Should diabetes be commissioned through multidisciplinary networks, rather than Practice Based...
-
Upload
david-simmons -
Category
Documents
-
view
216 -
download
3
Transcript of Should diabetes be commissioned through multidisciplinary networks, rather than Practice Based...
O
Sn
Da
Ub
c
d
e
a
A
R
A
A
K
D
C
N
G
P
1
To
Cf
1d
p r i m a r y c a r e d i a b e t e s 5 ( 2 0 1 1 ) 39–44
Contents lists available at ScienceDirect
Primary Care Diabetes
j o u r n a l h o m e p a g e : h t t p : / / w w w . e l s e v i e r . c o m / l o c a t e / p c d
riginal research
hould diabetes be commissioned through multidisciplinaryetworks, rather than Practice Based Commissioning?
avid Simmonsa,∗, Patrick Englishb, Peter Robinsc, Andrew Craigd, Rachael Addicott e
Lead Community Diabetologist, Institute of Metabolic Science, Cambridge University Hospitals NHS Foundation Trust, Cambridge,nited KingdomPlymouth Hospitals NHS Foundation Trust, Plymouth, United KingdomCambridge, United KingdomWest Hoe Surgery, Plymouth, United KingdomKing’s Fund, London, United Kingdom
r t i c l e i n f o
rticle history:
eceived 24 December 2009
ccepted 19 September 2010
vailable online 16 October 2010
eywords:
iabetes
ommissioning
etwork
eneral practice
olicy
a b s t r a c t
Aims: Diabetes is recognized as a complex, long term, largely asymptomatic condition requir-
ing self management skills, a range of health care professionals and articulated health
services. Diabetes Networks have been introduced to provide guidance from people with
diabetes and local health professionals with different skills to ensure that diabetes care is
well organized, sustainable and delivers quality care. We have considered the role of Diabetes
Networks in the English setting.
Methods: Drawing on studies of health service organization and health policy, we describe
the context in which diabetes commissioning is currently occurring in England, the role of
Diabetes Networks and key components for an effective Diabetes Network.
Results: We have identified that Diabetes Networks are not currently mandatory and discov-
ered policy approaches that are likely to work against safe, timely, integrated approaches to
diabetes services with potentially harmful impacts on people with diabetes in the future.
Practice Based Commissioning, where it sidelines Diabetes Networks, is a particular concern.
We have identified key components of Diabetes Networks including explicit frameworks for
leadership, membership, funding, decision making, communication and action.
Conclusions: Diabetes is a condition requiring collaboration between all involved. Diabetes
tient
re sh
ry Ca
ing hospitalization, premature death, cardiovascular, renal,
Networks include pa
and how diabetes ca
© 2010 Prima
. Introduction
he impact of diabetes is increasing rapidly with the growingbesity epidemic [1]. Modern interventions are very effective
∗ Corresponding author at: Wolfson Diabetes and Endocrinology Clinic,ambridge University Hospitals NHS Foundation Trust, Cambridge CB2
ax: +44 1223 217 080.E-mail address: [email protected] (D. Simmons
751-9918/$ – see front matter © 2010 Primary Care Diabetes Europe. Puoi:10.1016/j.pcd.2010.09.002
s and all relevant health professionals and should dictate what
ould be commissioned within the local health economy.
re Diabetes Europe. Published by Elsevier Ltd. All rights reserved.
at reducing the incidence of diabetes complications includ-
Institute of Metabolic Science, Box 281, Addenbrooke’s Hospital,0QQ, United Kingdom. Tel.: +44 1223 216 913;
).
eye and foot disease [2]. However, the rapid rise in diabetesprevalence is overwhelming the benefits of effective diabetesmanagement [3]. There is one other “elephant in the room”
blished by Elsevier Ltd. All rights reserved.
b e t e s 5 ( 2 0 1 1 ) 39–44
Table 1 – Summary of “world class commissioning”.
Locally lead the NHSWork with community partnersEngage with public and patientsCollaborate with cliniciansManage knowledge and assess needsPrioritise investmentStimulate the marketPromote improvement and innovationSecure procurement skillsManage the local health systemMake sound financial investments
Department of Health. World class commissioning.
40 p r i m a r y c a r e d i a
around why the impact of diabetes is not diminishing at therate expected from trials: the multiple barriers to the deliv-ery of care and self care [4]. These include psychological,psychosocial and knowledge barriers and diabetes and non-diabetes related co-morbidities [5].
A further barrier revolves around how “the system” benefitsor obstructs care [6]. It has become clear that with a condi-tion as complex and multifaceted as diabetes, systems whichintegrate primary, community and secondary care around theneeds of the patient are most likely to optimise outcomes [7].This includes integrating information management.
2. Diabetes and integrated care
There are several special features regarding diabetes that workagainst service integration within and between health organi-zations:
• It is largely a asymptomatic condition [4]: reducing patientdemand for clinical action and promoting clinical inertia.
• Management impacts on daily living with its oral medica-tions, physical activity, frequent health service attendance,self injection of medications, finger prick testing and inten-sive lifestyle change (e.g. carbohydrate counting)
• The high prevalence of psychological or psychosocial barri-ers to self care [5,6,8]
• Distant benefits from intensive glycaemic management [9]• Transmission to offspring through an abnormal intrauterine
milieu [10].• Different aspects of care requiring different skill sets and,
an agreed, communicated, multidisciplinary approach[11], without which, conflicting professional advice canundermine trust and relationships. For this reason,multidisciplinary groups, known as “Diabetes Net-works”, have formed, with patients as active members,to coordinate and formulate diabetes policy for localcommunities [11].
While the role of the patient is crucial in coordinating care,maintaining this role, in an asymptomatic condition, withoften unpleasant or obtrusive interventions and no certaintyof harm avoidance on a day to day basis, is not surprisingly,very difficult. Clearly, any system which undermines closecollaboration between the different professional groups, andprovides conflicting messages is likely to delay key interven-tions and will be detrimental over time. We would suggestthat this situation now exists with the current promotionof the internal market, potential linkage between generalpractice income and service commissioning (Practice BasedCommissioning (PBC)), fixed price fee for service (Paymentby Results (PBR)) and competition between providers in the
health sector. This, will inevitably reduce quality of life andincrease overall long-term costs. It would appear to be a clas-sic lose, lose, lose situation for patient, commissioner andtax-payer.http://www.dh.gov.uk/en/Managingyourorganisation/Commissioning/Worldclasscommissioning/Competencies/index.htm (accessed 18.9.08)
3. The current health commissioningenvironment
PBC has been introduced as part of implementing a com-petitive, market system for health services, separating thepurchasers (now known as commissioners) from providers[12]. PBC has general practitioners (GPs) holding a theoreti-cal budget for all of their patients and redesigning services toobtain “better value for money”. New designs are handed tothe local Primary Care Trust (PCT) for refinement and com-missioning. Any provider fulfilling their defined criteria canbe commissioned. The principles around the commissioningare expected to reflect “world class commissioning” (Table 1).A key method to reduce expenditure is to reduce hospitalcosts, which are now fixed through the tariffs of the PBRmechanism. The balance between financial gain and potentialcosts of reduced quality and access has not yet been shown.Furthermore, the tariff for NHS organizations includes fixedinfrastructure costs (e.g. buildings) and costs of compliancewith NHS directives, policies and procedures.
While the principle is to have “clinicians” making the com-missioning decisions, GPs are also a group of private providerspotentially competing for work and one of the few non-salaried health professional groups whose personal incomeis potentially, ultimately, linked to any changes in cash flow.
4. Commissioning of diabetes
Currently, diabetes care is commissioned by PCT’s, under thedirection of PBC groups (where established), but without arequirement to follow local Diabetes Network advice [13].While British GPs are very skilled at primary care and at run-ning a small business, the depth of knowledge required acrossall conditions is, by the very nature of generalism, usually notpresent. For people with diabetes, and ultimately the tax payer,this can present a significant problem. Diabetes care is increas-ingly provided through primary care [14] with benefits to thosepatients able to receive comparable diabetes care closer to
home. However, this shift has not always been appropriate andhas frequently set primary care and secondary care againsteach other. There are examples of reductions in diabetes sec-ondary services with the loss of PBR tariff [7]. While primaryp r i m a r y c a r e d i a b e t e s 5 ( 2 0 1 1 ) 39–44 41
Table 2 – Overview of managed clinical networks for cancer in London.
Network A Network B Network C Network D Network E
Purpose ofnetwork
To implementgovernmentpolicy
Unclear tonetworkmembers
To implementgovernmentpolicy
Improve careCommonguidelines
Restructure provision of services
The NetworkManagementTeams’approach tonetworking
Non-directive Unsuccessfulbottom-up
Non-directive Successfulbottom-up
Top-down
Educationalactivities
Multi siteSinglediscipline
Minimal Minimal Multi-siteSinglediscipline
Single site Single discipline
Approach toorganiza-tional
Reactive Loose(bottom-up)
Reactive Inclusive Authoritative Centrally driven
ervic
c2b(rb
ggOpE1cattriiaohrobDmwTPtc
afcpsse
changeStaffing Manager, lead medical and nursing clinicians s
Source: Ref. [20].
are can deliver high quality care for many of those with Typediabetes, this works best when primary care is supported
y secondary care [15]: PBR does not fund such support. In aperceived to be) under-funded secondary care service whoseesources could be in a “bidding war” with primary care, it maye difficult for services to work together [16].
While most GPs are focused on patient care and colle-iality, there is a potential for conflict when incentives areiven for primary care not to use specialist services, e.g. inxfordshire, where GPs received cash bonuses not to sendatients to hospital [17]. Elsewhere, a PCT created a “Localnhanced Service” with GPs paid for each patient with Typediabetes not seen by specialist services. With the diffi-
ulty in balancing hypoglycaemia, weight gain, glycaemiand quality of life and the rapid changes in delivery sys-ems and medications to address this, it is remarkable thathere is a payment system that rewards GPs for not refer-ing patients to those with the expertise. A further examples where a PBC Group commissioned a team, already operat-ng partly in competition with secondary services, to create
diabetes plan. The plan was not endorsed by local sec-ndary services, excluded patients in its development andad a range of costing and factual errors. Its focus was onemoving funding from secondary care, rather than the needsf the patient or providing care closer to home, with fundingeing retained by GPs. Of greatest concern was that the localiabetes Network (including patients) which had undertakenany integrated activities to enhance care in previous years,as sidelined, and prevented from playing a substantial role.he plan was approved at various levels in the PCT where theBC Group had representation. Fortunately, the PCT redirectedhe intention to one of rewarding collaboration rather thanompetition.
Clearly, Diabetes Networks, even when present, integratednd active, may be excluded from an important advisory roleor the planning and commissioning of diabetes care underurrent policy. This is in spite of it being the only place where
eople with diabetes sit alongside representatives of primary,econdary and community care, public health and managerialtaff involved with diabetes care. While there should be anthical and logical obligation to go through the Network, thee improvement lead
Department of Health (DoH) does not mandate the process[13].
We propose that for an integrated, patient focused,approach, the Diabetes Network, with its health services,patients, health disciplines and PCT representatives, shouldhave the mandate for defining the overall plan for the PCT. Thisincludes the clinical pathways that patients should follow, theexpected times to referral, ensuring that appropriate clinicalgovernance is in place and monitoring the quality of care. Dia-betes care should be commissioned as a single geographicallyintegrated approach.
5. How would Networks work?
The need for a local multidisciplinary group, includingpatients, to oversee the care for those with diabeteswas recognized long ago [18]. The DoH [11] deliverystrategy for the Diabetes National Service Frameworksuggests establishing and resourcing local Diabetes Net-works. Engagement of all relevant stakeholders, integrationacross service boundaries, transparent lines of accountabilityand excellent leadership and management are recom-mended.
In practice, Diabetes Networks exist patchily across Eng-land, each operating in a unique manner, probably reflectingthe local circumstances including the expertise and char-acter of local individuals. In one study [14], DiabetesNetworks were largely comprised of informal conglomer-ates of primary care providers, with some secondary careinteraction. There was considerable variability in ability toinfluence the local agenda and delivery of diabetes care.Senior clinical representation, from both primary and sec-ondary care, was considered an essential motivator inenacting large scale change in the delivery of diabetescare.
Diabetes Networks have no statutory role in delivering key
policy targets and implementing national plans, unlike cancernetworks [19]. Cancer networks operate within a frameworkmandated by the Department of Health on a national leveland by Strategic Health Authorities on a local level. In Lon-42 p r i m a r y c a r e d i a b e t e s 5 ( 2 0 1 1 ) 39–44
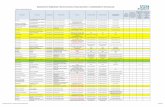
Table 3 – Proposed components of a Diabetes Network.
Component Description
Terms of reference Approving clinical governance, information management governance,service re-design, monitoring, standard setting, implementation of nationalpolicy
Limits of authority and commissioning role Defined by geographical area, Diabetes National Service Framework and NICEHealth Technology Assessments. Mandate to make firm commissioningrecommendations to PCT within and, where appropriate, outside budget
Leadership andexecutive activities
Chair could be appointed or electedExecutive to have paid protected time to ensure implementation ofrecommendations between meetings
Membership Primary care medical and nursing memberSecondary care medical and nursing memberAllied health members: dietitian, podiatry, pharmacistPatients with Type 1 and patients with Type 2 diabetesCarer of child and carer of older person with diabetesSenior secondary care manager (delegate of chief executive)Primary care managerSenior PCT manager(delegate of chief exec linked with commissioning)Community services member (connected to diabetes related and socialservices)Communications officer
Funding Chair timeAdmin supportCommunicationsMeeting expensesTraining of chair
Decision making By consensusWhere consensus is not reached, decision deferred to PCT
Conflict of Interest Needs to be declaredFrequency ofmeetings
QuarterlySubgroup meetingsExecutive consisting of lead consultant, GP, diabetes specialist nurse,primary care manager, secondary care manager in between
Subgroups Information management (including audit)Education (professional, patient)Guidelines (for production of diabetes management guidelines and review ofguidelines issued from other groups/subgroups)Patient/carer groupRetinal screeningPregnancyChildren and young adultsWorkforce (planning and training)
Communications To identify communications needs and to ensure distribution of timelyrmat
sts, dips, Media
infoTrugrouall m
don, cancer networks were largely similar in their structureand purpose [20], but showed wide variation in the inter-nal management structure and approach to organizationalchange (Table 2). While some emphasized the importance of aflat structure and were more reactive to the DOH remit, othershad deliberately developed a hierarchical configuration andwere more proactive in pre-empting national policy. The dif-ferences in configuration tended to reflect the level of clinicalleadership within Network. Often working through subgroups,the networks facilitated communication and defined proto-cols, guidelines, care pathways, information management andaudit. Some felt that the cancer networks should have direct
responsibility for funding. Inclusion of senior managers waspivotal in turning plans into action. Surprisingly, patient andcarer representatives were not present on the networks stud-ied.ion to all relevant groups, e.g. Chief Executives of SHAs, PCTs andabetes and Long term conditions leads, PEC chairs, DUK and useredia. Communications officer should be the point of reference forcommunications
6. Discussion
We would maintain that in diabetes, a chronic condition, withits history of motivated patients and a multidisciplinary inter-sectoral approach, a well defined modus operandus could becreated for Networks. Representation of all relevant disci-plines (from primary, community and secondary care), seniormanagement and particularly those with diabetes is needed.The suggested Terms of Reference, shown in Table 3, wouldsupport a move to the integrated approach recommendedin the Darzi report and in “A New Start” [21] and by the
Royal Colleges in “Teams without Walls” [22]. The PCT shoulddevolve a “diabetes budget” down to the network for thegeographical area, although the final commissioning deci-sion would rest with the PCT. In view of the complexity ofe t e s
cdthiMr
ovicapcemdcfie
wMtpmrnaf
abWatdi
C
TLbPaiRwst
hbTo
r
p r i m a r y c a r e d i a b
alculating the current, and future, real and excess costs ofiabetes, the Network should be able to define and priori-ise what is required and make recommendations about howospitalization and complication savings can be translated
nto services for prevention of complications (in advance).any of these costs are currently not coded as being diabetes
elated.There are genuine practical issues about having a group
f local providers work closely together to define ser-ices. However, this is already happening with PBC, albeitncluding only one sector: primary care. While integratedare limits some choices (particularly of provider), thislways occurs (e.g. by cost, knowledge, mobility, geogra-hy, culture and history). In diabetes, having a group ofommitted clinicians, managers and those with diabetesnsuring access to defined services must be preferable andore cost effective in the long term to a system where
ecisions are made through a competitive tendering pro-ess, often behind closed doors, based upon the short termnancial situation and without detailed diabetes knowl-dge.
Diabetes Networks are already recommended as theay forward by the National Diabetes Support Team [13].issing are a requirement for plans to be approved by
he Network, a clearly defined role in the commissioningrocess and a recommended framework most likely to pro-ote functionality and utility. There are opportunistic and
eal costs for those attending meetings and undertakingetwork activities. This requires both recognition and anssurance of the greatest likelihood that the work will be use-ul.
We hope that our framework will be helpful in definingpolicy which promotes an integrated approach to dia-
etes care and includes all of those involved with diabetes.hat is clear is that the current fragmented, competitive
pproach is likely to lead to more long term complica-ions in future years and make diabetes an even greateremand on individuals and health resources than it already
s.
ontributors
he initial concept arose from discussions within the Kingseadership Course for Diabetologists. DS and PE are dia-etologists with experience in diabetes service development,R is a patient with longstanding diabetes and chair of
local patient committee, AC is a GP partner involvedn commissioning and service redesign as a PEC member,A is a policy researcher with experience in health net-orks. DS wrote the first draft, all other authors added
ections and/or edited the document and approve its con-ent.
Since the submission of this paper, Government policy
as changed and commissioning is now to be undertakeny General Practice Consortia without Primary Care Trusts.he issues raised in this paper remain relevant to the debatever commissioning for diabetes.5 ( 2 0 1 1 ) 39–44 43
Conflict of interest
The authors state that they have no conflict of interest.
e f e r e n c e s
[1] P. Zimmet, K.G.M.M. Alberti, J. Shaw, Global and societalimplications of the diabetes epidemic, Nature 414 (2001)782–787.
[2] R. Williams, W. Herman, A.L. Kinmonth, N. Wareham,Evidence Based Practice in Diabetes, Wiley, London, 2002.
[3] P. Zhang, M.M. Engelgau, S.L. Norris, E.W. Gregg, V. Narayan,Application of economic analysis to diabetes and diabetescare, Ann. Intern. Med. 140 (2004) 972–977.
[4] R.G. Hiss, Barriers to care in non-insulin-dependent diabetesmellitus: the Michigan experience, Ann. Intern. Med. 124(1996) 146–148.
[5] D. Simmons, T. Weblemoe, J. Voyle, A. Prichard, L. Leakehe,B. Gatland, Personal barriers to diabetes care: lessons from amultiethnic community in New Zealand, Diabet. Med. 15(1998) 958–964.
[6] D. Simmons, S. Lillis, J. Swan, J. Haar, Discordance inperceptions of barriers to diabetes care between patients,primary care and secondary care, Diabetes Care 30 (2007)490–495.
[7] Primary Care Diabetes Society, Association of British ClinicalDiabetologists, Diabetes UK, Royal College of Nursing,Community Diabetes Consultants. Joint Position Statement:Integrated Care in the Reforming NHS-Ensuring Access toHigh Quality Care for All People with Diabetes, December2007.
[8] M. Peyrot, R.R. Rubin, T. Lauritzen, F.J. Snoek, D.R. Matthews,S.E. Skovlund, International DAWN Advisory Panel.Psychosocial problems and barriers to improved diabetesmanagement: results of the Cross-National DiabetesAttitudes. Wishes and Needs (DAWN) Study, Diabet. Med. 22(2005) 1379–1385.
[9] The Diabetes Control and Complications Trial/Epidemiologyof Diabetes Interventions and Complications (DCCT/EDIC)Study Research Group, Intensive diabetes treatment andcardiovascular disease in patients with Type 1 diabetes, N.Engl. J. Med. 353 (2005) 2643–2653.
[10] D. Dabelea, The predisposition to obesity and diabetes inoffspring of diabetic mothers, Diabetes Care 30 (Suppl. 2)(2007) S169–S174.
[11] Department of Health, National Service Framework forDiabetes: Delivery Strategy, DOH, London, 2002.
[12] J. Smith, R. Lewis, T. Harrison, Making commissioningeffective in the reformed NHS in England, Health PolicyForum, 2006 (Report No. 1).
[13] Department of Health Diabetes Commissioning Toolkit,http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH 4140284.
[14] L. Fitzgerald, C. Lilley, E. Ferlie, R. Addicott, G. McGivern, D.Buchanan, Managing Change and Role Enactment in theProfessionalised Organisation, NCCSDO, London, 2006.
[15] S. Griffin, A.L. Kinmonth, Systems for surveillance for peoplewith diabetes mellitus (review), The Cochrane Libr. 3 (2007)1–22.
[16] R. Charlton, Practice based commissioning: implications forsecondary care, Clin. Med. 8 (2008) 61–64.
[17] Brown D. GPs paid £1 a time not to refer patients to hospital:concerns about payments just to meet quotas. The TimesOctober 20, 2008.
b e t e
[22] Working Party of the Royal College of Physicians, The RoyalCollege of General Practitioners and the Royal College ofPaediatrics and Child Health, Teams Without Walls,
44 p r i m a r y c a r e d i a
[18] P. Wilson, D. Simmons, South Auckland Diabetes PlanningGroup, The development of a community orientatedrecommendations for diabetes care in South Auckland, N.Z.Med. J. 107 (1994) 456–459.
[19] R. Addicott, G. McGivern, E. Ferlie, The distortion of a
managerial technique? The case of clinical networks in UKhealth care, Br. J. Manage. 18 (2006) 93–105.[20] R. Addicott, Models of governance and the changing role ofthe Board in the “modernised” UK health sector”, J. HealthOrg. Manage. 22 (2) (2008) 147–163.
s 5 ( 2 0 1 1 ) 39–44
[21] Department of Health. A New Start. Department of Health,London, 2007.
Lavenham Group, Suffolk, England,2008.