Survival Benefit with Capecitabine/Docetaxel Versus Docetaxel Alone: Analysis of Therapy in a...
-
Upload
david-miles -
Category
Documents
-
view
212 -
download
0
Transcript of Survival Benefit with Capecitabine/Docetaxel Versus Docetaxel Alone: Analysis of Therapy in a...
Clinical Breast Cancer October 2004 • 273
IntroductionSingle-agent docetaxel has been shown to improve the
overall survival (OS) of patients with anthracycline-pretreat-ed metastatic breast cancer (MBC).1,2 The oral fluoropyrimi-dine capecitabine was designed to generate 5-fluorouracil (5-FU) preferentially in tumor tissue by exploiting the higheractivity of thymidine phosphorylase in tumor compared withnormal tissue.3,4 Clinical studies have shown that single-agent capecitabine is an effective and tolerable treatment inpatients with heavily pretreated MBC. In patients whose dis-ease has progressed with prior anthracycline- and taxane-
Submitted: Mar 2, 2004; Revised: May 14, 2004; Accepted: May 14, 2004
Address for correspondence: David W. Miles, MD, Clinical Oncology Unit,Guy’s Hospital, St. Thomas St, London, SE1 9RT, UKFax: 44-20-7188-0919; e-mail: [email protected]
1Guy’s and St Thomas’ Hospital, London, UK 2US Oncology, Tyler Cancer Center, TX 3NN Petrov Research Institute of Oncology, St Petersburg, Russia 4ISSSTE Hospital, Mexico City5Institut Bergonié, Bordeaux, France 6Perth Oncology, West Perth, Australia7Taipei Veterans General Hospital, Taiwan 8Hôpital Notre Dame, Montréal, Canada 9Baylor Sammons Cancer Center, US Oncology, Dallas, TX
Survival Benefit with Capecitabine/DocetaxelVersus Docetaxel Alone: Analysis of Therapy in a Randomized Phase III Trial
In a large phase III trial of 511 patients with anthracycline-pretreated advanced/metastatic breast cancer,capecitabine/docetaxel combination therapy was shown to have significantly superior efficacy compared withsingle-agent docetaxel, including superior progression-free and overall survival and objective response rate. Anupdated survival analysis with ≥ 27 months follow-up shows that patients receiving combination therapy main-tained significantly superior survival (hazard ratio [HR], 0.777 [95% CI, 0.645-0.942]; P < 0.01; median sur-vival, 14.5 months vs. 11.5 months) compared with those receiving single-agent docetaxel. Following the fail-ure of docetaxel monotherapy, 35% of patients did not receive additional cytotoxic chemotherapy. Among pa-tients randomized to single-agent docetaxel, only those given poststudy single-agent capecitabine had signifi-cantly prolonged survival compared with those given any other poststudy chemotherapy (HR, 0.500; P =0.0046; median survival, 21.0 months vs. 12.3 months, respectively). By contrast, poststudy vinorelbine-con-taining chemotherapy did not affect survival following progression on single-agent docetaxel compared withother poststudy chemotherapy regimens (HR, 1.014; P = 0.94; median survival, 13.5 months vs. 12.6 months,respectively). Among patients randomized to combination therapy, discontinuing docetaxel of capecitabine hasa similar effect on survival (HR, 0.720; P = 0.20; median survival, 15.8 months vs. 18.3 months, respectively).Median survival was 18.3 months in patients who discontinued docetaxel and continued to receive capecitabineversus 15.8 months in patients who discontinued capecitabine and continued to receive docetaxel, with a trendtoward improved survival in patients continuing to receive capecitabine. Although this is a retrospective analy-sis, these data suggest that the sequential administration of docetaxel followed by capecitabine is associatedwith prolonged survival in patients who are candidates for sequential single-agent therapy.
Clinical Breast Cancer, Vol. 5, No. 4, 273-278, 2004Key words: Anthracyclines, Combination therapy, Taxanes, Vinorelbine
contribution
Abstract
original
David Miles,1 Svetislava Vukelja,2 Vladimir Moiseyenko,3Guadalupe Cervantes,4 Louis Mauriac,5 Guy Van Hazel,6Wing-Yiu Liu,7 Jean-Pierre Ayoub,8 Joyce A. O’Shaughnessy9
Electronic forwarding or copying is a violation of US and International Copyright Laws.Authorization to photocopy items for internal or personal use, or the internal or personal use of specific clients, is granted by Cancer Information Group, ISSN #1526-8209, provided the appropriate fee is paid directly to Copyright Clearance Center, 222 Rosewood Drive, Danvers, MA 01923 USA 978-750-8400.
274 • Clinical Breast Cancer October 2004
Survival Benefit of Capecitabine/Docetaxel Versus Docetaxel Alone
containing regimens, single-agent capecitabine produces re-sponse rates of 15%-28%, disease control rates of 57%-63%,and median survival of approximately 1 year.5-9
Capecitabine and docetaxel are highly active as singleagents, with distinct mechanisms of action and little overlapof key toxicities,1,5,6 and with capecitabine associated with alow incidence of myelosuppression. In addition, taxanes fur-ther upregulate thymidine phosphorylase in tumor tissueand are synergistic with capecitabine in breast cancerxenograft models.10,11 Therefore, it was predicted that thecombination of capecitabine and docetaxel would offer highantitumor activity.
A phase III trial in 511 patients with anthracycline-pre-treated MBC demonstrated the superior efficacy ofcapecitabine/docetaxel.12 The combination resulted in signifi-cantly superior median time to disease progression com-pared with single-agent docetaxel (6.1 months vs. 4.2months; P = 0.0001). The combination regimen also demon-strated a significantly superior objective response rate (42%vs. 30%; P = 0.006). With minimum follow-up of 23 months, asuperior median OS of 14.5 months with capecitabine/docetaxelwas observed, compared with 11.5 months with single-agent do-
cetaxel. At 12 months, the survival rate was 57% (95% CI, 51%-63%) with combination therapy versus 47% (95% CI, 41%-53%)with docetaxel alone.
Compared with single-agent docetaxel, patients receivingdocetaxel plus full-dose capecitabine (1250 mg/m2 twicedaily) had a higher incidence of grade 3 adverse events, es-pecially hand-foot syndrome. However, grade 4 neutropeniawas more common with single-agent docetaxel than withcapecitabine/docetaxel. There were no significant differencesin patients’ quality of life between treatment groups.12
In this phase III trial, a high proportion of patients in bothtreatment arms received poststudy chemotherapy. Effectivepost-study therapy could significantly influence survival.Therefore, we have performed a retrospective analysis ofdata from the study to explore the impact of poststudy treat-ment on survival.
Patients and MethodsPatient Population
Eligibility criteria have been described in detail.12 In brief,eligible patients were female, aged ≥ 18 years, with bidi-mensionally measurable, unresectable, locally advancedand/or metastatic disease. All patients had recurrent breastcancer after anthracycline treatment. Patients were ineligi-ble if they had previously received docetaxel as therapy inthe adjuvant or metastatic settings or if they had received ≥ 3chemotherapy regimens for advanced/metastatic disease.
Study TreatmentPatients were stratified according to whether they had re-
ceived prior paclitaxel therapy. They were randomized to re-ceive oral capecitabine 1250 mg/m2 twice daily on days 1-14plus docetaxel 75 mg/m2 administered as a 1-hour intra-venous infusion on the first day of each 21-day cycle(capecitabine/docetaxel combination) or docetaxel 100mg/m2 administered as a 1-hour intravenous infusion on thefirst day of each 21-day cycle (single-agent docetaxel).
Patients who exhibited a response or stable disease after 6weeks of therapy continued to receive treatment until dis-ease progression or the development of unacceptable toxici-ty. In the combination arm, patients were regarded as re-maining on study therapy if docetaxel was discontinued be-fore disease progression and the patients continued to re-ceive capecitabine alone. However, if capecitabine was dis-continued before disease progression and patients continuedto receive single-agent docetaxel, patients were considered tobe receiving docetaxel as poststudy treatment. The choice ofpoststudy therapy administered following disease progres-sion on study therapy was not defined in the protocol andwas made at the treating physician’s discretion.
Statistical MethodsThe impact of poststudy treatment on OS was assessed
using a proportional-hazards regression model. A 2-sidedlog-rank test (α = 0.05) was used to test differences in OS.
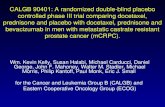
Overall Survival After a Minimum Follow-upof 27 Months
Figure 1
40
20
60
80
100
16 0 1284 36
Time (Months)
Estim
ated
Pro
babi
lity
of O
vera
ll Su
rviva
l (%
)
40 4420 4824 28 32
Docetaxel/CapecitabineDocetaxel Hazard Ratio = 0.777 Log-Rank P < 0.01
11.5 14.5
Surgery
Radiation Therapy
Systemic Therapy
Chemotherapy
Hormone therapy
Trastuzumab
Patients Receiving Poststudy Therapies for Breast CancerTable 1 Docetaxel/
Capecitabine(n = 255)
DocetaxelAlone
(n = 256)
17 (7%)
82 (32%)
204 (80%)
184 (72%)
84 (33%)
25 (10%)
12 (5%)
81 (32%)
185 (72%)
166 (65%)
77 (30%)
24 (9%)
Therapy
Clinical Breast Cancer October 2004 • 275
ResultsPatient Population
In total, 511 patients were enrolled from 75 centers in 16countries. The intent-to-treat population comprised 255 pa-tients in the combination arm and 256 patients in the single-agent arm.
The baseline characteristics and treatment histories of pa-tients were well balanced between the 2 treatment groupsand have been previously described.12 As defined in the pro-tocol, all patients had received prior anthracycline-basedchemotherapy for early-stage or advanced disease. Approxi-mately one third of patients in each arm received studytreatment as first-line therapy for metastatic disease (35%in the combination arm and 31% in the single-agent arm),and approximately two thirds received study treatment assecond- or third-line therapy (65% in the combination armand 68% in the single-agent arm).12
EfficacyAn updated survival analysis performed after a minimum
follow-up of 27 months showed that the OS advantage of thedocetaxel/capecitabine combination was maintained versussingle-agent docetaxel. Median survival remained at 14.5months (95% CI, 12.3-16.3; 82% of events) with the combi-nation and at 11.5 months (95% CI, 9.8-12.7; 87% of events)with single-agent docetaxel (hazard ratio [HR], 0.777 [95%CI, 0.645-0.942]; P < 0.01; Figure 1).
Poststudy Therapies for Breast CancerAfter a minimum follow-up of 23 months, 218 patients
(85%) in the combination arm and 198 patients (77%) in thedocetaxel arm received ≥ 1 poststudy treatment for breastcancer. Similar percentages of patients in the 2 treatmentgroups received poststudy surgery, radiation therapy, en-docrine therapy, and systemic therapy (Table 1). The ma-jority of patients received poststudy chemotherapy (72% inthe combination arm and 65% in the docetaxel arm).
A similar number of poststudy chemotherapy regimenswere given to patients in each treatment arm, with most ofthose given poststudy chemotherapy receiving 1-2 subse-quent treatment regimens (Table 2). In addition, a similarproportion of patients in each treatment arm received post-study combination or single-agent chemotherapy.
The treatment arms were well balanced with regard tothe range of cytotoxic agents administered during poststudytherapy (Table 3), except for poststudy capecitabine andpoststudy docetaxel. Poststudy capecitabine was adminis-tered more frequently in the single-agent arm (18%) than inthe combination arm (3%), and poststudy docetaxel was ad-ministered more frequently in the combination arm (21%)than in the single-agent arm (7%). Of those patients who re-ceived poststudy docetaxel after combination therapy, twothirds were patients who had capecitabine therapy discon-tinued prior to disease progression but continued with doc-etaxel alone. As described earlier, in accordance with the
prespecified protocol criteria, docetaxel in these patientswas classified as poststudy therapy.
The most frequently administered poststudy chemother-apeutic agent was vinorelbine, as monotherapy or in combi-nation with other therapeutic agents. The most commonlyused first poststudy combination regimen was vinorelbineplus a second chemotherapeutic agent (predominantly 5-FU),administered to 7% of patients in both arms. Some patients(11%) in each arm received poststudy anthracycline thera-py. Fifty-two patients (20%) in the combination arm re-ceived poststudy 5-FU; of these, 10 patients (4%) receivedsingle-agent 5-FU and 42 patients (16%) received 5-FU incombination with another cytotoxic agent.
David Miles et al
Patients Receiving Post-study Chemotherapy
Poststudy CombinationChemotherapy (Any Line)
Poststudy Single-AgentChemotherapy (Any Line)
Number of Poststudy Chemotherapy Regimens
1
2
3
≥ 4
Number of Poststudy Chemotherapy RegimensTable 2 Docetaxel/
Capecitabine(n = 255)
DocetaxelAlone
(n = 256)
184
54%
46%
60
29
5
7
166
51%
49%
54
28
14
4
Patients Receiving Specific Poststudy Cytotoxic AgentsTable 3 Docetaxel/
Capecitabine(n = 255)
DocetaxelAlone
(n = 256)
8 (3%)
42 (16%)
10 (4%)
85 (33%)
29 (11%)
77 (30%)
29 (11%)
53 (21%)
5 (2%)
46 (18%)
47 (18%)
13 (5%)
71 (28%)
28 (11%)
40 (16%)
24 (9%)
18 (7%)
2 (1%)
Capecitabine
5-FU
In combination therapy
Alone
Vinorelbine
Anthracyclines
Taxanes
Paclitaxel
Docetaxel
Both
Therapy
276 • Clinical Breast Cancer October 2004
Survival Benefit of Capecitabine/Docetaxel Versus Docetaxel Alone
Impact of the First Poststudy Chemotherapy on Outcome After Single-Agent Docetaxel
Among patients initially randomized to receive single-agent docetaxel, those who received single-agentcapecitabine as their first poststudy chemotherapy had im-proved median OS compared with patients who received anyother chemotherapy agent. The HR for death in patientswho received single-agent capecitabine after study versus allother first poststudy chemotherapy agents was 0.500, indi-cating a 50% reduction in risk of dying (P = 0.0046) associ-ated with administration of capecitabine following progres-
sion on docetaxel. Median OS was 21.0 months (95% CI,15.6-27.6 months) in patients who received capecitabine fol-lowing docetaxel versus 12.3 months (95% CI, 10.5-14.0months) in those who received any other chemotherapyagent following docetaxel (Figure 2). Of the 128 patients whoreceived poststudy chemotherapy after single-agent docetax-el, 78 received a combination, most commonly 5-FU/vinorel-bine or cyclophosphamide/methotrexate/5-FU, and 50 re-ceived another single agent, most commonly vinorelbine, 5-FU, or additional taxanes.
In contrast, the administration of vinorelbine, the mostfrequently used poststudy chemotherapy agent, either as asingle agent or in combination, as first poststudy therapy didnot provide a survival benefit versus the administration of allother chemotherapy agents except capecitabine (Figure 3).The hazard ratio for death for patients who received vi-norelbine versus those who received any other chemothera-py agents, excluding capecitabine, is 1.014, indicating thatthe risk of death was similar in both groups (P = 0.94). Me-dian survival was 13.5 months (95% CI, 11.6-19.6 months) inpatients who received vinorelbine following progression ondocetaxel versus 12.6 months (95% CI, 11.5-15.6 months) inpatients who received any other chemotherapy agent follow-ing docetaxel, excluding capecitabine.
Impact of Discontinuing Docetaxel orCapecitabine in Patients who Received the Docetaxel/Capecitabine Combination
Among patients who were treated with the docetaxel/capecitabine combination, 45 patients (18%) discontinued do-cetaxel before disease progression and continued withcapecitabine alone, and 34 patients (13%) discontinuedcapecitabine before disease progression and continued withdocetaxel alone. Analysis of these subgroups showed that dis-continuing docetaxel or capecitabine has a similar impact onsurvival (HR, 0.720; P = 0.20; Figure 4). Median OS was 18.3months (95% CI, 14.5-23.4 months) in patients who discon-tinued docetaxel and continued to receive capecitabine versus15.8 months (95% CI, 9.9-21.5 months) in patients who dis-continued capecitabine and continued to receive docetaxel,with a trend toward improved survival in patients who con-tinued to receive capecitabine.
DiscussionThe addition of capecitabine to docetaxel 75 mg/m2 re-
sulted in a significant improvement in OS compared withsingle-agent docetaxel 100 mg/m2 in patients with anthracy-cline-pretreated MBC, a benefit that was maintained after aminimum follow-up of 27 months. The trial was not designedto determine whether combined docetaxel/capecitabine pro-vides superior benefit compared with the sequential single-agent administration of each agent. The debate over sequen-tial versus combination chemotherapy in patients with MBChas generated controversy in the oncology community. Todate, no combination chemotherapy regimen has beenshown to give a significant survival benefit over sequential
Median Overall Survival After CapecitabineFollowing Docetaxel Versus Other ChemotherapyAgents Following Docetaxel
Figure 2
40
20
60
80
100
16 0 1284 36
Time After Randomization to Docetaxel Arm (Months)
Estim
ated
Pro
babi
lity
(%)
4020 24 28 32
Single Agent CapecitabineAll Other Chemotherapy Hazard Ratio = 0.500 Log-Rank P = 0.0046
Impact of poststudy chemotherapy on survival of patients randomized to single-agent docetaxel: single-agent capecitabine (n = 28) as first poststudy treatment versus all other first poststudy chemotherapy regimens (n = 128).
12.3 21.0
Survival Benefit with Vinorelbine as a Single Agentor in Combination
Figure 3
40
20
60
80
100
16 0 1284 36
Time After Randomization to Docetaxel Arm (Months)
Estim
ated
Pro
babi
lity
(%)
4020 24 28 32
Vinorelbine-Containing Therapy*
All Other Chemotherapy
Hazard Ratio = 1.014 Log-Rank P = 0.94
*Vinorelbine as a single agent or in combination.Impact of poststudy chemotherapy on survival of patients randomized to single-agent docetaxel: vinorelbine-based poststudy treatment (n = 50) versus other first poststudy chemotherapy regimens (n = 106).
12.6 13.5
Clinical Breast Cancer October 2004 • 277
administration of the same single agents. In a landmarkphase III trial, patients with MBC received single-agent dox-orubicin followed at disease progression by paclitaxel alone(n = 224), paclitaxel alone followed at progression by single-agent doxorubicin (n = 229), or the combination of doxoru-bicin/paclitaxel (n = 230) as first-line chemotherapy.13 Effi-cacy was similar in the 2 sequential arms, but response rateand time to treatment failure were significantly superior in thecombination arm. However, these improvements did not trans-late into a significant improvement in OS. Two other trialshave also failed to demonstrate a benefit for combination ther-apy versus sequential administration of the same agents inMBC.14,15 Treatment-related toxicities are generally greaterwith combination chemotherapy than with single agents, animportant factor in the choice of treatment regimen.
In the present study, 35% of patients who received single-agent docetaxel did not receive poststudy chemotherapy fol-lowing disease progression. These patients were unable tobenefit from capecitabine or any other poststudy therapy be-cause of the higher early death rate observed with single-agent docetaxel compared with combination therapy or a de-terioration in their functional status, that precluded furtherchemotherapy. This suggests that a subset of patients withclinically significant tumor burden and/or rapidly progressivedisease is more likely to benefit from combination docetax-el/capecitabine than from sequential single agents. The sig-nificantly longer OS with poststudy capecitabine followingsingle-agent docetaxel, taken together with the longer sur-vival in patients given combination therapy, suggests thatcapecitabine can favorably affect the natural history of MBCwhether it is given together with docetaxel or following doc-etaxel. A study by the Mexican Oncology Study Group tocompare capecitabine followed at progression by taxane ther-apy versus capecitabine in combination with taxane therapy(docetaxel or paclitaxel) is ongoing.16 An initial analysis of re-sponse rates, time to disease progression, and 1-year survivalshows no significant difference in outcomes in patients whoreceived combined capecitabine/taxane versus capecitabinefollowed at disease progression by a taxane.16,17
ConclusionThis retrospective analysis of the OS rates of patients
treated with capecitabine following single-agent docetaxelshows a survival benefit similar to that achieved with com-bined docetaxel/capecitabine. This trial did not have acrossover design, and caution should be exercised in inter-preting the current subgroup analyses, which are based onsmall numbers of patients. However, these results are con-sistent with phase III study results that have shown no OSadvantage of combination chemotherapy compared with se-quential single-agent administration.13,14 Based on the pres-ent analysis, it appears that the combination ofdocetaxel/capecitabine and the sequential administration ofthese agents are excellent treatment options for patients withMBC. However, because more patients who received single-agent docetaxel died within 6 months of beginning therapy
compared with those who received combined docetaxel/capecitabine, patients with life-threatening or rapidly pro-gressive anthracycline-pretreated MBC may be best treatedwith the docetaxel/ capecitabine combination.
References1. Nabholtz JM, Senn HJ, Bezwoda WR, et al. Prospective randomized
trial of docetaxel versus mitomycin plus vinblastine in patients withmetastatic breast cancer progressing despite previous anthracycline-containing chemotherapy. J Clin Oncol 1999; 17:1413-1424.
2. Jones S, Erban J, Overmoyer B, et al. Randomized trial comparing do-cetaxel and paclitaxel in patients with metastatic breast cancer.Breast Cancer Res Treat 2003; 82(suppl 1):S9 (Abstract #10).
3. Miwa M, Ura M, Nishida M, et al. Design of a novel oral fluoropyrim-idine carbamate, capecitabine, which generates 5-fluorouracil selec-tively in tumors by enzymes concentrated in human liver and cancertissue. Eur J Cancer 1998; 34:1274-1281.
4. Schüller J, Cassidy J, Dumont E, et al. Preferential activation ofcapecitabine in tumor following oral administration in colorectal can-cer patients. Cancer Chemother Pharmacol 2000; 34:293-296.
5. Blum JL, Jones SE, Buzdar AU, et al. Multicenter phase II study ofcapecitabine in paclitaxel-refractory metastatic breast cancer. J ClinOncol 1999; 17:485-493.
6. Blum JL, Dieras V, Lo Russo PM, et al. Multicenter, phase II study ofcapecitabine in taxane-pretreated metastatic breast carcinoma. Can-cer 2001; 92:1759-1768.
7. Reichardt P, von Minckwitz G, Thuss-Patience PC, et al. Multicenterphase II study of oral capecitabine (Xeloda®) in patients withmetastatic breast cancer relapsing after treatment with a taxane-con-taining therapy. Ann Oncol 2003; 14:1227-1233.
8. Fumoleau P, Largillier P, Clippe C, et al. Multicentre, phase II studyevaluating capecitabine monotherapy in patients with anthracycline-and taxane-pretreated metastatic breast cancer. Eur J Cancer 2003;40:536-542.
9. Capecitabine/bevacizumab compared to capecitabine alone in pre-treated metastatic breast cancer: results of a phase III study [Re-search in Brief]. Clin Breast Cancer 2003; 3:375-377.
10. Sawada N, Ishikawa T, Fukase Y, et al. Induction of thymidine phos-phorylase activity and enhancement of capecitabine efficacy byTaxol/Taxotere in human cancer xenografts. Clin Cancer Res 1998;4:1013-1019.
11. Fujimoto-Ouchi K, Yasuno H, Tanaka Y. Schedule-dependency of an-titumor activity in combination therapy with capecitabine (Xeloda®)and docetaxel in breast cancer models. Proc Am Assoc Cancer Res2001; 42a.
12. O’Shaughnessy J, Miles D, Vukelja S, et al. Superior survival withcapecitabine plus docetaxel combination therapy in anthracycline-
David Miles et al
Impact on Survival of Discontinuing Docetaxel or Capecitabine
Figure 4
40
20
60
80
100
16 0 1284 36
Time (Months)
Estim
ated
Pro
babi
lity
(%)
4020 24 28 32
CapecitabineMonotherapy AfterDiscontinuationof Docetaxel
Docetaxel AfterDiscontinuationof CapcitabineMonotherapy
Hazard Ratio = 0.720
Log-Rank P = 0.20
Impact of poststudy chemotherapy on survival of patients randomized to docetaxel/capecitabine who discontinued docetaxel (n = 45) versus those who discontinued capecitabine (n = 34) prior to disease progression.
15.8 18.3
278 • Clinical Breast Cancer October 2004
Survival Benefit of Capecitabine/Docetaxel Versus Docetaxel Alone
pretreated patients with advanced breast cancer: phase III trial re-sults. J Clin Oncol 2002; 12:2812-2823.
13. Sledge GW, Neuberg D, Bernardo P, et al. Phase III trial of doxoru-bicin, paclitaxel, and the combination of doxorubicin and paclitaxel asfront-line chemotherapy for metastatic breast cancer; an Intergrouptrial (E1193). J Clin Oncol 2003; 21:588-592.
14. Joensuu H, Holli K, Heikkinen M, et al. Combination chemotherapyversus single-agent therapy as first- and second-line treatment inmetastatic breast cancer: a prospective randomized trial. J Clin Oncol1998; 16:3720-3730.
15. Koroleva I, Wojtukiewicz M, Zaluski J, et al. Preliminary results of aphase III randomized trial of Taxotere (T) and doxorubicin (A) given
in combination or sequentially as first line chemotherapy (CT) formetastatic breast cancer (MBC). Proc Am Soc Clin Oncol 2001; 20:30a(Abstract #117).
16. Reyes S, Torrecillas L, Acosta A, et al. Capecitabine and taxanes: com-bination versus sequential therapy in anthracycline-pretreatedmetastatic breast cancer (MBC): findings from the Mexican OncologyStudy Group (MOSG) phase III trial. Eur J Cancer 2003; 1(suppl5):S136 (Abstract #447).
17. Torrecillas L, Cortes P, Tokunaga J, et al. Capecitabine monotherapyor combined with taxanes: early results in quality of life in patientswith metastatic breast cancer. Proc Am Soc Clin Oncol 2003; 22:749(Abstract #3011).