Summer 2015, Vol 14 Ed 32 (PDF)
Transcript of Summer 2015, Vol 14 Ed 32 (PDF)

www.usafp.org 1
Journal of The Uniformed Services Academy of Family Physicians
Summer 2015 • Vol. 8 • Num. 4 • Ed. 32
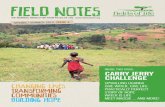
Mark Your Calendars to Attend the 2016 USAFP Annual Meeting & Exposition
HealtH is Primary18-22 MArCh 2016Sheraton Denver Downtown hotelDenver, Colorado
Thank you to Terry Schulte for over 20 years of service to Uniformed Family Physicians. See page 5.

The Uniformed Family Physician • Summer 20152
CHS and Community Health Systems are tradenames/trademarks of Community Health Systems Professional Services Corporation, which provides management services to affiliates of Community Health Systems, Inc.
Wherever you see yourself and your new practice, chances are a CHS-affiliated hospital is nearby. And if you choose to practice with one,chances are you’ll be glad you did. Approximately 22,000 physicians –employed and independent – serve on the medical staffs of nearly 200 CHS-affiliated hospitals in 29 states. e hospitals deliver a wide range of health services and function as vitally important members of their local communities.
In 2014, e Joint Commission recognized 107 CHS-affiliated hospitals as Top Performers on Key Quality Measures.® And, an array of national qualityrecognitions and honors for affiliated hospitals includes accredited chest paincenters, accredited stroke centers, and Centers of Excellence for bariatric services.
While we’re literally “all over the map,” we’re focused on helping you find aplace to build a successful practice. Affiliated hospitals have the flexibility tomeet individual needs and the ability to offer competitive recruitmentpackages and start-up incentives, which may include medical education debtassistance and even residencystipends. Hundreds of physicians choose CHS-affiliated hospitals eachyear – for quality of care and quality of life. One may be right for you!
For more information, visit: www.chsmedcareers.com.Email: [email protected] Call: 800-367-6813
Doctor Recommended.In 29 states and nearly 200 hospitals.

www.usafp.org 3
The Uniformed ServicesAcademy of Family Physicians
1503 Santa Rosa RoadSuite 207
Richmond, Virginia 23229804-968-4436
FAX 804-968-4418www.usafp.org
VISION
The USAFP will be the premier professional home that provides services to enhance the experience of current and future Uniformed Family Physicians.
MISSION
The mission of the USAFP is to support and develop Uniformed Family Physicians as we advance health through education, scholarship, readiness, advocacy, and leadership.
USAFP e-mailMary Lindsay White: [email protected]
Newsletter EditorJames Ellzy, MD: [email protected]
This newsletter is published by the Uniformed Services Academy of Family Physicians. The opinions
expressed are those of the individual contributors and do not reflect the
views of the Department of Defense or Public health Service.
4
56
6
academy leaders
resolution of aPPreciation
consultant rePort:army
8consultant rePort:air force
editor’s Voice
10
5President’s message
consultant rePort:naVy
122016 annual meeting PreView
13 teacHing and learning
22 committee rePorts: resident and student
Created by Publishing Concepts, Inc.David Brown, President • [email protected]
For Advertising info contact Michele Forinash • 1-800-561-4686
pcipublishing.com
Edition 32
16committee rePorts:clinical informatics
18 committee rePorts: Practice management
20committee rePorts:HealtH Promotion and
disease PreVention
24committee rePorts:member and
membersHiP serVices
25 leadersHiP book series
29welcome new members
32 members in tHe news
34member benefits

The Uniformed Family Physician • Summer 20154
your academy leaders
OFFicErSPresidentRobert C. Oh, MD, MPHOffice of the surgeon GeneralFalls Church, [email protected]
President-eleCtChristopher Paulson, MDeglin AFB, [email protected]
ViCe PresidentJames Ellzy, MDBUMed, Washington, [email protected]
seCretAry/treAsUrerKimberly Roman, MDUs Coast GuardWashington, [email protected]
PAst PresidentMark J. Flynn, MD, FAAFPCamp Pendleton, [email protected]
exeCUtiVe direCtOrMary Lindsay Whiterichmond, [email protected]
DirEcTOrSAir FOrCeChristopher Jonas, DOthe White House, Washington, [email protected]
Jessica Servey, [email protected]
Kirsten Vitrikas, MDtravis AFB, [email protected]
ArMyKevin Kelly, MD, MBAFt. Hood, [email protected]
Laurel Neff, DOMadigan Army Medical Center, [email protected]
Mark E. Stackle, MD, MBAFt. Bragg, [email protected]
nAVy John Laird, MDCamp lejeune, [email protected]
Michelle Lynch, MDCamp lejeune, [email protected]
Brian Smoley, MD, MPHCamp Pendleton, [email protected]
PUBliC HeAltH serViCeEdgardo Alicea, MDUsCG savannah, [email protected]
Maria DeArman, MDUsCG Corpus Christi, [email protected]
residentsJason Butler, DOFt. Bragg, [email protected]
Jed Siebel, DOnaval Hospital Jacksonville, [email protected]
Breanna Gawrys, DOFt. Belvoir, [email protected]
AAFP deleGAtesPamela M. Williams, MDnellis AFB, [email protected]
Mark B. Stephens, MDUsUHsBethesda, [email protected]
AlternAtes Robert C. Oh, MD, MPHOffice of the surgeon GeneralFalls Church, [email protected]
James Ellzy, MDBUMed, Washington, [email protected]
cONSUlTANTSAir FOrCeMarcus Alexander, MDAFMOA, san Antonio, [email protected]
ArMyShawn Kane, MDFt. Bragg, [email protected]
nAVyTimothy Mott, MDnaval Hospital Pensacola, [email protected]
cOmmiTTEE chAirSCliniCAl inFOrMAtiCs Matt Barnes, MDFt. Belvoir, [email protected]
CliniCAl inVestiGAtiOns Anthony Beutler, MDUsUHs, Bethesda, [email protected]
COnstitUtiOn And BylAWs James W. Keck, MDnaval Hospital Jacksonville, [email protected]
edUCAtiOn Douglas Maurer, DOMadigan AMC, [email protected]
HeAltH PrOMOtiOn And diseAse PreVentiOn Debra Manning, MD, MPHnaval Hospital Pensacola, [email protected]
MeMBer COnstitUenCiesLuis Otero, MDCharleston AFB, [email protected]
Yolanda Backus, MDJBer, [email protected]
MeMBersHiP And MeMBer serViCesAdam Saperstein, [email protected]
neWsletter editOrJames Ellzy, MD BUMed, Washington, [email protected]
nOMinAtinG Mark J. Flynn, MD, FAAFPCamp Pendleton, [email protected]
Robert C. Oh, MD, MPHOffice of the surgeon GeneralFalls Church, [email protected]
Christopher Paulson, MDeglin AFB, [email protected]
OPerAtiOnAl MediCine Jason Ferguson, DOtripler AMC, [email protected]
Barrett Campbell, MDFort irwin, [email protected]
PrACtiCe MAnAGeMentElizabeth Duque, MDFt. Hood, [email protected]
2015 PrOGrAM CO-CHAirsMichael Mercado, MDCamp Pendleton, [email protected]
Janet West, MDnaval Hospital Jacksonville, [email protected]
2016 PrOGrAM CO-CHAirsEdward Y. Kwon, MDFt. Belvoir, [email protected]
Shane Larson, MDFt. Belvoir, [email protected]
resident And stUdent AFFAirs Aaron Saguil, MD, MPHUsUHs, [email protected]
OFFiCers And COMMittees

www.usafp.org 5
Wow, what a busy quarter for USAFP! First, I want to sadly announce, after over 37 years of service to Family Medicine, our beloved Executive Director, Terry Schulte has retired as of July 1, 2015. We are planning some national recognition for Terry to celebrate his service to USAFP to
include a resolution to the AAFP Congress of Delegates. In conjunction with the Vir-ginia Academy of Family Physicians, the USAFP submitted a resolution of Appre-ciation for Terrence J. Schulte. (see below)
Secondly, I am very pleased to announce that our Board of Directors unanimously voted Mary Lindsay White as our new Executive Director. Please give your warm congratulations to ML! She’s already done a fantastic job during the transition, and I have complete confidence in her!
Finally, even during the midst of this transition, the team has been busy secur-ing the location for our next Annual Meeting, Denver, Colorado! Colorado is one of the healthiest states in our nation,
and it is with this backdrop that we will be having our “health is Primary” Annual Meeting & Exposition. If you have never been to Colorado, you’ll be impressed with its beauty and vibrancy.
I hope you have been looking for small ways that you can improve your health. In this edition, I also have written an article on nutrition. So, maybe you can squeeze in one more vegetable a day. Or maybe you can decrease your daily intake of sugar. For me, I’ve been on a FitBit group challenge in my office, and it has been increasing the number of steps I get every day at work. And, you don’t even need a FitBit, you just need the app and you too can join the FitBit group! I’d love to hear your stories!
Robert C. Oh, MD, MPHUSAFP PresidentOffice of the Surgeon GeneralFalls Church, [email protected]
president’s messagerOBert C. OH, Md, MPH
Whereas, Mr. Terry Schulte served on the staff of the Ameri-can Academy of Family Physicians for 11 years including service as Vice-President, and
Whereas, Mr. Terry Schulte has ably and honorably served as the Executive Vice President of the Virginia Academy of Family Physicians for 26 years, and
Whereas, Mr. Terry Schulte ably and honorably served as the Executive Vice President of the Uniformed Services Acad-emy of Family Physicians for 20 years, and
Whereas, Mr. Terry Schulte has served with distinction on a number of American Academy of Family Physicians com-mittees over the years and helped assure their work was rel-evant to and supportive of practicing family physicians, and
Whereas, Mr. Terry Schulte’s exemplary leadership skills and experience greatly served all three organizations in advanc-ing the best in Family Medicine and excellent patient care over the years, and
Whereas, Mr. Terry Schulte mentored many state chapter executives over the years, and
Whereas, Mr. Terry Schulte mentored many state chapter family physicians over the years, supporting them in their advancement to major leadership positions in state and national office, and
Whereas, Mr. Terry Schulte has always placed the needs of our organization and our mission as his first priority, and
Whereas, his father was a family physician and his heart and energy have always been focused on helping Family Medi-cine over the years, therefore, be it,
Resolved, that the American Academy of Family Physicians, the Virginia Academy of Family Physicians and the Uni-formed Services Academy of Family Physicians acknowl-edge Mr. Terry Schulte’s outstanding service and dedication to family medicine and extend our gratitude for his 37 years of service in advancing family medicine.
resolution of AppreciationTerrence J. Schulte
Submitted by Virginia Academy of Family Physicians and Uniformed Services Academy of Family Physicians

The Uniformed Family Physician • Summer 20156
editor’s voiceJAMes ellzy, Md
This newsletter is lighter on committee updates, but full of pearls for leadership and manage-ment (who knew there was a big difference…Dr. Duque explains more). Check out the President’s message for updates on next year’s USAFP Meeting.
And in case you haven’t heard, the DoD has announced the new Ehr…Cerner. Check out the press release at http://www.defense.gov/News-Article-View/Article/612714/dod-awards-contract-for-elec-tronic-health-records.
Enjoy your last days of summer and enjoy this quarter’s newsletter.
James Ellzy, MDWashington, [email protected]
consultant reportArMy
hello and happy Summer. PCS sea-son should be coming to an end, and I hope those that moved are getting settled in and the moves were uneventful and smooth. Congrats to all of our recent resi-dency and fellowship graduates.
I missed the last newsletter and wanted to take this time to thank COL Mark reeves for his years of work as our con-sultant. It only took me a few weeks in the seat to realize how much Mark did for us while representing our specialty.
It’s amazing what Family Physicians do everyday both in garrison and while deployed. This fact is not lost upon our leadership, and right now we are working with our AMEDD leadership to quantify the wartime critical skills needed for Family Physicians. This is a challenge as we serve in such a variety of positions – from battalion surgeons at remote FOBs to Ers and the wards of Combat Support and Theater hospitals. I will be reaching out to some of you to help fill in the gaps and to provide your experiences and insight.
Congratulations to those recently selected for promotion to LTC!! Promo-
tions and selections are going to continue to get more competitive as the size of our Army continues to drop. You can never go wrong with making sure the basics (pro-fessional military education, board certi-fication, APFT, OrB and doing a great job) are taken care of. It will take us a while to figure out the nuances of the new OEr. For those out there that are raters and senior raters pay attention to your profiles; if you don’t have a large denomi-
nator of officers you can quickly use up your “top blocks.”
Early in the fall I will contact the Fam-ily Medicine leadership across our MTFs to get an initial idea of who is staying and going at each facility. This list will be very fluid based on GME selections, 60A assignments and many other factors.
Please feel free to contact me via email or phone. Let me know if there is any-thing I can help with.
Shawn Kane [email protected]
It’s amazing what Family Physicians do everyday both in garrison and while deployed. This fact is not lost upon our leadership, and right now we are working with our AMEDD leadership to quantify the wartime critical skills needed for Family Physicians. This is a challenge as we serve in such a variety of positions – from battalion surgeons at remote FOBs to ERs and the wards of Combat Support and Theater hospitals. I will be reaching out to some of you to help fill in the gaps and to provide your experiences and insight.

www.usafp.org 7www.usafp.org 9
Clinical PharmacologyFellowship Program
Clinical PharmacologyFellowshipWhat is Clinical Pharmacology?Clinical Pharmacology is concerned with
better the understanding and use of existing
drugs, and development of more effective
and safer drugs for the future. Clinical
Pharmacology allows one to stand between
the research lab and the bedside, in a unique
position to translate laboratory research
Into new drug therapies. Clinical
pharmacologists are a bridge between the
science and practice of medicine.
Who can apply for the Fellowship?The Clinical Pharmacology training program
is available to active duty Army physicians
���������������������������������������� ����
specialty and active duty Army PhDs/
PharmDs (71A, 71B, or 67E) who have a
doctoral degree in one of the life or medical
sciences from an accredited academic
institution in the United States, Canada,
or non-U.S. degree equivalent. A research
background, mathematical inclination,
and pharmacology/medical experience is
preferred. Civilians could be considered
if they joined the Army and successfully
compete for a position in the program.
Additional activities include:�� ��������������������� ����
or clinical research under the
supervision of a mentor
�� ����������������������������
of Clinical Pharmacology to
medical students, house staff,
and practicing physicians
�� ������ ���������������������
review division at the FDA
�� �������������������������
medical education, research
seminars, and journal clubs
Potential Job Assignments�� �����
(Silver Spring, MD)
�� ���
(Bethesda, MD)
�� �������������
(Thailand, Kenya)
�� �������
(Ft. Detrick, MD)
�� ��������
(Ft. Detrick, MD)
�� �������
(Aberdeen Proving Ground, MD)
�������������� ������������ ���������
http://wrair-www.army.mil
Contact: LTC Kevin Leary, MD,
Uniformed Services University
http://ushus.mil
Contact: Louis Cantilena, MD, PhD

The Uniformed Family Physician • Summer 20158
consultant reportAir FOrCe
hello everyone. I know the summers are often strained with inbound and out-bound team members, but I hope you have been able to find a way to enjoy some time and recharge your batteries. It has been an exciting first year as your Family Medicine consultant. I am happy to report that we have made significant progress on many of the critical topics to FPs in the AFMS, and that we can be very optimistic for continued support and improvement.
The AFMS has adopted Trusted Care as its platform to be a high reliability organization with core tenants of leader-ship commitment, patient safety culture, and continuous process improvement. These tenants mirror how we as FPs have been approaching delivering qual-ity patient care. The executive leadership courses for PCMh are well underway and should help bolster MTF leadership understanding and support of PCMh concepts. Family Physicians continue to be key contributing leadership members in many forms: medical directors, flight commanders, squadron commanders, SGhs, program directors, group com-manders, and currently even Surgeon General. It is vital that we continue to seek out these roles. I strongly encour-age you to complete requirements for all potential positions that you may not iden-tify a desire to compete for until later in your career (keep all your options open). A few common requirements are: excel-ling clinically, leading when the opportu-nity arises, completing rank appropriate PME, and applying for special experience identifiers when you qualify.
The PCMh roll out continues to be at the heart of day to day activities for primary care. Primary care is hard work! This is reflected in low provider satisfac-tion surveys for the AFMS and even lower
provider satisfaction surveys amongst our peers in civilian practice. As a medical stu-dent, I watched those like Brian reamy, Kathy holder, and Pam Williams person-ally connect with a patient and make a difference in their life, reach a struggling student or resident and make a difference in their life, step up as a guiding leader for the clinic, MTF, or even nationally and make a difference for medicine, and last but not least provide servant leader-ship for their communities and families in order to be a difference maker. There was never a doubt that it was a lot of hard work for them to be successful, but the poten-tial to make a difference as they had was well worth it. Each and every one of you makes a difference for someone every day.
With that said, the goal is to work smarter instead of harder when we can. This requires evaluation of our processes and incorporating our success stories into our standardization. Many locations are succeeding in using lean manage-ment rounds as a method to identify and improve their processes with the support and incite of their leadership. The perfor-mance for improvement data is also being used AFMS wide to help identify success stories and possible areas of improve-ment in the way we operate. I will remain actively engaged with data regarding PCMh and hEDIS metrics and I will make every effort to assist in processes
that improve our quality in these areas. In addition to optimizing our pro-
cesses, we have made significant strides in available manpower to complete the PCMh mission. Out of our 303 active duty clinical family physician authoriza-tions, we filled 288 with active duty FPs and the remaining 15 with GS or con-tract 44Fs. Thus, the new PCMh model accurately reflects the FPs we have avail-able in our clinical positions. however, it is recognized that a manpower gap still exists when simultaneously performing our in garrison PCMh mission and our readiness mission. Additionally, provid-ers may be unavailable for medical con-ditions or administrative actions. While we continuously assess our retention and recruitment, we will have to evalu-ate alternative ways to mitigate this gap between requirements and available man-power. I intend to explore the possibility of strategic placement of POM contract positions at our continuous deployer MTFs in order to program for the known recurrent gaps instead of relying on short term contracting in the form of OCO and gapfill contracts. Solidifying the 44F manpower and embracing our col-laborative consultative relationship with our PAs and NPs places us in a strong position to provide outstanding care. We have some of the highest quality of pro-viders in the US and should support all of
Antoine (Marcus) Alexander, [email protected]
Family Physicians continue to be key contributing leadership members in many forms: medical directors, flight commanders, squadron commanders, SGHs, program directors, group commanders, and currently even Surgeon General. It is vital that we continue to seek out these roles.

www.usafp.org 9
our team members practicing at the full scope of their abilities.
Clinical currency has also been a focus of the AFMS as a foundation for our readi-ness. Updates to the SMArT curriculum have been submitted over the last 6 months that will potentially assist MTFs in filling in currency gaps once they are identified locally. Family Medicine currency gaps may exist if there are restrictions in the demographics and acuity of our enroll-ment, and if we do not continue to manage complex patients in environments similar to those in our readiness missions. I con-tinue to emphasize the need to include all ages in our enrollment and recurrent opportunities to manage complex patients in diverse settings such as inpatient wards and emergency rooms whenever possible.
Our Medical Corps Director and Dep-uty Director (Col hootsmans and LtCol Sherman) have proactively inquired about
the needs of our physicians, and made incredibly valuable resources easily avail-able at the Medical Corps website on the KX. The link to the Career Develop-ment page is https://kx2.afms.mil/kj/kx5/AFMedicalCorps/Pages/Career-Develop-ment-and-Mentoring.aspx
There are helpful resources regarding career tracks, promotions, PME, finan-cial benefits, special jobs, OPr writing, and much more. I highly recommend at least visiting to familiarize yourself with what is available.
My last reminder is that it is great to have a retirement plan that accounts for inflation and active duty pay raises for the rest of your life. The above breakdown for a Colonel retiring with 20 years of service in 2015 is a nice bonus on top of the amaz-ing people we have the privilege to care for and work with on a daily basis.
Thank you again for being the bed-rock of the AFMS. Please always feel free to reach out to me if I can help in any way. I can be reached at [email protected].
The Department of Family Medicine at NorthShore University HealthSystem, (NorthShore) the principal academic affiliate of the University of Chicago Pritzker School of Medicine, is currently seeking exceptional Family Medicine physicians for practice opportunities in several locations. Responsibilities include managing the care of patients of all ages in the office and using a strong hospitalist program for inpatient care. The Department has many distinguished faculty and attending physicians and continues to grow every year. This is an excellent opportunity to provide quality patient care in a lucrative practice within a highly successful organization. We offer a competitive salary and comprehensive benefits package.
The successful candidate for this position will have completed a family medicine residency and be board certified or board eligible by the American Board of Family Medicine. Academic appointment to the University of Chicago Pritzker School of Medicine is available to qualified candidates.
NorthShore is a member of the Mayo Clinic Care Network; Mayo’s only collaboration of its kind in the Chicago region. Located in Chicago’s Northern suburbs, NorthShore is a
Family Medicine Physician
Qualified candidates should submit their CV to:
Kathleen Gliva, Physician RecruiterEmail: [email protected]: (847) 663-8250
EOE: Race/Color/Religion/Sex/National Origin/Protected Veteran/Disability, VEVRRA Federal Contractor
Chicago’s Northern Suburbs
physician-led, multi-specialty group with 900 plus physicians and growing. You’ll benefit from being part of a fully integrated healthcare organization spanning 4 hospitals, along with more than 100 Medical Group offices. NorthShore has been named one of the “Most Wired” healthcare organizations in the country by Hospitals & Health Networks Magazine, and our EMR system, EPIC, is the “gold standard” in the industry.
Before Taxes After Taxes
Years Retired Year Monthly Pay Annual Pay Cumulative Annual Pay Cumulative
1 2015 $4,172 $50,070 $50,070 $36,050 $36,050 10 2024 $4,987 $59,838 $548,253 $43,084 $394,742 20 2034 $6,079 $72,943 $1,216,569 $52,519 $875,930 30 2044 $7,410 $88,917 $2,031,244 $64,020 $1,462,495 40 2054 $9,032 $108,389 $3,024,327 $78,040 $2,177,516

The Uniformed Family Physician • Summer 201510
consultant reportnAVy
transitionsSummer is a time of multiple transi-
tions and I want to point out a few which have already occurred, and then I’ll point out some others in the fall newsletter.
Family Medicine Graduates: Congrat-ulations to our newest board-certified FPs! We continue to perform well above the national average on first-time board pass rates out of our Belvoir, Bremerton, Jacksonville, LeJeune, Pendleton, and Pensacola residency programs. BZ!
New Detailer: CDr Samya Cruz has taken over from CDr rowena Papson. rowena did an astounding job as our Detailer—exquisitely balancing needs of the Navy and desires of our community members. Dare I say, this may be one of the hardest jobs out there, and she performed commendably! CDr Cruz will continue having the same FP Detailer phone num-ber, and her e-mail is [email protected].
New Program Director: CDr Tony Silvetti has taken over the helm of the FP/OB Fellowship from CDr Ingrid Sheldon. Ingrid launched and grew our FP/OB Fellowship at Nh Camp LeJeuene making it a top-notch train-ing option. her efforts have also stan-dardized expectations for OB refresher Training such that FPs continue to have full-scope opportunities and impact across the enterprise.
PromotionsSelection for CDr and CAPT is
becoming increasingly competitive. For FPs looking at selection for CAPT, 44% of those In-Zone were selected (that is 5% greater than the rest of the Medi-cal Corps). For those above zone, FPs selected at twice the rate as the rest of the Medical Corps, although that still equated to a quite low 14%.
Quite simply, your best chance to promote is when you are “in-zone.” So, attempt to plan your career well in advance. Positioning yourself for pro-motion hinges upon sustained supe-rior performance, breaking out on fit-ness reports from your peer group, and showing diversity in leadership roles and duty stations. Operational billets offer exceptional personal and profes-sional fulfillment, but the timing of when to take these roles is key as they typically have little (if any) peer group from which to break out. Therefore, “one-of-one” jobs are best targeted for the early years of a new rank. MTFs and other billets with large peer groups are great opportunities for leadership and proving your superior performance. Such billets with larger peer groups are ideal places to be for the 2-3 years head-ing into zone for promotion.
Please rest assured, there is not one formula for success to promotion, but the aforementioned guidance offers a broad, proven approach. For more mentorship and guidance in regard to promotion, please contact CDr Samya Cruz and/or me. We can review your record and help you plan your future.
gme selection ProcessThe 2015 BUMEDNOTE 1524 has
been published. It can be viewed on Mil-Suite or online. Unfortunately, the only fellowship opportunities available this
year will be for Sports Medicine, Geri-atrics and Informatics (there is a “zero goal” for both Faculty Development and FP/OB due to a relative surplus of fel-lows with that training). The application season opened on 15 July and will close on 15 September.
communicationUse of MilSuite is growing and the
Navy Family Medicine site now has over 150 followers. I am growing as well in how I can best use MilSuite to facilitate secure communication and dialogue with you, the rest of our community. Please, if you haven’t done so yet, sign up this week from a CAC-enabled computer and help build our community presence. Also, if you are not getting my “list-serve” e-mails or have any other questions, please con-tact me at [email protected].
…and one last transitionCAPT Jay Dudley, Family Physician,
Flight Surgeon, mentor, and friend to so many passed away on Sunday, July 12th at the age of 55. Jay profoundly influ-enced countless lives, primarily through his jobs as the Family Medicine Detailer and his various leadership roles at the Naval Aerospace Medical Institute. For those interested, and in lieu of flowers, Jay’s wife Selma requests that dona-tions in Jay’s name be made to the M.D. Anderson Cancer Center in houston, Texas. rest in peace, Shipmate!
Tim Mott, MDNaval Hospital Pensacola, FL
Positioning yourself for promotion hinges upon sustained superior performance, breaking out on fitness reports from your peer group, and showing diversity in leadership roles and duty stations.

www.usafp.org 11
Transitioning Military andFederal Healthcare Providers
• Relocatetothebeautifulmountainresort communityofPinetop,Arizona,locatedwithin thelargestcontiguousponderosapineforestinthe
worldwithover180milesofdevelopedhiking,mountainbiking,andcross-countryskiingtrailsthroughoutthecommunity
• Opportunitytopracticefull-spectrummedicineifdesired,toincludeER,urgentcare,low-riskOB,inpatientandoutpatientmedicine
• Alpineskiingandsnowboardingonly36milesaway;three18-holecoursesinPinetopandanadditionalfourcourseswithin20milesinnearbyShowLow,AZ
• Wonderfulfourseasonclimatewithsunshinemorethat70%ofthetimeyear-round
• OpeningsincludebothfederalcivilservantpositionsaswellaspositionsforuniformedofficersofthePublicHealthServiceCorps
• Militaryphysicians,FNPsandPA’shavetheopportunitytotransferservicesandretainactive
dutybenefits,toinclude20yearretirement,TSP, loanrepayment,Tricare,accesstomilitarybase
lodging,recreationalfacilitiesandspace-Aflights; forcompensationquestions:http://www.usphs.gov/profession/physician/compensation.aspx
CONTACT:Dr Patrick Lynch
(928) 205-2301

The Uniformed Family Physician • Summer 201512
Mark your calendars to attend the best CME meeting in the country. 2016 Program Chairs, Eddie Kwon, MD and Shane Larson, MD are planning for an outstanding event. The promotional brochure and pre-liminary program will be e-mailed to all members in October 2015. If you have questions regarding the meeting, please e-mail [email protected] or contact the USAFP headquarters Office at 804-968-4436.
don’t miss tHe 2016 usafP annual meeting & exPosition!!18-22 marcH 2016 – denVer, colorado
2016 annual meeting
The University of Tennessee Department of Family Medicine invites applications from highly qualified and experienced family physicians to fill two key leadership roles at our UT-Saint Francis Residency Program. We are seeking two eager, enthusiastic individuals to serve as the PreDoctoral Director for medical students at the University of Tennessee College of Medicine and a Medical Director for the newly established Physician Assistant program in the College of Allied Health Professions.
The PreDoc director will be responsible for all four years of medical student training in family medicine. The Director role involves developing goals and objectives, curriculum, evaluation systems, faculty development, scholarly engagement in the critical appraisal of the literature, directing the medical student lecture series and working closely with the Family Medicine Interest Group. The individual will work closely with our residency programs in Jackson, Knoxville and Chattanooga to ensure standardized training and evaluation for each student.
The Medical Director of the Physician Assistant program will work closely with the PA leadership team and faculty to provide oversight of the PA program. Curriculum development, evaluation and feedback, faculty development and providing lectures are the major responsibilities.
In addition to the specific leadership responsibility, the successful candidates will have the wonderful opportunity to work with a dynamic faculty, practice the full-spectrum of family medicine that includes obstetrics in a very supportive academic and practice environment; and help train a great group of medical students, residents and fellows. Qualified applicants should hold the MD/DO degree, be board certified, and have proven experience as a physician, leader and clinician educator. Obstetrics and research are negotiable. Academic rank and salary are commensurate with qualifications and experience.
Interested applicants should submit a cover letter and CV to
Dr. David L. Maness, Professor and Chair UT Department of Family Medicine 1301 Primacy Parkway, Memphis, TN 38119The University of Tennessee is an EEO/AA/Title VI/Title IX/ Section 504/ ADA/ ADEA institution in the provision of its education and employment programs and service.

www.usafp.org 13
Dr. Louis Pangaro’s rIME system (reporter, Interpreter, Manager, Educa-tor) has been embraced as an easy way to understand where a medical learner is in their learning process. What if I told you that there is a similarly simple way for leaders to approach management of any task? I recently read Ken Blanchard’s Leadership and the One Minute Man-ager, and was impressed by the simplicity of his approach to managing personnel. Two factors are required to determine which management style to use – the employee’s level of competence and their commitment. Once determined, the leader chooses one of four distinct styles to best meet the employee’s needs.
“That’s all well and good for people sitting in cubicles, but how does it apply to me in the clinic, on the ward, or running a department?” you may ask. What really excited me about Blanchard’s model, is that it is universally applicable. Since it is task based, I don’t have to be someone’s rater to employ it, and it allows me to change my style with the same individual for different tasks. I suspect that we all have role models who have done exactly that. Let me break it down for you.
The first step is to determine the indi-vidual’s level of competence for a particu-lar task or goal. Think rIME, if it helps. Then, Blanchard adds a second factor – commitment. This is how excited ver-sus disgruntled the individual is. he then divides learners into four developmental categories (D1-D4), based on the above; D1 is low competence and high com-mitment (think interns in July or newly hired staff), D2 is low to some compe-tence and low commitment (think interns
in December or staff who have not been given supportive leadership for some time), D3 is moderate to high competence and variable commitment, and D4 is high competence and high commitment.
Blanchard then matches the appro-priate leadership style to each of these developmental levels. The leadership styles are also based on two factors: directing and supporting. he calls the first style S1 or Directing. It provides a significant amount of structure, teaching and supervising and pairs very well with a D1 learner.
The second style is S2 or Coaching. This style is ideal for D2 learners who are feeling less committed and need to be reengaged. It involves teaching or direct-ing (recall the low to some competence associated with this developmental level), but also checking in with the learner for their feedback. By obtaining their per-spective and guiding their success, learn-ers can be reengaged and move forward in their development.
D3 pairs best with a Supportive (S3) style of leadership, because the skill set is there, but the commitment is variable, so praising, listening and facilitating help to improve the commitment to match the learner’s competence. There is still a time
commitment here, but it is spent more in reviewing results and getting input from the individual. These are the perfect folks to use the One Minute Management strategy of “catching people doing the right thing” and reinforcing it.
Finally, a Delegating style (S4) is rec-ommended for those who already have high competence and high commitment (D4). There is little that needs to be done for these self-starters, except to make sure the goal is clear. Blanchard recommends turning over the day-to-day decision-making to these learners.
however, it is important to know that a learner’s development can show some variability depending on the task at hand. This happens quite frequently in military medicine as we move from one location to another, picking up new titles and roles along the way. Someone who is a very com-petent physician may not (yet) be a com-petent OIC, and an eager D1 can quickly become a disgruntled D2 if not given the right tools to succeed. recognizing in yourself what areas you are strong in and which you need more direction in may help you to seek more assistance from your boss or other designee and avoid becoming disillusioned with a new job.
teaching and learning Dawn Sloan, MDFaculty Development FellowMadigan Army Medical Center, [email protected]
One Minute LeadershipLeadership Style to use with: Developmental LevelS1 – Directing (organize, teach, supervise)
D1 – Low competence, High commitment
S2 – Coaching (direct and support)
D2 – Little to low competence,Low commitment
S3 – Supporting (praise, listen, facilitate)
D3 – Moderate to high competence,Variable commitment
S4 – Delegating (turn over daily responsibility)
D4 – High competence,High commitment
continued on page 14

The Uniformed Family Physician • Summer 201514
The flip side of this model is that we each have the opportunity to help develop those around us. A new nurse hired into the PCMh model, will need additional guid-ance and time investment. how-ever, as that D1 receives the appro-priate direction and becomes a D3 and D4, your time investment will pay off with dividends.
Evaluating those you supervise or work with on a task-oriented developmental spectrum will help identify the best strategies to help them succeed. The danger in not taking the time to evalu-ate both competence and com-mitment is that one may select the wrong management style and create disgruntled employees or quagmires of inadequate work that ref lect poorly on the orga-nization. The good news is, once the right developmental stage has been established for a task, goals can be set and others can be enlisted to assist with the actual training – as long as they under-stand the expectations.
As more millennials enter the workforce, positive reinforcement and “catching people doing some-thing right” is becoming even more important, so embracing the direction versus support paradigm for leadership is a simple, straight-forward and easily implemented approach that can be added to any model already in place. Know-ing when to direct, coach, sup-port or delegate is an extremely effective tool as an Army leader. Blanchard’s model allows us to practice a simple approach with each individual we lead.
rEFErENCES: 1Blanchard, K, Zigarmi, P., Zigarmi,
D. (1985). Leadership and the One Minute Manager. New York: William Morrow and Co.
for advertising informationcontact
Michele Forinash at800.561.4686 ext.112
www.usafp.org 1
Journal of The Uniformed Services Academy of Family Physicians
Spring 2015 • Vol. 8 • Num. 3 • Ed. 31
Robert C. Oh, MD, MPHInstalled as 2015-2016
USAFP PresidentDr. Oh is pictured with AAFP Past President
Warren Jones, MD(see page 8)
Mayo Clinic Health System is a family of clinics, hospitals, and other health care facilities serving over 70 communities in Minnesota, Iowa, and Wisconsin. Sharing Mayo Clinic’s primary value of “the needs of the patient come first,” Mayo Clinic Health System links the expertise of Mayo Clinic in practice, education, and research with the health-delivery systems of our local communities. Today, more than 1000 physicians practice in the health system. Mayo Clinic offers a highly competitive compensation package, which includes exceptional ben-efits, and has been recognized by FORTUNE magazine as one of the “100 Best Companies to Work for.” We are seeking BC/BE Family Medicine physicians for our Northwest WI region.
Barron, WI (51512BR); Chetek, WI (39187BR); & Rice Lake, WI (19287BR):• Clinic/Hospital position at 25
bed Critical Access Hospital• General call of 1:8. If interested
in OB, OB call of 1:5• Location qualifies for J1 waiver
Eau Claire, WI (44474BR):• Clinic only position• Phone call of 1:26 and
participate in Urgent Care rotation
• Established Hospitalist program
Menomonie, WI (49397BR):• Clinic/hospital position at Critical
Access Hospital• Call of 1:10
Bloomer, WI (18449BR):• Clinic/Hospital position at 25 bed
Critical Access Hospital• General call 1:7• Established daytime Hospitalist
program
Eau Claire, WI (37576BR):• Urgent Care position• 8 hour shifts with an average of 36
hours/week• Full back up from all subspecialties
Mayo Foundation is an affirmative action and equal opportunity employer and educator.
Our current opportunities include:
If you wish to learn more or to express interest in this position, please contactKarly Wallace at 800-573-2580, email [email protected], or apply at http://www.mayoclinic.org/jobs/physicians-scientists
and search for the position number.

www.usafp.org 15

The Uniformed Family Physician • Summer 201516
committee reportsCliniCAl inFOrMAtiCs
Matthew Barnes, MDClinical Informatics
If you’ve followed any practice man-agement in the past 2 years, then you’ve no doubt heard ominous rumblings of the oncoming storm/apocalypse, the devourer of clinics, the provider-stomp-ing behemoth -- the threatening, the infamous: ICD-10. The rumors are true: this hungry beast is salivating and is wait-ing on the edge of the AhLTA dimen-sion. On October 1st (a day to live in infamy), a portal will open and this beast will pounce -- and will devour interns, chomp up residents, and turn staff into cowering puddles of goo!
Is there hope? how will we avoid the wrath of this monster? Thankfully, we’ve had some luck studying the creature and can prepare. If we can handle the FM boards, then I think we can handle this kraken of coding.
Let’s begin by comparing the current and future state of AhLTA’s AP module.
The interface is exactly the same -- it’s the AhLTA that everyone knows. ICD10 has been available in AhLTA for the past 6-ish months. All we have to do is flip the switch.
So wait. Where’s the fury? Where’s the wrath?
It’s there... the devil is always in the details. This will first impact those with “favorite diagnoses lists” – which is going to require that your ICD9 favorites are
equivalent to ICD10 codes. The good news is that many of those favorites in ICD9 are already “mapped” to a compa-rable ICD10 equivalent, so most of the work is already done.
If you update the problem list, you’ll also notice that this too will need updat-ing from ICD9 to ICD10. Again, the diagnoses will be mapped to their equiva-lents, but you’ll have to make sure each one is appropriate, one by one.
ICD10: Will it hurt?
Currently, we look at this: On ICD10 roll-out, we look at this:
It is important to state that you don’t necessarily have to fight this monster to the death. Absolutely nobody expects flawless coding. The resounding theme I’ve heard for the past year is one we can all agree on: doctors are not coders. Of course, doing better coding benefits you and the clinic, but it’s not the end-all.

www.usafp.org 17
hang on, what about that “Knee Pain NOS” diagnosis, we’ve used on that one patient for 10 years? Why doesn’t it match?
Well, ICD10 is much more specific when compared to ICD9 -- especially for musculoskeletal medicine. To begin, you’ll need to specify right or left side. (Oh, the horror!) Then, you need to specify acute versus chronic conditions. Finally, you’ll need to specify the exact cause of injury (is that an ankle injury of the calcaneal tendon, ATFL or NOS?).
Now this is the true face of the beast! Up to Three Extra Clicks for certain encounters! Flail in fear of the oncom-ing doom-monster! Coding Chthulu demands respect!
Thankfully, the AP module of AhLTA is loaded on your PC, so you won’t be working with too much lag on those boxes, but understandably this is going to make us docs annoyed.
But... is there a softer side? Is there any time when ICD10 might actually... *gasp* help?
There is, though it’s difficult to say if it outweighs the extra clicks.
In my opinion, one of the worst parts of coding is when you’re stuck in coding purgatory -- i.e. “I can’t find the right code for a skin exam.” If I triaged an OB patient at the labor deck, I’d probably just put it under supervision of normal preg-nancy, regardless of what was done on the visit. Now, there’s literally four times as many codes for obstetrics, so you won’t be looking for how to code that visit -- you’ll have more choices, so you can choose one that actually makes sense.
It is important to state that you don’t necessarily have to fight this monster to the death. Absolutely nobody expects flawless coding. The resounding theme I’ve heard for the past year is one we can all agree on: doctors are not coders. Of course, doing better coding benefits you and the clinic, but it’s not the end-all.
There are also numerous resources that can help fight the beast. If you have coding questions, 3M training is avail-able. The AF bought licenses to an app
for Precyse University, which has robust coding support (the other Services may have something similar). Tri-Service Workflow (TSWF) is making videos on coding that will be hosted on their web-site (www.tswf-mhs.com) and will be inte-grating some ICD10 coding support in their forms. Finally, you have two great human resources: clinical system trainers and the coders themselves. reach out to them before ICD10 happens! They can save you some major headaches on Oct 1!
So go ahead, train up, and slay that nightmare beast!
Now, on a serious note, everyone real-izes that ICD10 is going to be annoying -- that’s why it kept getting delayed! But ICD10 is inevitable, and other than get-ting a new Ehr (thanks to Dr. Ellzy and the knights of the Functional Advisory Council – they are the clinical champi-ons for the new Ehr!), we’re doing all we can with the system we have. have any questions? Any ideas? Any com-ments? E-mail me at [email protected] or [email protected].
On ICD10 roll-out, we look at this: Promoting Research in the Military Environment
Visit us online at www.usafp.org/research.htm for resources or to find a mentor.
Have a great idea for operational research but are unsure where to start or how to get approval?
Whether you are deployed or in
garrison, the USAFP research judges
can help!

The Uniformed Family Physician • Summer 201518
committee reportsPrACtiCe MAnAGeMent
Elizabeth Duque, MDFort Bliss, TX
I am sitting here on vacation recover-ing from this year’s provider evaluation season, and it has me thinking about the management skills that were required this time around. At the Army’s recent Primary Care Leaders’ Summit, Mr. Jody rog-ers stated in his leadership talk that “we are a system that is overly managed and under led.” This is not a new concept and military medicine is not alone with this problem. John Kotter, in his 2001 article “What Leaders really Do,” expressed that same sentiment about businesses in gen-eral. This has occurred despite our focus on leadership skills in military education and almost complete lack of management courses. We talk about leadership but we fall into the trap of management, espe-cially in medicine. Is there a balance or is one better than the other?
Kotter argues we need both leader-ship and management to be successful. I have seen this in the young leaders I have working with me. They have some great leadership qualities but struggle daily with the management aspects of their roles. We have all experienced the combination of good leaders and horrible managers or good mangers and horrible leaders. Neither of these combinations will lead to lasting success in our cur-rent military health system. how do we develop and grow both the managerial and leadership skills?
Management is focused on the orga-nization and daily running of the busi-ness. It is about “coping with complexity” by instilling procedures and practices in order to bring some sense of order and consistency to daily activities. Manage-ment looks at and develops data, metrics, individual objectives and long term plan-ning goals. We need managers if we are to
survive in the corporate or bureaucratic culture we work in. Even organizations that use a “self-management” model will state that managerial skills are essential in their employees. Currently most people in our system learn these skills on-the-job. Physician managers rely on their organiza-tional administrators to provide them with the subject matter expertise, but they still require a fundamental understanding of management. There are a few courses that leaders can attend to help them learn and understand their managerial roles better. The Army has a middle-manager course that is usually run locally and the Basic health Care Administrators course that it puts on in San Antonio. The other ser-vices have similar courses; ask your opera-tions or administrative sections about them. The practice management commit-tee runs a workshop at USAFP yearly and the AFP has its Family Practice Manage-ment journal. Although most physicians would rather spend their time and effort taking care of patients, I have found that it is essential to have the clinical voice in the room of data managers or we find our-selves on the end of decisions that make no clinical sense. Additionally, any active duty person working within the military medical system for more than a few years
will require some basic managerial skills. Fortunately, managerial skills are able to be developed. These skills focus on setting objectives or targets, planning specific courses of action to achieve those targets, and ensuring that employees are meeting and upholding those targets. Essential managerial skills include communication of objectives to individuals, knowing how to measure those objectives and evaluating people on the set of objectives. Managers need to know the system in which they work to navigate personnel actions, bud-get information and conflict management. Managers also work to recognize those employees that perform well and address issues with those that don’t.
Leadership, on the other hand, does not focus on daily task oriented goals, but is the ability to influence others to believe in a goal or vision. Leadership creates a desire within people to achieve those goals. It is motivating and inspiring. Leadership sets the direction and aligns the people to the shared vision. Accord-ing to Kotter, leadership is about “coping with change.” These skills can be innate characteristics of a person or be devel-oped. rather than teaching tasks, like managerial skills, leadership skills are more substantial. They involve commu-
Given the increasingly volatile and insecure system in which we work, it is essential that medical leaders have both the skills of a manager and a leader. When these skills co-exist staff are able to be aligned to your organization’s goals and they have a senses of ownership, loyalty and dedication to the success of the organization.

www.usafp.org 19
nication skills, relationship building and strategic thinking. Leadership requires the ability to motivate people to follow a shared goal. The relationship skills and communication skills are essential as one can only motivate, inspire and align peo-ple with a vision by being able to credibly describe that vision. You build credibility by building a relationship of trustwor-thiness, integrity and consistency. This comes from building relationships with employees, other departments and super-visors. Leadership is taught by challeng-ing junior leaders while giving them the opportunity and support to succeed or fail safely. Mentorship and coaching play a large role in leaders’ development. Many military schools focus on leadership devel-opment and it is where most military lead-ers get their formal leadership education. Civilian leader development may not be as structured as military leader development
but follow similar patterns and there are formal schools available to them as well.
Given the increasingly volatile and insecure system in which we work, it is essential that medical leaders have both the skills of a manager and a leader. When these skills co-exist staff are able to be aligned to your organization’s goals and they have a senses of ownership, loyalty and dedication to the success of the orga-nization. If all our employees had these values, our jobs as managers and leaders would be simple. Additionally, when staff are aligned to the organization’s vision and values, they are more resilient and flexible to handle the constantly changing envi-ronment. Strong managerial skills give staff a sense of predictability and security. They are not surprised by evaluations, they feel a sense of worth to the organization and they know what they are accountable for. An example of leadership and manage-
ment co-existing is the recognition of high performances. The leader ensures the per-son is recognized in the proper forum and that the person knows how and where they succeeded, motivating others to follow that person’s example. The manager makes sure the evaluations reflect the performance and the paperwork is done so that the per-son received appropriate compensation for their performance. So, as much as I dislike managerial tasks at times, there is value that is brought by doing these well. We as leaders need to ensure that your younger leaders are able to develop both leadership and management skills.
rEFErENCES: 1hamel, G. (2011, December). First, Let’s
Fire All the Managers. Harvard Business Review. retrieved June 2015, from https://hbr.org/2011/12/first-ets-fire-all-the-managers
Kotter, J. P. (2001, December). What Leaders really Do. Harvard Business Review. retrieved June 2015, from http://hbr.org
Faculty Position Available with academic rank commensurate with experience for full-time faculty member interest in ambulatory medicine. Qualified applicants should hold the MD degree or equivalent, be board eligible in internal medicine. Responsibilities include but are not limited to clinical and administrative responsibilities attending/teaching service. Responsibilities in the areas of research and clinical practice will be addressed in the interview process. Applicants for an Assistant Professor position must show exceptional promise in research and teaching, whereas applicants for the Associate and Full Professor ranks must have demonstrated excellence in research and teaching appropriate to the rank.
The Department of Internal Medicine is one of nine accredited programs sponsored by the University of Tennessee College of Medicine Chattanooga and our affiliated hospital Erlanger Health System. Internal Medicine is approved for 30 residents and co-sponsors a Transitional Year with 6 residents.
This is a great opportunity for dynamic candidate. Strong faculty and great residents in a Program with full accreditation. The University of Tennessee is an EEO/AA/Title VI/Title IX/Section 504/ADA/ADEA Employer
Send CV to: Louis Lambiase, M.D., Professor and Interim Chair Dept. of Internal Medicine, UT College of Medicine975 East Third St. Box 94, Chattanooga, TN 37403
UNIVERSITY OF TENNESSEECOLLEGE OF MEDICNE CHATTANOOGA
DEPARTMENT OF INTERNAL MEDICINEAmbulatory Care
PHYSICIANS NEEDED FARNORTHERN CALIFORNIA(HUMBOLDT-DEL NORTE)
www.hdncms.orgSevere need for Primary
Care (Family Medicine/Internal Medicine/Pediatrics) in
beautiful Humboldt-Del Norte counties. MedicalStudent Loan Repayment options due to our federal designations as health
manpower shortage areas (for primary care and mental
health). Please visit the Humboldt-Del Norte County Medical Society’s website
under “Physician Recruitment”

The Uniformed Family Physician • Summer 201520
committee reportsHeAltH PrOMOtiOn And diseAse PreVentiOn
Robert C. Oh, MD, MPHOffice of the Surgeon General
Falls Church, [email protected]
Greetings. I hope your summer is going well and you are surviving the PCS season and are enjoying the weather and kids out of school. Whether you are eating while writing AhLTA notes, at a theme park with the kids, or enjoying a leisurely meal at home, eating is both a necessity and a guilty pleasure of life. Unfortunately, education about nutrition is one of those areas that most physicians need more to effectively discuss with our patients—especially in the current times of increasing obesity rates and nutrition related diseases. In this column, I’d like to focus on nutrition. Every 5 years since 1980, nutrition experts, as part of the Dietary Guidelines Advisory Commit-tee (DGAC), come together to develop the Dietary Guidelines for America.1 Once the DGAC submits its report, two government agencies—the United States Department of Agriculture (USDA) and the Department of health and human Services (DhhS) come together to jointly write the guidelines. Previously, concepts like the Four Food Groups, the Dietary Pyramid, the MyPyramid and the current MyPlate have been produced by the guidelines. So what will the new guidelines be? Until the official release later this year, we can’t be sure. With that being said, I’m going to give my spin on how I think the new 2015 Dietary Guide-lines for America could look like, and how Uniformed Family Physicians can be more informed when it eventually is published later this year. There are two new articles that were published, and if nothing else everyone should read these two articles. The first comes from the Academy of Nutrition and Dietetics and
comments on the DGAC report.2 The second was an editorial printed in the July 15, JAMA entitled: “The 2015 US Dietary Guidelines: Lifting the ban on total dietary fat.”3 So, here’s where I think we are going with the new Guidelines.
1. you can HaVe your yolk and eat it too.
Cholesterol. Oops. Looks like a 180 degree turn on this one folks. If you keep up with nutrition, you know that eating cholesterol doesn’t raise serum cholesterol. Therefore, the DGAC recommended that cholesterol be removed as a “nutrient of concern.” “healthy” breakfast choices often substitute egg whites with regular eggs (and they have the gall to charge more too?) I have always been puzzled about the “egg white” healthy breakfast. The way I see things…the more you take out of nature, something goes awry.
2. don’t fear tHe fat! or, saturated fat—ain’t all tHat
This may be earthshattering news to us. Did you know that the recent evidence on saturated fat has found no associations with cardiovascular disease? Two recent meta-analyses, including a large one in 2014, demonstrated a lack of association of saturated fat with CV disease.4,5 Now, this probably isn’t the time to make an excuse to load up on bacon, as there continues to be debate on the saturated fat link to CV dis-ease. however, more consistent evidence shows that polyunsaturated fats have been consistently linked with reductions of CV disease. The Academy of Nutrition and Dietetics comments to the 2015 DGAC state: “Therefore it appears that the evi-
dence summarized by the DGAC suggests that the most effective recommendation for the reduction in cardiovascular dis-ease would be a reduction in carbohydrate intake with replacement by polyunsatu-rated fat (PUFA).” Also the editorial in JAMA encourages the USDA and DhhS to lift the bans on dietary fat. remember, we know that there are essential fats nec-essary for growth and development, espe-cially the nervous system. Therefore, let’s at least all agree to eat more of the good fats—the olive oil, avocado’s, the poly-unsaturated fats (omega-3s > omega-6s) found in fatty fish, nuts and seeds.
3. aVoid tHe wHite menace.Displacement of saturated fat may have
done the complete opposite of what the experts expected. Since the 1980 Dietary Guidelines were published, Obesity and Diabetes skyrocketed. Displacement of fat may have inadvertently increased carbohydrate intake in the diet. And..it wasn’t whole grains Americans ate. It was refined carbohydrates—white sugar, white pasta, white bread, white rice, white potatoes. Like the Academy of Nutrition and Dietetics recommended, avoiding the refined carbohydrates and replacing with more PUFAs may really make the differ-ence in CV health for the country.
4. eat more Plants.Interestingly, the DGAC commented
on considering a plant-based diet for envi-ronmental sustainability. Now, I think there are great benefits for plant-based diets, but I don’t think it’s for everyone. Especially our meat loving Americans! however, we can ALL eat more plants.
Nutrition – What Should All Americans Eat?

www.usafp.org 21
Despite all the research demon-strating the benefits of vegetables and fruits in cardiovascular disease, blood pressure and cancer, we don’t eat enough plants. Not surprisingly, only about 1 in 10 Americans eat the recommended 2-3 servings of veg-etables and 1.5-2 servings of fruits daily.6 Why is it so hard to eat veg-etables and fruits? Try to add one more serving of fruit and one more serving of vegetables each day, and eat it first before diving into any-thing else.
So, I tried to highlight what the new 2015 Dietary Guidelines for Americans could look like. But, until the guidelines are released, well, we’ll just have to wait. Until then, maybe now I can have my new “healthy breakfast” of 2 scrambled eggs and wild Alaskan Salmon on a healthy bed of kale sautéed in garlic and olive oil. But please..hold the enriched wheat toast and orange juice. Just coffee, black, for me.
rEFErENCES: 1Dietary Guidelines. Office of Disease
Prevention and health Promotion. Accessed online on July 19, 2015 at: http://www.health.gov/dietaryguidelines/
2Academy Comments re The DGAC Scientific report, May 15, 2015. Accessed online July 19, 2015 at http://www.eatrightpro.org/resource/advocacy/take-action/regulatory-comments/dgac-scientific-report
3Mozaffarian D, Ludwig DS. The 2015 US Dietary Guidelines: Lifting the ban on total dietary fat. JAMA 2015; 313:2421-2422.
4Siri-Tarino PW, Sun Q, hu FB, Krauss rM. Meta-Analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr 2010; 91:535-46.
5Chowdhury r, Warnakula S, Kunutsor S et al. Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med. 2014; 160(6):398-406.
6Moore LV, Thompson FE. Adults Meeting Fruits and Vegetable Intake recommendations – United States, ≠2013. MMWr 2015; 64: 709-13.
University of Colorado Anschutz Medical Campus
School of Medicine Department of Family Medicine
University of Colorado Family Medicine Clinic at Park Meadows
Senior Instructor – Physician, University Family Physicians at Park Meadows
Position #7840 – Job Posting #F02246
The Department of Family Medicine at the University of Colorado Denver Anschutz Medical Campus is seeking a full-time family physician for our South Metro-Area clinic site at Lone Tree/Park Meadows. The Department’s clinical faculty members are recognized for providing innovative, integrated, patient-centered care. The Park Meadows clinic is a busy, ambulatory clinic serving a mix of patients from the surrounding community and is part of the University Hospital system. The Park Meadows clinic is certified as Patient Centered Medical Home and is undergoing practice re-design towards exemplary patient-centeredness and a superior patient experience. Applicants must demonstrate experience and competence patient care and an interest in teaching. This position is full-time and applicants for full-time positions will have priority. Women and minorities encouraged to apply. Detailed job descriptions and qualifications required can be found on jobsatcu.com and the Department’s website, http://fammed.ucdenver.edu/home/careers.aspx.
Job ReSPonSIbIlItIeS: Applicant will be a member of the practice clinical faculty: Sees patients and manages patients within context of a Patient Centered Medical Home practice, serving as a continuity provider for a panel of patients. Teaches students in the provision of patient care, participates in scholarly activity, serves as a leader and role model for fellow physicians and learners.
ReqUIReD qUalIFICatIonS: MD/ DO degree, Colorado Medical License, DEA Certificate, Board Certified/Board eligible in Family Medicine. Practices full spectrum of ambulatory Family Medicine. Must obtain Medical Staff privileges at University of Colorado Hospital.
eSSentIal Job FUnCtIonS: 100% - Provides high quality patient care at University Family Medicine Clinic at Park Meadows
• ProvidesambulatorycareatUniversityFamilyMedicineClinicatParkMeadowsaminimum of 32 hours of appointments per week.
• Exemplifiesthehigheststandardsinpatientcareasafacultymember• Participatesinhomecallapproximatelyfiveweeksperyear.• Participatesinqualityimprovementefforts• Participatesineducationofinterdisciplinarystudentsassignedtotheclinic.
PReFeRReD qUalIFICatIonS: Two years of practice experience in ambulatory and Patient Centered Medical Home/Integrated Practice settings preferred. Individuals with other clinical or practice experience will be considered.
Salary is commensurate with skills and experience. The University of Colorado offers a full benefits package. Information on University benefits programs, including eligibility, is located at http://www.cu.edu/pbs/ Applications are accepted electronically at www.jobsatcu.com. Review of applications will begin immediately and continue until position is filled.
When applying at www.jobsatcu.com, applicants must include:1) A letter of application which specifically addresses the job requirements
and outlines qualifications2) A current Curriculum Vitae
Questions should be directed to [email protected].
“The University of Colorado Denver and Health Sciences Centerrequires background investigations for employment.”
“The University of Colorado is committed to diversity and equality in education and employment.”

The Uniformed Family Physician • Summer 201522
committee reportsresident And stUdent
The Uniformed Services University of the health Sciences Student Family Med-icine Interest Group has been chosen as one of ten recipients of the 2015 Program of Excellence (PoE) Awards as an overall winner. This is the second year in a row that the FMIG has been selected. The FMIG Network Program of Excellence Awards recognize FMIGs for their out-standing performance in organizational operation, community service, promot-ing the value of family medicine as pri-mary care, promoting the scope of family medicine, exposing residents to family medicine and family physicians, profes-sional development and measures of suc-cess. The award has been a cornerstone of the FMIG Network, as it facilitates the sharing of best practices of FMIGs from across the country and recognizes the hard work of these student groups.
The synopsis from the USU FMIG that was submitted to the AAFP is noted below.
Family Medicine is often referred to as “the backbone of military medicine.” At the Uniformed Services University (USU), our Family Medicine Interest Group (FMIG) is dedicated to creating a dynamic and engaging environment in which students are introduced to Family Medicine via community service, career development, and medical education. With an appreciation of the importance and increasing implementation of team-based, multi-disciplinary care, we also extend our efforts to others throughout the University, including our graduate school and our graduate school of nurs-ing. Our strategy has been to partner with local and national military and civil-ian agencies to engage with our com-
USUhS FMIG receives Excellence Award
Pictured left to right are: Ensign (ENS) Holly Berkley, USN; ENS Kristin Wertin, USN; Second Lieutenant (2LT) Tiffany Chang, USA; and Major (Dr.) Christopher Bunt, USAF.
USU students enjoyed attending the AAFP’s National Conference of Residents and Students in Kansas City, MO. Pictured from left to right with their POE award are ENS Megan Ohmer, USN; ENS Holly Berkley, USN; 2Lt Tejas Ranade, USAF, 2LT Tiffany Chang, USA; 2LT Michael Tracey, USA; CAPT Mark Stephens, USN; ENS Alexandra Osgood, USN.

www.usafp.org 23
munities. These initiatives include a student-run clinic for the home-less population, health education at local schools, and participation in Wounded Warrior outreach. Our chapter has two mottoes – the first, “We Got This,” pays homage to the integral role Family Physicians play in the delivery of care regardless of the time and place, a message close to home for military physicians who often serve in austere environments. The second, “healthcare Lifelong,” is used to emphasize the breadth of care that family physicians offer and to emphasize through simplicity what it is Family Physicians deliver each and every day.
The USAFP extends our con-gratulations to the students, faculty and staff who helped to make this award possible and applauds your effort, commends your achieve-ment and thanks you for promot-ing the values and philosophy of family medicine.
The award was presented to USU’s FMIG at the AAFP National Confer-ence of Family Medicine residents and Students held July 30 – August 1, 2015 in Kansas City, Missouri.
SHELLY ZIMMERMANN | [email protected]
Ministry Health Care is an integrated network of 15 hospitals and 46 clinics serving patients throughout Central, Northern
and Eastern Wisconsin. Together, with more than 650 employed clinicians, we have dedicated ourselves to delivering
high-quality, cost-effective care for the past 100 years.
NOW HIRINGFAMILY MEDICINE PHYSICIANS
With Ministry Health Care you’ll enjoy considerable practice autonomy and ample support from our PCMH model that enables you to make
the most of your time with patients. We are proud to offer our physicians a competitive compensation and benefit package, loan repayment,
flexible scheduling, the elusive work/life balance and most importantly, the voice to influence your practice today and into the future.
DON’T JUST TAKE OUR WORD FOR IT, HEAR FROM OUR PHYSICIANSWWW.MINISTRYHEALTH.ORG/RECRUITMENT
We’d love to learn more about YOU and the practice you’re looking for! [email protected] or (715) 346-5620.
Shishir Sheth, MD
Julia Pickens, MD
Eric Grajkowski, DO
Wendy Schroeder, DO
At the Uniformed Services University (USU), our Family Medicine Interest Group (FMIG) is dedicated to creating a dynamic and engaging environment in which students are introduced to Family Medicine via community service, career development, and medical education.
• FT/PT/Job sharing opportunity available• New Housing opportunities readily available• Lab and x-ray on site• Competitive compensation and benefit package
Please contact Cathy Brown804-794-5411 x1155 [email protected].
Practice Opportunity forFull time/Part time provider. Out patient opportunities.
A Division of Virginia Physicians, Inc.

The Uniformed Family Physician • Summer 201524
committee reportsMeMBer And MeMBersHiP serViCes
The USAFP Board of Directors and the Member and Membership Services Committee are pleased to announce the launch of the USAFP Mentorship Pro-gram! Our program uses a brief intake survey to identify a mentee’s needs and then matches that person with a men-tor well suited to meet those needs. regardless of your particular situation, we will work to identify a mentor to meet your needs.
ParticiPant resPonsibilities are as follows:1. Communicate with your mentor/men-
tee at least once per quarter
2. Before signing off, select a topic for discussion for the next session.
3. Continue the program for (at least) the next year.
4. Complete a brief feedback survey at the end of one year to help improve the program
sounds awesome! How do i get inVolVed? 1. Go to http://usafp.org/mentorship/2. Click on the link for your service3. Complete the intake survey where you
will select whether you would like to be a mentee, mentor, or both
4. Be matched!
wHen and How will i get my matcH?Great question! In order to optimize
the matching process, we need to develop the mentor cadre for each service. To do this, we will spend the first month (9/1/15-10/1/15) collecting intake surveys and will thereafter begin making matches (by mid October). Thereafter, matches will be made on a rolling basis.
is tHere anytHing i can do to HelP?Definitely! The success of the pro-
gram is directly tied to member partici-pation. To that end, we ask that you sign up and also share this information widely with your military Family Medicine col-leagues, including retirees.
Adam K. SapersteinUniformed Services University
Bethesda, [email protected]
LOOKING FOR ANOPPORTUNITY?
moonlightingsolutions.com800.807.7380Physician Owned…Physician Focused
Nationwide On-Site Opportunities
Telemedicine Opportunities
Telephone Call Coverage
Flexible Schedules
Malpractice Coverage With Tail
BC/BE Physicians
JOIN US
MS_1-3page_block_5.125x4.875_Layout 1 8/25/15 3:33 PM Page 1
Choose SFHC! • Family atmosphere • Southern hospitality • Competitive comp & benefits • Weekdays/dayshifts • National Health Service Corps º Loan Repayment Program º Scholars Program
Kristen Varner, HR [email protected]
(803)774-4639www.sumterfhc.com
JOIN OUR FAMILY!Join our growing practice in our mission to improve
our community's health and well-being! Sumter Family Health Center (SFHC) is a primary care and multi-specialty Community Health Center located
in the sunny midlands of South Carolina.

www.usafp.org 25
Throughout my career in military med-icine, I have seen an increasing emphasis placed on not only “providing high qual-ity care to our patients” but also on the seemingly endless metrics that inform us whether or not we are actually providing this high level of care. I spend my days trying to improve a myriad of measures (Continuity with PCM, decreased ED Usage, hEDIS, OrYX, Provider Pro-ductivity, Enrollment, Patient Satisfac-tion, and Soldier readiness). In fact, in the Army’s current model (IrIS) for funding Medical Facilities, 23 of the 44 metrics that shape how much money our hospital will get are directly related to the “Primary Care Service Line” and the care that we give through our PCMh homes. I feel like I am at an arcade playing “Whack a Mole;” we “fix” one metric, but then others go below the target. Over time, we may hear our hospital Leadership say things like “your progress on achieving Continuity targets has ‘flat-lined’” or “I see incremental progress, but we need to do better.” It’s enough to drive you crazy!
With my struggles to execute all the goals being asked of me, I wanted to find
some wisdom that would help me be more successful, and I think I have found a book that provides us with the tools to more con-sistently execute the critical tasks assigned to us. The following is a brief summary of the key points from the excellent book The 4 Disciplines of Execution:
strategy and executionThere are two principal things a leader
can influence when it comes to producing results: your strategy (or plan) and your ability to execute that strategy. Which area do most leaders struggle with? Almost all leaders will agree that it is exe-cution. But what do leaders study during business classes or in an MBA? Strategy…so, it is no surprise that leaders struggle more with execution.
tHe wHirlwindThe real enemy of execution is your day
job/the “whirlwind;” it’s the massive amount of energy that’s necessary just to keep your
operation going on a day-to-day basis; and, ironically, it’s also the thing that makes it so hard to execute anything new. The whirl-wind robs you of the focus required to move your team forward; it is urgent and it acts on you and everyone working for you every minute of every day. When urgency and importance clash, urgency will win every time. Executing in spite of the whirlwind means overcoming not only its powerful distraction, but also the inertia of “the way it’s always been done.”
tHe Problem of executionLeaders often focus too much on strat-
egy but not enough on execution. Trying to focus on too many priorities means you are not focusing on any of them. From the authors’ many years of consulting expe-rience, organizations achieve an inverse number of goals compared to the total number of goals that they designate, as shown in the following chart:
Number of Goals 2-3 4-10 11-20
Goals Achieved with Excellence 2-3 1-2 0
The 4 Disciplines of Executionby Chris McChesney, Sean Covey and Jim Huling
Key TaKeaways:• Executionofstrategicplansoftenprovestobefarmorechallengingthanmostleadersexpectbecauseour
employees often get lost in the “whirlwind” of daily activities which keep us from focusing on our most “Wildly Important Goals”/WIG.
• Thebeststrategyintheworldquicklysuccumbstoaleader’sdecisiontotrytofocussimultaneouslyontoomanytoppriorities; 2-3 “Wildly Important Goals” are all that even highly functioning teams can achieve at the same time.
• The4DisciplinesofExecutionaresimplestepstocreatepredictableprogressonthemostchallengingtasksthatyou are responsible to accomplish.
continued on page 26
leadership book series John O’Brien, MDMadigan Army Medical Center, [email protected]

The Uniformed Family Physician • Summer 201526
4dx model
disciPline 1: focus on tHe wildly imPortant
Focus your finest efforts on the one or two goals that make all the difference, instead of giving mediocre effort to doz-ens of goals. Many of our goals are impor-tant, but only one or two are WILDLY IMPOrTANT. Execution starts with focus; without it, the other 3 disciplines won’t be able to help you “There will always be more good ideas than there is the capacity to execute.” The best ever example of a clear “WIG” is from Presi-dent John F. Kennedy: “We will put a man on the moon and return him home safely by the end of the decade.”
disciPline 2: act on leadmeasures
Apply disproportionate energy to the activities that drive your LEAD Mea-
sures. While a LAG measure tells you if you have achieved the goal, the LEAD measure tells you if you are likely to achieve the goal; LEAD measures need to be both predictive and influenceable.
disciPline 3: keeP a comPelling scoreboard
Make sure everyone knows the score at all times, so that they can tell whether or not they are winning. The book has numerous excellent examples of score-boards that keep your team informed of their progress. This Discipline is really about the Discipline of “engagement” of your entire team. Don’t allow the distrac-tion of the “whirlwind” to take focus off your WIG!
disciPline 4: create acadence of accountability
The “Cadence of Accountability” is a frequently recurring cycle of account-ing for past performance and planning
to move the score forward. Optimal fre-quency is weekly. Duration is short, 30 minutes is ideal. WIG Meeting Elements:1. Account: report on commitments
that you made in the previous week.2. review Scoreboard: Learn from suc-
cesses and failures. What do our LEAD and LAG measures tell us about the changes we have been making?
3. Plan: Clear the path and make new commitments for the coming week.My Primary Care Team at Madigan
is currently utilizing these Disciplines to improve our “3rd Next Available Acute Appointment” metric, and the principles described in this book have helped us to focus our efforts and make significant progress in a short time. Long term, we plan to keep “PCM Continuity” as our top “Wildly Important Goal,” as this metric drives so many of the other met-rics that matter to our patients.
EvEry Doc can Do rEsEarchhave you wanted to do a research project but were not sure how? Would you like a user friendly workbook to help you over the inertia of starting a project? The Clinical Investigation Committee is pleased to offer user friendly tools for organizing, planning, and starting a research project.
If interested, please send a request to [email protected]. Tools Available:• EveryDocCanDoResearchWorkbook• EveryDocCanDoAPoster• EveryDocCanDoAScholarlyCaseReportWorkbook
Clinical Investigation research Tools also available on-line at www.usafp.org.
Throughout my career in military medicine, I have seen an increasing emphasis placed on not only “providing high quality care to our patients” but also on the seemingly endless metrics that inform us whether or not we are actually providing this high level of care.

www.usafp.org 27
IT ALL HAPPENS
Equal Opportunity Employer - Minorities • Females • Protected Veterans • Individuals with Disabilities
7 hospitals | 650+ physicians | 70+ specialties | 220 practice sites| 23 GME programs
At Carilion Clinic, in the heart of Virginia’s Blue Ridge, you’ll not only build a career, you’ll help lead the way in the transformation of patient care. Explore a range of rewarding opportunities at CarilionClinic.org/careers or reach us by calling 800-856-5206.
Opportunities available in the following locations: Bedford (FM) Bridgewater (FM) Dublin (FM) Floyd (FM, available 2016) Galax (IM or FM) Lexington (IM or FM) Martinsville (IM or FM) Rocky Mount (FM) Waynesboro (FM)
MEMbErS INthE NEwS
The USAFP Board of Directors encourages each of you to submit information on USAFP “Members in the News” for publication in the newsletter. Please submit “Members in the News” to Cheryl Modesto at [email protected].
NEwSlEttErSubMISSION
DEaDlINE
REMINDER: The deadline for submissions to the fall magazine is 1 October 2015.
rESEarch GraNtS
The Clinical Investigations Com-mittee accepts grant applications on a rolling basis. Visit the USAFP Web site at www.usafp.org for a Let-ter of Intent (LOI) or Grant Applica-tion. Contact Dianne reamy if you have questions. [email protected].
rESEarch JuDGES
Applications for research judges are accepted on a rolling basis. Please contact Dianne reamy ([email protected]) to request an application.
do you feel strongly about sometHing
you read in tHe uniformed family PHysician? about
any issue in military family medicine?
Please write to me...James Ellzy, [email protected]
Northwest Permanente, P.C. is currently seeking BOARD CERTIFIED/BOARD ELIGIBLE ADULT PRIMARY CARE PHYSICIANS FOR FAMILY MEDICINE & URGENT CARE in OREGON AND WASHINGTON. Specialty care is provided by a full spectrum of Northwest Permanente specialists.
WE OFFER EXCELLENT BENEFITS
Shareholder opportunities Vacation & educational leave Professional liability coverage
To apply, visit nwp.kpphysiciancareers.com & click on Apply Now. Interested candidates may also call (503) 496-7768 to speak with a Recruiter. EEO/AA
Leadership opportunities Combined clinical & research positions
Cross-specialty inter-regional collaboration
GROW YOUR CAREER IN THE PACIFIC NORTHWEST
When you choose a career with us, you are also afforded a variety of opportunities to
advance your career:
JOIN OUR FAMILY OF PHYSICIANS
Competitive compensation Medical & dental coverage Retirement benefits

The Uniformed Family Physician • Summer 201528

www.usafp.org 29
ACTIVEJeffrey Acree MDCharles Allen MDDerek Austin DOMiranda Bales Marshall MDKimberly Baptiste MDAlison Baum MDHillery Bavani DOJacques Bouchard MDDaniel Brennan MDMatthew Brown MDMatthew Bryant MDAi-Hien Bui DOBrian Burke MDDavid Bury DODanielle Cadle DOStephanie Carroll MDElisabeth Chang MDArtemio Chapa MDTimothy Chen MDYong Chun MDBianca Chun MDKevin Connolly MDAaron Conway DOAmie Dalton DOJeremy DeFoe DORichard Detheridge MDCaleb Dickison DOMichael Dickman DOBrian Doyle MDAntonio Duran MDRebecca Englebretson DOMindy Fairbanks DOWilliam Farkas DOJerry Fasoldt MDMichael Fedewa DOBrian Ford MDBrandi Freelon MDBenjamin Friday MDMatthew Gagnon MDJessica-Renee Gamboa MD
David Garcia MDNicholas Garcia DOShari Gentry MDDennis Gerold MDEva Grant DOKevin Gray MDEsther Guard DOScott Hahn DOGregory Hamilton MDKyle Harvey MDRichard Hawkins MDMatthew Hawks MDBrandon Hecht DOJoel Herness MDBrandon Hill MDJustin Hill MDSequia Holland MDMark Hooten DO, PhDElise Johnson MDDrew Kafer MDAaron Karmes DOSheila Kemper MDDaniel Kim DOKyle Kutsche MDLaShell LaBounty DOJohn Lax MDMichael Lee DOLeslie Lemanek MDCourtney Lennon MDDana Lilli MDNicholas Longstreet MDJoseph Lotterhos MDMai Luu MDBruce Matchin DOKimberley Maxwell DOAdam Mazur MDAndrew McDermott MDIan McIver DOStephen McMullan MDJason Meredith MDStephanie Meyer MD
William Michael MDLisa Mitchell MDJesse Mix DOAmina Moghul DOGordon Mok DODaniel Monlux MDDavid Moore MDChris Mullin DOJelaun Newsome DOFrederick Nielson MDMary Noel MDClifford Nolt MDValerie O’Brien MDJaime Obszanski DOMichael Odom MDJohn Olshefski MDErika Overbeek-Wager DOChristine Persinger MDKeith Petersen DOTimothy Peterson MDBryan Petti DOChristopher Pham DOPhung Phan DOClifford Porter MDRobert Powell DOZachary Prather MDNatasha Pyzocha DOJeremy Raab MDRyan Rahman MDBrian Rauch DOErika Reese MDEdward Reese MDStephanie Reiser DOJames Ries DOBenjamin Roberts DONorberto Rodriguez MDAshley Roselle DOJennifer Salguero DORicardo Sequeira MDJeanette Shimkus DOJustin Shirley MD
Samuel Sigoloff DOJenna Silakoski DOEsan Simon MDWendy Singleton MDKevin Sisk DOKristen Slappey DOKatherine Snyder MDShelby Spandl MDJon Standley DOSarah Strickland MDJoshua Tatum MDChuong Thai MDThomas Tonkin DOWilliam Valencia MDMarcel Vargas DOKarla Vega-Colon MDJohn Vincent MDJohn Vogel DOJayme Vogt DOBrian Wallin DOPamela Waters MDLuke Wicke DOMark Wirtz MDDanielle Yuen DODavid Yun MD
RESIDENTMichael Aguilar DOSyed Ali MDAndrew Ames MDLincoln Andreasen DOAmanda Antonio MDAnne Atalig MDTheresa Baumstark DOSalvatore Bertucci DOSarah Bobnick DOBrett Boyce MDPaul Bricker MDMatthew Bubuis DONathan Bumbarger MD
new memberstHe UsAFP WelCOMes tHe FOllOWinG neW MeMBers…
continued on page 30

The Uniformed Family Physician • Summer 201530
Dawn Callahan MDBrock Cardon MDGretta Carroll MDMaggie Castile MDBridget Caulkins MDRobert Caulkins MDJustin Chaltry DOJoseph Chin MDStephanie Chinchen MDAnna Christensen MDMaryrose Chuidian DORandal Cieslak DOZachariah Clark MDDillon Cleary MDKatie Coble MDCharlie Collenborne MDErin Connor MDHolly Crellin MDArthur Daniel MD, MBChBJoshua Davis MDCaitlyn DeKanter DOTroy Dillon DOAdriel Dizon MDEmma Doran MDAlicia Evans MDKara Farley MDGlynnis Flickinger MDJoanne Gbenjo MDJenner Gibson MDNathaniel Gordon MDCaitlin Granadillos DOCharles Graves MDJonathan Gruber DOBrian Guzzetti DOAndrew Hamm DODavid Harris MDJacob Heath DOAdam Henderson MDMatthew Henry DOKorey Kasper MDJohn Koch MDSabrina Kunciw MDKyle Lammlein MDJob Larson MDAmanda Lau MDMatthew Levasseur DOJanelle Lindow DORobert Lystrup MDDaniel Mactlue MD
Bryan Malave MDChristopher Manganello MDRebecca Mattson MDKenneth McArtan DOClara McComb DOKevin McDermott DOIan McDowell DOBrad McNeal DORobert McReynolds MDEric Mehta MDBryce Meyers DOLeslie Myers DOJustin Noble DOAndrea Ochab DOTheodore Ogren MDDavid Oliver MDKatrina Ostermann DOAnthony Patterson MDJared Patton MDLauren Paul DOAaron Perreault MDJonathan Pickett MDSarah Reinhart DOLeigh Rexius DOVanessa Rivera MDMary Roelofs MDJordan Ryan MDKerry Sadler MDCourtney Saint DOHolly Schmidt MDJohn Sealander MDAnna Sealander MDJustin Sevy DOJoseph Shevchik DOMaxwell Simard DOSean Simmons MDJoseph Simoneau MDAnthony Slade DOChristopher Snyder MDNofisat Sonekan MDAlexander Sparkman-Royo MDSabrina Sutherland MDKarl Swinson MDChristopher Taylor MDDylan Tracy DOSean Turner MDRyan Vonderhorst MDBettina Watkins MDMatthew Wessner DO
Haleigh White DO, DNPWilliam Wilson Jr MDLuke Womble MDVictor Wongk MDJennifer Woosley DOYou Xu MDDaniel Yee DORyan Zaleski DOMary Zorechak DO
STUDENTBryan AdamsArmando AguileraJacob ArthurJason AusmanElena BakerNathan BastienYusof BeckerAustin BellYaroslav BodnarJoshua BoothJeremy BrennemanTiffany ChangJamielou ChoKyla Christensen-SzalanskiKevin ClimacoDonald ColantonioTheodore Crisostomo-WynneJohn CurtinNathan DavidsonMichelle DentingerMatthew EarlyTobiah ElbertChin-Hsiang FengVladimir FridkinMatthew GangidineMary GasserRobert GeisDaphne GellersonRyan GillisTim GregoryJoseph GutierrezLiat GutinShelby HermanHannah HollanderAlexandria JakshaJason JonesFeel KangEddie Kwan
Maunoo LeeYizhen LiuBrent LleraErin MackElizabeth MaldonadoRyan MannTravis MoriokaSenthil MudaliarVincent NguyenOsmund NograLinda OkaiElizabeth OkonekSidney PerlesDawn QuigleyTejas RanadeCory RiccioDallin RowleyKeith RyanSandra SalzmanJoseph SaretteJohn SaretteElizabeth SchroffEvan ShawlerYarrow SheldonTyler ShortElise SienickiPatrick SingleyCarolina StarkSamuel StevensShannon ThompsonKristine TolentinoMichael TraceyAlexander VostalChloe WardDaniel WidoMichael WilliamsPaul YoungSerena ZhangDaniel Zink

www.usafp.org 31
Open 8 am to 10 pm, 365 days a year, Patient First isthe leading urgent care and primary care provider in themid-Atlantic with over 50 locations throughout Virginia,Maryland, Pennsylvania, and New Jersey. Patient Firstwas founded by a physician and we understand theflexibility and freedom you want in both your career andpersonal life. If you are ready for a career with PatientFirst, please contact us.
Each physician enjoys: • Competitive Compensation • Flexible Schedules• Personalized Benefits Packages• Generous Vacation & CME Allowances• Malpractice Insurance Coverage• Team-Oriented Workplace• Career Advancement Opportunities
Are you looking for a satisfying career and a life outside of work? Enjoyboth to the fullest at Patient First. Opportunities are available inVirginia, Maryland, Pennsylvania, and New Jersey.
Please contact Eleanor Dowdy at (804) 822-4478 [email protected].

The Uniformed Family Physician • Summer 201532
May 26, 2015 – NPR along with seven pub-lic radio stations around the country – is chroni-cling the lives of America’s troops where they live. NPR is calling the project “Back at Base.”
Caring for the nation’s veterans at the end of their lives can be a complex task. Service members — especially combat veterans — can struggle with guilt, abandonment and regret. The Army and the Department of Veter-ans Affairs are working to help them. At one Army hospital south of Seattle in Tacoma, WA, its mission is to make those last days meaningful.
Mark Goodwin rode a harley. he liked to barbecue, and he loved the Seattle Seahawks — the retired Army first ser-geant was a season ticket holder. “he’s the kind of person that wanted to make sure that everyone else in his life was taken care of,” says his wife, Traci Goodwin. “I think that’s part of being a soldier, of being a leader. So he was used to looking after people.”
But when Mark was diagnosed with stage 4 colorectal cancer last year, she says it was Mark who needed someone to look after him. he ended up at Madigan Army Medical Center in Tacoma, Wash. The Palliative Care Team including USAFP member COL Kenneth Trzep-kowski, MD helped the couple manage everything from pain care to Mark’s vet-eran benefits. “While we were focused on recovery and healing, they wanted to make sure that all of his documents were in order ... to make sure that I wouldn’t
be left with a pile of paperwork or unsure of what to do,” Traci says.
The end of life is an intimate jour-ney. When confronted with it, many are unprepared. To help, Madigan has one of the Army’s most comprehensive and well-trained end-of-life teams. It includes physicians, nurses and social workers.
Chaplain George Wallace works with the group full time.
“Sometimes what emerges are issues of betrayal and guilt. We have these really, really high — almost superhuman — standards. We call it the warrior ethos: ‘I’ll never quit,’ that sort of thing, and that’s great,” Wallace says. “But it often
members in the news
USAFP Member Kenneth Trzepkowski, MD Featured in NPR’s “Back at Base” Radio Series
Patricia MurphyREPORTER
KUOW: Seattle News and Information
Col. Kenneth Trzepkowski, chief of palliative care at Madigan Army Medical Center, unfolds one of the handmade quilts donated to the hospital for the palliative care patients.

www.usafp.org 33
comes with baggage after the fact, if you feel like you didn’t live up, or, ‘I left a buddy behind that I couldn’t bring home.”
There are other challenges: Some vets are alone at the end of life. They may be estranged from friends and family because of post-traumatic stress or sub-stance abuse issues. It can be a terrifying place, but also ripe for transformation and forgiveness. Wallace says he has witnessed it many times. “You begin to realize that you’re running out of time, so that has a
way of jarring and opening a space that can be very fruitful,” he says.
Mark and Traci Goodwin weren’t alone. But they still needed help. They spent a year at the medical center — the doctors trying to save him. But the couple knew they were walking on a knife’s edge. “When Mark finally realized that perhaps it wasn’t going to work out the way we had been praying for, he called them in along with his nursing team and wanted to talk to them, and he actually asked me to leave
the room so that he could speak to them in private,” Traci says. She says she was stunned. They’d been married for two decades and told each other everything.
Marc Goodwin’s request to speak pri-vately with his caregivers revealed the extraordinary relationship he’d built with them. he entrusted them to deliver a mes-sage to his wife about his deepest fears dur-ing his final hours. “They relayed to me that his concerns were me and how I would deal with it,” she says. “I went in after that to give him the peace of saying it’s OK. If you are ready, then I can let you go.”
Mark died the next evening.When a veteran or a service member
dies at Madigan Army Medical Center or the VA, an American flag is placed over the body. As it’s wheeled from the room, hospital staff line the hallway. Some salute, others stand at attention, to honor a veteran’s service and sacrifice.
The University of Tennessee-Saint Francis Family Medicine Residency Program in Memphis is seeking a highly qualified, full service family physician to train the family physicians of tomorrow at our unopposed (8-8-8) residency program. We seek an energetic, enthusiastic family physician that loves to teach and wants to make a difference in the lives of students, residents and practicing physicians along with patients, families and the community. We are especially interested in a physician with C-section training to teach in our well-known Advanced Women’s Health Fellowship that has produced high quality graduates for years. The residency is located in a 25,000 square foot building immediately adjacent to Saint Francis Hospital. Our physicians practice full service family medicine to include inpatient, intensive care and obstetrics. In addition, our physicians perform a variety of inpatient and outpatient procedures. We receive the best support from Saint Francis Hospital and UT. Qualified applicants should hold the MD/DO degree, be board certified, and have proven experience as a physician, leader and clinician educator. Duties include teaching students, residents, and fellows, patient care, administration, community service and research. C-section training is preferred. Academic rank and salary are commensurate with qualifications and experience.
Interested applicants should submit a cover letter and CV to
Dr. David L. Maness, Professor and Chair
UT Department of Family Medicine, 1301 Primacy Parkway, Memphis, TN 38119The University of Tennessee is an EEO/AA/Title VI/Title IX/ Section 504/ ADA/ ADEA institution in the provision of its education and employment programs and services.
Caring for the nation’s veterans at the end of their lives can be a complex task. Service members — especially combat veterans — can struggle with guilt, abandonment and regret. The Army and the Department of Veterans Affairs are working to help them. At one Army hospital south of Seattle in Tacoma, WA, its mission is to make those last days meaningful.

The Uniformed Family Physician • Summer 201534
daily infoPoemsthe UsAFP is pleased to continue providing as
a membership benefit a free subscription to daily POeMs from essential evidence Plus. daily POeMs (Patient Oriented evidence that Matters) alerts and 3,000+ archived POeMs help you stay abreast of the latest and most relevant medical literature. delivered directly to you by e-mail every Monday through Friday, daily POeMs identify the most val-id, relevant research that may change the way you practice. Monthly, the complete set is compiled and sent for additional summary review. Ongoing since 1996, their editors now review more than 1,200 studies monthly from more than 100 medical jour-nals, presenting only the best and most relevant as POeMs. the acclaimed POeMs process applies spe-cific criteria for validity and relevance to clinical practice. if you want to subscribe, please e-mail the UsAFP at [email protected] so your e-mail address can be added to the distribution list.
audio digestthe UsAFP is pleased to provide as a membership
benefit continued access to Audio digest MP3 files in the area of Family Medicine, Pediatrics and OB/Gyn.
For those not familiar with Audio-digest, they produce over 300 audio CMe/Ce programs each year. these programs are derived from lectures re-corded at more than 285 CMe/Ce meetings across the country, always with permission of the sponsor-ing organizations and the lecturers involved. the objective of Audio-digest CMe/Ce activities is to update healthcare professionals on advances in the diagnosis and management of medical disor-ders. the primary goal of each activity is to provide practical information that will improve professional competence in caring for patients.
the UsAFP has an institutional subscription which allows our members to access the MP3 files in Family Medicine, Pediatrics and OB free of charge. if you are interested in obtaining CMe for the modules, please call Audio-digest at (800) 423-2308 and they can as-sist you with the paid subscription of your choice.
to access the MP3 files in each module, please visit www.audio-digest.org. the user name is usafp2007 and the password is military2007.
stfm teacHing resourcesthe UsAFP provides a complimentary subscription
for UsAFP members to the society of teachers of Family Medicine “teaching Physician” online resource! the site
offers videos, tips, answers to frequently asked ques-tions, and links to in-depth information on teaching topics, such as:• Preparingyourpracticeteamforalearner• Integratingalearnerintoofficeroutines• Settingexpectations• Teachingstrategies• Givingfeedback• Evaluatinglearners• Billing
this will help All UsAFP members teach medics, PA’s, nP’s, medical students, residents and each other and provides you with quick answers to questions that arise during your daily interaction with learners. you can also earn up to 40.5 CMe credits by reviewing the information on the site! if you are interested in receiv-ing a log-in and password to access these resources, please e-mail [email protected] or call the UsAFP Headquarters Office at 1-804-968-4436.
Don’t Miss Out on ComplimentaryUSAFP Membership Benefits
The Uniformed Services Academy of Family Physicians proudly supports the candidacy of Mark B. Stephens, MD, MS, FAAFP for the position of AAFP Vice Speaker. The role of AAFP Vice Speaker specifically requires someone who can lis-ten, take orders, support their family physi-cian peers/leaders, offer candid advice and step in to take charge when necessary. This Mark can do!
Mark’s leadership, executive, clinical and academic experiences have prepared him to capably and successfully serve in the role of Vice Speaker. he is running his campaign on the theme, “Communication, Collabora-tion, Courage, and Conviction.” The elec-tion will take place during the AAFP Con-gress of Delegates September 28-30, 2015 in Denver, Colorado. The USAFP wishes Mark a successful campaign!
members in the news
USAFP Past President Mark Stephens, MD, MS, FAAFP Candidate for AAFP Vice Speaker

www.usafp.org 35
Arkansas’ PremierBehavioral Healthcare System
Proudly Serving Our Military Families
Pinnacle Pointe Hospital is TRICARE® certifi ed for acute and residential inpatient care services. We are committed to healing the children of military families. Our TRICARE military program offers treatment for youth and teens ages 5 to 17.
Pinnacle Pointe Behavioral Healthcare System • 11501 Financial Centre Parkway • Little Rock, Arkansas 72211
501.223.3322 • 800.880.3322 • www.PinnaclePointeHospital.com
“TRICARE” is a registered trademark of the TRICARE Management Activity. All rights reserved.
TRICARE®
Certifi ed

The Uniformed Family Physician • Summer 201536
The Uniformed Services Academy of Family Physicians1503 Santa rosa road, Suite 207richmond, Virginia 23229www.usafp.org
As the largest community health center in the Pacific Northwest, Yakima Valley Farm Workers Clinic offers the perfect balance between career, community, and quality of life.
We offer:
• Patient Centered Medical Home
• Behavioral Health and Medical Nutrition Integration
• New compensation packages comparable to private practice
• State-of-the-art EMR: Epic
Yakima Valley Farm Workers Clinic
“Working at Yakima Valley Farm Workers Clinic is like getting to practice international medicine with first world resources.”
- Tamera Schille, MD
OREGON
Wapato
GrandviewProsser
PortlandWoodburn
Salem
SunnysidePasco
Toppenish
Yakima
Spokane
Walla Walla
Hermiston
WASHINGTON
Washington • Oregon | [email protected] | 1-877-983-9247 | www.yvfwc.org