Special Hematologic Examination
Transcript of Special Hematologic Examination
-
8/4/2019 Special Hematologic Examination
1/5
Review: STEM CELL LINEAGE AND DIFFERENTIATION
(kindly check your histology books for this one)
SUMMARY ON BLOOD COAGULATION
Function of the Coagulation System
1. Controlling bleeding2. To maintain blood in a clot free state (thrombosis
should be controlled)
3. To maintain the integrity of the endothelium due toendothelial injury
Key Regulators of Coagulation System (NEVERFORGET!):
1. VASCULAR WALL2. COAGULATION SYSTEM3. PLATELETS
Platelet defects can be classified as:
a. Quantitative : either there is a decrease orincrease in the number of platelets.
- ThrombocytoPENIA = decrease inplatelet count
- ThrombocyTOSIS = increase in plateletcount
- REMEMBER: normal platelet count =150,000-450,000/L of blood
(labtestsonline.com)
b. Qualitative : defect is on the surface membraneprotein or granules (factors that contribute to
platelet integrity and function)
Examples of Qualitative Disorders
Glanzmanns thrombasteniaDefect :
- Failure of the platelets to aggregate inresponse to a normal stimuli
- Absence or reduced platelet glycoprotein(GP) IIb or IIIa as well as fibrinogen
receptors needed for aggregation
Characteristics:
- Inherited, autosomal recessive- Platelets appear normal, platelet count is
normal and platelets adhere to exposed
subendothelial proteins.
Prolonged BT but Normal PT & APTT
BT = Bleeding time
PT = Prothrombin time
APTT = Activated partial thromboplastin time
Bernard Soulier SyndromeDefect :
- Deficiency of platelet surfaceglycoproteins (GP) Ib / Ix
Characteristic:
- Autosomal recessive disorderProlonged BT, large platelets,
thrombocytopenia
- Bleeding occurs because affectedplatelets do not adhere to the Von
Willebrand factor in the subendothelial
matrix
There are several platelet function disorders
relating to platelet secretion, which refers to
the release of the contents of platelet
granules that occurs following platelet
activation
- This includes:Gray Platelet syndrome
Chediak-Higashi syndrome (CHS)
Dense Granule deficiency
Review questions:
What is the common congenital bleeding disorder?
Ans : Von Willebrand Disease
What is the common congenital coagulation disorder?
Ans : Factor VIII or Hemophilia A
What test is used to detect coumarin or heparin?
Ans: PT (Prothrombin Time)
Test to detect Heparin? PTT
Test for Intrinsic factor? PTT (APTT)
Test for extrinsic factor? PT
Lecture Proper
Special Hematologic Test
Categories:
I. Tests to determine presence of hemolysis(hemolytic anemia)
II. Hemoglobin electrophoresisIII. Bone marrow examination (bone marrow
aspirate and biopsy)
Subject: Pathology (CP)
Topic: Special hematologic tests
Lecturer: Dr. Pascual
Date of Lecture: August 18, 2011
Transcriptionist/Editor: RAAJAH
Pages:SY
2011-2012
-
8/4/2019 Special Hematologic Examination
2/5
I. TESTS TO DETERMINE PRESENCE OF HEMOLYSIS(HEMOLYTIC ANEMIA)
A.RETICULOCYTE COUNT- A measure of marrow erythropoiesis (bone
marrow production of RBCs)
Principle:
- Reticulocytes are immature, non-nucleatedRBCs with remnants of RNA.
- Stage between orthochromatic normoblast andmature erythrocytes
Procedure:
1. Mix an equal amount of patients blood witha supravital stain
** supravital stain may be either Methylene
blue or brilliant cresyl blue
** cytoplasmic RNA does not take up the
stain used normally for CBC that is why
supravital stain is needed.
**Supravital stain - test used for detecting
reticulocytes
**Giemsa or wright stain - used for CBC
2. Incubate for 15 minutes3. Make a smear4. Count the number of reticulocytes that you
see in 1000 RBC/10
Normal value:
Reticulocyte : 0.005 0.015 or (0.5 1.5%)
**divide the # of reticulocytes by 10 if you want
to get the percent equivalent.
Interpretation:
- An increase in reticulocyte count indicates anincrease in bone marrow erythropoiesis
- A decrease in reticulocyte count indicates adecrease in bone marrow erythropoiesis
Indications:
- May be used in the diagnosis of hemolyticanemia
**Remember: in hemolytic anemia there is no defect
in RBC production but rather, this may reflect an
increased RBC destruction in the circulation
**Hemolytic anemia = increased reticulocyte count
due to the increased destruction in the periphery
(circulation), the bone marrow tries to compensate
by producing more red cell precursors (reticulocytes)
- May be used to monitor patients response toiron therapy in the treatment of iron deficiencyanemia
B.DIRECT ANTIGLOBULIN (COOMBS TEST)Principle:
- Some forms of hemolytic anemia can be due toiso-antibodies or auto-antibodies which detects
red cell membrane antigens as foreign
o These antibodies then attach to the cellmembrane antigen and induce hemolysis
- Direct Coombs test detects the coating of thered cell by these antibodies (iso-antibodies and
auto-antibodies attached to red cells)
Direct coombs test detects in-vivo coating of RBCs by
antibodies
Px RBC (coated w/ Ab) + Coombs reagent (AntiH & Ab)
Procedure
- Patients RBCs (coated with antibody) are mixedwith commercially prepared Coombs reagent
(antihuman globulin antibody)
**If patient red cells are coated by antibodies, anti-
human antibodies (reagent) will bind to the patient
antibodies = AGGLUTINATION
Interpretation:
(+)result : + Agglutination = POSITIVE Coombs Test
(-) result : - Agglutination = NEGATIVE Coombs TestIndications:
- May be used in the diagnosis of the following:o hemolytic disease of the newborno hemolytic anemia in adultso hemolytic transfusion reactions
** In all these settings, you have antibodies attached to
the red cell membrane
C. OSMOTIC FRAGILITY TEST / INCUBATED OSMOTICFRAGILITY TEST
- Measures the ability of the red cells to take upfluid without lysing
- Fragility of the cell is primarily dependent on theshape of the cell
- Assesses primary factors that determine how redblood cells react in the osmotic fragility test
- Requested if one is suspecting congenitalhereditary spherocytosis
3 primary factors that determine how red blood cellsreact in the osmotic fragility test
1. Functional status of the cell membrane2. Volume of the cell3. Surface area of the cell
Best example is a spherocyte - due to its smaller
surface area resulting from a defect in its red cell
cytoskeleton, it is more fragile
Principle:
- Red cells placed in an isotonic solution, usually a0.85 0.9 NaCl solution, the fluid will neitherenter or leave the cell
- Placing the red cells in a hypotonic solution, (eg.0.25 NaCl solution), the cells swell and rupture.
- Spherocytes (defect with ankerin) are moresusceptible to hemolysis in hypotonic solution
than normal RBC that hemolyse at
concentrations above normal
-
8/4/2019 Special Hematologic Examination
3/5
Procedure:
1. Mix patients blood with NaCl solution ofdecreasing concentration
2. Centrifuge and incubate for 30 mins at roomtemperature (osmotic fragility test)
** incubate it for 24 hours for incubated
osmotic fragility test
3. Examine the optical density of the supernatantusing a spectrophotometer4. Calculate for % hemolysis using the formula:
% Hemolysis = OD of the supernatant x 100
OD of the test tube (no NaCl)
**OD Optical Density
Reference values
Hemolysis usually begins at 0.50 NaCl concentration and
is completed at 0.30 NaCl concentration
**increased osmotic fragility hemolysis starts at a
higher concentration (0.55 1 NaCl)
**decreased osmotic fragility hemolysis starts at
lower concentration less than 0.30 NaCl (normal)
NORMAL VALUES
NaCl
Concentration
%
Hemolysis
1.00 0.55 0
0.50 0 5
0.45 0 45
0.40 50 90
0.35 90 99
0.30 97 100
0.20 0.10 100
Interpretation:
- INCREASED OSMOTIC FRAGILITY is usuallyobserved in cases of congenital spherocytosis
and acquired hemolytic anemia
- DECREASED OSMOTIC FRAGILITY (DOF) is usuallyobserved in cases of iron deficiency anemia,
thalassemia and sickle cell anemia** disease entities of DOF shows target cells in the
periphery as seen in thalassemia, severe iron
deficiency anemia and some liver diseases.
Indications:
- May be used in the diagnosis of CongenitalSpherocytosis
o This inherited disorder is caused by intrinsicdefects in the red cell membrane
Abnormally in the red cell membrane
cytoskeleton (proteins)
Weakness of themembrane
o Morphology: the spherocytosis appear asmicrocytes without central pallor:
abnormally small, dark staining
(hyperchromic) red cells lacking the normal
central zone of pallor
o Moderate splenic enlargement ischaracteristic (500 gm to 1000 gm). It results
in the congestion of the cords of Billroth and
work hyperplasia due to markedly
increased erythrophagocytosis
o When these red cells go in the circulationbecause of this membrane instability, there
would be fragmentation of red cellmembrane in order for the red cell to
compensate and contain the same amount
of hemoglobin, it will assume a spherical
shape less deformable less elasticwhen
it is in the spleen it will not be able to leave
the spleen making it stay longer in the spleen
and be more exposed to phagocytic cells
hemolysis chronic hemolytic anemia
D. ACID SERUM (HAMS) TEST-
This test is used in the diagnosis ofparoxysmalnocturnal hemoglobinuria
Principle:
- Patients with PNH (paroxysmal nocturnalhemoglobinuria) are more susceptible to
complement mediated hemolysis because of a
red cell membrane defect
** in PNH you also have hemolytic anemia
**basic defect in PNH can be traced to the cell
membrane which is susceptible to complement
mediated hemolysis due to a defect in GP-I
(glycoprotein-1) membrane enzymes.
** CD 55 or decay accelerating factor
** CD 59 or membrane inhibitor of reactive lysis
** CD 8
Procedure:
1. Patients red cells are mixed with normal serum(ABO compatible serum), with the patients own
serum and with normal serum inactivated to
destroy complement.
2. Patients washed RBC + ABO compatible normalserum + a weak acid (0.15 NHCL)
** when you acidify the mixture, you are
actually activating complement by the
alternative pathway and facilitates binding of C3
to the RBC membrane
** Control: using normal red cells
3. Incubate at 37C for 1 hour** normal acidified serum and treated serum
prepared by incubation at 56C for 30 minutes to
inactivate complement activity are also added to
the patient and control cells in separate tubes.
4. Determine the percent hemolysed red cells.5. (+) result: >10-15% RBC hemolysed
II. HEMOGLOBIN ELECTROPHORESIS- Used to detect abnormal hemoglobin
*Ex. Hemoglobin S Sickle Cell Anemia
Hemoglobin H Thalassemia
-
8/4/2019 Special Hematologic Examination
4/5
Hemoglobin A Normal
- Used to diagnose hemoglobinopathyPrinciple:
- Hb molecules in alkaline solution have a net (-)charge and migrate toward the anode in an
electrophotometric system
Procedure
1. Patients hemolysate is placed in a celluloseacetate membrane and immersed on both endsin buffered solution.
** a hemolysate is prepared from the patients
blood sample and placed on the cathode side of
the acetate strip because they ave a net negative
charge in an alkaline solution so they will migrate
toward positive side.
2. Electric current is applied and allows Hb tomigrate different speeds (slow, intermediate or
fast). Ex A2 (slowest) < C < S < F < A (fastest)
** since each of the different hemoglobins has
distinctly different amino acid contents, the
different hemoglobins migrate along the acetate
strip at different rates of speed for a specific pH
** the speed at which the hemoglobin travels is
directly dependent on the net harge (because of
the amino acid content)
** the differences in the speed, you can separate
one hemoglobin kind from the other.
3. Upon separation, Hbs is stained and quantitated4. Unknown identified by comparison with known
Hb
** by placing the acetate strip in a densitometer,
one is able to quantify the different hemoglobins
present
** cellulose acetate method is for screening
** citrate agar method is for confirmation; has
an acidic medium
Indications:
- To detect and identify abnormal hemoglobin
III. BONE MARROW EXAMINATION (BONE MARROWASPIRATE AND BIOPSY)
- Marrow fills the spaces between the trabeculaeof bone in the marrow cavity and is soft and
semi-fluid. It is therefore, amendable to
sampling (for smear preparation)
TWO PARTS:
1. ASPIRATE (SMEAR): FOR MORPHOLOGY Cytologic types, proportions of the
hematopoietic cells in the marrow.
2. CORE BIOPSY (HEMOLYTIC REACTIONS) : FORCELLULARITY
Anatomic relation of cells to fat, connectivetissue stroma
Important for evaluating disease thatproduces focal lesions (ex. NHL, MM,
metastatic tumors, amyloidosis, granulomas)
Mandatory for dry taps on aspiration (inaplastic anemia)
This is done under local anesthesia Biopsy usually follows aspiration. This is
performed by changing the direction of the
needle to avoid the aspiration site
COMMON SITES : Adults
1. Posterior superior iliac crest (most common site)2. Anterior superior iliac crest3. Sternum
COMMON SITES: Newborn / infants
1. Upper end of tibial boneSYSTEMATIC APPROACH IN EXAMINING MARROW
SMEAR OR BIOPSY INCLUDE:
1. Cellularity** just examine the proportion of cells to fat
**as one ages the proportion of fat increases as
compared to the number of cells.
2. Myeloid : Erythroid ratio** normal ratios is 3 myeloid elements for every
erythroid elements (3:1)
3. Maturation of erythroid series4. Maturation of myeloid (granulocytic) series5. Number of megakaryocytes (precursor of
platelets)
** normally you should see 1-3 per HPF
6. Other cells: histiocytes, osteoclast, fibroblastand metastatic cells
7. Other abnormalities (granuloma, fibrosis,necrosis and abscess)
** Special stains
o IRON STAIN : iron deficiency anemiao RETICULIN STAIN : assess marrow fibrosis in the
case of myelofibrosis
Indications:
1. Diagnosis or confirmation of certain anemias notpossible by other procuedures
Ex. Iron deficiency anemia, megaloblastic anemia
2. To determine the cause of pancytopeniaEx. Myelodysplastic syndrome, aplastic anemia,
aleukemia leukemia (low wbc count and no
blasts), hypersplenism (problem is no longer in
the bone marrow instead it is the periphery)
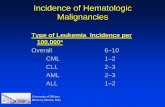
3. Diagnosis and classification of leukemias andlymphoid neoplasm
Ex. Acute leukemia, multiple myeloma
4. Staging of lymphoid neoplasm and metastaticcarcinoma
-
8/4/2019 Special Hematologic Examination
5/5
Ex. Breast cancermetastatic carcinoma in the
bone marrow stage 4
5. Demonstrate focal lesions (granuloma andmetastatic lesions)
SLIDES PICTURES (POWERPOINT) DOUBLE CHECK PLS
NORMOCELLULAR MARROW
- Equal amount or proportion off fat as comparedto marrow on marrow elements
HYPOCELLULAR MARROW
- Increased fat as compared to marrow elements
HYPERCELLULAR MARROW
- May be due to acute leukemia
APLASTIC MARROW (APLASTIC ANEMIA)
- No marrow elements
IDIOPATHIC THROMBOCYTOPENIA PURPURA
- Megakaryocytes are present and it is increasedin ITP
BONE MARROW METASTASIS (MYELOPHTHISIC
ANEMIA)
- Pale staining area with epithelial cells andnormal marrow elements
- @tip of arrow: nests of carcinoid tumor(http://www.va.gov/telepathvisn6/hemcase.htm)
END OF TRANSCRIPTIONAnd He said, My grace is sufficient for you; for My strength is made perfect in
weakness. 2 Corinthians 12:9
http://www.va.gov/telepathvisn6/hemcase.htmhttp://www.va.gov/telepathvisn6/hemcase.htmhttp://www.va.gov/telepathvisn6/hemcase.htmhttp://www.va.gov/telepathvisn6/hemcase.htm