Suppression of experimental autoimmune encephalomyelitis by oral administration of myelin basic...
-
Upload
ariel-miller -
Category
Documents
-
view
212 -
download
0
Transcript of Suppression of experimental autoimmune encephalomyelitis by oral administration of myelin basic...
Journal of Neuroimmunology, 46 (1993) 73-82 73 © 1993 Elsevier Science Publishers B.V. All rights reserved 0165-5728/93/$06.00
JNI 02404
Suppression of experimental autoimmune encephalomyelitis by oral administration of myelin basic protein
VI. Suppression of adoptively transferred disease and differential effects of oral vs. intravenous tolerization
Ariel Miller a,1, Z. Jenny Zhang a, Raymond A. Sobel <2, Ahmad AI-Sabbagh a and Howard L. Weiner a
a Center for Neurologic Diseases, Division of Neurology, Department o f Medicine, Brigham and Women's Hospital, Boston, MA, USA, and b Department of Pathology, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA
(Received 20 November 1993) (Revision received 4 March 1993)
(Accepted 8 March 1993)
Key words: Experimental autoimmune encephalomyelitis; Oral tolerance: Myelin basic protein
Summary
Antigen-driven tolerance is an effective method of suppressing cell-mediated immune responses. We have previously shown that oral administration of myelin basic protein (MBP) suppresses experimental autoimmune encephalomyelitis (EAE) when it is actively induced by MBP emulsified in complete Freund's adjuvant. In order to further study antigen-driven tolerance in this model, we investigated the effect of oral tolerization on adoptively transferred EAE and compared oral tolerance to intravenously (i.v.) administered MBP in both actively induced EAE and adoptively transferred EAE. Although orally tolerized animals were not protected from adoptively transferred EAE, spleen cells from orally tolerized animals suppressed adoptively transferred EAE when co-trans- ferred with encephalitogenic cells or when injected into recipient animals at a different site at the time encephalitogenic cells were transferred. This suppression was mediated by CD8 ÷ T cells, correlated with suppres- sion of DTH responses to MBP, and was associated with decreased inflammation in the spinal cord. Unlike oral tolerization, spleen ceils from i.v. tolerized animals did not suppress adoptively transferred EAE when co-trans- ferred with encephalitogenic cells although i.v. tolerized animals were protected from adoptively transferred EAE. MBP peptides were then utilized to further characterize differences between i.v. and oral tolerization in the actively induced disease model. Both orally and intravenously administered MBP suppressed actively induced EAE. However, EAE was only suppressed by prior i.v. tolerization with the encephalitogenic MBP peptide 71-90, but not with the non-encephalitogenic peptide 21-40, whereas prior tolerization with 21-40 did suppress actively induced EAE when administered orally. These results suggest a different mechanism of tolerance is initiated by oral vs. intravenous administered antigen. Specifically, oral tolerization suppresses primarily by the generation of active suppression whereas the dominant mechanism of suppression' associated with i.v. tolerization appears most consistent with the elicitation of clonal anergy.
Correspondence to: H.L. Weiner, Center for Neurologic Diseases, 221 Longwood Avenue, Boston, MA 02115, USA. 1 Present address: Department of Neurology, Carmel Medical Cen-
ter, Haifa, Israel. 2 Present address: Laboratory Service, Palo Alto Veteran's Adminis-
tration Medical Center, Palo Alto, CA 94304, USA.
Introduction
Immunological tolerance is the ability of the im- mune system to discriminate self from non-self and occurs by a variety of mechanisms. Although clonal deletion is a major mechanism for the maintenance of
74
self tolerance (Kappler et al., 1987; Kisielow et al., 1988), clonal deletion does not eliminate all autoreac- tive T cells and autoreactive cells that are not deleted in the thymus may be regulated through clonal anergy (Ramsdell et al., 1989; Schwartz, 1989), or active sup- pression (Gershon and Kondo, 1971; Miller et al., 1991a). Understanding the mechanisms of tolerance is of major interest for the control of autoimmune dis- eases in which there is a breakdown of self-tolerance.
When the immune system is exposed to antigen, tolerance or immunity may result depending on several factors, including the concentration and physical state of the antigen, whether adjuvants are used and the route of administration (Dinitzis and Dinitzis, 1990). We have been studying antigen-driven tolerance by oral administration of antigens, a long-recognized method to induce tolerance (Mowat, 1987). Further- more we have used oral tolerance as a method to down-regulate autoimmune process and we and others have demonstrated that oral administration of au- toantigens is an effective way of suppressing a variety of experimental autoimmune diseases (Bitar and Whitacre, 1988; Higgins and Weiner, 1988; Lider et al., 1989; Nussenblatt et al., 1990; Zhang et al., 1990, 1991; Brod et al., 1991; Miller et al., 1991b, 1992a).
The primary experimental model we have studied is experimental autoimmune encephalomyelitis (EAE) in- duced by active immunization with MBP emulsified in complete Freund's adjuvant (CFA). We have found that oral tolerization to MBP results in active suppres- sion. Specifically, CD8 ÷ T cells are generated follow- ing oral administration of MBP and these cells can adoptively transfer protection (Lider et al., 1989; Miller et al., 1991) and mediate suppression both in vitro and in vivo, by the release of TGF-/3 following triggering by the fed antigen (Miller et al., 1992a). Active suppres- sion that can be adoptively transferred has also been demonstrated following oral tolerization to type II col- lagen in adjuvant arthritis (Zhang et al., 1990) and oral administration of insulin in the NOD mouse (Zhang et al., 1991).
Other investigators have found clonal anergy to be associated with oral tolerance. Whitacre et al. (1991), using a different oral tolerization protocol in their studies of oral tolerance to MBP in the Lewis rat model of EAE, have been unable to transfer suppres- sion from orally tolerized animals, and report that clonal anergy is the predominant mechanism of oral tolerance in their system. Similarly, Friedman and col- leagues have found clonal anergy to be the primary mechanism of oral tolerance in their studies of oral tolerance to ovalbumin (Melamed and Friedman, 1993).
In a current report, we undertook a series of investi- gations to further understand mechanisms associated with oral tolerance and to provide a framework from which to further investigate the contributing roles of
clonal anergy vs. active suppression in this model. Two approaches were taken. First, we studied oral tolerance in adoptively transferred EAE, a form of EAE we have yet to study. Second, we compared intravenous and oral tolerance to both MBP and to MBP peptide fragments in an attempt to dissociate clonal anergy from active suppression.
Understanding mechanisms associated with oral tol- erance has taken on added relevance since oral toler- ance is being used clinically to treat patients with autoimmune diseases such as multiple sclerosis, rheumatoid arthritis and uveitis (Marx, 1991; Weiner et al., 1993).
Materials and Methods
Animals Female Lewis rats 6-8 weeks of age were obtained
from Harlan-Sprague Dawley Inc. (Indianapolis, IN). Animals were housed in Harvard Medical School Ani- mal Care Facilities and maintained on standard labora- tory chow and water ad libitum. Animals were main- tained in accordance with the guidelines for the Com- mittee on Care of Laboratory Animals of the Labora- tory Research Council (Publ. No. DHEW:NIH, 85-23, revised 1985).
Antigens and reagents Guinea pig MBP was purified from brain tissue by
the modified method of Deibler et al. (1972). Protein content and purity were checked by gel electrophoresis and amino acid analysis. Concanavalin A and histone were obtained from Sigma (St. Louis, MO). Peptides were synthesized in the peptide facility of the Center for Neurologic Diseases, Brigham and Women's Hospi- tal, and purified on HPLC. The amino acid sequences of the peptides synthesized encompassed the following regions of guinea pig MBP according to Martenson (1972): 21-40, MDHARHGFLPRHRDTGILDS; 71- 90, SLPQKSQRSQDENPVVHF, residues 78 and 79 are deleted in the guinea pig sequence (Martenson, 1972); 151-170, GTLSKIFKLGGRDSRS, residues 162-165 are deleted in the guinea pig sequence (Mar- tenson, 1972).
Induction of tolerance For oral tolerance, rats were fed 1 mg of MBP
dissolved in 1 ml PBS, or PBS alone, by gastric intuba- tion with a 18-gauge stainless steel animal feeding needle (Thomas Scientific, Swedesboro, N J). Animals were fed five times at intervals of 2-3 days with the last feeding 2 days before immunization. For intra- venous tolerance, rats were injected with 0.1 mg of MBP, MBP peptides, or histone dissolved in 0.1 ml PBS, or PBS alone. Animals were injected via the
ocular vein five times at intervals of 2-3 days with the last injection 2 days before immunization.
Induction of EAE For actively induced disease, Lewis rats were immu-
nized in the left foot pad with 25/zg of MBP in 50/zl of PBS emulsified in an equal volume of complete Freund's adjuvant (CFA) containing 4 mg m1-1 of Mycobacterium tuberculosis (Difco). For adoptively transferred EAE, an MBP-reactive T cell line was established from rats immunized with MBP in CFA, raised and maintained according to the method of Ben-Nun et al. (1982). Encephalitogenic cells were collected after activation by culture with ConA (2 /zg ml-~) for 48 h using irradiated thymocytes as APCs. Cells were harvested from cultures via a Ficoll hypaque gradient (Hypaque 1077, Sigma) and washed twice in PBS prior to transfer. 5 x 106 encephalitogenic cells were injected in the flank in 0.1 ml PBS into irradiated (750 rads, 24 h earlier) recipient rats. Cell viability of both modulator and encephalitogenic cells was deter- mined by trypan blue exclusion and was greater than 90%. In all experiments five animals were used per experimental group.
Adoptive transfer of protection following oral or intra- venous tolerization
Whole spleen populations from MBP-fed, intra- venously (i.v.) injected, or control animals were cul- tured (5 x 10 6 cells in 1 ml of proliferation media), in the presence of ConA (2 /zg ml -~) for 48 h. After ConA stimulation, cells were ficolled, passed over ny- lon wool, and adoptively transferred. In other experi- ments, depletion of lymphocyte subsets was then per- formed by negative selection using magnetic beads according to a modified method of Cruikshank et al. (1987). Spleen cells were incubated with a 1:10 dilu- tion of mouse anti-rat CD8 or CD4 monoclonal anti- body (clones O X / 8 or W3/25, respectively, Serotec/ Bioproducts, Indianapolis, IN) for 30 min on ice, washed twice, and then added to prewashed magnetic particles, with an average diameter of 4.5/xm (M-450) with goat anti-mouse IgG covalently attached (Dynal, Fort Lee, N J). The quantity of magnetic beads used was calculated as being 10 times the estimated target cell population. The cells were incubated with the beads in 0.5 ml of RPMI 1640 medium supplemented with 10% fetal calf serum in a 10-ml round-bottom test tube (Nunc) for 30 min on ice with gentle shaking every 5 min. After incubation, the bead/cel l suspension was washed with 5 ml of medium, and the cell-mAb-bead complexes were separated from unlabeled cells in a strong magnetic field using a magnetic-particle concen- trator (Dynal-MPC-1) for 2 min. The supernatant was removed, and the procedure was repeated twice to obtain the non-adherent fraction. The cells in the
75
CD4 ÷ and CD8 ÷ depleted populations were > 95% CD4+CD8 - or CD4-CD8 ÷, as demonstrated by indi- rect flow cytometry.
Clinical evaluation Animals were evaluated in a blinded fashion every
day for evidence of EAE. Clinical severity of EAE was scored as in our previous studies as follows: 0, no disease; 1, limp tail; 2, hind limb paralysis; 3, hind limb paraplegia, incontinence; 4, tetraplegia; and 5, death. Duration of disease was measured by counting the total number of days from disease onset (usually days 10 or 11 after active immunization and 3-5 days after adoptive transfer of disease) until complete recovery for each animal.
Delayed type hypersensitivity (DTH) testing DTH was tested by injecting 25/xg of MBP in PBS
subcutaneously in the ear. Thickness was measured by a blinded observer, before and 48 h after challenge, using micrometer calipers (Mitutoyo, Japan). The dif- ference of ear thickness before and after challenge was recorded for each animal, and the result was expressed as the mean for each experimental group + SEM.
Histology Histological analysis of pathological changes was
performed in rats with adoptively transferred EAE. Spinal cords were removed on day 15 after adoptive transfer and fixed with 10% neutral buffered formalin. Paraffin sections were prepared and stained with Luxol fast blue-hematoxylin and eosin, by standard proce- dures (Sobel et al., 1984). Spinal cord tissue was sam- pled in an identical manner for each animal and num- bers of inflammatory loci per section (clusters of > 20 or more aggregated inflammatory cells), in parenchyma and meninges were scored in a blinded fashion (Cruikshank et al., 1987).
Statistical analysis Clinical scales were analyzed with a two-tailed
Wilcoxon rank sum test for score samples, chi square analysis was used in comparing the incidence of disease between groups, and comparison of means was per- formed by using Student's t-test. For individual experi- ments, five animals were used per group. Results are expressed as experimental or control __ standard error of the mean.
Results
Suppression of adoptively transferred EAE by oral toler- ization to MBP
To evaluate the effect of prior oral administration of MBP on adoptively transferred EAE, MPB-fed and
76
A
- . - o - - PBS~d
• MBP F~J
5 10 15 20
DAYS AFTER CELL TRANSFER
3 ¸ B
E A N Modula tor cel ls
c L 2 / \ • Coq~ (cv-m~ecled) [
c A L
S C O II E
0 I . . . . . . . . , . . . . , . . . . , 5 10 15 20
DAYS AFTER CELL TRANSFER
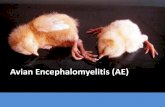
Fig. 1. Suppression of adoptively transferred EAE by oral toleriza- tion to MBP (A) Animals were orally tolerized to MBP and then inoculated in the flank with 5 × 106 MBP-specific, ConA-stimulated, encephalitogenic line cells 2 days after the last feeding (B) 15 x 106 nylon wool passaged spleen cells from animals orally tolerized to MBP were co-transferred with 5 x 106 encephalitogenic cells in the left flank or injected separately in the right and left flanks
respectively.
con t ro l ra ts were i n t r ape r i t onea l l y inocu la t ed with 5 × 106 MBP-spec i f ic , C o n A - s t i m u l a t e d , e n c e p h a l i t o g e n i c l ine cells. MBP- reac t i ve cei ls were t r ans f e r r ed 2 days af te r the last feeding . A s shown in Fig. 1A, ora l admin- i s t ra t ion of M B P had no effect on adop t ive ly t rans- f e r r ed E A E . However , adop t ive ly t r ans f e r r ed E A E was s u p p r e s s e d when sp leen cells f rom oral ly to l e r i zed ani- mals were co - t r ans f e r r ed with the e n c e p h a l i t o g e n i c cells to naive rec ip ien t s (Fig. 1B) ( m e a n maximal score 2.7 + 0.3 vs. 0.8 + 0.2, P < 0.01). F o r co- t ransfer , cells f rom ora l ly to le r i zed an imals were mixed with en- cepha l i t ogen ic ceils and injected. In o r d e r to ru le ou t tha t the in vi t ro mixing of cells a r t e fac tua l ly r e l a t e d to suppress ion , the m o d u l a t o r cei ls and e n c e p h a l i t o g e n i c cells were in jec ted s epa ra t e ly i n t r ape r i t onea l l y t h rough the lef t and r ight f lank so tha t all ce l lu la r in te rac t ions would occur in vivo. As also shown in Fig. 1B, s imi lar p ro t ec t i on was obse rved when e n c e p h a l i t o g e n i c and m o d u l a t o r cells were in jec ted i n t r ape r i t onea l ly sepa- ra te ly in the r ight and left f lanks ( m e a n maximal score 2.7 + 0.3 vs. 0.7 _+ 0.2, P < 0.01).
Suppression of adoptively transferred EAE is dependent on CD8 + T cells from orally tolerized animals
To d e t e r m i n e w h e t h e r suppress ion o f adop t ive ly t r ans f e r r ed E A E was d e p e n d e n t on a specif ic T cell
M E A N
C 2 . M o d u l a t o r cMI~ L
MBPF~J
• CD4 I ~ e ~
- - - - O - - - C '~ D ~ t e d 1
0 . . . . . ) 5 10 15 20
DAYS AFTER CELL TRANSFER
Fig. 2. Suppression of adoptively transferred EAE by co-transfer of CD4 or CD8-depleted T cells from MBP-fed animals. Spleen cells from MBP-fed animals were depleted of CD4 + and CD8 + T cell subsets prior to co-transfer. Adoptive transfer of protection was abrogated by depletion of CD8 +, but not CD4 + T cells (mean
maximal score 2.3 + 0.2 and 0.7 + 0.2, respectively; P < 0.01).
subset , sp l een cells f rom M B P - f e d an imals were de- p l e t e d of CD4 ÷ or CD8 ÷ T cell subsets p r io r to adopt ive t ransfer . As shown in Fig. 2, adop t ive t rans fe r of p ro t ec t i on was a b r o g a t e d by d e p l e t i o n of CD8 +, bu t not CD4 ÷ T cells ( m e a n maximal score 2.3 + 0.2 vs. 0.7 + 0.2 respect ively , P < 0.01).
Delayed type hypersensitivity (DTH) responses associated with adoptively transferred EAE
W e have previous ly found a co r re l a t ion be tween D T H responses and the suppress ion of act ively in- duced E A E fol lowing ora l t o l e r ance (Mil lor e t al., 1991, 1992). To d e t e r m i n e w h e t h e r a ~imilar cor re la - t ion exis ted in adopt ive ly t r ans fe r r ed E A E , D T H re- sponses were measu red . As shown in Fig. 3, p r o m i n e n t D T H responses d e v e l o p e d in animals unde rgo ing E A E
Moc
neg
con
M B P -
C D 4
CD8
f 0 1 2 3
A E A R T H I C K N E S S ( 1 0 .2 inches)
Fig. 3. DTH responses associated with protection by co-transfer of T
cell subsets from MBP-fed animals. DTH responses to MBP were measured 14 days after co-transfer of CD8+-depleted, CD4+-de - pleted or whole spleen cells from MBP-fed animals. Neg. control, naive animals; none, transfer of encephalitogenic cells only; control, co-transfer of cells from unfed animals; MBP-fed, co-transfer of cells from MBP-fed animals; CD4 or CD8-depleted, co-transfer of de-
pleted populations from MBP-fed animals.
and DTH responses were suppressed by the co-transfer of splenocytes from animals orally tolerized to MBP. The suppressed DTH responses were abrogated by depletion of CD8 ÷, but not CD4 ÷ T cells prior to transfer (A ear swelling in CD4 ÷ depleted vs. CD8 ÷ depleted 0.6 + 0.1 vs. 1.8 + 0.2, P < 0.01)
A
77
Effect of co-transfer of cells from MBP orally tolerized animals on CNS histology in adoptively transferred EAE
We have previously found that oral administration of MBP suppresses CNS inflammation in actively in- duced EAE (Higgins and Weiner, 1991). Nevertheless, not all immune specific immunomodulatory treatments
i !! i ii ii~ili! ̧I - B
80-
70-
60"
50"
~ 0"
~ 21)
10
~CONTROL
[ ] MBP-FED
• CD4-DEPLETED
[~CDg-DEPLETED
0 MENINGES PAREN-C HYMA
Fig. 4. Histological analysis of spinal cord in adoptively transferred suppressed by co-transfer of cells from MBP-fed animals (A) Typical meningeal and parenchymal mononudear cell infiltrate in rat with adoptively transferred EAE with co-transfer of spleen cells from non-tolerized animals (B) Absence of inflammation with co-transfer of MBP-fed spleen cells (C) Absence of inflammation with spleen cells from MBP-fed animals depleted of CD4 + cells (D) Typical EAE infiltrate with spleen cells from MBP-fed animals depleted of CD8 + cells (E) Quantitative histological analysis of inflammatory foci. All sections of spinal cord were stained with Luxol fast blue-hematoxilin and eosin. Magnifica-
tion × 200.
78
A Hisl~e I.V.
MBP I.V.
10 12 14 16 18
DAYS AFTER IMMUNIZATION
20
4"
M B ~ Hisl0m I.V. g A ~ MBP I.V. N
3- ) D ~ ----{3-- co-ua~ MBPlme+ C , . L 1 N I 2 - C A L
S 1 C O R E 0 .
0 2 4 6 8 10
DAYS AFTER CI.;LL TRANSFER
F ig . 5. S u p p r e s s i o n o f a c t i v e l y i n d u c e d a n d a d o p t i v e l y t r a n s f e r r e d
EAE associated with i.v. administration of MBP (A) Actively induced EAE. Animals received five intravenous injections of 0.1 mg of MBP or histone at intervals of 2-3 days; animals were injected with MBP/CFA 2 days after the last injection (B) Adoptively transferred EAE. An encephalitogenic MBP line was adoptively transferred into animals tolerized i.v. with MBP (e) or histone (©). Animals receiving i.v. MBP were protected. Co-transfer of MBP-line cells and spleen cells from i.v. tolerized animals with an encephalitogenic MBP line
( [] ); no protection was observed.
of E A E that suppress clinical disease affect CNS in- f lammation (Offner et al., 1991). As shown in Fig. 4, there was decreased inf lammation in both the
parenchyma and meninges when cells from MBP-fed animals were transferred and this suppression was ob- served when CD4+-depleted, but not CD8+-depleted, modulator spleen cells from orally tolerized animals were transferred. Number of CNS (parenchyma + meninges) inflammatory foci for the specific groups were as follows: control, 76 + 8.2; MBP-fed, 3.8 + 1.8; CD4+-depleted, 2 . 8 _ 1.0; CD8+-depleted, 65 + 4 ; ( P < 0.01, MBP-fed and CD4+-depleted vs. control or CD8 +-depleted).
Suppression of actively induced and adoptively trans- ferred EAE following L v. administration of MBP
As shown in Fig. 5A, i.v. injection of MBP markedly suppressed E A E actively induced with M B P / C F A (mean maximal score 0.5 _+ 0.2, vs. control injected histone 3.0 _+ 0.3; P < 0.01), in an analogous manner to suppression by oral tolerization with MBP. In contrast to oral tolerization, however, which did not protect against adoptively transferred E A E (Fig. 1A), i.v. injec- tion of MBP did suppress adoptively transferred EAE (mean maximal score 0.4 _+ 0.2 vs. control 3.2 _+ 0.2; P < 0.01) (Fig. 5B). However, unlike oral tolerization, disease protection could not be adoptively transferred with spleen cells from i.v. tolerized animals when such cells were co-transferred with an MBP encephalito- genic line (mean maximal score 2.8 + 0.2 vs. control, P = N.S.) (Fig. 5B).
Suppression of EAE following oral or L v. administration of MBP peptides
To further investigate the mechanism of oral vs. i.v. tolerance, MBP peptides encompassing both encephal- itogenic and non-encephali togenic regions of MBP were administered both orally and intravenously prior to immunization for actively induced disease. MBP pep- tide 71-90 of guinea pig MBP is encephalitogenic in Lewis rats (Martenson, 1992). As shown in Fig. 6, suppression of EAE via i.v. tolerization only occurred with whole MBP and peptide 71-90, but not with
O R A L I.V. T O L E R I Z A T I O N T O L E R I Z A T I O N
H i s t o
MI
p21-
p71-
p I 3 1 - 1 S Q
0.0 0.5 1.0 1.5 2 .0 2 .5 0.0 0.5 1.0 1.5 2 .0 2.5 M E A N M A X I M A L S C O R E MEAN M A X I M A L S C O R E
F i g . 6. S u p p r e s s i o n o f E A E f o l l o w i n g o r a l o r i.v. a d m i n i s t r a t i o n o f M B P - p e p t i d e s . W h o l e M B P o r M B P p e p t i d e s w e r e f e d o r i n j e c t e d i.v. f ive
t i m e s a t 2 - 3 - d a y i n t e r v a l s a f t e r w h i c h a n i m a l s w e r e i n d u c e d f o r E A E w i t h M B P / C F A .
peptide 21-40. Oral tolerization with 21-40, however, was effective in suppressing EAE. Peptide 21-40 was chosen as experiments demonstrate that it triggers TGF-/3 release from spleen cells of animals orally tolerized to whole MBP (Miller et al., 1992; Miller, in preparation). Control peptide 131-150 did not sup- press when administered either orally or intravenously. Of note is that in addition to suppressing via the i.v. route, 71-90 also suppressed when given orally.
Discussion
In the present study we have found basic differences in the mechanism of antigen-driven tolerance between orally vs. intravenously administered MBP in the Lewis rat model of EAE. The results suggest that orally administered antigen acts predominantly via the gener- ation of active suppression, whereas no active suppres- sion can be demonstrated following intravenously ad- ministered antigen. Even though both i.v. and orally administered MBP suppress actively induced EAE, cells that will adoptively transfer protection can only be recovered from the spleens of orally tolerized animals.
Although prior oral tolerization prevents actively induced EAE (Bitar and Whitacre, 1988; Higgins and Weiner, 1988), in the present study we found that prior oral tolerization does not protect animals from adop- tively transferred EAE. However, adoptively trans- ferred EAE can be suppressed when CD8÷T cells from the spleens of orally tolerized animals are co- transferred with the encephalitogenic line or are in- jected intraperitoneally at the same time separately through a different site. Such co-transfer not only suppresses clinical EAE, but also DTH responses, and inflammation in the central nervous system. The pro- tection of adoptively transferred EAE by co-transfer experiments following oral tolerization are consistent with our previous observations in the NOD-mouse model of diabetes, in which co-transfer of spleen cells from NOD mice fed insulin suppressed adoptively transferred diabetes (Zhang et al., 1991).
Our interpretation of prior oral administration of MBP protecting against actively induced EAE but not adoptively transferred EAE is as follows. We have shown that oral tolerance to MBP is mediated by a CD8 + cell that acts by the secretion of the suppressive cytokine TGF-/3 following triggering by the fed antigen (Miller et al., 1992a). In order for TGF-/3-secreting CD8 ÷ cells generated by oral tolerance to suppress, two conditions must exist: they must encounter antigen and they must be in proximity to CD4 ÷ encephalito- genic cells. Thus, oral tolerization to MBP prior to active immunization suppresses the affector phase of the immune response, presumably by CD8 ÷ cells en-
79
countering antigen in draining lymph nodes and secret- ing TGF-/3 during the time when the immune response is being generated. In adoptively transferred EAE, activated encephalitogenic cells are injected, they mi- grate to the brain where they encounter MBP and invoke an inflammatory response. Prior oral toleriza- tion does not prevent adoptively transferred disease as the adoptively transferred cells migrate rapidly to the brain and initiate the inflammatory response before sufficient numbers of CD8 ÷ cells appear in the brain to downregulate the response. However, if CD8 ÷ cells from orally tolerized animals are transferred into the animal at the same time as the encephalitogenic cells, they migrate to the brain simultaneously, are activated by MBP to release TGF-fl and prevent encephalito- genic cells from initiating the inflammatory response. Thus, the ratio of regulatory to encephalitogenic cells at the target organ and the timing of their entry to the target organ is crucial. Of note is that in our experi- ments both modulator and encephalitogenic cells were intentionally stimulated in vitro with ConA and not MBP prior to co-transfer to prevent antigen carry-over and potential downregulation elicited by introduction of the autoantigen itself together with the transferred cells.
The differential effects of MBP peptides given orally or intravenously further support the postulate that a different mechanism of tolerization occurs depending on the route in which MBP is administered. Our hy- pothesis is that i.v. MBP induces clonal inactivation or anergy whereas orally administered MBP induces ac- tive suppression. The immunodominant and encephali- togenic region of guinea pig MBP in the Lewis rat EAE model is contained in the 71-90 epitope (Martenson, 1992). Peptides 21-40 and 131-150 are not immunodominant or encephalitogenic. Thus, as was found in the present investigation, it would be expected that if the i.v. route induces clonal inactiva- tion or anergy, i.v. administration of only the 71-90 portion of the MBP molecule would suppress EAE. In vitro studies are required to extablish whether clonal anergy as opposed to clonal deletion occurs following i.v. administration of MBP. In terms of the mechanism of oral tolerization with MBP peptides, if a region distinct from 71-90 suppresses EAE following oral administration, the mechanism of action must involve activation of non-encephalitogenic cells. We have pre- viously shown that oral administration of MBP frag- ment 1-37 suppresses EAE in the Lewis rat induced with guinea pig MBP (Higgins and Weiner, 1988) and in the present investigation found similar results using MBP peptide 21-40. Furthermore, we have found orally administered 21-40 and other non-encephalitogenic peptides produce TGF-/3 when stimulated by antigen in vitro (Miller et al., 1992c; manuscript in preparation). Thus, suppression by orally administered 21-40 is con-
80
sistent with our demonstration of transferrable active suppression in this model. Of note is that peptide 71-90 suppressed when given either orally or intra- venously. The degree to which orally administered 71- 90 induces active suppression is currently under inves- tigation.
Using a different feeding protocol, Whitacre et al. (1991) have also reported that orally administered MBP suppresses actively induced EAE in the Lewis rat, but postulate that clonal anergy is the primary mechanism. Their group was unable to adoptively transfer protec- tion from orally tolerized animals to suppress actively induced disease as we have reported (Lider et al., 1989; Miller et al., 1991) and argue that the inability of orally tolerized animals to be protected from adoptively transferred disease further demonstrates clonal anergy to be the primary mechanism of oral tolerance in the Lewis rat EAE model. Given the results of the present investigation, we believe that differences in the method of oral tolerance induction utilized by Whitacre and ourselves most probably account for the differences. Whitacre administers four 5-mg feedings of MBP (20 mg total) in conjunction with a soybean trypsin in- hibitor which prevents degredation of MBP in the stomach. Our protocol involves five 1-mg feedings of MBP in PBS (5 mg total). It is known that small amounts of orally administered antigen pass into the bloodstream through the intestine (Mowat, 1987), and we have found TCA-precipitable MBP in the blood- stream after feeding iodinated MBP (AI-Sabbagh and Weiner, in preparation). Furthermore, investigators have reported that degredation of proteins in the stom- ach may actually be required for the generation of oral tolerance (Michael, 1989), to facilitate antigen process- ing in the gut. Thus, apart from technical differences, we postulate that Whitacre is inducing clonal anergy by orally administering MBP in a manner that delivers unprocessed MBP into the bloodstream and that by- passes the mechanism that leads to active suppression elicited by stimulating gut associated lymphoid tissue. Of note is that in some instances the induction of oral tolerance in autoimmune models is dependent on a relatively narrow therapeutic dose range and oral toler- ance may be lost when too much antigen is fed. This has been shown for feeding collagen type II in arthritis models (Nagler-Anderson et al., 1986; Zhang et al., 1990), insulin in diabetes models (Zhang et al., 1991), and we have observed this effect in some of our experi- ments involving the chronic relapsing EAE model (Brod et al., 1991). Thus, taken together, our experiments and those of Whitacre suggest that varying degrees of both clonal anergy and active suppression may occur following oral administration of MBP in the Lewis rat EAE model depending on the conditions under which the MBP is administered and how the antigen encoun- ters the gut-associated lymphoid tissue.
An important potential role of suppressor T cells in the downregulation of EAE has been suggested by other investigators. In previous studies Swanborg and colleagues reported the generation of suppressor cells by pretreatment of animals with MBP in IFA (Swier- kosz et al., 1977). Consistent with our results, he was also able to suppress actively induced EAE by intra- venously administered MBP, but could not demon- strate suppressor cells in animals tolerized by the i.v. route. Swanborg has also reported CD4 ÷ post-recovery suppressor cells in the Lewis rat EAE model that also appear to act via the secretion of downregulatory cy- tokines such as TGF-fl and IL-4 (Karpus et al., 1991). The precise mechanism by which i.v. administered MBP tolerizes is not known, but may relate to antigen pre- sentation in the absence of the appropriate co-stimula- tory factors or the preferential inhibition of Thl vs. Th2 cells (Burstein and Abbas, 1993).
Two major distinguishing features of oral vs. i.v. tolerance in the present study include the generation of cells that actively mediate suppression and induction of tolerance by different epitopes of MBP. In addition, we have recently shown that oral tolerance to MBP is associated with the expression of inhibitory cytokines such as TGF-/3 and IL-4 in the target organ (Khoury et al., 1992). This appears to be further evidence for the generation of active suppression following oral toler- ance using our protocol for oral tolerization as it would not be expected that anergy would be associated with an increase of suppressive cytokines in the target or- gan. In this regard, we have previously shown that oral administration of alloreactive cells suppresses acceler- ated allograft rejection (Sayegh et al., 1992) and more recently that oral alloantigen is associated with the expression of IL-4 within graft tissue whereas no IL-4 is present when i.v. alloantigen is administered (Han- cock et al., 1992).
The present findings may have important implica- tions for designing immunotherapy for human autoim- mune diseases based on antigen-driven tolerance. Im- munotherapeutic strategies based on mechanisms of anergy are restricted to autoimmune diseases in which the inducing autoantigens and immunodominant epi- topes are well-characterized. In chronic EAE the role of different CNS autoantigens in the elicitation of the primary autoimmune process or triggering secondary T cell reactivity differs at various stages of the disease (Perry and Barzaga, 1987; McCarron et al., 1990) and spreading of T cell autoimmunity to cryptic determi- nants of an autoantigen has been described (Lehmann et al., 1992). Oral tolerization that resulted in the generation of active suppression would appear to obvi- ate this problem as regulatory ceils generated by the oral administration of an antigen from the target organ would migrate to target tissue, be triggered by the fed tissue antigen to release suppressive cytokines in the
local microenvironment at the target tissue and down- regulate inflammation irrespective of the specificity of the disease-producing cells. In this regard, we have recently demonstrated suppression of PLP-induced re- lapsing EAE in SJL mice by oral administration of MBP (A1-Sabbagh et al., 1992).
Acknowledgements
This work was supported by NIH grants N529352 (H.L.W.) and NS26773 (R.A.S.) and by a grant from AutoImmune, Inc. A.M. is the recipient of a Public Health Service Fogarty International Research Fellow- ship (1F05TW04418, 1CP). In accordance with disclo- sure guidelines of the Harvard Medical School, H.L.W. holds a financial interest in AutoImmune Inc. We thank Byron Waksman for helpful scientific discussions and Amy Hostetter for support in manuscript prepara- tion.
References
A1-Sabbagh, A., Miller, A., Sobel, R.A. and Weiner, H.L. (1992) Suppression of PLP induced EAE in SJL mice by oral adminis- tration of MBP. Neurology 42 (Suppl. 3), 346.
Ben-Nun, A., Wekerle, H. and Cohen, I.R. (1982) The rapid isola- tion of clonable antigen-specific T lymphocyte lines capable of mediating autoimmune encephalomyelitis. Eur. J. Immunol. 11, 195.
Bitar, D. and Whitacre, C.C. (1988) Suppression of experimental autoimmune encephalomyelitis by the oral administration of myelin basic protein. Cell. Immunol. 112, 364-370.
Brod, S.A., AI-Sabbagh, A., Sobel, R.A., Hailer, D.A. and Weiner, H.L. (1991) Suppression of chronic relapsing experimental au- toimmune encephalomyelitis by oral administration of myelin antigens. Ann. Neurol. 29, 615-622.
Burstein, H.J. and Abbas, A.K. (1993) In vivo role of interleukin 4 in T cell tolerance induced by agneous protein antigen. J. Exp. Med. 177, 475-463.
Cruikshank, W.W., Berman, J.S., Theodore, A.C., Bernardo, J. and Center, D.M. (1987) Lymphokine activation of T4 + T lympho- cytes and monocytes. J. Immunol. 138, 3817.
Deibler, G.E., Martenson, R.E. and Kies, M.W. (1972) Large scale preparation of myelin basic protein from central nervous tissue of several mammalian species. Prep. Biochem. 2, 139-164.
Dintzis, H.M. and Dintzis, R.S. (1990) Antigens as immunoregula- tors. Immunol. Rev. 115, 243-250.
Gershon, R.K. and Kondo, K. (1971) Infectious immunological toler- ance. Immunology 21,903-914.
Hancock, W.W., Sayegh, M.H., Kwok, C.A., Weiner, H.L. and Car- penter, C.B. (1992) Oral but not intravenous alloantigen prevents accelerated allograft rejection by selective intragraft TH2 cell activation. Transplantation 55, 1112-1118.
Higgins, P.J. and Weiner, H.L. (1988) Suppression of experimental allergic encephalomyelitis by oral administration of myelin basic protein and its fragments. J. Immunol. 140, 440-445.
Kappler, J.W., Roehm, N. and Marrack, P. (1987) T-cell tolerance by clonal elimination in the thymus. Cell 49, 273-280.
Karpus, W.J. and Swanborg, R.H. (1991) CD4 + suppressor cells inhibit the function of effector cells of experimental autoimmune
81
encephalomyelitis through a mechanism involving transforming growth factor-beta. J. Immunol. 146, 1163-1168.
Khoury, S.J., Hancock, W.W. and Weiner, H.L. (1992) Oral toler- ance to myelin basic protein and natural recovery from experi- mental autoimmune encephalomyelitis are associated with down- regulation of inflammatory cytokines and differential upregula- tion of TGF-/3, IL-4, and PGE expression in the brain. J. Exp. Med. 147, 1355-1362.
Kisielow, P., Bluthman, H., Staerz, U.D., Steinmetz, M. and von Boehmer, H. (1988) Tolerance in T-cell-receptor transgenic mice involves deletion of nonmature CD4+8 ÷ thymocytes. Nature 333, 742-746.
Lider, O., Santos, L.M.B., Lee, C.S.Y., Higgins, P.J. and Weiner, H.L. (1989) Suppression of experimental autoimmune en- cephalomyelitis by oral administration of myelin basic protein. II. Suppression of disease and in vitro immune responses is medi- ated by antigen-specific CD8 + T lymphocytes. J. Immunol. 142, 748-752.
Martenson, R.E. (1992) Myelin: Biology and Chemistry. CRC Press, Boca Raton, FL, p. 785.
Marx, J. (1991) Testing of autoimmune therapy begins. Science 252, 27-28.
Mattingly, J.A. and Waksman, B.H. (1978) Immunologic suppression after oral administration of antigen. I. Specific suppressor cells formed in rat Peyer's patches after oral administration of sheep erytrocytes and their systemic migration. J. Immunol. 121, 1878- 1883.
McCarron, R.M., Fallis, R.J. and McFarlin, D.E. (1990) Alterations in T cell antigen specificity and class II restriction during the course of chronic relapsing experimental allergic encephalomyeli- tis. J. Neuroimmunol. 29, 73-79.
Melamed, D. and Friedman, A. (1993) Direct evidence for anergy in T lymphocytes tolerized by oral administration of ovalbumin. Eur. J. Immunol. 23, 935-940.
Michael, J. (1989) The role of digestive enzymes in orally induced immune tolerance. Immunol. Invest. 18, 1049-1054.
Miller, S.D. and Hanson, D.G. (1979) Inhibition of specific immune response by feeding protein antigens. IV. Evidence for tolerance and specific active suppression of cell mediated immune response to ovalbumin. J. Immunol. 123, 2344-2350.
Miller, A., Hailer, D.A. and Weiner, H.L. (1991a) Tolerance and suppressor mechanisms in experimental autoimmune en- cephalomyelitis: Implications for immunotherapy of human au- toimmune diseases. FASEB J. 5, 2560-2566.
Miller, A., Lider, O. and Weiner, H.L. (1991b) Antigen driven bystander suppression following oral administration of antigens. J. Exp. Med. 174, 791-798.
Miller, A., Lider, O., Roberts, A.B., Sporn, M.B. and Weiner, H.L. (1992a) Suppressor T cells generated by oral tolerization to myelin basic protein suppress both in vitro and in vivo immune responses by the release of TGF-/3 following antigen specific triggering. Proc. Natl. Acad. Sci. USA 89, 421-425.
Miller, A., Lider, O., AI-Sabbagh, A. and Weiner, H.L. (1992b) Suppression of experimental autoimmune encephalomyelitis by oral administration of myelin basic protein. V. Hierarchy of suppression elicitated by myelin basic protein from different species. J. Neuroimmunol. 39, 243-250.
Miller, A., Prabhu Das, M. and Weiner, H.L. (1992c) Epitopes of myelin basic protein (MBP) that trigger TGF-/3 release following oral tolerization to MBP are different from the encephalitogenic epitopes. FASEB J. 6, 1686.
Mowat, A. (1987) The regulation of immune responses to dietary protein antigens. Immunol. Today 8, 193.
Nagler-Anderson, C., Bober, L.A., Robinson, M.E., Siskind, G.W. and Thorbecke, G.L. (1986) Suppression of type II collagen-in- duced arthritis by intragastric administration of soluble type II collagen. Proc. Natl. Acad. Sci. USA 83, 7443-7446.
82
Nussenhlatt, R.B., Caspi, R.R., Mahdi, R., Chan, C.-C., Roberge, F., Lider, O. and Weiner, H.L. (1990) Inhibition of S-antigen in- duced experimental autoimmune uveoretinitis by oral induction of tolerance with S-antigen. J. Immunol. 144, 1689-1695.
Offner, H., Hashim, G.A. and Vandenbark, A.A. (1991) T cell receptor peptide therapy triggers autoregulation of experimental encephalomyelitis. Science 251,430-432.
Perry, L.L. and Barzaga, M.E. (1987) Kinetics and specificity of T and B cell responses in relapsing experimental autoimmune en- cephalomyelitis. J. Imunol. 138, 1434-1441.
Ramsdell, F., Lantz, T. and Fowlkes, B.J. (1989) A nondeletional mechanism of thymic self tolerance. Science 246, 1038-1041.
Sayegh, M.H., Zhang, Z.J., Hancock, W.W., Kwok, C.A., Carpenter, C.B. and Weiner, H.L. (1992) Down-regulation of the immune response to histocompatibility antigens and prevention of sensiti- zation by skin allografts by orally admnistered alloantigen. Trans- plantation 53, 163-166.
Schwartz, R.H. (1989) Acquisition of immunologic self-tolerance. Cell 57, 1073-1081.
Sobel, R.A., Blanchette, B.W., Bhan, A.K. and Colvin, R.B. (1984)
The immunopathology of experimental allergic encephalomyeli- tis. I. Quanitative analysis of inflammatory cells in situ. J. Im- munol. 132, 2393-2401.
Swierkosz, J.E. and Swanborg, R.H. (1977) Immunoregulation of experimental autoimmune encephalomyelitis: conditions for in- duction of suppressor cells and analysis of mechanisms. J. Im- munol. 119, 1501-1506.
Weiner, H.L., Mackin, G.A., Matsui, M., Orav, E.J., Khoury, S.J., Dawson, D.M. and Hailer, D.A. (1993) Double-blind pilot trial of oral tolerization with myelin antigens in multiple sclerosis. Sci- ence 259, 1321-1324.
Whitacre, C.C., Gienapp, I.E., Orosz, C.G. and Bitar, D. (1991) Oral tolerance in experimental autoimmune encephalomyelitis. III. Evidence for clonal anergy. J. Immunol. 147, 2155-2163.
Zhang, Z.J., Lee, C.S.Y., Lider, O. and Weiner, H.L. (1990) Suppres- sion of adjuvant arthritis in Lewis rats by oral administration of type II collagen. J. Immunol. 145, 2489-2493.
Zhang, Z.J., Davidson, L., Eisenbarth, G. and Weiner, H.L. (1991) Suppression of diabetes in NOD mice by oral administration of porcine insulin. Proc. Natl. Acad. Sci. USA 88, 10252-10256.