SOG - Process Flow Template Word Version February 2010
-
Upload
mark-giberson -
Category
Documents
-
view
216 -
download
0
Transcript of SOG - Process Flow Template Word Version February 2010
-
8/3/2019 SOG - Process Flow Template Word Version February 2010
1/10
STANDARD OPERATING GUIDELINES
Roles and Responsibilities
ManagerThe Manager is responsible for providing technical guidance to and coordinating the workflow of your
Abilities Case Managers. They are your contact if you have issues with Claims Management, Speed
of Service etc.
Abilities Case Managers (ACM)The Abilities Case Manager is responsible for the initial absence assessment and for ongoing case
management of all STD/ LTD claims. The ACM is your contact for day to day claims inquiries and
case management planning.
Health Management Consultants (HMC)Our Abilities Case Managers (ACMs) assess every absence for rehab potential. Where rehab is
indicated, they engage one of our professional HMCs to identify and address non-medical
(psychosocial or workplace) issues that may be affecting recovery
The primary goal of our rehabilitation plans is to bring the plan member back to his or her own jobwhere feasible. This may require further treatment, re-conditioning or job accommodations such as
temporarily modified hours. If return to own work is not feasible, the Health Management Consultant
would consider alternate occupation planning.
Disability Payment and Eligibility Analyst (DPEA):
Responsible for LTD coverage eligibility review and management of routine claim related functions.Routine claim related functions include but are not limited to rehabilitation calculations, CPP
calculations and requesting updates on permanent or annual review claims.
-
8/3/2019 SOG - Process Flow Template Word Version February 2010
2/10
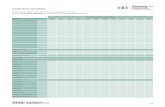
Absence record is set -up within 24 hourson Sun Lifes systems and forward to
ACM
ACM completes case managementabsence assessment in 5 business days
Plan Member , PlanSponsor advised of
absence assessmentconclusion
Plan Member ,Plan Sponsor
advised of
absence
assessmentconclusion
CaseManagement Plan
Developed
HealthManagement ?
Transition to LTD
Appeal,
if applicable
Health ManagementConsultants
Plan Sponsor sends Absence notificationpackage to Sun Life
Plan Member return to work and
absence file closed .
Yes
Sup
ported
No
Plan Sponsoraddresses
employmentstatus
Plan Sponsor /ACM sendTransition forms to Plan
Member and Plan Sponsor
completes their transitionform.
NotSupported
Plan Member /PlanSponsor advised of
additional informationrequired
InsufficientInformation
Yes
No
LTD Transition:
8 - 10 weeks before theend of the STD benefitperiod.
Where applicable , joint
action plan between ACMsto determine next steps for
transition.
Case Management Strategies include :
Frequent contact with Plan Member
to update recovery and potential for
return to work
Ongoing assessment for healthmanagement intervention
Other interventions such as IME ,FAE, Health Partners
EarlyRETURNS
Full Case Management
Process Map
Full Case Management isassessment through to resolution ,
resolution being :
Return to workor
Transition to a LTD claim
Absence assessmentconclusion
Ongoing Case
Management Strategies
Appeal Process
Employee notifies Plan Sponsorof illness
-
8/3/2019 SOG - Process Flow Template Word Version February 2010
3/10
Absence record is set-up within 24 hours
on Sun Lifes systems and forward to
ACM
ACM completes service provider express
absence assessment in 5 business days
Plan Sponsor sends
Service Provider Expressabsence notification package
to Sun Life
ACM engages correct network provider
ACM notifies Plan Sponsor and PlanMember of engaged network provider
ACM provides Plan Sponsor withrecommendations and appropriate next
steps through to conclusion
EarlyRETURNS
Service Provider Express
Process Map
Potential for ACM to remain involved and
assist with recommendations and next
steps
-
8/3/2019 SOG - Process Flow Template Word Version February 2010
4/10
Absence record is set-up within 24 hours
on Sun Lifes systems and forward to
ACM
ACM completes assessment for return towork potential in 5 business days
Plan Sponsor sends
Return to Work Advisory Services
absence notification packageto Sun Life
EarlyRETURNS
Return to Work Advisory Services
Process Map
ACM provides one time assessment of
medical and all information provided.
ACM to remain involved and assist with
recommendations and next steps
ACM provides Plan Sponsor withrecommendations which will include
appropriate steps to take in case
management
Employee notifies Plan Sponsor
of illness
-
8/3/2019 SOG - Process Flow Template Word Version February 2010
5/10
Absence record is set-up within 24 hours
on Sun Lifes systems and forward to
ACM
ACM completes assessment for chronic
casual absence in 5 business days
Plan Sponsor sends Chronic Casual
Absence Services notification packageto Sun Life
EarlyRETURNS
Chronic Casual Absence Services
Process Map
ACM provides Plan Sponsor with
recommendations and appropr iate nextsteps through to conclusion
Potential for ACM to remain involved and
assist with recommendations and next
steps
-
8/3/2019 SOG - Process Flow Template Word Version February 2010
6/10
STD Adjudication
Claim is set-up on Sun Lifes systemsand forwarded to ACM
ACM Adjudicates claim within 5 businessdays
ClaimDecision
Plan Member, PlanSponsor advised of
claim decision.
Plan Member,Plan Sponsor
advised of claimdecision.
CaseManagement Plan
Developed
HealthManagement
Services Requires?
Appeal?
Health
ManagementServices
Appeal Process
Completed Claim Package Received atSun Life
Yes
Ap
pro
ved
No
Plan Sponsoraddresses
employmentrelationship
Declined
Plan Member/Plan
Sponsor advised ofadditional information
required
IncompleteInformation
MemberRTW?
STD file closedYes
Yes
No
No
Case Management Strategiesmayinclude: Frequent contact with Plan Member
to update recovery and potential forreturn to work
Ongoing assessment for healthmanagement intervention
Other interventions such as IME,FAE, Health Partners
Ongoing Case
ManagementStrategies
Transition to
LTD?
STD ClaimResolved File
Closed
Return to WorkDeathNo Longer DisabledMaximum Age
STD to LTDTransition
No Yes
-
8/3/2019 SOG - Process Flow Template Word Version February 2010
7/10
LTD Adjudication
DPEA Assesses Contractual Eligibilityand forwards claim to ACM
ACM adjudicates claim within 10business days (LTD)
ClaimDecision
Plan Member, PlanSponsor advised of
claim decision.
Plan Member, PlanSponsor advised of
claim decision .
Health
ManagementServices Requires ?
Appeal?
Health ManagementServices
Appeal Process
Declined
Completed Claim Package Received atSun Life
Yes
No
App
rov
ed
No
Plan Sponsor addresses
employment relationship
Plan Member/Plan
Sponsor advised ofadditional information
required
IncompleteInformation
Claim Resolution
Ongoing case management
Decision letter will includenext steps in casemanagement
Assessment may include :Telephone interview with PlanMemberReview by Health PartnerDiscussion with Plan Sponsor
Resolution: Return to Work Settlement Age 65
Retirement
No longer totallydisabled
Death of Member Change of Definition
Ongoing Case Management strategiesmayinclude: Frequent contact with Plan Member to update
recovery and potential for return to workplanning.
Ongoing assessment for health managementservices
Pursue offsets where appropriate (CPP/QPP)
Non-litigated Settlements Strategic partnerships Change of Definition
Yes
-
8/3/2019 SOG - Process Flow Template Word Version February 2010
8/10
Health Management
ACM refers claim for HealthManagement Services
Referral to HealthManagementConsultant
Pre-clearance callto Plan Sponsor
Schedule Visit with
Plan Member/PlanSponsor/Physician
Health ManagementServices Appropriate ?
Visit outcome communicatedto Plan Member, Plan
Sponsor,Physician and ACM
HealthManagement
Plan Developed
Implement HealthManagement
Plan
Gradual Return to Work/Return to Work Plan
Developed in conjunctionwith Plan Sponsor, PlanMember and Physician
Return to work planmonitored by Sun Life and
Plan Sponsor, andadjusted as required
Return to Work
Ready?
Return to work full-time
Yes
Full-timeReturn toWork?
Return to work full-time
No
Yes
Ongoing casemanagementIntervention
Yes
No
Workplace issues identified Return to work barriers identified Potential for accommodation Preliminary joint planning
No
Return to WorkVocational AssistanceNon-Litigated Settlement
-
8/3/2019 SOG - Process Flow Template Word Version February 2010
9/10
Start
ACM decline or termination,
with right to object within
contractual appeal period
(contractual period)
Plan member objects*, with or
without new information
ACM considers, with any
argument/information
ACM declines appeal (maintains decision ),
advises in writing with reasoning , & right to
object within original contractual period . If appealis after contractual period , advise that time is up
& decision remains unless extension beyond
original contractual period is appropriate
No Plan Member Objection
Plan member objects, no new
information
Plan member objects, with
new information
ACM considersinformation
ACM decides wouldmaintain decision
ACM writes letter/EM advising that
objection being considered at 2nd
level or
appeal and sends referral to Manager
ACM approves claim
(changes decision ), advises
in writing, benefits paid
END
ACM approves claim,
advises in writing,
benefits paid
**Note: Any appeals that are received >1 year from the original date of decline /
termination letter must be referred to an
SDCC to consider the impact of
applicable limitation period
* All objects in
document should be readas objects in writing
Appeal Level #1 - ACM
Appeal Level #2 Manager
Manager ** declines appeal,
advises in writing with reasoning
& right to object (contractual
period no longer applies)
No Objection
Manager ** approves claim
and sends to ACM for
approval letter and ongoing
claims management
Plan member objects, no new
information
Plan member objects, with
new information
Manager decides would
maintain decision
Manager considers
information
Manager writes letter/EM advising thatobjection being sent to Senior Disability
Claims Consultant (SDCC), 3rd and final level
of appeal and sends referral to SDCC queue
END
Manager approves claim and
sends to ACM for approval
letter and ongoing claims
management
Appeal Level #3 SDCC
SDCC considers appeal
SDCC declines appeal,advises in writing with
reasoning
SDCC changes decision afterdiscussion with ACM/Manager, and
sends to ACM for approval letter andongoing claims management
Litigation Ombudsman No Objection END
* All Manager in
document should be readas Manager or
designate
Appeal Flowchart: Clients with contractual appeal wording
-
8/3/2019 SOG - Process Flow Template Word Version February 2010
10/10
Start
ACM decline or
termination, with
right to object
Plan member objects*, with or
without new information
ACM considers, with any
argument/information
ACM declines appeal(maintains decision ), advises
in writing with reasoning, &
right to object
No Plan Member Objection
Plan member objects, no new
information
Plan member objects, with
new information
ACM considers
information
ACM decides wouldmaintain decision
ACM writes letter/EM advising that
objection being considered at 2nd
level orappeal and sends referral to Manager
ACM approves claim
(changes decision ), advises
in writing, benefits paid
END
ACM approves claim,
advises in writing ,
benefits paid
**Note: Any appeals that are received >1 year from the original date of decline/
termination letter must be referred to anSDCC to consider the impact of
applicable limitation period
* All objects in
document should be read
as objects in writing
Appeal Level #1 - ACM
Appeal Level #2 Manager
Manager ** declinesappeal, advises in
writing with reasoning &
right to object
No Objection
Manager ** approves claimand sends to ACM for
approval letter and ongoing
claims management
Plan member objects, no new
information
Plan member objects, with
new information
Manager decides would
maintain decision
Manager considers
information
Manager writes letter/EM advising that objection
being sent to Senior Disability Claims Consultant
(SDCC), 3rd
and final level of appeal and sendsreferral to SDCC queue
END
Manager approves claim and
sends to ACM for approval
letter and ongoing claims
management
Appeal Level #3 SDCC
SDCC considers appeal
SDCC declines appeal,
advises in writing with
reasoning
SDCC changes decision after
discussion with ACM/Manager, and
sends to ACM for approval letter and
ongoing claims management
Litigation Ombudsman No Objection END
* All Manager in
document should be readas Manager or
designate
Appeal Flowchart: Clients without contractual appeal wording