Smoking Hypertension Cpd 2011 Art 2
-
Upload
muhammad-fauzi -
Category
Documents
-
view
214 -
download
2
description
Transcript of Smoking Hypertension Cpd 2011 Art 2
Current Pharmaceutical Design, 2011, 17, 2987-30012987
Smoking and Hypertension: Effects on Clinical, Biochemical and Pathological Variables Due to Isolated or Combined Action on Cardiovascular System
Linda Landini and Aurelio Leone*
Department of Internal Medicine, University of Pisa, Italy; *Fellow of the Royal Society for Promotion of Health, London, UK
Abstract: Changes in clinical, biochemical and pathological variables characterize cardiovascular damage from smoking and hyperten-sion when it acts independently. However, combined action of these major risk factors increases the rate of cardiovascular events. Ischaemic heart disease with stable effort angina, myocardial infarction and post-infarction arrhythmias may affect cardiovascular system because of smoking exposure. Among cerebrovascular disease, there is evidence that stroke would be related primarily to active smoking.
Isolated hypertension plays significantly major action to cause cerebrovascular disease including stroke, recurrent stoke and transient ischaemic attack. Among cardiac events, heart failure is, often, the end-point of hypertensive disease, even if manifestations of ischaemic heart disease similar to those caused by smoking may be increased in rate.
Combined action of smoking and hypertension usually increases the rate of cardiovascular complications and leads to a progression of atherosclerosis with narrowing and plaque primarily at the the level of coronary, carotid and cerebrovascular arteries. A pattern specific of both active and passive smoking exposure, but not hypertension, is the thromboangiitis obliterans that dramatically worsens in continu-ing smokers while it can be improved by stopping smoking.
Keywords: Smoking, hypertension, combined action, cardiovascular system.
INTRODUCTION
Smoking and hypertension are two major risk factors for car-diovascular disease [1].
Many reports identify cardiovascular system as one of the ma-jor target organs for smoking [2-12]. Both active and passive smok-ing damage the heart and blood vessels although pathological mechanisms may differ for type of action but not chemical toxics of which cause the alterations [13-30]. In addition, changes in blood pressure, whatever responsible cause there is, influence heavily cardiovascular function and structure [32].
No unanimous opinion exists on the relationship between smok-ing and hypertension with regard to their association in cardiovas-cular damage.
Some authors [33-34] support the hypothesis that there is only a limited association between hypertension and smoking while others [22-29] underline a strong association. Some others then [14,35,36] emphasize the role of smoking on the cardiovascular system either independently or by increasing the harmful effects of other risk fac-tors including hypertension. In addition, the age of smokers and duration of smoking habit could influence the blood pressure.
The purpose of this review is to describe clinical, biochemical and pathological effects of both smoking and hypertension as inde-pendent and combined risk factors for cardiovascular system.
SMOKING AND CARDIOVASCULAR SYSTEM
Commonly, smoking is the inhalation of the smoke of burning tobacco of cigarettes, pipes or cigars. However, epidemiological and statistical reports analyse primarily the effects of cigarette smoking.
Clinical, biochemical and pathological factors [36] interact to lead to a strong harm of cardiovascular system. In addition, they may be also a consequence of smoking exposure. Some body or-gans like lungs, heart and blood vessels, epithelial glands, and brain are a target of smoking toxics. Both active and passive smoking play a significant role to cause cardiovascular damage.
*Address correspondence to this author at the Via Provinciale 27, 19030 Castelnuovo Magra (SP), Italy: Tel/Fax: +390187 676346;E-mail: [email protected] Large population findings have demonstrated that the rate of cardiovascular disease in smokers statistically increased in absence of other major cardiovascular risk factors. Therefore, smoking may be considered as an independent risk factor for both cardiovascular disease and events, although the risk is closely dependent on several variables related to characteristics of smoking as well as individu-als health.
Adverse effects of tobacco smoke are the result of some chemi-cals usually concentrated and condensed into tobacco mixture, par-ticularly when the mixture is burning [23]. Of the more than 4,000 chemicals of burning tobacco, only a few participate actively to cardiovascular damage, since a large majority of them has carcino-genic effects. However, those chemical compounds able to damage heart and blood vessels have a high toxicity of either acute or chronic type. That, undoubtedly, increases the rate of morbidity and mortality for cardiovascular events. Deaths and disability due to cigarette smoking are currently and continuously reaching values that modify the concept of epidemiological transition just described in a review of this issue [37-38].
Worldwide, more than 3 million people [24-25] die each year for smoking, being half of them as old as fewer 70 years. In addi-tion, more than one third of current smokers meet partial or perma-nent disability, which is responsible for enormous costs to public health.
Both active and passive smoking have almost the same adverse effects on cardiovascular system, although they are differently dated in time and with a few different characteristics.
Tobacco Smoke Compounds
Three chemical compounds of smoking have been, for a long time, recognized able to damage cardiovascular system: nicotine and its metabolites, carbon monoxide and thiocyanate. However, there is an increased evidence [39-40] that ammonia, benzene and some carcinogens play an evident effect on changes in heart and blood vessels. Table 1 reports the main chemicals that may affect cardiovascular system as well as the other body structure involved.
Carcinogens act primarily throughout two mechanisms: exert-ing effects, which increase the damage induced by nicotine, and stimulating the action of carbon monoxide.
1381-6128/11 $58.00+.00 2011 Bentham Science Publishers2988 Current Pharmaceutical Design, 2011, Vol. 17, No. 28
Table 1. Tobacco Chemicals Damaging Cardiovascular System and Other Body Organs
ChemicalStructure
NicotineSympathetic system, Vascular bed,
Heart, Adrenergic system
Carbon monoxideArterial wall, Myocardium
ThiocyanateThyroid metabolism, Blood vessels
Myocardium
AmmoniaBlood vessels
2-naphtylamineBlood vessels
Benzo-anthraceneArterial wall, Myocardium
Benzo-pyreneArterial wall, Myocardium
Nicotine [41-42] is an alkaloid that constitutes approximately 0.63.0% of the dry weight of tobacco. Fresh leaves of nicotine have high toxicity in both animals and humans with specific effects involving insects and harvesters since nicotine biosynthesis occurs in the roots and leaves. In low concentrations (an average cigarette yields about 1 mg of absorbed nicotine), the substance exerts stimu-lant and addictive effects. According to the 1988, Surgeon Gen-eral's Report [43], cigarettes and other forms of tobacco are addict-ing; nicotine is the drug that causes addiction; pharmacological and behavioural characteristics that determine tobacco addiction are similar to those of heroin and cocaine.
Nicotine can be dosed in blood plasma or urine to confirm a diagnosis of poisoning or smoking exposure. Urinary or salivary cotinine, the main metabolite of nicotine, is frequently measured for the screening of smoking habit as well as for purposes of pre-employment and health insurance. In addition, a correct interpreta-tion of the results is important, since passive smoking exposure can also determine a significant accumulation of nicotine or its metabo-lites in various body fluids [44-45]. Nicotine, entered the blood, acts on the nicotinic acetylcholine receptor specifically the ganglion type nicotinic receptor and one CNS nicotinic receptor. The former is present particularly in the adrenal medulla, while the latter is pre-sent in the central nervous system (CNS). In small concentrations, nicotine increases the activity of these receptors. In addition, nico-tine has effects on a variety of other neurotransmitters closely stimulating those structures currently involved for the control of blood pressure and other functional heart parameters, primarily heart rate [46]. Indeed, there is evidence that nicotine has very powerful effects on arteries, raises blood pressure and is also a vasoconstrictor, which adversely influences heart pump function.
Finally, nicotine, after its stimulating effects, undergoes a phase of depression that can vary in the time for duration, but, usually, it is transient although prolonged.
Carbon monoxide is a gas quickly absorbed into the blood and, then, it reduces blood capacity to carry oxygen. Inhalation of car-bon monoxide has the same effects on active or passive smoking since the result depends on the concentrations reached by the gas into the blood [17]. Carbon monoxide toxicity is primarily due to the strongest bond with haemoglobin with production of carboxy-haemoglobin. The bond of haemoglobin with carbon monoxide is about 400 times stronger than that with the oxygen. In addition, the gas exerts a directly detrimental action on the heart and blood ves-sels by affecting heavily either myocardium or arterial wall at vari-ous levels including particularly coronary, carotid and cerebrovas-cular arteries. Blood concentrations of carboxyhaemoglobin are re- Landini and Leone
lated to carbon monoxide inhaled smoking cigarettes or that breathed from burned cigarettes into the environment.
The mechanism of carbon monoxide toxicity involves four stages [47]: removing oxygen from oxyhaemoglobin, bond between haemoglobin and the gas with lack to carrying out the oxygen, hy-poxia of body tissues and impairment of intracellular chains de-puted to respiratory metabolism. Thus, aerobic metabolism is heav-ily damaged with marked reduction or loss of functional responses of involved body structures [48-52].
The symptoms of toxicosis as well as the degree of organ dam-age depend primarily on the percent concentration of carboxyhae-moglobin into the blood.
Biochemical monitoring of carbon monoxide inhaled either from cigarette smoking or passive smoking exposure may be as-sessed by the dosage of blood carboxyhaemoglobin. However, the dosage of carbon monoxide coming from smoking is difficult to be established because of a large amount of carbon monoxide derived from industries, car fuel and other machineries acting as environ-mental pollutant.
Experimental findings [53] conducted on non-smoker individu-als exposed to passive smoking measured carboxyhaemoglobin lev-els before and after exposure. In addition, dosage of carboxyhae-moglobin can be made in an arterial or venous blood sample, al-though the estimated value cannot be totally attributed to cigarettes smoked. Usually, the concentration of carboxyhaemoglobin follow-ing acute exposure to passive smoking up to a carbon monoxide concentration 30-35 ppm/air increases from twice to four times the value detected before exposure [53].
Thiocyanate is the third smoking chemical able to induce car-diovascular damage, although with a lower power than that of nico-tine and carbon monoxide. Instead, thiocyanate increases the dam-aging effects of both those chemicals. Evidence indicates that active and passive smokers have a mean blood thiocyanate concentration 0.4 mcg/ml.
Thiocyanates are a group of chemical compounds that have toxic effects on several body organs [54-56]. They inhibit mito-chondrial ferricytochrome oxidase and other enzymatic chains and hence block electron transport. A reduced oxidative metabolism and oxygen utilization is the result of these mechanisms. Thus, there is an impairment of cellular respiratory chain with tissue hypoxia or worsening the degree of pre-existing hypoxia.
Burned tobacco commonly releases thiocyanates which increase their blood concentrations in individuals exposed to smoking.
There are some foods like milk, almonds, garlic, onion, leek, cabbage and cauliflower which contain thiocyanates. Such a fact makes hard to dose the exact amount of the thiocyanate produced by burned cigarettes in smokers. In addition, monitoring serum thiocyanate is more expensive than that of nicotine and cotinine currently used to assess smoking habit. However, thiocyanate causes cellular hypoxia, which strengthens that due to both carbon monoxide and nicotine.
Carcinogens have been recently identified chemical compounds able to damage cardiovascular system [36] because of a direct ac-tion on cellular components. However, their action on heart and blood vessels is poor when compared to the damage of respiratory system and other body organs.
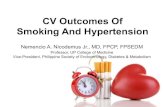
In conclusion, the toxic effects of tobacco smoke compounds are primarily due to carbon monoxide and nicotine, whereas the other chemicals exert same effects of very limited power. Fig. (1) shows the percent importance of the different tobacco chemicals involved in cardiovascular damage according to their power, as re-ported by the literature on the subject.
In addition, it is worthy noting that carbon monoxide always causes a morphological damage that leads, in time, to irreversibleSmoking and HypertensionCurrent Pharmaceutical Design, 2011, Vol. 17, No. 28 2989
Carbon Monoxide
97%
Nicotine
95%
Thiocyanate
45%
Carcinogens
8%
100%
Fig. (1). Smoking chemicals primarily involved in cardiovascular damage. Carbon monoxide, the most dangerous chemical of smoking, exerts both a direct action on cardiovascular system and adverse effects on some cardiovascular parameters. It is closely followed by nicotine.
lesions of cardiovascular system as well as the appearance of non-fatal and fatal cardiovascular and cerebrovascular events.
Clinical Variables
The analysis of the data provided mainly by observational study allows identifying some clinical patterns specifically related to cigarette smoking.
Clinical damage involves primarily those individuals who have other major cardiovascular risk factors associated with cigarette smoking. Among these factors, high LDL-Cholesterol concentra-tions and hypertension play a strong role. Symptoms related to an-gina pectoris, myocardial infarction, arrhythmias, stroke or recur-rent stroke occur with higher rate [10-16, 26, 57-61]. Table 2 shows the main clinical patterns related directly or mediated by other func-tional or pathologic parameters to cigarette smoking.
Clinical damage is often associated with other types of damage caused by smoking exposure including functional and pathological manifestations. In addition, clinical damage may worsen an under-lying cardiovascular disease.
Some characteristics can identify the damage caused by ciga-rette smoking.
Coronary heart disease associated with clinical symptoms may be the result of a large number of pathologic factors including in-creased blood carboxyhaemoglobin, diminished oxygen transport, enhanced platelet adhesiveness and aggregation, and impaired car-diac performance. These factors, primarily due to a combined ac-tion of carbon monoxide and nicotine, exacerbate, in the long end, the atherosclerotic process [62]. Effort angina often accompanies both smokers and non-smokers exposed to passive smoking [8]. A clear worsening of clinical manifestations and appearance of chest pain during exercise at a lower threshold level may, usually, be seen. Authors analysed the performance to exercise of 10 men with stable effort angina. The men underwent exposure to environmental tobacco smoke twice: in a smoke-free environment and in an envi-ronment polluted by carbon monoxide. Exposure to passive smok-ing induced an increase in heart rate, blood pressure, and carboxy-haemoglobin concentrations and a statistically significant decrease of threshold angina equal to 22% during smoking exercise. Im-paired cardiac performance in both healthy and subjects suffering from pre-existing myocardial infarction was also documented dur-ing passive smoke exposure by Leone et al [53]. Nine healthy sub-jects and 10 with a previous myocardial infarction, who were tested and controlled, performed the same exercise on a bicycle ergometer twice: in a smoke-free environment and, then, in the same environ-ment polluted by 30 to 35 ppm/air carbon monoxide arising from burning cigarettes. Analysed parameters of the study were the peak of exercise power, time to recovery of pre-exercise heart rate, Table 2. Main Clinical Patterns in Active and Passive Smokers
1. Active smokersIschaemic heart disease
- Effort angina
- Myocardial infarction
- Recurrent infarction
- Arrhythmias
- Sudden cardiac death (?)
Cerebrovascular disease
- Transient ischaemic attack
- Stroke
- Recurrent stroke
- Cerebral artery lesions
Hypertension
Atherosclerosis
Systemic artery disease
- Aortic aneurysms
- Burger disease2. Passive smokersIschaemic heart disease
- Impaired cardiac performance
- Effort angina worsening
- Postinfarction arrhythmias
Cerebrovascular disease
Hypertension
Atherosclerosis
Peripheral artery disease progres-
sion
carboxyhaemoglobin level, and level of expired carbon monoxide. In a smoking environment, healthy subjects showed a statistically prolonged time to recovery of pre-exercise heart rate and increased carboxyhaemoglobin concentrations, while the subjects with a pre-vious myocardial infarction had all studied parameters heavily im-paired. In addition, individuals with pre-existing myocardial infarc-tion documented ventricular arrhythmias, which needed to stop ex-ercise in some of them [10]. Pimm et al [63] analysed twice the re-sponse to exercise of 20 healthy young men and women in a free-smoking environment and in an environment polluted by carbon2990 Current Pharmaceutical Design, 2011, Vol. 17, No. 28
monoxide at a concentration of 24 ppm/air. Exercise on a bicycle ergometer lasted 7 minutes. In a smoking environment, there was a significant increase in carboxyhaemoglobin not associated with other functional disorders of cardiovascular system. Finally, McMurray et al. [64] reported that the exercise of eight healthy in-dividuals, 4 smokers and 4 non-smokers, reduced its duration in passive smoke environment. Finally, other two studies [65-66] ana-lysed the exercise tolerance of individuals with a history of ischae-mic heart disease. Both these findings documented appearance of clinical signs of myocardial ischaemia and ventricular arrhythmias when carbon monoxide concentration was elevated in the exercise environment.
There is evidence that the effects of smoking compounds on cardiovascular system may be better identified by experimental studies conducted in passive smoking exposure since, clinically, they allow to establish those changes of analysed parameters due to the concentrations of carbon monoxide in the environment where the experiment is performed. Indeed, it is very difficult to attribute clinical symptoms of smoker or non-smoker individuals passively exposed to smoking since the symptoms that characterize ischaemic heart disease are similar to both groups as well as in never smokers. However, a significant impairment of the signs of myocardial ischaemia was, undoubtedly, documented by experimental findings.
The characteristics of sudden cardiac death need some consid-erations. Clinically, life-threatening ventricular arrhythmias as well as sympathetic or adrenergic stimulation, mainly due to the action of nicotine, play primarily a pathogenic role which determine func-tional responses. [67-68]. A direct cause-effect relationship between smoking and sudden cardiac death has not been clearly docu-mented, and the observations that hypothesize smoking as a risk factor for sudden cardiac death are explained by statistical estimates that analyse, indirectly, the phenomenon.
Epidemiologically, cerebrovascular disease ranks with the third all-cause mortality and morbidity in civilized countries following age and hypertension [69-70]. However, the relationship between clinical patterns of cerebrovascular disease including stroke, recur-rent stroke and transient ischaemic attack, and smoking is yet under debate since existing opinions draw away from each to other. Gen-erally, hypertension is the first factor which increases the risk of both ischaemic and haemorrhagic stroke, while cigarette smoking would act only in active smokers after lifetime exposure [71]. In addition, there would be evidence that passive smoking is not strongly associated with cerebrovascular disease. No association between passive smoking and cerebrovascular disease including stroke was found in five case-control, cross-sectional and cohort-studies [60, 72-75]. In contrast, the study of Bonita et al. [58] showed a significant association between home passive smoking and acute stroke in both male and female sexes. Moreover, there is scientific evidence that Bonita et al. study is an excellent finding that carefully analyses important variables related to cardiovascular risk since it follows the diagnostic criteria of stroke defined by the WHO [76]. Finally, it is worth noting that stroke of smokers is, usually, an ischaemic rather than a haemorrhagic stroke because the compounds of tobacco smoke primarily have a thrombotic mecha-nism, increasing platelet adhesiveness and aggregation.
Systemic artery disease shows, clinically, symptoms and char-acteristics of atherosclerosis progression [77] particularly at carotid artery site. However, clinical symptoms depend on the arterial tree compromised and, usually, are similar to those related to other fac-tors, unless Burger disease (thromboangiitis obliterans) [78], where claudication may be reduced by stopping smoking. In contrast, con-tinuing smokers may develop gangrene followed by leg amputation that concludes the spontaneous history of the disease. Observations reported the appearance of Burger disease in never smokers and that was probably due to passive smoking exposure [79-80]. Landini and Leone
There is an axiom of five words that undoubtedly underlines how clinical claudication may be improved stop smoking and keep walking [81].
Biochemical Variables
Cardiovascular alterations due to smoking depend on the effects of some smoking compounds or, alternatively, they may be the re-sults of changes in haematological parameters related to the degree of atherosclerosis progression.
Among involved parameters (Table 3), some are related to atherogenic and thrombogenic risk such as increased LDL-cholesterol, low-density lipoproteins, triglycerides, total with, red, and platelet blood cell count, hematocrit, prothrombine time, partial thromboplastin time, and fibrinogen. Some others depend on patho-logical changes of myocardial cell components such as mitochon-dria, enzyme chains, intracellular bodies, and cellular receptors [29].
Table 3. Biochemical Markers Involved in Cardiovascular Damage from Smoking
Parameters InvolvedBiological Variables
Thrombogenesis/thrombosisChanges in platelet function
Changes in platelet shape
Coagulation-fibrinolysis changes
Arterial wallEndothelial dysfunction
Arterial stiffness
Haematological parametersChanges in blood cell count
Changes in blood cell shape
Increased C-reactive protein
Changes in blood viscosity
Metabolic parametersChanges in lipid metabolism
Changes in glucose metabolism
Increased catecholamine release
Decreased estrogen levels
Oxidative stress
Immunological responsesAlterations in T-cell function
Reduced immune response
Susceptibility to infections
Platelet response and survival are adversely affected primarily by chronic smoke although there is evidence that while a subject smokes actively cigarettes, platelet adhesiveness and aggregation increase acutely [82]. Endothelial dysfunction strongly influences such a condition. Usually, normal endothelium is a non-reactive structure with the constituents of circulating blood and it responds to stimuli by a vasodilator mechanism primarily due to nitric oxide. When endothelial surface is denudated or covered by prosthetic ma-terial, the coagulation-fibrinolysis cascade is activated by an ele-vated production of fibrinogen and thrombogenic factors including factor VII, that contribute to non-occluding or occluding thrombi formation. There is clear evidence that current smokers [83-85] have higher fibrinogen levels related with the number of cigarettesSmoking and Hypertension
smoked. In addition, past smokers have fibrinogen levels similar to those of non-smokers.
Endothelial dysfunction has been shown [19, 86-87] in both healthy and ischaemic individuals.
Other haematolgical factors contribute to trigger atherosclerotic process. Plasma viscosity interferes with red cell deformability, while plasminogen, which contributes to the lysis of fresh thrombi, reduces its concentration during exposure to cigarette smoke. Fi-brinogen and factor VII are currently independent risk factors for coronary artery disease and stroke [83, 88].
Tobacco smoke adversely influences several metabolic steps of lipid and glucose metabolism with changes in concentration of those substances actively involved in the protection or progression of atherosclerotic process. Results showed that repeated measure-ments of blood lipid concentrations in both active and passive smokers identified primarily LDL-Cholesterol and triglycerides in-crease and HDL-cholesterol decrease [89-92].
There are always newer data on the relationship between glu-cose metabolism and tobacco smoke. Smoking is an independent, modifiable risk factor for non-insulin dependent diabetes mellitus [93]. Findings on individuals exposed to active and passive smok-ing showed that smoking was associated with an increased risk of developing glucose intolerance [94-98]. In addition, individuals passively exposed to smoke had an intermediated risk of developing glucose intolerance [98]. The degree of risk was similar to that of past smokers after their quitting smoke.
Insulin resistance syndrome, which consists of a large number of metabolic disorders affecting blood pressure, body weight, changes in lipid and glucose metabolism and, primarily, high blood insulin levels, is now recognized to be a risk factors for heart dis-ease [99-100]. Findings [100-101] showed that smoking exposure could increase insulin resistance particularly in women, although another report did not support similar statement [102].
Cigarette smoking enhances the release of plasma catechola-mine, inhibits cyclo-oxygenase- prostacyclin related, and increases thromboxane byosynthesis [103]. Prostacyclin is a potent inhibitor of platelet aggregation [104] while thromboxane is a potent vaso-constrictor and platelet agonist. Therefore, increased catecholamine release acts either enhancing platelet aggregation or stimulating sympathetic nervous system. Both these factors are able to induce arterial lumen narrowing for a progression of atherosclerotic proc-ess via thrombus formation.
In this context, some considerations need oxidative stress. Ciga-rette smoking contains a large amount of oxidants and evidence suggests that oxidative stress is involved in the pathogenesis of many cardiovascular diseases [105-108]. Oxidative stress is the re-sult of an imbalance between the production of reactive chemicals, including reactive oxygen and nitrogen chemicals, with damaging effects and biological systems deputed to readily detoxify the reac-tive intermediates in an attempt to easily repair the resulting dam-age. Reactive chemicals are, usually, smallest molecules with a sig-nificantly high reactivity. They play a strong role on cellular me-tabolism through specific modifications of cell signalling protein [109] which leads to the activation of pathways that control cell proliferation, hypertrophy, hypoxia and apoptosis [110]. By these processes, antioxidant substances are inhibited and, then, cellular damage progresses.
Finally, cigarette smoking may induce alterations in immune function [111] influencing negatively T-cell activity and antibody response. Inflammatory haematological markers can modify their values in smokers with a major susceptibility to infections and manifestations of increased plasma viscosity. Indeed, there is evi-dence that heavy smokers suffer frequently from chronic bronchitis with recurrent exacerbation and altered immunological responses. In addition, increased levels of C reactive-protein, documented in heavy smokers, are an indicator of activated immune system and Current Pharmaceutical Design, 2011, Vol. 17, No. 28 2991
inflammation, which, undoubtedly, favour atherosclerosis progres-sion and occurrence of heart attacks.
Pathological Variables
Pathological alterations of heart and blood vessels caused by cigarette smoking are similar qualitatively in both active and pas-sive smokers, although active smokers, usually, absorb major con-centrations of toxic compounds. In addition, structural alterations caused by smoking are similar to those of other cardiovascular events able to cause the same disease, unless for some ultra-structural manifestations, which seem to be typical lesions from smoking. However, differences exist primarily for the site and size of the alterations induced by smoking as well as for the choice of some cardiovascular structures instead of others. Generally, at the beginning of exposure, there is evidence that active smoking causes mainly pathological alterations related to cardiac and cerebrovascu-lar complications while passive smoking induces functional disor-ders [12, 31,112]. Table 4 lists the main manifestations of cardio-vascular pathology due to both active and passive smoking accord-ing to their type and related incidence.
The major observations on the morphological alterations of car-diovascular system due to both active and passive smoking expo-sure [22, 29-31, 113] are coming from experimental findings con-ducted on animals exposed to smoking or carbon monoxide alone [30, 52, 114-116]. The ultrastructural analysis of the damage identi-fies undoubtedly that carbon monoxide is the main factor of both myocardium and artery lesions. The damage, however, may be a consequence of either coronary circulation changes or a direct ef-fect of carbon monoxide on cardiovascular system without any im-pairment in coronary circulation. In addition, nicotine supports hy-poxic mechanisms of damage, which aggravates the effects of car-bon monoxide at cellular level.
Myocardial necrosis and, particularly, its type-because there are different patterns of necrosis- is the main pathological manifesta-tion to be discussed. Necrosis may be well defined the result of those morphological changes, which follow cell death in a living tissue or organ with partial or total loss in their function. All in-farcts of the myocardium belong to the group of necrotic lesions, although not all cardiac necroses are necessarily infarcts. The ne-crosis of an infarct recognises a coronarogenic mechanism with coronary vessel narrowing or occlusion, while some necroses, mor-phologically, affect directly myocardium with no coronary artery involvement. Smoking exposure may cause the development of both types of necrosis: necrosis supported by a coronarogenic mechanisms and non-coronarogenic necrosis. Sometimes, both ne-croses may be associated with markedly morphological damage of myocardial cells. Fig. (2) schematizes the main mechanisms which support the different types of necrosis.
Microscopic alterations due to vascular mechanism follow steps characterised by cellular lysis, fragmentation of cardiocytes and disappearance of nuclei. Contract band formation, polimorphonu-clear infiltrates and, then, formation of a granulation tissue, that will evolve in a firm scar completing the healing process, usually ac-company myocardial lesions . Coronary arteries usually show vari-ous degree of narrowing, partial or complete occlusion due to old thrombi, superimposed fresh thrombi, atherosclerotic plaque rup-ture with, sometimes, distal embolisation. Coronary wall may con-tain calcium deposits. When non-coronarogenic mechanism causes myocardial cell death, coronary alterations may be totally absent or supported by minimal lumen narrowing.
A pathologic pattern specifically attributed to smoking action is the smoke cardiomyopathy[114-115]. The term cardiomyopathy is currently used to describe all those degenerative lesions of the myocardium caused directly by toxic or metabolic substances and, indirectly, by changes in oxygen availability with chronic hypoxia. Therefore, smoke cardiomyopathy does not present typically coronarogenic necrotic manifestations, but, instead, altered function2992 Current Pharmaceutical Design, 2011, Vol. 17, No. 28
Landini and Leone
Table 4. Cardiovascular Pathology Related to Smoking Exposure
Cardiovascular Events
Active SmokingPassive Smoking
Coronary artery disease
++++++
Stable angina
++++++
Vasospasm angina
+++
Myocardial infarction
++++++
Arrhythmias
+++++
Experimental cardiomyopathy
+++
Sudden cardiac death
++ (?)
Cerebrovascular disease
+++++
Stroke
++++
Recurrent stroke
+++++
Transient ischaemic attack
+++++
Peripheral artery disease
+++++
Thromboangiitis obliterans
+++++
Symbols: +++ = elevated rate; ++ = moderate rate; ++ = mild rate; + (?) = uncertain rate.
Fig. (2). Main pathological mechanisms of myocardial necrosis. There is evidence that myocardial necrosis may be caused by a coronarogenic mechanism involving coronary circulation as well as by a toxic mechanism without or with coronary circulation involvement.
and morphology of those intracellular components primarily in-volved in carrying out metabolic and respiratory pathways. Experi-mental studies [117-120] show that a wide number of factors can cause alterations in myocardial cells. These alterations morphologi-cally consist of myolysis, non-ischaemic necrosis, hyalinosis, and inflammatory foci. Calcifications and fibrosis, particularly intersti-tial fibrosis, often develop in the context of the lesions. Smoking compounds, primarily carbon, monoxide induce, experimentally, all these alterations associated with the presence of perivascular haem-orrhagic infiltrates, which are specific manifestations of smoke car-diomyopathy [30]. Table 5 summarizes the main morpho-patho-logical patterns of smoke cardiomyopathy. Haemorrhagic foci into the context of necrotic area need some explanations since they are a typical pattern of smoke cardiomyopa-thy. Haemorrhagic foci are necrotic zones of myofilaments in the context of which isolated or confluent punctuate microhaemor-rhages give a typical microscopic aspect. These alterations are the result of carbon monoxide toxicity since they are strongly associ-ated with gas poisoning in a quantity much more extended than those of cigarette smoking. Carbon monoxide causes these altera-tions because of its link with haemoglobin [121-124]. Oxygen availability to the myocardium is reduced up to a degree which strictly depends on blood carboxyhaemoglobin concentrations. InSmoking and Hypertension
Table 5. Morpho-pathological Patterns of Experimental SmokeCardiomyopathy
Pathological FeatureMain Characteristics
MyocytolysisColliquative degeneration of cardiocytes
Intracellular oedema
Nuclear alterations
Vacuolisation
Vascular damagePerivascular infiltrates
Small artery wall inflammation
HyalinosisHomogeneous glassy deposits in myocardium
Homogeneous glassy deposits in arterial wall
InflammationInflammatory cell infiltrates
Cardiocyte necrosis
Haemorrhagic fociPerivascular and interstitial foci
Punctate haemorrhage into myocardium
FibrosisPerivascular fibrosis
Interstitial fibrosis
Calcium depositArterial wall and myocardium
Atheroma of advanced atherosclerosis
addition, myocardial infarction in individuals with normal coronary arteries may be caused by this mechanism as an interesting paper shows [124].
Figures (3) and (4) show same ultrastructural patterns of ex-perimental smoke cardiomyopathy.
The analysis of these observations shows that severe morpho-patholgical changes in coronary circulation and myocardial cells may be seen, either when they are isolated or differently combined among themselves. That may cause a large spectrum of pathologi-cal features, which lead to impairment or aggravate both pre-existing myocardial function and structure.
The pathologic changes in cerebrovascular circulation are simi-lar of coronary circulation even if they are primarily related to ac-tive smoking. Smoking damages cerebral circulation by two main mechanisms often associated (Table 6). They cause morphopa-tological alterations of ischaemic or haemorrhagic type. Usually ischaemic lesions occur with higher rate since they are well related to atherosclerosis progression or thrombosis, while haemorrhagic alterations are a consequence of artery wall rupture mainly due to severe o malignant hypertension in elderly.
Cerebral arteries usually show narrowing of different degree with, sometimes, intimal rupture and non-occlusive or occlusive superimposed thrombi. Figs. (5) and (6) are an example of two types of morphopathological alterations of cerebral arteries.
Findings demonstrate that thickness in carotid artery wall deeply influences the morphology of cerebrovascular circulation. Indeed, smoking is a strong risk factor for carotid wall thickening [59, 75].
The effect of smoking on arterial stiffness needs some observa-tions since changes in artery distensibility adversely influence both haemodynamic and structural responses of cardiovascular function. Current Pharmaceutical Design, 2011, Vol. 17, No. 28 2993
Fig. (3). Smoke cardiomyopathy: microhaemorrhagic interstitial infiltrates (white line) and severe alterations in myocardial fibers. Isolated and conflu-ent areas of interstitial fibrosis may be seen.
Fig. (4). Smoke cardiomyopathy. Presence of contract bands as a result of coagulative necrosis.
Fig. (5). Anterior cerebral artery with mild intimal thickness and moderate lipid subintimal circular deposits (our autopsy observation).
Stefanidis et al. [125] investigated aortic elasticity in male patients most of whom had coronary ischaemic disease. Exposure to passive smoking significantly reduced aortic distensibility with increased left ventricular afterload and worsening in myocardial function.2994 Current Pharmaceutical Design, 2011, Vol. 17, No. 28
Fig. (6). Anterior cerebral artery. There is evidence of narrowing caused by an eccentric thrombus, which is partly calcified, and fragmentation of elastic fibers (our autopsy observation).
Table 6. Morphopathological Alterations of Cerebrovascular Disease Caused by Smoking Exposure.
MechanismMorphopathologyCerebral Disease
AtherosclerosisCerebral artery nar-Transient ischaemic attack
rowing
Ischaemic stroke
Recurrent ischaemic
stroke
Cerebral atrophy
ThrombosisCerebral artery occlu-Ischaemic stroke
sion
Recurrent ischaemic
stroke
HaemorrhageWall artery ruptureHaemorrhagic stroke
Impairment or loss in arterial elasticity actively induce atheroscle-rotic lesions similarly to other damaging mechanisms related to smoking.
Morphopathological alterations in systemic arteries are, usually, those of atherosclerotic lesion, unless thromboangiitis obliterans [78] where inflammatory elements are prevailing. Indeed, throm-boangiitis obliterans is an arteriopathy from cigarette smoking.
In conclusion, there is no doubt that both active and passive smoking cause severe clinical, biochemical and pathological altera-tions of cardiovascular system. These alterations are the result of the combined harmful effects of tobacco smoke compounds, pri-marily nicotine and carbon monoxide. However, the latter undoubt-edly has a greater role in inducing morphopathological lesions by a double mechanism of action: a direct effect on myocardium and arterial wall because of its toxicity, and an effect mediated by car-boxyhaemoglobin with reduced oxygen availability. Therefore, ex-posure to smoking is a strong risk for both healthy and individuals with pre-existing cardiovascular disease. American Heart Associa- Landini and Leone
tion, as the excellent paper of Glantz and Parmley emphasizes [14], included also passive smoking among the major risk factors for heart disease in both adults and children. In addition, evidence indi-cates that a strong relationship links smoking with arterial hyperten-sion.
HYPERTENSION AND CARDIOVASCULAR SYSTEM
Hypertension is one of the major modifiable risk factors for coronary, cerebrovascular and other vascular diseases since numer-ous drugs are able to reduce both systolic and diastolic blood pres-sure values. However, despite large-scale approaches to diagnose, treat and educate lifestyle of hypertensive patients, the impact of hypertension control is strongly discouraging [126] either for the scarce attention of the patients with regard to their blood pressure or for poor results related to treatment. In addition, there is evidence that the early stages of hypertension are asymptomatic, and such a fact contributes, usually, to identify hypertensive patients for an occasional clinical control or for dated vascular complications. Therefore, clinical and pathological variables of hypertensive dis-ease are mainly related to the cardiovascular complications, despite the fact that some data on an existing hypertension could be de-duced by measurements of some biochemical parameters, which are, however, many expensive and, then, not fully estimated by large-scale methods. However, hypertensive patients need a careful control particularly after a diagnosis of hypertension in an attempt to assess whether they meet lowering in blood pressure during ther-apy or, on the contrary, appearance of target organ damage.
Clinical Variables
Initial clinical symptoms of hypertension are of difficult as-sessment either for the different lifestyle of groups of population or for the characteristics of elevated blood pressure [127-132]. On the contrary, the symptoms related to complications of hypertension may be easily identified and, therefore, talking of hypertensive vas-cular disease would be more correct.
Three types of symptoms, usually, carry hypertensive patients to the physician (Table 7): symptoms related to elevated blood pressure, symptoms associated with target organ damage and symp-toms of an underlying disease in presence of secondary hyperten-sion. However, the large majority of individuals with early hyper-tension have no clinical symptoms and signs or, at a maximum, a merely cardiac enlargement when compensated hypertension exists.
Table 7. Symptoms and Signs of Hypertensive Patients.
Symptom CategoriesClinical Signs
1.Symptoms related to high blood pressureMorning headache
Dizziness
Walking fatigue
Others (aspecific)
2.Symptoms associated to target organ dam-Epistaxisage
Hematuria
Blurring vision
Chest pain
Dyspnoea
3.Symptoms related to underlying diseaseThose of underlying
disease
Smoking and Hypertension
Other signs that can help to assess hypertension are a family history of elevated blood pressure or vascular disease and appear-ance of newer symptoms related to ischaemic heart disease, heart failure, cerebrovascular troubles and peripheral vascular insuffi-ciency.
These data put in evidence that it is necessary addressing the attention on the heart, neurological system and kidney in an attempt to deduce retrospectively whether a patient had been affected by early hypertension. On the contrary, long-standing hypertension records rapidly symptoms of target organ involvement. A clinical syndrome which requires a careful control is hypertensive encepha-lopathy [133-135]. Hypertensive encephalopathy is a neurological dysfunction induced by malignant hypertension. It is a cerebral condition, typically reversible, caused by sudden and sustained severe elevation of blood pressure. It occurs in eclampsia, acute nephritis and hypertensive crises. Clinical symptoms consist of a complex of alterations characterized by severe hypertension, altered consciousness, increased intracranial pressure with sickness and vomiting, retinopathy with papilledema, and seizures. The patho-genesis of hypertensive encephalopathy is yet under discussion and doubts have been hypothesized on a possible vascular mechanism. The syndrome may be accompanied to focal or massive haemorr-hagic cerebral infarct, and there is no common opinion that it could be controlled by a rapid lowering of blood pressure.
Baseline electrocardiography and echocardiography constitute a valid support to assess clinical manifestations of hypertension.
The described signs may lead to a diagnosis of hypertension, which, however, may be easily documented whether the physicians control routinely blood pressure in their patients every time during a medical exam.
Biochemical Variables
Biochemical variables which may provide details on the mechanisms and prognostic significance of hypertension belong to two main categories: biochemical evaluation of routine blood sam-ples and specific biochemical substances related to pathogenetic mechanisms of hypertension.
Together with clinical exam, assessing biochemical variables is a useful support in an attempt to establish those markers of known causes of hypertension, to stratify hypertensive individuals with regard to their age, sex and race, and, then, to define the true risk profile of an individual towards hypertension. In addition, novel markers associated with hypertensive heart disease and heart failure from hypertension should be monitored [136-138]. Table 8 summa-rizes the main biochemical markers to assess for a correct interpre-tation of different types of hypertension.
These markers allow a more correct approach to interpret, treat and identify the type of hypertension.
Among the biochemical markers related to routine control, complete blood count with hematocrit, glucose and lipid profile are also involved in the damage caused by cigarette smoking [82-84, 88-102]. On the contrary, other markers are specific for assessing the role of elevated blood pressure. Plasma renin primarily feels changes in sodium balance [139-141]. Plasma renin activity may screen high blood pressure of kidney origin as well as allow plan-ning the treatment of essential hypertension often aggravated by excess sodium intake. In addition, plasma renin activity helps to evaluate the diagnosis of excess aldosterone.
Enhanced plasma renin activity probably contributes to early phase of hypertension, although there would be evidence that it mainly related to the development of severe hypertension. Contro-versies, however, exist on this hypothesis.
The measures of renin-sodium profile associated with the as-sessment of plasma potassium, serum urea and creatinine, 4-hr Current Pharmaceutical Design, 2011, Vol. 17, No. 28 2995
Table 8. Biochemical Markers in Hypertension.
VariablesBiochemical Markers
1. Variables related to routine con-Complete blood count with he-trolmatocrit
Urine analysis
Blood urea nitrogen
Serum creatinine
Serum uric acid
Fasting blood sugar
Lipid profile
Serum electrolytes
2. Variables related to specific pat-Plasma reninterns
Plasma and urinary catechola-
mine
Urinary free cortisol
Urinary 17-
hydroxycorticosteroids
Urinary aldosterone
3. Novel biochemical substancesPlasma CT-1
Annexin A5
microalbuminuria excretion rate and 24-hr urinary sodium and po-tassium values are useful biochemical markers to identify either secondary causes of hypertension or the pathophysiologic profile of the patients. In addition, they may be predictors of vascular disease or benign essential hypertension [142-143].
Biochemical markers of lipid and glucose profile address to the same considerations described for the action of smoking com-pounds. These markers may be elevated in several forms of secon-dary hypertension, like Cushings syndrome and pheochromocy-toma that are associated with hyperglycaemia and changes in hor-mone release respectively corticosteroids and catecholamine [144-145]. A reduction in lipid concentration can be a factor improving blood pressure, even if doubts have been raised more recently [146-147]. It would seem that biochemical variables of hypertension and smoking are walking on two parallel ways with a meeting point when the damage caused by each of them reaches its maximum de-gree.
The markers specifically related to structural components of the heart are pathological substances, which provide important data on the outcome of both hypertensive disease and target organ damage. Among these markers, Cardiotrophin-1 (CT-1), belonging to inter-leukin-6 family, and Annexin A5 have been, primarily, measured in hypertensive patients. These biochemical compounds exert their action on the same tissues, like heart muscle, also target organ of smoking compounds.
CT-1 is produced by cardiocytes and cardiac fibroblasts in case of functional or mechanical stress [148]. Increased concentration of CT-1 has been documented in hypertensive patients particularly with left ventricular hypertrophy as well as in those patients devel-oping heart failure with a higher concentration than that of subjects2996Current Pharmaceutical Design, 2011, Vol. 17, No. 28
with left ventricular hypertrophy but not heart failure [149-151]. Therefore, there would be evidence that CT-1 may be a biochemical marker, which allows following the progression of hypertensive disease and the involvement of cardiac muscle.
Annexin A5 is a protein involved in cardiomyocyte apoptosis [152-153]. Its increase in concentration occurs experimentally or clinically in either hypertensive animals or patients developing left ventricular hypertrophy and, particularly, heart failure. Available data suggest that plasma Annexin A5 in hypertensive patients would be an effective biochemical marker of apoptosis-related car-diomyocyte dysfunction and, by this way, it may contribute to in-terpret both hypertension course and target organ involvement in-cluding specifically heart involvement.
Finally, collecting data demonstrate that biochemical markers of hypertension are continuously in progress and, moreover, novel markers would be related to manifestations of cardiovascular dam-age which is very similar to that due to smoking exposure.
Pathological Variables
Pathological variables of hypertension include a great number of morphological alterations which are well dated and known. This statement is true in its context when hypertensive vascular disease is analysed namely and the complications of hypertension display target organ damage. Indeed, early hypertension, usually clinically and metabolically asymptomatic, does not show pathological altera-tions of high degree.
Pathological alterations of early hypertension consist, the most, of a moderate cardiac enlargement with mild or no hypertrophy and a few changes of arteriosclerotic type in small arteries due to vaso-constriction of peripheral circulation. These alterations would be a consequence of increased afterload caused by elevated blood pres-sure or, probably, they pre-exist to hypertension according to the results of some studies [154]. Isolated areas of fibrosis also may be seen in several organs like heart and kidney with, however, no change in shape and gross morphology of them.
A wide spectrum of pathological alterations characterizes com-plicated hypertension to the macroscopic or histological exam. Some cases, undergone autopsy in our observations, showed a dif-ferent degree of target organ damage as Figs. (7-10) and (11) clearly show. The subjects died for a cardiac event complicating the hypertension. However, vascular alterations affecting the arteries of the other target organs are quite similar to coronary alterations, un-less for the brain where rupture of the wall of cerebral arteries associated with haemorrhagic stroke may be seen. Landini and Leone
Fig. (8). Post-mortem study of the heart in a patient with essential hyperten-sion. A moderate cardiac hypertrophy may be seen. The heart was examined by the technique of Roussy and Ameuille [158]. By this method, the heart is cut in transverse slices of thickness approximately 1 cm, parallel to each other. Myocardial alterations may be recorded and, then, measured by the analysis of the photograph.
Fig. (9). Minimal changes in the arterial wall due to hypertension.
Fig. (7). Rupture of the heart following an acute myocardial infarct in a pa-tient with severe hypertension. There is evidence of rupture of the free wall of the left ventricle into the area of infarct and severe hypertrophy of the heart. Hypertensive subjects with myocardial infarct and cardiac hypertro-phy undergo frequently postinfarction cardiac rupture [155-157].
Fig. (10). Changes in arterial wall due to hypertension. There is moderate narrowing and increased thickness of the arterial wall with patent arterial lumen.Smoking and Hypertension
Fig. (11). An almost total occlusive (95%) thrombus in a coronary artery of a subject with severe hypertension.
Two main mechanisms play a basic role to cause pathological alterations of cardiovascular system in patients with vascular hyper-tensive disease: increased afterload and increase of peripheral arte-rial resistance, which is a consequence of vasoconstriction caused by mechanical but also biochemical variables of the hypertension.
Pathological alterations of hypertension complicated by target organ damage are, however, not strictly specific of the disease. Pathological diagnosis of hypertensive heart disease with cardiac hypertrophy, left ventricular thickening and increase in size and weight of the heart can be made only when other cardiac abnormali-ties able to cause similar alterations like valvular lesions, some congenital heart disease and diseases of the aorta can be absolutely excluded. Indeed, the autopsy technique for heart exam proposed by Roussy and Ameuille [158] well helps to make a differential diag-nosis.
Cardiac hypertrophy due to hypertension is defined a concentric hypertrophy since it occurs, once the early stage of hypertension has passed, at expense of the left ventricular chamber which re-duces significantly its volumetric width. When hypertension is complicated by heart failure, an important cardiac enlargement oc-curs with reduced thickening of left ventricular wall and pump function.
In conclusion, pathological variables observed in hypertensive individuals at the autopsy are similar to those triggered by cigarette smoking inducing atherosclerotic plaque progression. The chemi-cals released by smoking strongly support vascular alterations of complicated hypertension.
COMBINED SMOKING AND HYPERTENSION
The effects of the combined action of smoking and hyperten-sion on the cardiovascular system usually involve several vascular beds, which, in its turn, may determine functionally abnormal re-sponses as well as specifically clinical symptoms. Coronary, cere-bral and carotid arteries are, primarily, adversely affected.
The relationship between cigarette smoking and left ventricular mass was investigated by Verdecchia et al [159]. In this case-control study, the association of blood pressure with heavy cigarette smoking (equal or more than 20 cigarettes/day) adversely influ-enced left ventricular mass in male and female essential hyperten-sive patients.
Coagulation-fibrinolysis system is another parameter involved in cardiovascular damage caused by smoking and associated hyper-tension.. Smoking adversely influences coagulation-fibrinolysis cascade with alterations of the thrombogenic mechanisms [160- Current Pharmaceutical Design, 2011, Vol. 17, No. 28 2997
161]. Similarly, hypertension feels the adverse effects related to changes in plasma viscosity and hematocrit [84, 133].
Atherosclerosis in smokers develops approximately 10 years earlier than that in non-smokers [162]. Indeed, a very high percent-age (84%) of smokers was in a group of inpatients with unilateral or bilateral renal artery stenosis [163], an occurrence which is able to cause hypertension with high rate.
The association of hypertension with cigarette smoking is fre-quent in patients with malignant hypertension [164-165]. In particu-lar, there was evidence that hypertensive smokers are 5 times more likely to develop malignant hypertension than non-smokers are [166].
Although cigarette smoking may not be associated with the de-velopment of essential hypertension, its significant impact on prog-nosis of hypertensive patients has been extensively documented by several epidemiological and prospective trials. In the Multiple Risk Factor Intervention Trial (MRFIT), the age-adjusted rate of coro-nary artery disease death was greater in smokers than that non-smokers at all levels of blood pressure [167]. Data from the Systolic Hypertension in the Elderly Program (SHEP), a clinical trial that evaluated the benefit of treating over 60-year-old patients with iso-lated systolic hypertension ( 160 mmHg), indicated that cigarette smoking independently increased the risk of cardiovascular disease events by more than 50% [168]. The more recent Hypertension Op-timal Treatment (HOT) trial [169] analysed cardiovascular morbid-ity and mortality of over 18,000 hypertensive patients subjected to intensive lowering of diastolic blood pressure. These data have sub-sequently been analyzed after stratification of the patients according to global cardiovascular risk, and, even after effective lowering of elevated diastolic blood pressure, other cardiovascular risk factors still played an important role in determining the residual risk of hy-pertensive patients [170]. In particular, it was clearly demonstrated that the highest total mortality was seen in smokers with an inci-dence of approximately twice as high as in non-smokers. The harm-ful effect of smoking was evidenced even during a short observa-tional period.
Large-scale trials conducted in hypertensive patients show un-doubtedly that hypertension is a strong risk factor which aggravates the harmful atherosclerotic effects of smoking on cardiovascular system although there is evidence that smoking, usually, precedes the appearance of hypertension. Building the stairs of cardiovascu-lar damage, smoking is at the first step followed by hypertension. Therefore, there is a close relationship between these two factors that, possibly, act independently but also additively on vascular damage.
Clinical trials have shown that lowering blood pressure below 140 mmHg for systolic and 90 mmHg for diastolic values deter-mines both clinical and prognostic benefits. Moreover, blood pres-sures between 120/80 and 139/ 89 mmHg have identified a pattern defined pre-hypertension which may be considered a precursor of stage 1 hypertension and predictor of excessive cardiovascular risk
Acute exposure to passive smoking adversely influences either blood vessel dilation, since there is a reduced release of NO, or ar-terial stiffness with increased blood pressure values. Although the type of pathological changes accompanying blood pressure is, usu-ally, proven later, there is evidence that it begins acutely while an individual smokes [14].
In conclusion, even if assessing the course of systolic blood pressure immediately after smoking exposure may be difficult un-less in experimental findings, one cannot deny its increase related to smoking exposure. Thus, adverse effects of smoking on the arterial wall are pre-existing to the hypertension, which, usually, could ap-pear when structurally severe and irreversible alterations begin [172].2998 Current Pharmaceutical Design, 2011, Vol. 17, No. 28
Therefore, smoking and hypertension, when they act together, are two parallel tracks directed towards the same station: the station of an increase of cardiovascular damage.
CONFLICT OF INTEREST
No.
REFERENCES
Hopkins PN, Williams RR. Identification and relative weight of cardiovascular risk factors. Cardiol Clin 1986; 40: 3-31.
Sherman CB. Health effects of cigarette smoking. Clin Chest Med. 1991 Dec; 12(4): 643-58.
Leone A. The heart: a target organ for cigarette smoking. J Smok-ing-Related Dis 1992; 3: 197-201.
US Department of Health, Education, and Welfare: The health con-sequences of smoking: a report of the Surgeon General. Cardiovas-cular disease. Rockville, MD: US Department of Health and Hu-man Services, Public Health Service Office of Smoking and Health. DHHS Publication NO (PHS) 84-50204, 1983.
Leone A. Cigarette smoking and health of the heart. J Roy Soc Health 1995; 115: 354-5.
Hammond EC, Garfinkel L. Coronary heart disease, stroke and aortic aneurysm. Arch Environ Health 1969; 19: 167-82.
McBride PE. The health consequences of smoking. Cardiovascular diseases. Medical Clinics of North America 1992; 76: 333-53.
Aronow WS: Effect of passive smoking on angina pectoris. N Engl J Med 1978; 299: 21-4.
Sparrow D, Dawber TR, Colton T. The influence of cigarette smoking on prognosis after a first myocardial infarction. J Chronic Dis 1978; 31: 425-32.
Leone A, Bertanelli F, Mori L, Fabiano P, Bertoncini G. Ventricu-lar arrhythmias by passive smoking in patients with pre-existing myocardial infarction. J Am Coll Cardiol 1992; 3: 256 (A).
Wilhelmsson C, Vedin JA, Elmfeldt D, Tibblin G, Wilhelmsen L. Smoking and myocardial infarction. Lancet 1975; 1: 415-20.
Auerbach O, Carter HW, Garfinkel L, Hammond EC. Cigarette smoking and coronary heart disease, a macroscopic and micro-scopic study. Chest 1976; 70: 697-705.
Reid DD, Hamilton PJS, McCartney P, Rose G. Smoking and other risk factors in coronary heart disease in British civil servants. Lan-cet 1976; 11: 979-84.
Glantz SA, Parmley WW. Passive smoking and heart disease. JAMA 1995; 273: 1047-53.
Wells AJ. Passive smoking as a cause of heart disease. J Am Coll Cardiol 1994; 24: 546-54.
Meinert CL, Forman S, Jacobs DR, Stamler J. Cigarette smoking as a risk factor in men with a prior history of myocardial infarction. J Chronic Dis 1979; 32: 415-25.
Glantz SA, Parmley WW. Passive smoking and heart disease: epi-demiology, physiology, and biochemistry. Circulation 1991; 83: 1-12.
Baer L, Radichevich I. Cigarette smoking in hypertensive patients. Blood pressure and endocrine responses. Am J Med 1985; 78: 564-8.
Celermajer DS, Adams MR, Clarkson P, et al. Passive smoking and impaired endothelium-dependent arterial dilatation in healthy young adults. N Engl J Med 1996; 334:150-4.
Leone A, Lopez M. Oral contraception, ovarian disorders and to-bacco in myocardial infarction of woman. Pathologica 1986; 78: 237-42.
Pojola S, Siltanen P, Romo M. Five-year survival of 728 patients after myocardial infarction. Br Heart J 1980; 43: 176-83.
Leone A. Relationship between cigarette smoking and other coro-nary risk factors in atherosclerosis: risk of cardiovascular disease and preventive measures. Curr Pharm Des 2003; 9: 2417-23.
Byrd JC. Environmental tobacco smoke. Medical and legal issues. Medical Clinics of North America 1992; 76: 377-97.
Peto R, Lopez AD, Boreham J, Thun M, Heath C. Mortality from smoking in developed countries: 1950-2000. Oxford: Oxford Uni-versity Press 1994.
Wald NJ, Hackshaw AK. Cigarette smoking: an epidemiological overview. Br Med Bull 1996; 52: 3-11. Landini and Leone
Leone A, Bertanelli F, Mori L, Fabiano P, Battaglia A. Features of ischaemic cardiac pathology resulting from cigarette smoking. J Smoking-Related Dis 1994; 5: 109-14.
Health or Smoking. Follow-up Report of the Royal College of Phy-sicians. Pitman Publishing, London 1983.
Astrup P. The arterial wall in atherogenesis. In Cavallero Ed. Athe-rogenesis. Padua, Piccin Medical Books 1965: 77-92.
Leone A. Biochemical markers of cardiovascular damage from tobacco smoke. Curr Pharm Des 2005; 11: 2199-2208.
Leone A, Landini L Jr, Biadi O, Balbarini A. Smoking and cardio-vascular system: cellular features of the damage. Curr Pharm Des 2008; 14: 1771-7.
Leone A. Cardiovascular damage from smoking: a fact or belief? Int J Cardiol 1993; 38: 113 7.
Ghiadoni L, Taddei S, Virdis A, et al. Endothelial function and common carotid wall thickening in patients with essential hyper-tension. Hypertension 1998; 32: 25-32.
Smoking and Health. Report of the Surgeon General, U.S. Depart-ment of Health, Education, and Welfare; 1979: 1964.
Khan HA, Medalie JH, Newfeld HN, Riss E, Goldbourt U. The incidence of hypertension and associated factors: the Israel ischemic heart disease study. Am Heart J 1972; 84: 171-182.
John S, Schmieder RE. Impaired endothelial function in arterial hypertension and hypercholesterolemia: potential mechanisms and differences. J Hypertens 2000; 18: 363-74.
Leone A. Passive smoking exposure and cardiovascular health. In: Passive smoking and health research, NA Jeorgensen ed, Nova Sci-ence Publishers, Inc, New York 2007; 65-94.
Olshansky SJ, Ault AB. The fourth stage of the epidemiologic tran-sition: The age of delayed degenerative diseases. Milbank Q 1986; 64: 355-91.
Omran AR. The epidemiologic transition: A key of the epidemiol-ogy of population change. Milbank Mem Fund Q 1971; 49: 509-38.
Leone A, Giannini D, Bellotto C, Balbarini A. Passive smoking and coronary heart disease. Curr Vasc Pharmacol 2004; 2: 175-82.
Office of Health and Environmental Assessment, Office of Re-search and Development: Respiratory health effects of passive smoking: lung cancer and other disorders. Report N EPA/600/6-90/006F. Washington, DC: US Environmental Protection Agency, 1992.
Armitage AK, Turner DM. Absorption of nicotine in cigarette and cigar smoke through the oral mucosa. Nature 1970; 226: 1231-2.
Armitage AK, Dollery CT, George CF, Houseman TH, Lewis PJ, Turner DM. Absorption and metabolism of nicotine from ciga-rettes. BMJ 1975; 4: 313-6.
Surgeon General Report, Center for Health Promotion and Educa-tion, Office on Smoking and Health. The health consequences of smoking nicotine addiction: A Report of the Surgeon General. DHHS Publication N (CDC) 88-8406; 1988.
Benowitz NL, Hukkanen J, Jacob P. Nicotine chemistry, metabolism, kinetics and biomarkers. Handb. Exp. Pharmacol. 192: 29-60, 2009.
Baselt R, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biochemical Publication, Foster City, CA, 2008; 1103-7.
Leone A, Landini L, Leone A. What is tobacco smoke? Sociocul-tural dimensions of the association with cardiovascular risk. Curr Pharm Des 2010; 16: 2510-7.
Leone A. Biochemical markers of passive smoking. In: Passive Smoking and Cardiovascular Pathology, Mechanisms and Physiopathological Basis of Damage, A Leone ed, Nova Science Publishers Inc, New York 2007; 19-37.
Adams JD, Erickson HH, Stone HL. Myocardial metabolism dur-ing exposure carbon monoxide in the conscious dog. J appl Physiol 1973; 34: 238-42.
Horwath SM, Raven PB, Dahms TE, Gray DJ. Maximal aerobic capacity at different levels of carboxyhemoglobin. J appl Physiol 1975; 38: 300-3.
Lewey FH, Drabkin DD. Experimental chronic carbon monoxide poisoning of dogs. Am J Med Sci 1944; 208: 502-11.
Anderson RF, Allensworth DC, DeGroot WJ. Myocardial toxicity from carbon monoxide poisoning. Ann Intern Med 1967; 11: 72-82.
Thomsen HK, Kjeldsen K. Threshold limit for carbon monoxide-induced myocardial damage. Arch Environ Health 1974; 29: 73-8.Smoking and Hypertension
Leone A, Mori L, Bertanelli F, Fabiano P, Filippelli M. Indoor pas-sive smoking: its effect on cardiac performance. Int J Cardiol 1991;247-52.
Apple FS. Serum thiocyanate concentrations in patients with nor-mal or impaired renal function receiving nitroprusside. Clin Chem 1996; 42: 1878-9.
De la Higuera AJ. Determination of serum thiocyanate in patients with thyroid disease using a modification of the Aldridge method. J Anal Toxicol 1994; 18: 58-9.
Olea F, Parras P. Determination of serum levels of dietary thiocy-anate. J Anal Toxicol 1992; 16: 258-60.
Hole DJ, Gillis CR, Chopra C, Hawthorne VM. Passive smoking and cardiorespiratory health in a general population in the West of Scotland. BMJ 1989; 299: 423-7.
Bonita R, Duncan J, Truelsen T, Jackson RT, Beaglehole R. Pas-sive smoking as well as active smoking increases the risk of acute stroke. Tob Contr 1999; 8: 156-60.
Howard G, Wagenknecht L, Cai J, Cooper L, Kraut M, Toole JF. Cigarette smoking and other risk factors for silent cerebral infarc-tion in the general population. Stroke 1998b; 29: 913-7.
You RX, Thrift AG, McNeil JJ, Davis SM, Donnan GA, for the Melbourne Stroke Risk Factor Study (MSRFS) Group. Ischemic stroke risk and passive exposure to spouses cigarette smoking. Am J Public Health 1999; 89: 572-5.
Whincup PH, Gilg JA, Emberson JR, et al. Passive smoking and risk of coronary heart disease and stroke: prospective study with cotinine measurement. BMJ 2004; 329: 200-5.
Ross R. Factors influencing atherogenesis. In: Hurst, The Heart, Hurst JW ed, McGraw-Hill, New York 1982; 935-50.
Pimm PE, Silverman F, Shepard RJ. Physiological effects of acute passive exposure to cigarette smoke. Arch Environ health 1978; 33: 201-13.
McMurray RG, Hicks LL, Thompson DL. The effects of passive inhalation of cigarette smoke on exercise performance. Eur J Appl Physiol 1985; 54: 196-200.
Allred EN, Blecker ER, Chaitman BR, et al. Short-term effects of carbon monoxide exposure on the exercise performance of subjects with coronary artery disease. N Engl J Med 1989; 321: 1426-32.
Sheps DS, Herbst MC, Hinderliter AL, et al. Production of ar-rhythmias by elevated carboxyhemoglobin in patients with coro-nary artery disease. Ann Intern Med 1990; 113: 343-51.
Royal College of Physicians. Health or Smoking. Follow-up report 1983, Pitman Publishing, London, 1983.
Leone A. Cigarette smoking and cardiovascular damage: Analytic review of the subject. Singapore Med J 1994; 35: 492-4.
Herbert K, Kaif M, Tamariz L, et al. Prevalence of stroke in sys-tolic heart failure. J Card Fail 2011; 17: 76-81.
Leone A. Does smoking act as a friend or enemy of blood pres-sure? Let release Pandoras box. Cardiology Research and Practice vol 2011; Article ID 264894, 7 pages. doi: 104061/2011/264894.
Molgaard CA, Bartok A, Peddecord M, Rothrock J. The associa-tion between cerebrovascular disease and smoking: A case-control study. Neuroepidemiology 1986;5: 88-94.
Lee PN, Chamberlain J, Alderson MR. Relationship of passive smoking to risk of lung cancer and other smoking-associated dis-eases. Br J Cancer 1986; 54: 97-105.
Donnan GA, McNeill JJ, Adena MA, Doyle AE, OMalley HM, Neill GC. Smoking as a risk factor for cerebral ischaemia. Lancet 1989; 2: 643-7.
Sandler DP, Comstock GW, Helsing KJ, Shore DL. Deaths from all causes in non-smokers who lived with smokers. Am J Public Health 1989; 79: 163-7.
Howard J, Wagenknecht LE, Burke GL, et al. for the ARIC Inves-tigators. Cigarette smoking and progression of atherosclerosis; The atherosclerosis risk in communities (ARIC) study. JAMA 1998;
157-8.
WHO-Steps-Stroke Manual (version 1.2). The WHO stepwise ap-proach to stroke surveillance.
]77]Howard G, Burke GL, Szklo M, et al. Active and passive smoking are associated with increased carotid wall thickness. Arch Intern Med 1994; 154: 1277-82.
Buerger L. Thrombo-angiitis obliterans: a study of the vascular lesions leading to presenile spontaneous gangrene. Am J Med Sci 1908; 136: 567-80. Current Pharmaceutical Design, 2011, Vol. 17, No. 28 2999
Young C, Beynon H, Haskard D. Buergers disease (thromboangi-itis obliterans): a reversible cause of upper limb digital infarcts. Rheumatology 2000; 39: 442-3.
Lambotte O, Chazerain P, Vinciguerra C, Meyer O, Ziza JM. Thromboangiitis obliterans with inagural rheumatic manifestations. A report of three cases. Rev Rheum Engl Ed 1997; 64: 334-8.
Housley E. Treating claudication in five words. BMJ 1988; 296: 1483-4.
Meade TW, Imeson J, Stirling Y. Effects of changes in smoking and other characteristics on clotting factors and the risk of ischemic heart disease. Lancet 1987; 2: 986-8.
Kannel WB, DAgostino RB, Belanger AJ. Fibrinogen, cigarette smoking, and risk of cardiovascular disease: insights from the Framingham Study. Am Heart J 1987; 113: 1006-10.
Smith FB, Lee AJ, Fowkes FG, Price JF, Rumley A, Lowe GD. Hemostatic factors as predictors of ischemic heart disease and stroke in the Edinburgh Artery Study. Arterioscler Thromb Vasc Biol 1997; 3321-5.
Armani C, Landini L Jr, Leone A. Molecular and biochemical changes of the cardiovascular system due to smoking exposure. Curr Pharm Des 2009; 15: 1038-53.
Giannini D, Leone A, Di Risceglie D, et al. The effects of acute passive smoke exposure on endothelium-dependent brachial artery dilation in healthy individuals. Angiology 2006; 57: 564-8.
Leone A, Balbarini A. Exposure to passive smoking: A test to pre-dict endothelial dysfunction and atherosclerotic lesions. Angiology 2008; 59: 220-3.
Stone MC, Thorpe JM. Plasma-fibrinogen-a major coronary risk factor. JR Coll Gen Pract 1985; 35: 565-9.
Craig WY, Palomaki GE, Haddow JE. Cigarette smoking and se-rum lipid and lipoprotein concentrations: an analysis of published data. BMJ 1989; 298: 784-8.
Milionis HJ, Elisaf MS, Mikhailidis DP. The effects of lipid-regulating therapy on haemostatic parameters. Curr Pharm Des 2003; 9: 2425-43.
Fisher ER, Wholey M, Shoemaker R. Cigarette smoking and cho-lesterol atherosclerosis of rabbits. Arch Pathol 1974; 98: 418-21.
Pedersen TR. Lowering cholesterol with drugs and diet. N Engl J Med 1995; 333: 1350-1.
Rimm EB, Can J, Stampfer MJ, Colditz GA, Willet WC. Prospec-tive study of cigarette smoking, alcohol use, and the risk of diabe-tes in men. BMJ 1995; 310: 555-9.
Wannamethee SG, Shaper AG, Perry IJ. Smoking as a modifiable risk factor for type 2 diabetes in middle-aged men. Diabetes Care 2001; 24: 1590-5.
Rimm EB, Manson JE, Stampfer MJ, et al. Cigarette smoking and the risk of diabetes in women. Am J Public Health 1993; 83: 211-4.
Kawakami N, Takatsuka N, Shimizu H, Ishibashi H. Effects of smoking on the incidence of non-insulin-dependent diabetes melli-tus: replication and extension in a Japanese cohort of male employ-ees. Am J Epidemiol 1997; 145: 103-9.
Haire-Joshu D, Glasgow RE, Tibbs TL. Smoking and diabetes. Diabetes Care 1999; 22: 1887-98.
Houston TK, Person SD, Pletcher MJ, Liu K, Iribarren C, Kiefe CI. Active and passive smoking and development of glucose intoler-ance among young adults in a prospective cohort: CARDIA Study. BMJ 2006; 332: 1064-9.
Reaven GM. The insulin resistance syndrome: Definition and die-tary approaches to treatment. Ann Rev Nutr 2005; 25: 391-406.
Kendall DM, Sobel BE, Coulston AM, et al. The insulin resistance syndrome and coronary artery disease. Coron Art Dis 2003; 14: 335-48.
Henkin L, Zaccaro D, Haffner S, et al. Cigarette smoking, envi-ronmental tobacco smoke exposure and insulin sensitivity: the In-sulin Resistance Atherosclerosis Study. Ann Epidemiol 1999; 9: 290-6.
Reaven GM, Tsao PS. Insulin resistance and compensatory hyper-insulinemia: the key player between cigarette smoking and cardio-vascular disease? J Am Coll Cardiol 2003; 41: 1044-7.
Benowitz NL. Pharmacologic aspects of cigarette smoking and nicotine addiction. N Engl J Med 1988; 319: 1318-30.
FitzGerald GA, Oates JA, Nowak J. Cigarette smoking and hemo-static function. Am Heart J 1988; 115: 267-71.
Gibbons GH, Dzau VJ. The emerging concept of vascular remodel-ling. N Engl J Med 1994; 330: 1431-8.3000Current Pharmaceutical Design, 2011, Vol. 17, No. 28
Kojda G, Harrison D. Interaction between NO and reactive oxygen species: pathophysiological importance in atherosclerosis, hyper-tension, diabetes and heart failure. Cardiovasc Res 1999; 43: 562-71.
Nedeljkovic ZS, Gokce N, Loscalzo J. Mechanisms of oxidative stress and vascular dysfunction. Postgrad Med J 2003; 79: 195-200.
Ceconi C, Boraso A, Cargnoni A, Ferrari R. Oxidative stress in cardiovascular disease: myth or fact? Arch Biochem Biophys 2003;217-21.
Harrison D, Griendling KK, Landmesser U, Hornig B, Drexler H. Role of oxidative stress in atherosclerosis. Am J Cardiol 2003; 91: 7A-11A.
TaniyamaY, Griendling KK. Reactive oxygen species in the vascu-lature: molecular and cellular mechanisms. Hypertension 2003; 42: 1075-81.
Holt PG. Immune and inflammatory function in cigarette smokers. Thorax 1987; 42: 241-9.
Penn A, Chen LC, Snyder CA. Inhalation of steady-state side-stream smoke from cigarettes promotes arteriosclerotic plaque de-velopment. Circulation 1994; 90: 1363-7.
Barnoya J, Glantz SA. Cardiovascular effects of secondhand smoke. Nearly as large as smoking: Circulation 2005; 111: 2684-98.
Lough J. Cardiomyopathy produced by cigarette smoke. Ultrastruc-tural observations in guinea pig. Arch Pathol Lab Med 1978; 102; 377-80.
Gvozdjakova A, Bada V, Sany L, et al. Smoke cardiomyopathy: disturbance of oxidative processes in myocardial mitochondria. Cardiovasc Res 1984; 18: 229-32.
Kjeldsen K, Thomsen HK, Astrup P. Effects of carbon monoxide on myocardium. Ultrastructural changes in rabbits after moderate, chronic exposure. Circ Res 1974; 34: 339-48.
Bing RJ, Castellanos A, Gradel E, Lupton C, Siegel A. Experimen-tal myocardial infarction: circulatory, biochemical and pathologic changes. Am J Med Sci 1956; 232: 533-54.
Caulfield J, Klionsky B. Myocardial ischemia and early infarction; an electron microscopic study. Am J Pathol 1959; 35: 489-523.
Bryant RE, Thomas WA, ONeil RM. An electron microscopic study of myocardial ischemia in the rat. Circ Res 1958; 6: 699-709.
Cantin M, Leone A. Morphology of myocardial infarction. Meth Achiev Exp Pathol 1981; 10: 244-84.
Ehrich WE, Bellet S, Lewey FH. Cardiac changes from carbon monoxide poisoning. Am J Med Sci 1944; 208: 511-21.
Chance B, Erecinska M, Wagner M. Mitochondrial response to CO toxicity. Ann NY Acad Sci 1970; 174: 193-204.
Hayes JM, Hall GV. The myocardial toxicity of carbon monoxide. Med J Aust 1964; 1: 865-8.
Marius-Nunez AL. Myocardial infarction with normal coronary arteries after acute exposure to carbon monoxide. Chest 1990; 97: 491-4.
Stefanidis C, Vlachopoulos C, Tsiamis E. Unfavorable effects of passive smoking in aortic function in men. Ann Intern Med 1998;
426-34.
Salvetti A, Versari D. Control of blood pressure in the community: an unsolved problem. Curr Pharm Des 2003; 9: 2375-84.
Berglund G, Andersson O, Wilhelmsen L. Prevalence of primary and secondary hypertension: Studies in a random population sam-ple. BMJ 1976; 2: 554-6.
Williams GH. Quality of life and its impact on hypertensive pa-tients. Am J Med 1987; 82: 98-105.
Luma GB, Spiotta RT. Hypertension in children and adolescents. Am Fam Physician 2006; 73(9): 1558-68.
Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: di-agnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 2008; 51(6): 1403-19.
Kearney PM, Whelton M, Reynolds K, et al. Global burden of hy-pertension: analysis of worldwide data. Lancet 2005; 365: 217-23.
Falkner B. Hypertension in children and adolescent: epidemiology and natural history. Pediatr Nephrol 2010; 25: 1219-24.
Pickering GW. Transient cerebral paralysis in hypertension and in cerebral embolism- with special references to the pathogenesis of chronic hypertensive encephalopathy. JAMA 1948; 137: 423-30. Landini and Leone
Carpenter RE. Neurological complications of hypertension, with special reference to hypertensive encephalopathy. J Okla Med As-soc 1963; 56: 63-5.
Cruz-Flores S, Gondin de Assis Aquino M, Leira EC. Brainstem involvement in hypertensive encephalopathy: clinical and radio-logical findings. Neurology 2004; 62. 1417-9.
Gonzales A, Lopez B, Ravassa S, et al. Biochemical markers of myocardial remodelling in hypertensive heart disease. Cardiovasc Res 2009; 81: 509-18.
Vasan RS. Biomarkers of cardiovascular disease: molecular basis and practical considerations. Circulation 2006; 113: 2335-62.
Morrow DA, de Lemos JA. Benchmarks for the assessment of novel cardiovascular biomarkers. Circulation 2007, 115: 949-52.
Brown TC, Davis JO, Olichney MJ, Johnston CI. Relation of plasma renin to sodium balance and arterial pressure in experimen-tal renal hypertension. Circ Res 1966; 18: 475-83.
Bianchi G, Tenconi LT, Lucca R. Effect in the conscious dog of constriction of the renal artery to a sole remaining kidney on haemodynamics, sodium balance, body fluid volumes, plasma ren-nin concentration and pressor responsiveness to angiotensin. Clin Sci 1970; 38: 741-66.
Leenen FH, deJong W. Plasma renin and sodium balance during development of moderate and severe renal hypertension in rats. Circ Res 1975; 36: 179-86.
Yudkin JS, Forrest RD, Jackson CA, et al. Microalbuminuria as a predictor of vascular disease in non-diabetic subjects. Lancet 1998;530-3.
Parving HH, Mogensen CE, Jensen HAE, Evorr PE. Increased uri-nary albumin excretion rate in benign essential hypertension. Lan-cet 1974; 15: 1190-2.
Ross EJ, Linch DC. Cushings syndrome-killing disease: discrimi-natory value of signs and symptoms aiding early diagnosis. Lancet 1982; 2: 646-9.
Bravo EL, Tarazi RC, Gifford RW, et al. Circulating and urinary catecholamines in pheochromocytoma. N Engl J Med 1979; 301: 682-6.
Oliver MF. Reducing cholesterol does not reduce mortality. J Am Coll Cardiol 1988; 12: 814-7.
Taylor WC, Pass TM, Shepard DS, Komaroff AL. Cholesterol re-duction and life expectancy. Ann Intern Med 1987; 106: 605-14.
Kuwahara K, Saito Y, Harada M, et al. Involvement of cardiotro-phin 1 in cardiac myocyte-nonmyocyte interactions during hyper-trophy of rat cardiac myocytes in vitro. Circulation 1999; 100: 1116-24.
Lopez B, Gonzales A, Lasarte JJ, et al. Is plasma cardiotrophin- 1 a marker of hypertensive heart disease? J Hypertens 2005; 23: 625-32.
Gonzales A, Ravassa S, Loperena I, et al. Association of depressed cardiac gp130-mediated antiapoptotic pathways with stimulated cardiomyocyte apoptosis in hypertensive patients with heart failure. J Hypertens 2007; 25: 2148-57.
Pemberton CJ, Raudsepp SD, Yandle TG, Cameron VA, Richards AM. Plasma cardiotrophin-1 is elevated in human hypertension and stimulated by ventricular stretch. Cardiovasc Res 2005; 68: 109-17.
Cederholm A, Frostegard J. Annexin A5 as a novel player in pre-vention of atherothrombosis in SLE and in general population. Ann N Y Acad Sci 2007; 1108: 96-103.
Ravassa S, Gonzales A, Lopez B, et al. Upregulation of myocardial Annexin A5 in hypertensive heart disease: association with systolic dysfunction. Eur Heart J 2007; 28: 2785-91.
Goldblatt H. The renal origin of hypertension. Physiol Rev 1947;
120-165.
London RE, London SB. Rupture of the heart. Circulation 1965;202-
Leone A. Postinfarction cardiac rupture: a challenge to try surgical reparation. G Ital Cardiol 1987; 17: 252-8.
Leone A. Are we able to prevent death due to postinfarction cardiac rupture by early diagnosis and surgical treatment? Jpn Heart J 1991; 32: 635-44.
Roussy G, Ameuille P. Technique des autopsies et des recherches anatomo-pathologiques lAnphithatre. O Doin et Fils, Paris, 1910.
Verdecchia P, Schillaci G, Borgioni C, et al. Cigarette smoking, ambulatory blood pressure and cardiac hypertrophy in essential hy-pertension. J Hypertens 1995; 13: 1209-15.Smoking and Hypertension
Stewart MJ, Jyothinagaram S, McGinley IM, Padfield PL. Cardio-vascular effects of cigarette smoking: ambulatory blood pressure and BP variability. J Hum Hypertens 1994;8:19-22.
Ridker PM, Hennekens CH. Hemostatic risk factors for coronary heart disease. Circulation 1991; 83: 1098-1100.
Zieske AW, Malcom GT, Strong JP. Natural history and risk fac-tors of atherosclerosis in children and youth: the PDAY study. Pe-diatr Pathol Mol Med 2002;21:213-37.
Mackay A, Brown JJ, Cumming AM, Isles C, Lever AF, Robertson JI. Smoking and renal artery stenosis. BMJ 1979; 2:770.
Tuomilehto J, Elo J, Nissinen A. Smoking among patients with malignant hypertension. BMJ 1982; 284:1086.
Petitti DB, Klatsky AL. Malignant hypertension in women aged 15 to 44 years and its relation to cigarette smoking and oral contracep-tives. Am J Cardiol 1983; 52: 297-8.
Isles C, Brown JJ, Cumming AM, et al. Excess smoking in malig-nant-phase hypertension. BMJ 1979; 1: 579-81.
Multiple risk factor intervention trial. Risk factor changes and mor-tality results. Multiple Risk Factor Intervention Trial Research Group. JAMA 1982; 248:1465-77.
Received: June 28 2011Accepted: August 4, 2011 Current Pharmaceutical Design, 2011, Vol. 17, No. 28 3001
Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Sys-tolic Hypertension in the Elderly Program (SHEP). SHEP Coopera-tive Research Group. JAMA 1991; 265: 3255-64.Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive
blood-pressure lowering and low-dose aspirin in patients with hy-pertension: principal results of the Hypertension Optimal Treat-ment (HOT) randomised trial. HOT Study Group. Lancet 1998; 351:1755-62.
Zanchetti A, Hansson L, Menard J, et al. Risk assessment and treatment benefit in intensively treated hypertensive patients of the hypertension Optimal Treatment (HOT) study. J Hypertens 2001; 19:819-25.
Julius S, Nesbitt SD, Egan BM, et al. for the Trial of Preventing Hypertension (TROPHY) Study Investigators. Feasibility of treat-ing prehypertension with an angiotensin-receptor blocker. N Engl J Med 2006; 354: 1685-97.
Ballantyne D, Devine BL, Fife R. Interrelation of age, obesity, cigarette smoking, and blood pressure in hypertensive patients. BMJ 1978; 1: 880-1.