanxiety scores. In the multiple linear regression anal-ysis, longer PNS tone recovery times were indepen-dently associated with neuroticism scores.Furthermore, when dichotomizing according to per-sonality traits and disease status, our data also suggestimportant differences in SNS and PNS recovery.
The ANS is a hierarchically controlled, bidirec-tional, body–brain interface that integrates afferentbodily inputs and central motor outputs for homeo-static and emotional processes. The pattern of ANSresponse we observed to esophageal intubation was, inpart, what might be reasonably expected in a typical‘fight-flight’ defense response. Nevertheless, it is strik-ing to note that PNS withdrawal significantly out-lasted the SNS activation. This prolonged PNSwithdrawal could represent what Thayer and Friedmanterm cardiac ‘disinhibition’ related to the ‘threatappraisal’.26 The widely held belief among cognitiveneuroscientists is that the default response to anythreat, in this case esophageal intubation, is activationof sympatho-excitatory circuits in preparation foraction. This activation is likely to be related to thephenomenon of ‘negativity bias’ such that negative/threatening information being processed is more likelyto display a degree of preponderance over the posi-tive.27,28 Taken from the evolutionary/survival out-look, this represents an adaptive response that ‘errs’ onthe side of caution. However, the continued chronicperception of threat is considered to be maladaptive, asit is associated with dysregulation endocrine andautonomic output, in addition to cognitive decline.29,30
Thus, in response to, as the subject’s perception ofthreat decreases after intubation has taken place,presumably due to the very nature of the study,reflected in earlier normalization of sympatho-excit-atory influences before those PNS influences.31
Nevertheless, this does not adequately explain thecausal factors of the prolongation of the recovery of
PNS tone to baseline. Until recently, it had been thegenerally accepted opinion that visceral pain waslargely mediated by spinal afferents, with the primaryfunction of vagal afferents being the transmission ofinteroceptive information from the periphery to centralstructures. However, three emerging strands of pre-clinical and clinical evidence have postulated as to therole of the vagus nerve in modulating nociception,particularly from the viscera. Firstly, electrical physi-ological studies have demonstrated that electrical orchemical stimulation of vagus nerve can activatespinothalamic tract neurons.32 Secondly, in animalmodels, Chen et al. demonstrated that topical applica-tion of local anesthetic to sub-diaphragmatic vagalafferents increased pain thresholds33 and more recentlyFuruta et al. observed that following vagotomy colonicpain thresholds were decreased.34 Thirdly, a recentsmall open-label Phase I/II trial of vagus nerve stimu-lation in patients with fibromyalgia reported improve-ments in pain measures.35 By amalgamating thesestrands of evidence, it is possible to conjecture that theprolonged recovery of CVT that we observed in thisstudy was in fact a compensatory antinociceptiveresponse to esophageal intubation, As it is reasonablywell-established that those subjects who have higherneuroticism and anxiety scores demonstrate height-ened pain sensitivity,10,36 it is possible to speculatethat the higher neuroticism and anxiety subjects had aprolonged antinociceptive CVT response due to height-ened pain sensitivity in this group ab initio.
Esophageal intubation is widely utilized in experi-mental and clinical studies across a diverse array ofdisciplines. These techniques have become increas-ingly refined with the passage of time from simplemanometry and balloon inflation, to the barostat tomultimodal techniques combined with high-resolu-tion imaging. Whilst there is little doubt that thisconsiderable body of work has added significantly toour knowledge of esophageal physiology and sensori-motor mechanisms in health and disease, the very actof intubation remains a fundamental physiologicallimitation and arguably a barrier to large-scale recruit-ment to studies. To date, to the best of our knowledge,there is an absence of agreement regarding the timethat should be left between intubation and commence-ment of any intervention or measurement. Thus, itshould not come as any surprise that within thepresent literature, there is considerable variation andtherefore could be a source of potential confounderaffecting many areas of interest including, but notlimited to, GI tract physiological, visceral pain, andfunctional neuroimaging studies. A considerable pro-portion of studies do not report the length of time
© 2013 John Wiley & Sons Ltd6
A. D. Farmer et al. Neurogastroenterology and Motility

between intubation and the application of astimulus.37–40 However, a number of studies, however,report a rest period of between 0 and 15 min36,41,42 yetothers a period greater than 15 min.43,44 Thus giventhis degree of difference, standardization is warranted,particularly when considering balloon distension stud-ies. This consideration has particular salience infunctional chest pain as esophageal hypersensitivityto balloon distension, first described in 1986 byRichter et al. and subsequently confirmed by others,is considered to be a pathophysiological feature in thisdisorder.2,45 However, this hypersensitivity has insuf-ficient specificity and sensitivity for routine diagnosticuse in clinical practice which maybe due to the lack ofthe aforementioned standardization.2,45,46 Moreover,as a wider implication, given the resources and costrequired for conducting research studies, particularlywith respect to functional neuroimaging, the ability todelineate and stratify recovery times following esoph-ageal intubation presents a number of advantages. Forexample, these include the potential for increasingthroughput of participants by not waiting for excessiveperiods following intubation but not at the expense ofintroducing confounders by not leaving enough time.Based on the data presented herein, the measurementof personality traits, through the use of validatedquestionnaires, may allow an individualized approachto subjects, in health and disease, when consideringrecovery times in paradigm design and in standardoperating procedures for esophageal manometry.
Thus, our results may have important ramificationsin the routine clinical practice of esophageal manom-etry. It has recently been demonstrated that peristalticdysfunction within the esophagus may be associatedwith vagal hyper-reactivity47 yet, to date, neither theAmerican Neurogastroenterology and Motility Soci-ety, the European Society of Neurogastroenterologyand Motility48 nor the American GastroenterologicalAssociation49 have made recommendations regardingthe rest periods following intubation. It is also likelythat the British Society of Gastroenterology’s guide-lines of a 5–10 min rest period before measurementsare taken may be insufficient for some individuals,particularly those who have heightened anxiety orneuroticism.50 Furthermore, it is likely that thoughtshould be given to the type, and indeed caliber, ofesophageal catheter that measurements are takenwith. For instance, given the increasingly widespreadadoption of high-resolution esophageal pressure topog-raphy, differences in catheter design may alsoinfluence ANS recovery.
This study is not without its limitations. Whilst thenumber of subjects we studied is reasonably large for
this type of study, whether such results are applicableto larger cohorts of healthy subjects and other FGIDremains to be seen. In addition, we acknowledge thatsome of the differences we have observed in ANSrecovery could be due to purely psychological differ-ences between healthy subjects and patients withfunctional chest pain, given its defining feature ischronic visceral pain, it is possible that there areimportant neurobiological differences in autonomicreactivity, and thus recovery, in response to stress.51
We also readily acknowledge that we have not studiedevery single personality and anxiety factors that mayinfluence ANS response to intubation, for instancemeasures such as depression or coping, we adopted apragmatic approach examining those which areamongst the most widely studied by other groups.Whether these results are also applicable to the per
oral route of esophageal intubation is uncertain,although it is likely that the per nasum routeactivates a similar heightened stress response. Finally,we have not stratified groups according to previousexperience of esophageal intubation. In this study, allpatients had previously undergone esophageal intuba-tion at esophageal manometry yet this previousexperience was variable amongst healthy subjectsand therefore could potentially have contributed tothe elevated STAI-S seen in the former. Nevertheless,STAI-S was not independently associated with pro-longed ANS recovery times in the multiple linearregression analysis. In addition, whether the measure-ment of cardiotropically derived autonomic parame-ters accurately reflects gut-specific autonomic toneremains an area of considerable controversy withinthe field and, in our opinion, to date remains a centralunanswered question.
In conclusion, esophageal intubation activates acomplex ANS response whose recovery is influencedby personality traits and disease status. In futureresearch and clinical studies, these differences shouldbe controlled for when defining rest periods duringprotocol design. Whether such differences are applica-ble to wider patients groups, such as those with a FGIDother than functional chest pain, is uncertain andwarrants further investigation. As an overall recom-mendation, based on these data, we would suggest arest period of 10 min between esophageal intubationand the acquisition of data.
ACKNOWLEDGMENTS
This research/ADF was funded by a Medical Research Councilproject grant. Medical Research Council grant number –MGAB1A1R.
© 2013 John Wiley & Sons Ltd 7
Autonomic response to esophageal intubation

FUNDING
Medical Research Council grant number – MGAB1A1R.
CONFLICTS OF INTEREST
No conflicts of interest
REFERENCES
1 Giamberardino MA. Visceral Pain:Clinical, Pathophysiological andTherapeutic Aspects. Oxford: OxfordUniversity Press, 2009.
2 Rao SS, Gregersen H, Hayek B, Sum-mers RW, Christensen J. Unexplainedchest pain: the hypersensitive, hyper-reactive, and poorly compliant esoph-agus.AnnInternMed1996;124: 950–8.
3 Wingate DL. The irritable bowel syn-drome. Gastroenterol Clin North Am1991; 20: 351–62.
4 Bouin M, Plourde V, Boivin M et al.Rectal distention testing in patientswith irritable bowel syndrome: sensi-tivity, specificity, and predictive val-ues of pain sensory thresholds.Gastroenterology 2002; 122: 1771–7.
5 Drossman DA. Rome III: The Func-tional Gastrointestinal Disorders, 3rdedn. McLean, VA: Degnon Associates,2006.
6 Farmer AD, Aziz Q. Visceral painhypersensitivity in functional gastro-intestinal disorders. Br Med Bull2009; 91: 123–36.
7 Reyes del Paso GA, Langewitz W,Mulder LJ, van Roon A, Duschek S.The utility of low frequency heart ratevariability as an index of sympatheticcardiac tone: a review with emphasison a reanalysis of previous studies.Psychophysiology 2013; 50: 477–87.
8 Julu PO. A linear scale for measuringvagal tone in man. J Auton Pharmacol1992; 12: 109–15.
9 Paine P, Kishor J, Worthen SF, Greg-ory LJ, Aziz Q. Exploring relation-ships for visceral and somatic painwith autonomic control and person-ality. Pain 2009; 144: 236–44.
10 Farmer AD, Coen SJ, Kano M et al.Psychophysiological responses topain identify reproducible humanclusters. Pain 2013; doi: 10.1016/j.pain.2013.05.016.
11 Zigmond AS, Snaith RP. The hospitalanxiety and depression scale. ActaPsychiatr Scand 1983; 67: 361–70.
12 Weinberger DA, Schwartz GE, David-son RJ. Low-anxious, high-anxious,and repressive coping styles: psycho-metric patterns and behavioral andphysiological responses to stress. JAbnorm Psychol 1979; 88: 369–80.
13 Spielberger CD.Manual for the State/TraitAnxietyInventory (FormY): (SelfEvaluationQuestionnaire). Palo Alto:Consulting Psychologists Press, 1983.
14 Paine P, Worthen SF, Gregory LJ,Thompson DG, Aziz Q. Personalitydifferences affect brainstem auto-nomic responses to visceral pain.Neurogastroenterol Motil 2009; 21:1155–e98.
15 Benarroch EE, Opfer-Gehrking TL,Low PA. Use of the photoplethysmo-graphic technique to analyze the Val-salva maneuver in normal man.Muscle Nerve 1991; 14: 1165–72.
16 Eckert S,HorstkotteD.Comparison ofPortapres non-invasive blood pressuremeasurement in the finger with intra-aortic pressure measurement duringincremental bicycle exercise. BloodPress Monit 2002; 7: 179–83.
17 Cacioppo JT, Tassinary LG, BerntsonGG. Handbook of Psychophysiology,3rd edn. Cambridge: CambridgeUniversity Press, 2007.
18 Julu PO, Cooper VL, Hansen S, Hains-worth R. Cardiovascular regulation inthe period preceding vasovagal syn-cope in conscious humans. J Physiol2003; 549: 299–311.
19 Goldberger JJ, Le FK, Lahiri M, Kan-nankeril PJ, Ng J, Kadish AH. Assess-ment of parasympathetic reactivationafter exercise. Am J Physiol HeartCirc Physiol 2006; 290: H2446–52.
20 Cook EW 3rd, Miller GA. Digitalfiltering: background and tutorial forpsychophysiologists. Psychophysiol-ogy 1992; 29: 350–67.
21 Toichi M, Sugiura T, Murai T, Seng-oku A. A new method of assessingcardiac autonomic function and itscomparisonwith spectral analysis andcoefficient of variation of R-R interval.J Auton Nerv Syst 1997; 62: 79–84.
22 Heart rate variability standards ofmeasurement, physiological interpre-tation and clinical use. Task Force ofthe European Society of Cardiologyand the North American Society ofPacing and Electrophysiology. Circu-lation 1996; 93: 1043–65.
23 D’Agostino RB, Stephens MA. Good-ness-of-fit Techniques. New York: M.Dekker, 1986.
24 Zobel A, Barkow K, Schulze-Raus-chenbach S et al. High neuroticism
and depressive temperament areassociated with dysfunctional regula-tion of the hypothalamic-pituitary-adrenocortical system in healthyvolunteers. Acta Psychiatr Scand2004; 109: 392–9.
25 McCleery JM, Goodwin GM. Highand low neuroticism predict differentcortisol responses to the combineddexamethasone–CRH test. Biol Psy-chiatry 2001; 49: 410–5.
26 Thayer JF, Friedman BH. Stop that!Inhibition, sensitization, and theirneurovisceral concomitants. Scand JPsychol 2002; 43: 123–30.
27 Cacioppo JT, Gardner WL. Emotion.Annu Rev Psychol 1999; 50: 191–214.
28 Herry C, Bach DR, Esposito F et al.Processing of temporal unpredictabil-ity in human and animal amygdala.J Neurosci 2007; 27: 5958–66.
29 McEwen BS, Sapolsky RM. Stress andcognitive function. Curr Opin Neu-robiol 1995; 5: 205–16.
30 Seeman TE, Crimmins E. Socialenvironment effects on health andaging: integrating epidemiologic anddemographic approaches and perspec-tives. Ann N Y Acad Sci 2001; 954:88–117.
31 Thayer JF, Sternberg E. Beyond heartrate variability: vagal regulation ofallostatic systems. Ann N Y Acad Sci2006; 1088: 361–72.
32 Chandler MJ, Zhang J, Foreman RD.Vagal, sympathetic and somatic sen-sory inputs to upper cervical (C1-C3)spinothalamic tract neurons inmonkeys. J Neurophysiol 1996; 76:2555–67.
33 Chen SL, Wu XY, Cao ZJ et al. Sub-diaphragmatic vagal afferent nervesmodulate visceral pain. Am J PhysiolGastrointest Liver Physiol 2008; 294:G1441–9.
34 Furuta S, Matsumoto K, Horie S, Su-zuki T, Narita M. Subdiaphragmaticvagotomy induces a functional changein visceral Adelta primary afferentfibers in rats. Synapse 2012; 66:369–71.
35 Lange G, Janal MN, Maniker A et al.Safety and efficacy of vagus nervestimulation in fibromyalgia: a phaseI/II proof of concept trial. Pain Med2011; 12: 1406–13.
© 2013 John Wiley & Sons Ltd8
A. D. Farmer et al. Neurogastroenterology and Motility

36 Sharma A, VanOudenhove L, Paine P,Gregory L, Aziz Q. Anxiety increasesacid-induced esophageal hyperalgesia.PsychosomMed 2010; 72: 802–9.
37 Andreollo NA, Thompson DG, Ken-dall GP, Earlam RJ. Responses of theupper esophageal sphincter andesophageal body to graded intralumi-nal distension. Braz J Med Biol Res1987; 20: 165–73.
38 Kendall GP, Thompson DG, Day SJ,Garvie N. Motor responses of theoesophagus to intraluminal disten-sion in normal subjects and patientswith oesophageal clearance disorders.Gut 1987; 28: 272–9.
39 Smout AJ, DeVore MS, Dalton CB,Castell DO. Cerebral potentialsevoked by oesophageal distension inpatients with non-cardiac chest pain.Gut 1992; 33: 298–302.
40 Lu HC, Hsieh JC, Lu CL et al. Neu-ronal correlates in the modulation ofplacebo analgesia in experimentally-induced esophageal pain: a 3T-fMRIstudy. Pain 2010; 148: 75–83.
41 Rao SS, Patel RS. How useful aremanometric tests of anorectal func-
tion in the management of defecationdisorders? Am J Gastroenterol 1997;92: 469–75.
42 McMahon BP, Frokjaer JB, Kunwald Pet al. The functional lumen imagingprobe (FLIP) for evaluation of theesophagogastric junction. Am J Phys-iol Gastrointest Liver Physiol 2007;292: G377–84.
43 Galeazzi F, Luca MG, Lanaro D et al.Esophageal hyperalgesia in patientswith ulcerative colitis: role of exper-imental stress. Am J Gastroenterol2001; 96: 2590–5.
44 Remes-Troche JM, Attaluri A, Cha-hal P, Rao SS. Barostat or dynamicballoon distention test: which tech-nique is best suited for esophagealsensory testing? Dis Esophagus 2012;25: 584–9.
45 Richter JE, Barish CF, Castell DO.Abnormal sensory perception inpatients with esophageal chest pain.Gastroenterology 1986; 91: 845–52.
46 Nasr I, Attaluri A, Hashmi S, Greger-sen H, Rao SS. Investigation of esoph-ageal sensation and biomechanicalproperties in functional chest pain.
Neurogastroenterol Motil 2010; 22:520–6, e116.
47 Amarasiri DL, Pathmeswaran A,Dassanayake AS, de Silva AP, Ranas-inha CD, de Silva HJ. Esophagealmotility, vagal function and gastro-esophageal reflux in a cohort of adultasthmatics. BMC Gastroenterol2012; 12: 140.
48 Murray JA, Clouse RE, Conklin JL.Components of the standard oesoph-ageal manometry. Neurogastroenter-ol Motil 2003; 15: 591–606.
49 Pandolfino JE, Kahrilas PJ, AmericanGastroenterological Association.AGA technical review on the clinicaluse of esophageal manometry. Gas-troenterology 2005; 128: 209–24.
50 Bodger K, Trudgill N. Guidelines forOesophageal Manometry and pHMonitoring [New edn]. Bodger K,Trudgill N, eds. Great Britain: BritishSociety of Gastroenterology, 2006.
51 Farmer AD, Kano M, Coen SJ, Aziz Q.Psychophysiological responses tooesophageal stimulation in func-tional chest pain: a case controlstudy. Gut 2011; 60: A153.
© 2013 John Wiley & Sons Ltd 9
Autonomic response to esophageal intubation

Graphical AbstractThe contents of this page will be used as part of the graphical abstract
of html only. It will not be published as part of main.
The psychological trait of neuroticism retards autonomic recovery following esophageal intubation in health andfunctional chest pain.