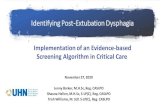
Standardizing Dysphagia Practice In Patient-Centered Care · – Hypertension – Arthritis •...
Transcript of Standardizing Dysphagia Practice In Patient-Centered Care · – Hypertension – Arthritis •...

5/30/2016
1
Bonnie Martin-Harris, PhD, CCC-SLP, BRS-S, ASHA Fellow
Professor, Dept. of Otolaryngology-Head & Neck Surgery
Professor, Dept. of Health Sciences & Research
Director, Evelyn Trammell Institute for Voice & Swallowing
Director, PhD Program in Health & Rehabilitation Science
Clinical Scientist, Ralph H. Johnson VA Medical Center
Standardizing Dysphagia Practice
In Patient-Centered Care
• NIH/NIDCD K24, Research and Mentoring on Swallowing Impairment and Respiratory-Swallow
Coordination, 2013-2018
• NIH/NIDCD R01, Standardization of Swallowing Assessment in Bottle-fed Children, 2010-2015
• NIH/NICDC R21, Respiratory Phase Training in Head and Neck Cancer, 2009 ─ 2012
• VA RR&D, Respiratory Phase Training in Dysphagic Veterans with Oropharyngeal Cancer, 2010 ─
2013
• VA RR&D, SPiRE, 2013-2015
• NIH/NIDCD K23, Standardiza<on of Swallowing Assessment, 2003 ─ 2009
• NIH/NIDCD R03, Respiratory and Laryngeal Dynamics During Swallow, 2000 ─ 2003
• Mark and Evelyn Trammell Trust, 1993 ─ 2019
• Bracco Diagnos<cs, Inc., 2009 ─ 2012
• Northern Speech Services, 2010 ─ present
• Given, Imaging, 2013- present
Support and Disclosures

5/30/2016
2
Standardized Assessment &
Essential for Translation
Guided Intervention
Swallowing Specialist
“A clinician who specializes in the neural control, function, impairment and restoration of the swallowing mechanism in dysphagic patients.”
~ Bonnie Martin-Harris, PhD

5/30/2016
3
• EVIDENCE, rather than opinion, should guide clinical
decision-making
• BROADER RANGE OF PATIENT OUTCOMES needs to be
measured in order to understand the true benefits and
risks of health care interventions
• RESEARCH PRIORITIES should be guided in part by public
HEALTH NEEDS
WHY Standardized Measurement?
WHAT Should Be Standardized?
• The INSTRUMENT – Contents and format
• DATA COLLECTION Protocol – Approach and method
• ANALYSES – Minimize variation in scoring and interpretation
• REPORTING – Well-tested approaches to presenting results
TRANSLATING RESEARCH INTO PRACTICE (TRIP)-II.
FACT SHEET, AHRQ PUBLICATION No. 01-P017.

5/30/2016
4
Modified Barium Swallow Study
Brief History
• Martin Donner
– 1965 used cine fluoroscopy for
diagnosis of neurologic dysphagia
• Jeri Logemann
– 1970’s MBSS for assessment of patients
with head and neck cancer.
Videofluoroscopic Imaging
Identify and distinguish :
• Type and severity of
impairment
• Sensorimotor function
• Cause of airway invasion
• Physiologic targets for treatment
Modified Barium Swallow Study

5/30/2016
5
GOALS:
• Valid
• Reliable
• Physiologic vs. symptom based
• Clinically practical
• Linked to clinical action
– Targeted therapy
Modified Barium Swallow Study
STANDARDIZEDMBS Measurement Tool

5/30/2016
6
Physiologic Components of Swallowing
1. Lip Closure
2. Tongue Control
3. Bolus Preparation/Mastication
4. Bolus Transport/Lingual Motion
5. Oral Residue
6. Initiation of Pharyngeal Response
7. Soft Palate Elevation
8. Laryngeal Elevation
9. Anterior Hyoid Excursion
10. Epiglottic Movement
11. Laryngeal Vestibular Closure
12. Pharyngeal Stripping Wave
13. Pharyngeal Contraction
1. Pharyngoesophageal Segment
Opening
2. Tongue Base Retraction
3. Pharyngeal Residue
4. Esophageal Clearance
Functional Targets
MBSImP™©: Standardized Protocol
ORALORAL PHARYNGEALPHARYNGEAL ESOPHAGEALESOPHAGEAL
© 2008 & © 2011 Medical University of South Carolina
Targeted Treatment of thePhysiologic Mechanism

5/30/2016
7
BiofeedbackIsometric/Isotonic
VoiceSwallowing
Sensation
• Tactile
• Auditory
• Visual
Targeted InterventionMulti-modality Dysphagia Treatment
What type of intervention is necessary?
– Compensation
• Postural techniques
• Sensory techniques
• Bolus modification
• Intraoral Prosthetics
Treatment Planning
- Exercise
• Direct
• Indirect
• Isotonic
• Isometric

5/30/2016
8
• Use it or loose it
• Use it and improve it
• Plasticity is experience specific
• Repetition matters
• Intensity matters
• Time matters
• Salience matters
• Specificity matters
• Age matters
• Compensation
• Restitution
• Self-regulation
Principles of Activity-dependent Neuroplasticity (Cortical Reorganization)
Training Paradigms
Case Study
• History of Present Illness:
– 54 year old male
– T4 N0 Mx SCCa right floor of mouth/oral tongue
– Status post right floor of mouth resection, right glossectomy, bilateral neck dissection, tracheostomy, PEG
• Past Medical History:
– Hypertension
– Arthritis
• Past Surgical History:
– Tonsillectomy
– L5 fusion

5/30/2016
9
Pre-Treatment MBS
Pre-Treatment MBSImP Scores

5/30/2016
10
PAS Scores
• Thin – 8: material enters airway, passes the vocal
folds, no effort to eject
– Occurred after the swallow only; 2° pharyngeal residue
• Nectar – 2: material enters airway, remains above the
vocal folds, ejected from airway
• Honey – 2: material enters airway, remains above the
vocal folds, ejected from airway
0 = Cohesive bolus between tongue to palatal seal
1 = Escape to lateral buccal cavity and/or floor of mouth
3 = Posterior escape of greater than half of bolus
Targeted InterventionComponent 2: Bolus Hold

5/30/2016
11
• Compensation
- Modify bolus volume
- Modify bolus texture
• Sensory
- Stereognosis
• Motor
- Tongue to palatal seal
(anterior, lateral, posterior)
Targeted InterventionComponent 2: Bolus Hold
Tongue Exercise
• Improved tongue strength in healthy young and old (isometric
tongue strengthening exercises – resistance exercise)
- Lazarus et al., 2003; Hind & Robbins, 2004; Robbins et al., 2005 & 2008
• And in patients with CVA – improved maximum
isometric tongue pressures, maximum swallow
pressures, PA Scale
- Kays et al., 2004
Targeted InterventionComponent 2: Bolus Hold

5/30/2016
12
SwallowSTRONG
• Facilitates increased pressures generated by tongue and other
oropharyngeal musculature through progressive resistance isometric
exercise
- Measures pressure generation
- 4 sensor custom fit mouthpiece
- Auto calculates exercise targets
- Provides knowledge of results to user
- Transfers from non-swallowing practice to swallowing behavior
• U.S. patent # 6702765 FDA Registered
• http://www.swallowsolutions.com/Swallow_Solu
tions_LLC/Home.html
Targeted InterventionComponent 2: Bolus Hold
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
COMPENSATION
Targeted InterventionComponent 2: Bolus Hold

5/30/2016
13
0 = Timely and efficient chewing and mashing
1 = Slow prolonged chewing/mashing with complete re-collection
2 = Disorganized chewing/mashing with solid pieces of bolus unchewed
3 = Minimal chewing/mashing with majority of bolus unchewed
Targeted InterventionComponent 3: Bolus Prep
• Compensation
- Modify bolus volume
- Modify bolus texture
- Optimize intra-oral placement
• Sensory
- Stereognosis
• Motor
- Tongue strengthening (resistive) exercise
- Tongue flexibility (range of motion) exercise
- Mandibular strengthening (resistive) exercise
- Mandibular flexibility (range of motion) exercise
Targeted InterventionComponent 3: Bolus Prep

5/30/2016
14
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
COMPENSATION
Treatment PlanningComponent 3: Bolus Prep
0 = Brisk tongue motion
1 = Delayed initiation of tongue motion
2 = Slowed tongue motion
3 = Repetitive/disorganized tongue motion
Targeted InterventionComponent 4: Bolus Transport

5/30/2016
15
• Compensation
• Modify bolus volume
• Modify bolus texture
• Optimize intra-oral placement
• Sensory
• Stereognosis
• Motor
• Tongue strengthening (resistive) exercise
• Tongue flexibility (range of motion) exercise
• Suck-swallow and squeeze
Targeted InterventionComponent 4: Bolus Transport
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
• Suck-swallow exercise
COMPENSATION
• Syringe
• Suck-swallow maneuver
Treatment PlanningComponent 4: Bolus Transport

5/30/2016
16
0 = Complete oral clearance
1 = Trace residue lining oral structures
2 = Residue collection on oral structures
4 = Minimal to no clearance
Targeted InterventionComponent 5: Oral Residue
• Compensation
• Modify bolus volume
• Modify bolus texture
• Optimize intra-oral placement
• Sensory
• Stereognosis
• Motor
• Tongue strengthening (resistive) exercise
• Tongue flexibility (range of motion) exercise
• Suck-swallow and squeeze
Targeted InterventionComponent 5: Oral Residue

5/30/2016
17
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
• Suck-swallow exercise
COMPENSATION
• Syringe
• Suck-swallow maneuver
Treatment PlanningComponent 5: Oral Residue
0 = Bolus head at posterior angle of ramus
1 = Bolus head in valleculae
2 = Bolus head at posterior laryngeal surface of epiglottis
4 = No visible initiation at any location
Targeted InterventionComponent 6: Initiation

5/30/2016
18
• Compensation
• Modify bolus volume
• Modify bolus texture
• Postural adjustment (chin tuck)
• Sensory
• Bolus Hold: Tongue to palatal seal (anterior, lateral,
posterior)
• Oropharyngeal stimulation followed by productive
tongue movement
• Taste manipulation
• Motor
• Tongue strengthening (resistive) exercise
• Tongue flexibility (range of motion)
Targeted InterventionComponent 6: Initiation
Chin Tuck
• Delayed initiation of the
pharyngeal swallow
• Widens valleculae (timing)
• Improves vestibular closure
• Brings pharyngeal wall closer
to tongue base
Targeted InterventionComponent 6: Initiation

5/30/2016
19
Motor
• Pharyngeal shortening - falsetto
Targeted InterventionComponent 6: Initiation
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
• Suck-swallow exercise
• Falsetto extensions
COMPENSATION
• Syringe
• Suck-swallow maneuver
• Chin tuck
Treatment PlanningComponent 6: Initiation

5/30/2016
20
0 = Complete anterior movement
1 = Partial anterior movement
Targeted InterventionComponent 9: Anterior Hyoid Excursion
• Sensory
- Visual feedback
• Motor
- Suprahyoid strengthening and range of motion
- Sustained hyolaryngeal movement at the height of the swallow (Mendelsohn maneuver)
- Shaker exercise (contraindicated – trach)
- Expiratory Muscle Strength Training (EMST)
Targeted InterventionComponent 9: Anterior Hyoid Excursion

5/30/2016
21
– Feedback of electrical activity from muscle groups is immediate
– Duration of of laryngeal elevation (Mendelsohn Maneuver)
– Amount of electrical activity in submandibular muscles (Effortful Swallow)
Mendelsohn Maneuver Effortful SwallowSteele et al., 2012
Surface Electromyography (sEMG) Biofeedback
Suprahyoid Musculature
Targeted InterventionComponent 9: Anterior Hyoid Excursion
Mendelsohn maneuver
• Reduced hyolaryngeal motion
• Facilitates and sustains
laryngeal closure and PES
opening (Cook et al., 1989;
Jacob et al., 1989)
• Facilitates and sustains
contraction of oropharyngeal
muscles
Kahrilas, Logemann, Krugler & Flanagan, 1991
Targeted InterventionComponent 9: Anterior Hyoid Excursion

5/30/2016
22
Kahrilas, Logemann, Krugler, & Flanagan, 1991
Mendelsohn Maneuver: Sustained Hyolaryngeal Excursion
Targeted InterventionComponent 9: Anterior Hyoid Excursion
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
• Suck-swallow exercise
• Falsetto extensions
• Mendelsohn maneuver– sEMG
COMPENSATION
• Syringe
• Suck-swallow maneuver
• Chin tuck
Treatment PlanningComponent 9: Anterior Hyoid Excursion

5/30/2016
23
0 = Complete inversion
1 = Partial inversion
Targeted InterventionComponent 10: Epiglottic Inversion
• Compensation
- Effortful Swallow
• Sensory
- Viscous Bolus
• Motor
– Pharyngeal contraction exercise (swallow and squeeze)
– Tongue base retraction
Targeted InterventionComponent 10: Epiglottic Inversion

5/30/2016
24
Targeted InterventionComponent 10: Epiglottic Inversion
Increased Bolus Viscosity has a positive effect (lower score)
on key swallowing components
Epiglottic Movement Scores
Pudding
Th
in
0 1 2
0 43 0 0
1 16 14 1
2 9 13 23
p < 0.001
Worse scores on thin
Blair J, Armeson K, Hill, E., Martin-Harris B
• tongue base retraction
• pharyngeal contraction/stripping
• Effort increasea posterior tongue
base and pharyngeal movement
(Pouderour & Kahrilas, 1995)
Effortful swallow (swallow and squeeze)
Targeted InterventionComponent 10: Epiglottic Inversion

5/30/2016
25
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
• Suck-swallow exercise
• Falsetto extensions
• Mendelsohn maneuver– sEMG
• Therapeutic viscous bolus trials
• Effortful swallow– sEMG
COMPENSATION
• Syringe
• Suck-swallow maneuver
• Chin tuck
• Effortful swallow
Treatment PlanningComponent 10: Epiglottic Inversion
0 = Complete distension and duration; no obstruction of flow
1 = Partial distension/partial duration; partial obstruction of flow
2 = Minimal distension/minimal duration; marked obstruction of flow
Targeted InterventionComponent 14: PES Opening

5/30/2016
26
• Compensation
- Modify bolus volume
- Modify bolus texture
- Postural techniques (head turn, chin tuck)
- Employ maneuver (Mendelsohn)
• Motor
- Suprahyoid strengthening and flexibility
(range of motion)
- Sustained hyolaryngeal movement at the
height of the swallow
- Pharyngeal contraction exercise (swallow
and squeeze)
- Shaker exercise
Targeted InterventionComponent 14: PES Opening
Targeted Intervention
Increased Bolus Viscosity has a positive effect (lower score)
on key swallowing components Blair J, Armeson K, Hill, E., Martin-Harris B
Pharyngeal Stripping Wave Scores
Pudding
Th
in
0 1 2
0 53 0 0
1 16 34 1
2 1 4 10
p < 0.001
Worse scores on thin
Component 14: PES Opening

5/30/2016
27
Chin tuck + Head turn
• Delayed initiation of the pharyngeal
swallow
• Unilateral pharyngeal bulging/paresis
• Decreased PES opening
• Unilateral laryngeal dysfunction
• Extrinsic pressure to thyroid
cartilage, increases adduction
Targeted InterventionComponent 14: PES Opening
• Shaker exercise
- Improved hyolaryngeal excursion and UES/PES opening
- Healthy normal subjects and patients with chronic dysphagia
- Contraindicated in individuals with tracheostomy
Suprahyoid Muscles & UES/PES Opening
Shaker et al., 1997 & 2002
Targeted InterventionComponent 14: PES Opening

5/30/2016
28
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
• Suck-swallow exercise
• Falsetto extensions
• Mendelsohn maneuver– sEMG
• Therapeutic viscous bolus trials
• Effortful swallow– sEMG
COMPENSATION
• Syringe
• Suck-swallow maneuver
• Chin tuck
• Effortful swallow
• Mendelsohn maneuver
• Head Turn
Treatment PlanningComponent 14: PES Opening
0 = No bolus between TB and PPW (Posterior Pharyngeal Wall)
1 = Trace column of contrast or air between TB and PPW
2 = Narrow column of contrast or air between TB and PPW
4 = No appreciable posterior motion of TB
Targeted InterventionComponent 15: Tongue Base Retraction

5/30/2016
29
• Compensation
• Modify bolus volume
• Modify bolus texture
• Posture (chin tuck)
• Motor
• Tongue hold (Masako maneuver)
• Pharyngeal contraction
exercise (Effortful swallow)
Targeted InterventionComponent 15: Tongue Base Retraction
• Anchoring the anterior tongue
causes the glossopharyngeal portion
of the superior constrictor muscle to
use more force in contracting.
• Decreases space between base of
tongue and posterior pharyngeal
wall to aid in efficiency of bolus
transport in pharynx.
Masako maneuver
Targeted InterventionComponent 15: Tongue Base Retraction
swallowingdisorderfoundation.com
Logemann & Fujiu, 1996

5/30/2016
30
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
• Suck-swallow exercise
• Falsetto extensions
• Mendelsohn maneuver– sEMG
• Therapeutic viscous bolus trials
• Effortful swallow– sEMG
• Masako maneuver
COMPENSATION
• Syringe
• Suck-swallow maneuver
• Chin tuck
• Effortful swallow
• Mendelsohn maneuver
• Head Turn
Treatment PlanningComponent 15: Tongue Base Retraction
0 = Complete pharyngeal clearance
1 = Trace residue within or on pharyngeal structures
2 = Collection of residue within or on pharyngeal structures
3 = Majority of contrast within or on pharyngeal structures
Targeted InterventionComponent 16: Pharyngeal Residue

5/30/2016
31
• Dependent on physiologic cause (pharyngeal contraction (Components
12/13), tongue base retraction (Component 15), PES opening (Component
14))
• Compensation
- Modify bolus volume
- Modify bolus texture
- Alter position
- Liquid wash
- Double/multiple Swallows
Targeted InterventionComponent 16: Pharyngeal Residue
Reclined Position
• Inefficient oral transit
• Decreased pharyngeal clearance
• Utilizes gravity to clear oral cavity
• Redirects bolus away from
laryngeal vestibule
• Maintains retention in pharyngeal
recesses
Targeted InterventionComponent 16: Pharyngeal Residue

5/30/2016
32
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
• Suck-swallow exercise
• Falsetto extensions
• Mendelsohn maneuver– sEMG
• Therapeutic viscous bolus trials
• Effortful swallow– sEMG
• Masako maneuver
COMPENSATION
• Syringe
• Suck-swallow maneuver
• Chin tuck
• Effortful swallow
• Mendelsohn maneuver
• Head turn
• Reclined position
• Liquid wash
• Double swallow
Treatment PlanningComponent 16: Pharyngeal Residue
Tailored Therapy
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
• Suck-swallow exercise
• Falsetto extensions
• Therapeutic viscous bolus trials
• Mendelsohn maneuver– sEMG
• Effortful swallow– sEMG
• Masako maneuver
COMPENSATION
• Syringe
• Suck-swallow maneuver
• Chin tuck
• Head turn
• Reclined position
• Effortful swallow
• Mendelsohn maneuver
• Double swallow
• Liquid wash
DIET• PEG
• Supplemental nectar thick liquids

5/30/2016
33
• 10 weeks of structured therapy:
– 2 weeks at 3x/week as IP• Sessions lasted 30-45 minutes
• 15 repetitions of each exercise were performed
• Goal: 5 reps/min
– 8 weeks at 1x/week as OP• 1 hour
• 25 reps each
• 5 reps/min
– Independent home exercise• Adherence: 3x daily performance of all exercises
• 10 reps each
• 5 reps/min
Treatment Course
Post-Treatment MBS

5/30/2016
34
Post-Treatment MBSImP Scores
PAS Scores
• Thin – 2: material enters airway, remains above the
vocal folds, ejected from airway
• Nectar – 1: material does not enter airway
• Honey – 1: material does not enter airway
• Pudding – 1: material does not enter airway
• Solid – 1: material does not enter airway

5/30/2016
35
Additional Tailored Therapy
EXERCISE
• Resistive tongue exercise– SwallowSTRONG© device
• ROM exercise
• Suck-swallow exercise
• Mendelsohn maneuver– sEMG
• Effortful swallow– sEMG
• Masako maneuver
• Shaker
COMPENSATION
• Suck-swallow
• Effortful swallow
• Double swallow
• Liquid wash
DIET
• DC PEG
• Thin liquids
• Mechanical soft
SCHEDULE
• Continue structured tx 1x/week for 4 weeks – focus on oral components
• Continue independent exercise at 2x/day, 10 reps/exercise, 5 reps/min
Standardized Reporting
• Improved financial performance
• Improved quality of care
• Reduced malpractice risk
• Compliance with HIPAA, other government
regulations
• Improved job satisfaction for providers and staff
TRANSLATING RESEARCH INTO PRACTICE (TRIP)-II.
FACT SHEET, AHRQ PUBLICATION No. 01-P017.
Electronic Medical Record

5/30/2016
36
Database and Dysphagia Registry
• Database - medical, demographic, MBSImP™© scores, treatment, outcome data (de-identified)
MBSImP™© Clinical Report
The Interface Allows the Registered Clinician to…
• enter patient medical histories, MBSImP™© study scores, and
related information in a manner that is efficient and HIPAA
compliant
• quickly produce a clinical report of each MBSImP™© study
• track the status of his/her patients over time
• evaluate the success of patient management and treatment
strategies
• optimize patient care through practices consistent with evidence-
based medicine

5/30/2016
37
History & Subjective Information
• Demographics
• Primary diagnosis
• Comorbidities
• Morbidities
• Medical history
• Surgical history
• Medical treatments
• Medications
• Allergies
• Social History
MBSImP™© Clinical Report
• Intake/diet status
• FOIS score
• Pain assessment
• Patient reported outcomes
History & Subjective InformationMBSImP™© Clinical Report

5/30/2016
38
History & Subjective InformationMBSImP™© Clinical Report
• Patient Positioning
• VFSS Viewing Planes
• Consistencies & Volumes
• MBSImP Scores Narrative
Study Details & ScoresMBSImP™© Clinical Report

5/30/2016
39
• Clinical findings
• Measurement of function
• Standardized scoring
• Outcome Tracking
Study Details & ScoresMBSImP™© Clinical Report
Study Details & ScoresMBSImP™© Clinical Report

5/30/2016
40
Clinical Assessment & Plan of CareMBSImP™© Clinical Report
Clinical Assessment & Plan of CareMBSImP™© Clinical Report

5/30/2016
41
• Specific • Achievable • Timely
• Measurable • Realistic
Prognosis & GoalsMBSImP™© Clinical Report
Prognosis & GoalsMBSImP™© Clinical Report

5/30/2016
42
Editing, Downloading & ReportingMBSImP™© Clinical Report
Tracking Swallowing OutcomesMBSImP™© Query