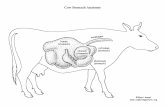
Stomach
description
Transcript of Stomach

Stomach

Gastric UlcerEtiology
Acid is less important than duodenal ulcer Lack of mucin and HCO3 secretion Decrease of prostaglandins Decrease mucosal blood flow H pylori infection ( 70%)

Gastric UlcerDiagnosis
UGI endoscpy is mandatory
Multiple biopsy and brushings
H pylori biopsy

Gastric UlcerDiagnosis
Lesion larger than 2.5 cm and located near greater curvature is considered malignant unless proven otherwise
Lesions with everted margins are suspicious for malignancy
Nondistended stomach is suggestive of linitis plastica
Atypia in bx suggest maligancy

Gastric UlcerTypes
Type 1 - 60% of all ulcers, lesser curvature, assoc with blood group A
Type II- 20% , assoc with hypersecretion and duodenal ulcer, blood group O
Type III – 5-10%, prepyloric
Type IV – 10%, within 2cm of GE junction
Type V – assoc with NSAIDs

Gastric UlcerMedical Management
Antisecretory agents
Treatment of H-pylori

Gastric UlcerIndications for Operation
Non healing ulcer
Complication ( bleeding, perforation )
Morphologic or histologic evidence of malignancy
Failed medical therapy after 3 months

Gastric UlcerPrinciples of Surgical Treatment
In contrast to duodenal ulcer, gastric ulcer should be excised
Vagotomy is indicated only for gastric ulcer asociated with hypersecretion

Gastric UlcerSurgical Treatment
Type I Antrectomy with Bilroth I is ideal Excellent results in 90-95% of
cases
Type II & III Antrectomy and vagotomy is ideal Vagotomy, drainage procedure
are alternative therapy

Gastric UlcerSurgical Treatment
Type IV Excision of ulcer is treatment of
choice

Gastric UlcerSurgical Treatment
For complication of gastric ulcer, the ulcer must be excised.
Gastric ulcer must not be patched
Bleeding ulcer should not be oversewn

H.Pylori
Gram negative, spiral, motile bacteria
Most commonly involves antrum and lower part of stomach
20% of population are carriers
90% infection among duodenal ulcer patients
70% among gastric ulcer patients

H.PyloriMechanism of Gastric ulcer Formation
Reduces surfactant effect of active phospholipid
This in time reduces gastric mucosal barrier

H.PyloriMechanism of Gastric Cancer
Formation
Causes gastritis
Intestinal metaplasia of gastric mucosa
Further progression to cancer

H.PyloriDiagnosis
Breath test ( CLO test ) , non invasive for diagnosis and for evaluation of treatment success
Biopsy – histology and monclonal antibody staining – expensive and invasive
Serology – good for initial diagnosis but not suitable to evaluate for treatment success
Urea HydrolysisH pylori survival strategy in the acid environment of the stomach
Urea is broken down to ammonia and carbon dioxide

H.PyloriTreatment
Triple antibiotic with
• Amoxicillin• Bismuth sulfate • Flagyl
• Tetracycline• Bismuth sulfate • Clarithromycin
Simultaneous treatment with anti secretory and antibiotics increases treatment success
After adequate treatment a f/u CLO test should be done in 3 weeks

Gastric Neoplasiamalignant tumor
Carcinoma Lymphoma Sarcoma Carcinoid

Gastric carcinoma
More common in males
More common among blacks
Peake age 7th decade

Gastric carcinomaTypes
Intestinal type – associated with mucosal atrophy and intestinal metaplasia
Diffuse type – no known pre-cancerous condition , associated with blood group A and female

Gastric carcinomaEtiology
Pernicious anemia Adenomatous
polyp Metaplastic change Diet rich in
nitrosurea H.pylori infection

Gastric carcinomaRole of H.pylori
90% intestinal , 30% diffuse
Distal gastric cancer

Gastric carcinomaDiagnosis
UGI endoscopy – multiple biopsy and brushing
CT scan of abdomen and pelvis
Endoscopic ultrasound
CEA/CA-125

Gastric carcinomaMorphologic type
Polypoid Fungating Ulcerative Diffuse

Gastric carcinomaHistology
Adenocarcinoma either diffuse of intestinal type
Signet cell carcinoma has poor prognosis

Gastric carcinomaTreatment
Two surgical issues
1. Extent of gastric resection2. Extent of lymphadenectomy
depends on location of cancer

Gastric carcinomaTreatment of proximal lesion
Total gastrectomy with end to side esophagojejunostomy
Proximal gastrectomy
If tumor extends to lower esophagus – distal esophagectomy with proximal gastrectomy and esophagogastric
anastomosis in right chest

Gastric carcinomaTreatment of mid gastric lesion
Subtotal gastrectomy
Routine splenectomy has higher complication without survival benefit
Omentectomy is routinely performed

Gastric carcinomaTreatment of distal gastric lesion
Distal gastrectomy with omentectomy

Gastric carcinomaTreatment for all gastric
carcinoma
At least 5 cm margin is desirable
Must do frozen section of prox and distal margins

Gastric carcinomaLymphadenectomy
D1 : resection of the regional perigastric lymph nodes (N1) with the gastric resection.
D2 : resection of the perigastric lymph nodes and those along the feeding vessels (N2) with the gastrectomy specimen

Gastric carcinomaLymphadenectomy
D2 disection does not improve survival over D1 dissection
Higher complication rate with D2 dissection

Gastric carcinomaAdjuvant therapy
No survival advantage of systemic chemo or intraperitoneal chemo
Radiation therapy for high risk gastric cancer reduces local recurrence but does not improve survival

Hiatal Hernia
Type I sliding hernia. Type II paraesophageal. Type III mixed hernia
The GE junction slides up through the esophageal hiatus during moments of increased pressure in the abdominal cavity.
The fixed type implies that there is no sliding up and down. A portion of the stomach remains stuck in the chest cavity. GE junction intact
Combination of sliding and paraesophageal

Hiatal Hernia

Hiatal Hernia
Indication for operative repair of sliding
hiatal hernias :
symptomatic hernias or
complications of GERD

Hiatal HerniaThe presence of a paraesophageal
hiatal hernia is an indication for surgical
repair
bleeding infarction perforation

Hiatal Hernia
Based on pathophysiologic studies on patients with a paraesophageal hernia, the repair of the paraesophageal hernia should include an antireflux procedure to correct the sphincter characteristics associated with a mechanically incompetent cardia.

Hiatal Hernia If time permits, preoperative
evaluation with 24-hour pH monitoring and esophageal manometry allows the identification of patients with competent cardias.
Such patients are candidates for simple anatomic repair, provided it can be done without surgical dissection of the cardia.

Performed through the abdomen or chest -360 degrees gastric fundus
wrap around the lower 1-2 cm
of
the esophagus
Rx of Hiatal Hernia Antireflux Repairs:

Rx of Hiatal Hernia Antireflux Repairs:
270 degrees gastric
wrap generally performed through
the chest
Belsey-Mark

Rx of Hiatal Hernia Antireflux Repairs:
Toupet 270 degree
Wrap

Rx of Hiatal Hernia Antireflux Repairs:
Hill posterior gastropexy
180 degrees wrap performed through the abdomen with the phrenoesophageal ligament anchored to the median arcuate ligament of the diaphragm

Gastric Volvulus
Mesenteroaxial antrum lies above cardia (i.e., rotation around
line connecting greater and lesser curvature) form seen in neonates usually acute
Organoaxial rare in kids associated with large hiatus hernia
rotation along long axis of stomach

Gastrinoma

Diagnosis of Gastrinoma
Fasting hypergastrinemia (>200 pg/ml) in the face of gastric acid hypersecretion defined as basal acid output >15mEq/h
Most patients with gastrinoma have serum gastrin levels >500 pg/ml.
A test is usually done to confirm diagnosis when serum gastrin is in the range of 200-500 pg/ml.
secretin provocative
Secretin Provocative Test: Following 2 u/kg secretin IV bolus, a rise in serum gastrin level of 200 pg/ml within 15 min or doubling of the fasting gastrin level
is diagnostic of gastrinoma.

Diagnosis of Gastrinoma
Upper GI or endoscopy will show ulcers often in unusual locations, i.e. 2nd & 3rd portions of duodenum or jejunum. The stomach may have prominent rugal folds along with excessive luminal secretions.
CT scan may show tumor in the pancreas or paraduodenal areas.
Angiography with portal venous sampling may show "hot spots" of gastrin secretion
Additional Studies:

Gastrinoma 60% of the gastrinomas are
non-beta islet cell carcinomas
25% are solitary adenomas
10% are microadenomas, or hyperplasia.

Gastrinoma One-quarter of gastrinomas are
associated with the MEN-I syndrome, in which case the tumors are usually multiple and benign.
Sporadic gastrinomas are more often single and malignant.
Even when malignancy is present, the tumors are often slow growing and compatible with a long survival.

Gastrinoma Over 90% of the patients are adequately
controlled with H2-blockers
All patients with sporadic gastrinoma should undergo surgical exploration unless there is evidence of extensive metastatic disease.
The patients with gastrinoma and the MEN-I syndrome have multiple, small pancreatic tumors that cannot be resected, and surgery is generally not indicated.
At operation, the gastrinoma should be enucleated if possible. If not, a distal pancreatectomy may be considered.

Step 1: Check gastrin level. Measure at least 3 fasting levels of gastrin on different days.
Step 2: Perform gastric acid secretory studies. A BAO value of greater than 15 mEq/h or a gastric volume of greater than 140 mL and pH of less than 2.0 are highly suggestive of gastrinoma.
Step 3: Perform a provocative test. The secretin stimulation test is the preferred test.
Step 4: Perform somatostatin receptor scintigraphy (SRS).
Step 5: Perform imaging studies to stage and localize the gastrinoma. Step 6: Determine if patient is a surgical candidate for tumor resection.
Algorithm for the evaluation of a patient with suspected gastrinoma is as follows:

Barrett's esophagus columnar epithelium-lined esophagus
complication of persistent reflux esophagitis.
at risk for development of
adenocarcinoma.

Barrett's esophagus
is an indication for multiple mucosal biopsies.
If high grade dysplasia is documented by at least two pathologists or if intramucosal carcinoma is found, esophageal resection is indicated.
If these histologic changes are not present, an antireflux procedure should be performed in an effort to halt progression of the disease.

Determination of Resectability of Cancer of
the Esophagus Pre-operative assessment of the resectability of
esophageal carcinoma is often difficult.
The usual workup for esophageal carcinoma includes:
1. Endoscopic evaluation of esophagus to confirm the diagnosis and location, and extent of disease.
2. CT scan of chest and abdomen to determine extension of disease beyond esophagus and metastatic spread.
3. Comorbidities and associated risk as listed above

Cancer of the Esophagus
Palliation is suggested in the following circumstances:
1. Location - Upper or middle third esophageal tumors that have penetrated esophageal wall (enbloc resection not possible without removal of vital structures).
2. Age - Patient over 75 years have higher operative risk and shorter life expectancy.
3. Fitness - Ejection fraction <40% or FEV1 <1.25 suggest high perioperative morbidity and mortality along with overall decreased life expectancy due to cardiopulmonary disease.
4. Clinical staging factors indicating advanced disease - recurrent nerve paralysis, Horner's syndrome, persistent spinal pain, diaphragm paralysis, fistula formation, malignant pleural effusion, tumor >9 cm, more than 20% weight loss, enlarged mediastinal lymph nodes by CT.
5. Intraoperative Staging - Unresectable primary tumor, cavitary spread, distant metastasis, extension through mediastinal wall, multiple metastatic (gross) lymph nodes.

Cancer of the Esophagus
If palliative resection cannot be done (i.e. patient
physiologically unfit or invasion of vital strictures)
radiotherapy and/or chemotherapy
(cisplatin + 5-Fu) may be helpful.
Also laser tumor ablation, esophageal intubation or stents, alone or in combination, can provide some palliation.

Perforated Cancer of the Esophagus
The diagnosis of cancer of the esophagus requires endoscopy and biopsy.
The most serious complication of esophagoscopy, with or without dilation of strictures, is perforation, which occurs in 1-2% of patients even in the hands of the most experienced endoscopists.
Because the mortality and morbidity of an esophageal perforation is directly related to the time interval between the occurrence of the injury and its diagnosis and repair, a suspected perforation must be immediately investigated.
The occurrence of pain or fever after esophageal instrumentation represents an esophageal perforation until proven otherwise.

Perforated Cancer of the Esophagus
The mortality is 10-15% in patients treated less than 24 hours following injury, and increases to 50% or more for patients with delayed surgical therapy.
If perforation is discovered promptly in a patient with intrinsic esophageal disease (esophageal cancer) and surgical treatment is undertaken early, definitive therapy i.e. esophagectomy with esophagogastrectomy is the therapy of choice.
Simple closure of a perforation above an obstructing esophageal carcinoma cannot be expected to be successful. With a delay in diagnosis, i.e. greater than 24 hours, operative choices are limited by the dangers of attempting to suture infected and edematous tissues. Nevertheless, aggressive surgical therapy may salvage an appreciable number of patients.

Operative treatment in these circumstances
include:
1. Extensive drainage of infected secretions 2. Intensive nutrition support (jejunostomies/TPN) 3. Antibiotics 4. Aggressive surgical support in a surgical ICU setting
Drainage tubes should be placed away from the aorta and major vessels to avoid erosion and serious hemorrhage and where closure has been attempted, rotation of organs as flaps, i.e. gastric fundal patch, pleural pedicle flaps have been credited with better survival.
Esophagectomy, cervical esophagostomy and gastrostomy drainage of the chest with delayed esophageal replacement is another consideration of therapy in delayed cases.
Results obtained in treating late perforations appear to be related more to the time interval between perforation and operation and to the underlying disease than to any specific techniques used.