Shock Hypovolemic
-
Upload
chance-jackson -
Category
Documents
-
view
15 -
download
0
description
Transcript of Shock Hypovolemic

v^S^r rp^ 2-19 CONTINUING EDUCATION© 2005 Uppineott Williams & Wilkins, Itic,
Hypovolemic ShockAn Overview
Dorothy M. Kelley, MSN, RN, CEN
Resuscitation of major trauma victims suffering from shock remains a challenge for trauma systemsand trauma centers. Rapid identification, and ensuring correct, aggressive treatment, are necessaryfor patient survival. This article discusses shock encountered in trauma victims: hypovolemic, car-diogenic, obstructive, and distributive shock. Emphasis is placed on hypovolemic shock and itssequelae. The critical care nurse plays an important role as part of the team involved in the re-suscitation and ongoing care of these patients. Understanding the underlying pathophysiology,recognizing signs and symptoms, and being prepared to effectively respond will further enablethe nurse to contribute to positive patient outcomes. Key words: hypovolemia, resuscitation,shock, trauma
RESUSCITATION of major trauma victimssuffering from shock remains a chal-
lenge for trauma systems and trauma cen-ters. Rapid identification, and ensuring cor-rect, aggressive treatment, are necessary forpatient survival. Trauma patients are at riskfor several types of shock states: hypov-olemic, cardiogenic, obstructive, and distribu-tive. Physiologically, regardless of the type ofshock, inadequate tissue perfusion is the re-sult of reduced or poorly distributed bloodvolume. The body activates compensatorymechanisms in an effort to improve perfu-sion. Care providers must recognize and in-tervene rapidly to support tissue oxygenationand blood flow; otherwise, these compen-satory mechanisms will fail, resulting in a cas-cade of events to include inflammatory re-sponse, release of mediators, organ failure,and death.'
The critical care nurse plays an importantrole as part ofthe team involved in the resusci-tation and ongoing care of these patients. Un-derstanding the underlying pathophysiology,recognizing signs and symptoms, and beingprepared to effectively respond will further
From the Scripps Mercy Hospital, San Diego, Calif.
Corresponding author: Dorothy M. Kelley, MSN, RN, CEN,11076 Montaubon Way, San Diego, CA 92131 (e-mail:kelley. dorothy®scrippshealth. org).
enable the nurse to contribute to positive pa-tient outcomes.
This article describes these 4 categoriesof shock states. However, since hypovolemicshock is the most common type of shockencountered in the trauma patient popula-tion, the majority of the discussion will bededicated to its recognition, definition, andtreatment.
CASE STUDY
A 35-year-old male, helmeted motorcycledriver, "T-boned" a taxicab at high speed. He wasejected, landing on pavement 30 ft from his bike.Witnesses accessed the 911 emergency medi-cal response system; paramedics arrived quickly.They found the patient lying unresponsive on thepavement; respirations were agonal; pulse, weak,and thready; BP was unobtainable. They placedthe patient in full spinal immobilization, adminis-tered oxygen, and supported respirations via abag, valve, mask (BVM) device. Transport timewas less than 2 minutes from the trauma center,so they elected to "scoop and haul." Upon arrival,the trauma team evaluated the patient, using Ad-vanced Trauma Life Support (ATLS) guidelinesand reported these findings upon primary survey:
Ainway: patent; C spine precautions maintainedBreathing: No spontaneous respirationsCirculation: Thready femoral pulse rate 56;
hypotensive with unobtainable blood pressure.Skin, cool pale and dry.

Hypovolemic Shock
Disability: GCS 3, pupils unequal, slightlyreactive.
The patient was intubated immediately upon ar-rival, using rapid sequence intubation (RSI) tech-nique. Breath sounds auscultated after Intubationwas diminished, despite validation that the ETtube was correctly placed. The respiratory thera-pist reported difficulty ventilating the patient. Bilat-eral needle thoracostomy was performed. A rightfemoral vein cordis was placed, as well as inser-tion of 2, large bore, 16-gauge, peripheral intra-venous catheters, A clot was sent off for type andcross. Normal saline solutions were administeredintravenously; the patient remained hypotensiveand bradycardic. On secondary survey the pa-tient was found to have the following:
Head: abrasions and scalp laceration with oc-cipital skull fracture
Chest: diminished breath sounds; CXR, nega-tive for hemothorax
Abdomen: multiple contusions, distended, hy-poactive bowel sounds
Pelvis: unstable to compression and palpationGU: absent rectal tone (paralytics on board
from RSI); meatus WNL; prostate WNLExtremities: dusky, delayed capillary refill, un-
able to palpate peripheral pulsesBack/spine: no obvious step offA foley catheter was inserted. Focused Abdo-
minal Sonogram for Trauma (FAST) was nega-tive. Blood for baseline laboratory studies wassent off, and radiological studies were ordered
Laboratory findings: ABG, pH 7.01; PCO2 68;P02 38; BE -13 ; HCO3 11.7%; OzSat 59%; O215L/min 100%; INR 1.5.
The patient remained hypotensive. Pulse var-ied widely between a low of 32 and high of 120.After infusion of warmed crystalloid, packed redblood cells and FFP the BP stabilized at 102 sys-tolic. Cardiac monitor demonstrated regular si-nus rhythm at 98. The trauma surgeon electedto transport the patient, with the trauma team inattendance, to radiology for CT scan.
CT results: Closed head injury with intra-parenchymal contusions; C-spine fractures atmultiple levels; T-spine fractures; open bookpelvic fracture, with intrapelvic blood vessel in-juries, multiple lower extremity fractures.
The case described above demonstrates thecomplex critical thinking processes requiredby trauma team members. This patient ex-hibited classic signs and symptoms of "trau-
matic" shock. Initially, he suffered from ob-structive shock as a result of tension pneu-mothorax. Further investigation revealed thatthe patient suffered from hypovolemic shockfrom pelvic fractures and internal injuries. Hehad also suffered distributive shock secondaryto cervical and thoracic cord transection asso-ciated with spinal column fractures. His life-threatening, multisystem injuries proved chal-lenging to sort out. However, hypovolemicshock must always be the primary consider-ation until ruled out.
TRIMODAL DEATH PATTERN
Researchers have identified 3 major epi-demiological events, or trimodal patterns ofdeath from trauma. Immediate deaths, thosethat occur on scene shortly after injury, ac-count for approximately 50% of deaths dueto trauma. These usually result from cata-clysmic events resulting in high central ner-vous system injuries, or devastating injuriessuch as lacerations to the heart or majorblood vessels. Early deaths occur within sev-eral hours and are typically the sequelae ofacute hemorrhage or traumatic brain injury.Late deaths may occur weeks after injury andare typically the result of infection or multisys-tem organ failure. The preponderance of datademonstrates that immediate and early deathsaccount for approximately 80% of trauma-related fatalities, with the majority as a re-sult of rapid exsanguination. There is a pre-ventable death rate associated with a failure torecognize and adequately treat patients at riskfor acute hemorrhage. This has been reportedas high as 27%. These data suggest that thedevelopment and implementation of a strate-gic approach to provide care for at-risk pa-tients could greatly improve outcomes. Goalsare aimed at early recognition, and adequate,timely treatment to reduce the overall deathrate.^
ROLE OF TRAUMA CENTERS
Trauma systems have been designed to getthe "right patient, to the right resources, in

4 CRITICAL CARE NURSING QUARTERLY/JAMJARY-MARCH 2005
the right time frame." Inclusive trauma sys-tems assure the availability of rapid transport,by adequately trained prehospital providers,to centers prepared to receive the critically in-jured patients. The "right resources" and des-tinations are typically trauma centers, whichare required to demonstrate rigorous physi-cal plant and care provider requirements. Theright time frame is sometimes referred to asthe "golden hour."' The cornerstone of thisapproach is the rapid recognition and earlyevaluation and treatment of severely injuredpatients.^ This early resuscitation phase hastypically taken place in emergency depart-ments; however, the resuscitation phase hasnow moved beyond the walls of the emer-gency department and now includes operat-ing room resuscitation and continued aggres-sive resuscitation in the intensive care unitGCU). Therefore it is imperative that nurses inthese arenas be proficient In the recognition,assessment, and care of the severely injuredtrauma patient.'
DEFINITION
As described in the literature, there aremultiple definitions of shock. In the 1870s,Samuel D. Gross described shock as the "rudeunhinging of the machinery of life."^ Onehundred years later, in the 1970s, G. T. Shiresdiscussed the severity of shock states as pro-portional to the depression in the cellularmembrane potential. He proposed that shockoccurs when the physiologically regulated cir-culation of blood fails to deliver sufficient oxy-gen to sustain aerobic metabolism to the cel-lular mitochondria. Therefore, resuscitationfrom shock is restoration of adequate oxy-gen deUvery to mitochondria. Organ failure,as shock sequelae, is proportional to the hy-poxic damage to intrinsic cellular function.'As defined by Advanced Trauma life Support(ATLS), shock is the consequence of insuf-ficient tissue perfusion, resulting in inade-quate cellular oxygenation and an accumula-tion of metabolic waste. The consequences ofuntreated shock are metabolic derangementsthat result in a vicious cascade to include hy-
pothermia, acidosis, and coagulopathy. If un-resolved, shock progresses to an irreversiblestate, resulting in multisystem organ failureand death.^ Others have further describedshock as a basic biochemical inability to prop-erly utilize oxygen and other nutrients, or aninappropriate or ampMed stimulation of cel-lular signaling cascades.^
SHOCK CLASSIFICATIONS
Although there are a variety of definitionsand methods of classification, "^ for the pur-poses of this discussion, shock is dividedinto 4 pathophysiologic categories: (1) hypo-volemic, (2) obstructive, (3) cardiogenic, and(4) distributive. All the 4 interfere with end-organ cellular metabolism. -*°
HYPOVOLEMIC SHOCK
Hypovolemic shock occurs as a result of de-creased circulating blood volume, most com-monly from acute hemorrhage. It may also bethe result of fluid sequestration w ithin theabdominal viscera or peritoneal cavity. Theseverity of hypovolemic shock depends notonly on the volume deficit loss, the time framewithin which the fluid is lost, but also on theage and preinjury health status of the individ-ual. Clinically, hypovolemic shock is classifiedas mild, moderate, or severe, depending onthe whole blood volume loss.'"
In mild or compensated shock, less than20% of blood volume is lost. Vasoconstric-tion begins and redistribution of blood flowis shunted to critical organs. Moderate shockreflects 20% to 40% of blood volume loss;there is decreased perfusion of organs suchas kidneys, spleen, and pancreas. In severeshock, greater than 40% of blood volume islost; there is decreased perfusion of the brainand heart. Hypovolemic shock produces com-pensatory physiologic responses in almost allorgan systems.10
Pathophysiology of hypovolemic shock
Hypovolemic shock usually means hem-orrhagic shock in the trauma patient. The

Hypovolemic Shock
patient may be bleeding internally or exter-nally, and as a result circulating blood vol-ume is decreased. This volume loss reducesboth preload and stroke volume and causesreduced cardiac output.
Signs and symptoms of early hypovolemicshock include an altered level of conscious-ness, sometimes manifested in agitation andrestlessness, or any central nervous systemdepression. Physical assessment may demon-strate nonspecific signs and symptoms such ascool, clammy skin, orthostatic hypotension,mild tachycardia, and vasoconstriction.'' Thebody is able to sustain blood pressure andtissue perfusion by employing compensatorymechanisms that primarily promote vasocon-striction to support an increase in intravascu-lar volume,^
Late signs of shock include worseningchanges in mental status to include coma, hy-potension, and marked tachycardia. It is im-portant to know, however, that healthy adultswith impending hemorrhagic hypovolemicshock may not become hypotensive untU asmuch as 30% of their circulating blood volumeis lost."
VASOCONSTRICTION
Vasoconstriction is an early compensatoryresponse mechanism to shock. The initial de-crease in blood pressure inhibits the afferentdischarge of baroreceptors in the aortic archand carotid sinus. This stimulates sympatheticnervous system output. The decrease in bloodvolume inhibits the discharge of stretch re-ceptors in the right atrium and also stimu-lates afferent discharge from chemoreceptorsin the aortic arch and carotid bodies. The re-sulting increased sympathetic tone causes therelease of catecholamines, epinephrine, andnorepinephrine, intensifying venous tone, in-creasing heart rate, myocardial contractility,and subsequently, cardiac output. This com-pensatory mechanism is an effort to improveperfusion to the vital organs and tissues,^It is important to understand, however,that not all patients in hypovolemic shockdemonstrate tachycardia. Patients who are on
/3-blockers are unable to mount a compen-satory tachycardia. Patients who have a con-comitant spinal cord injury cannot increaseheart rate in response to volume loss andhypotension due to inhibition of the sympa-thetic nervous system,"
This catecholamine release, causing arterio-lar constriction, does not affect all systems tothe same degree. The body preserves bloodflow to the heart and brain at the expenseof the gastrointestinal (GI) tract, the skin,and skeletal muscle. However, if the shockstate persists or worsens, myocardial func-tion eventually becomes impaired. The great-est decrease in circulation during vasocon-striction occurs in the visceral and splanchniccirculation. Intestinal perfusion is depressedout of proportion to reduction in cardiacoutput,'°
Blood flow to the kidneys is preservedwith a small to moderate hemorrhage; how-ever, the renal vessels will constrict w ithlarge blood loss. Eventually there is a de-cline in glomerular filtration and urine out-put. The kidneys require high blood flowto maintain cellular metabolism. Sustainedhypotension may result in tubular necro-sis. Blood flow to the liver is reduced butto a lesser extent than in peripheral tis-sue. Decreased circulation to the skin is re-sponsible for the coolness associated withhypovolemia,^
PLASMA VOLUME
Vasoconstriction causes a shift of fluidbetween the vascular compartment and theinterstitial spaces. Normally, there is littlefluid movement between these 2 compart-ments. In early or compensated shock, thereis a reduction in capillary hydrostatic pres-sure, w hich allows movement of protein-freefluid from the interstitium to the vascularspace, increasing intravascular volume anddecreasing interstitial volume. This extracel-lular fluid mobilization usually occurs overa 6- to 12-hour period. It is not responsiblefor large volume changes in early phases ofhemorrhagic shock,

CRITICAL CARE NURSING QUARTERLY/JANUARY-MARCH 2005
Decreased renal blood flow activates therenin-angiotensin system, stimulating produc-tion of angiotensin I, Angiotensin I is sub-sequently converted to angiotensin II, astrong vasoconstrictor that promotes aldos-terone release from the adrenal cortex. Si-multaneously, angiotensin II potentiates theaction of adrenocorticotrophic hormone onthe adrenal cortex and further promotesepinephrine release from the adrenal medulla,Adrenocorticotrophic hormone is releasedfrom the adrenal cortex, increasing renalsodium and water retention, as well as potas-sium excretion, which support the intravas-cular volume. Simultaneously, the posteriorpituitary releases additional antidiuretic hor-mone, or vasopressin, which promotes re-absorption of solute-free water in the distaltubules and collecting system of the kid-neys. It also further stimulates peripheralvasoconstriction,
CATABOLISM
During shock states, catecholamine out-put and glucocorticoid production createa catabolic state. Plasma concentrations ofglucagon rise. Together, catecholamines andglucagon promote glycogenolysis and lipoly-sis. As a result, hyperglycemia, as well as ele-vated lactate and fatty acid levels, may be ob-served as the shock state progresses.^
ACID-BASE DISTURBANCES
Acid-base disturbances are reflective ofthe shock state. Measures of anaerobicmetabolism include serum bicarbonate, pH,base excess, and lactate. In compensated,or mild to moderate, shock, the most fre-quently observed acid-base abnormality isrespiratory alkalosis. It is important to mon-itor blood gases on a regular basis. Hypoxicor hypotensive stimulation of the aortic andcarotid chemoreceptors, the presence ofmetabolic acidosis, and painful stimuli acti-vate the respiratory center, causing hyperven-tilation. As the shock state progresses, anaer-
obic metabolism predominates, stimulatinglactate production and subsequent metabolicacidosis. The resultant metabolic acidosis fur-ther exacerbates the shock state, decreasingsensitivity to catecholamines and stress hor-mones, resulting in decreased myocardial con-tractility, promoting predisposition to cardiacdysrhythmias,^
Lactic acidosis, the physiologic deficit re-sulting from inadequate perfusion, is reflectedin high serum lactate levels. The amount oflactate produced correlates with total oxygendebt, signifying the magnitude of hypoperfu-sion, the severity of shock, and also adequacyof resuscitation. Serum lactate is considereda sensitive indicator of occult shock and maybe useful in patients •with a significant mech-anism of injury yet demonstrating vital signswithin normal limits. Since the 1960s, sev-eral studies have pointed to increased deathrates associated with metabolic acidosis, as re-flected in arterial pH, lactate, and base deficitclearance,^'^ Base deficit is defined as theamount of base, measured in millimoles, re-quired to titrate 1 L of whole arterial blood toa pH value of 7,40, the sample is completelysaturated •with oxygen at 37°C, and has a PCO2of 40 mm Hg,' Base deficit is used as an indexof the severity of shock in the adequacy of re-suscitation, measuring global tissue acidosis.Some studies suggest a correlation betweenbase deficit and survival probability, althoughothers refute this,'^'''
Arterial blood gases assess acid base, ven-tilation, and oxygenation status in the in-jured patient. Hypoxemia contributes to tis-sue oxygen deficit present in hemorrhagicshock; therefore, measurement of arterialPCO2 helps drive decision making regard-ing the need for intubation and ventilatorysupport.
Treatments for metabolic acidosis are aimedat correcting the underlying cause: hypoper-fusion. Supporting adequate oxygen deliverythrough volume loading, transfusions, and ju-dicious inotropic support are used to achieveresuscitation goals of normal values in ar-terial pH, base deficit, lactate, and gastric

MONITORING DURING SHOCK ANDRESUSCITATION
Frequent assessment and reassessmentthrough continuous monitoring is necessaryto identify and correct the causes for cir-culatory compromise. Cardiac monitoringshould be initiated upon arrival and contin-ued throughout the critical care phase tomonitor and evaluate abnormalities in rateand rhythm. Persistent tachycardia, despiteaggressive resuscitation efforts, may indicateongoing hemorrhage. Rhythm disturbancesmay reflect a progressive shock state. On-going blood pressure monitoring, pulseoximetry, core body temperature, and urineoutput are all useful in assessing circulatorystatus. Urine output reflects renal perfusionand indirectly, overall central perfusion, Aurine output of 1 to 2 mL/kg per hour isnormal; output of less than 1 mL/kg per hoursuggests inadequate resuscitation and poorperfusion,^
Central venous pressure monitoring is typ-ically not initiated during early resuscitation,but may prove useful in patients with pro-longed and extensive resuscitation, includ-ing massive transfusion. It may be necessaryto establish central venous access in patientswhere adequate peripheral intravenous (TV)access has not been successful. It is alsoan adjunctive tool to aid in the diagnosisof undefined shock or measurement of vol-ume status in patients with CHF or renaldisease.^ Pulmonary artery catheter (PAC)placement may be considered in the criticalcare unit for patients suffering from undif-ferentiated shock, and to guide volume re-placement for patients with comorbid factorssuch as congestive heart failure and renalinsufficiency. Consideration for a PAC maybe useful in guiding resuscitation for pa-tients who are not hypotensive, but exhibitmore subtle signs of shock such as cool ex-tremities and elevated lactate levels.''* How-ever, PACs are invasive, time-consuming to in-sert and maintain, and carry certain risks ofmorbidity.
Hypovolemic Shock 1
OBSTRUCTIVE SHOCK
Obstructive shock refers to a symptom com-plex where mechanical obstruction interfereswith the ability of the heart to generate ade-quate cardiac output. Intravascular volume issufficient and the heart pumping action is ad-equate. Basically, "blood can't flow where itneeds to go." The most frequently describedcauses of obstructive shock are tension pneu-mothorax, pericardial tamponade, and pul-monary embolus. Recall our case study. Uponarrival to the trauma center, the patient wasintubated. However, the respiratory therapistreported difficulty ventilating the patient, de-spite the fact that correct endotracheal tubeplacement was confirmed. The trauma sur-geon performed a needle thoracostomy to re-lieve intrathoracic cavity pressure for a sus-pected tension pneumothorax.
In tension pneumothorax, air accumulatesin the intrathoracic cavity, causing compres-sion of the vena cava. As a result, venous re-turn to the heart is compromised, limiting car-diac output. This is a life-threatening situationand must be corrected immediately,
In pericardial tamponade, fluid accumu-lates in the pericardial space, elevating Ln-trapericardial pressure and impairing ventric-ular filling. As a result, stroke volume andcardiac output are reduced. As aortic pres-sure falls, coronary blood flow is reduced dur-ing a period of increased myocardial oxygendemand and, as a result, myocardial faUure,shock, and cardiac arrest may follow.'
CARDIOGENIC SHOCK
Cardiogenic shock is defined as the inabilityof the heart to maintain adequate tissue perfu-sion secondary to impaired pump function orfailure. In the presence of trauma, cardiogenicshock is likely the result of an acute myocar-dial infarction either from pretraumatic eventor from direct myocardial injury, Cardiogenicshock could also result from transection of acoronary vessel or chamber injury after a pen-etrating ^^

8 CRITICAL CARE NURSING QUARTERLY/FANUARY-MARCH 2005
DISTRIBUTIVE SHOCK
Distributive shock describes abnormalitiesin vascular resistance, causing maldistributionof blood flow. Some of the more commoncauses are sepsis, anaphylaxis, and spinal cordinjury.
From a pathophysiologic standpoint, lowvascular resistance increases intravascular ca-pacity. This expanded vascular capacity, in thepresence of a normal or low intravascular vol-ume, causes a functional hypovolemia, result-ing in inadequate tissue perfusion. Distribu-tive shock is also sometimes termed "warmshock." Spinal cord injury above the levelof Tl results in almost unopposed parasym-pathetic tone. These patients do not vaso-constrict and may not demonstrate the coolclammy skin commonly associated w ith hem-orrhagic shock, Transection of the cervicalspinal cord may impair cardiovascular con-trol. Unopposed vagal tone contributes to thebradycardia, loss of arterial tone, and the hy-potension witnessed in neurogenic shock. **
Septic shock, resulting from infection, isunusual in the early stages of acute trauma,except in the patient presented w ith grosslycontaminated wounds,'' Septic shock will bediscussed with multisystem organ failure, as itis a frequent sequela of hypovolemic shock,
DIFFERENTIAL DIAGNOSIS
Shock due to hypovolemia may be confusedwith, or confounded by, shock from othercauses. In some instances, there may be morethan one type of shock in play. Consider the el-derly patient who may have had a myocardialevent before his car crash, Cardiogenic shockproduces signs and symptoms as those foundin hypovolemia with the exception that theneck veins are usually distended. However, re-member that vein distention may not occur ifthere is inadequate circulating fluid volume,
Hypotensive patients who sustain highspinal cord injuries may be challengingdiagnostically. These patients will exhibithypotension secondary to peripheral vasodi-lation. This type of shock may be relatively re-
sistant to fluid administration. However, thepatient is typically bradycardic because of in-creased parasympathetic tone and the inhibi-tion of the sympathetic nervous system. Theteam must consider the possibility of spinalcord injury once hypovolemic shock is ex-cluded, How ever consider the major traumapatients with multisystem injuries w ho maybe suffering from both hypovolemic shockand spinal cord injury. However, it is imper-ative to assume that shock in spinal cord in-jury patients is due to hypovolemia, and notdue to neurogenic shock. Only after bloodloss is summarily ruled out, the physicianshould consider the diagnosis of neurogenic
Diagnosis is most challenging when morethan one cause is present. Another exampleis the patient who suffers a myocardial contu-sion from blunt trauma and w ho also has hy-povolemic shock from other injuries. Remem-ber that many trauma patients suffer injuriesto more than one system.
Drug and alcohol intoxication may alsomake the diagnosis of hypovolemia trouble-some. Serum ethanol elevation causes the skinto be warm, flushed, and dry. Urine is usu-ally dilute. These patients may be hypoten-sive when supine, with exaggerated changesin postural blood pressures measurements,Hypovolemic shock victims present as cold,clammy, oliguric, and tachyeardic,^''
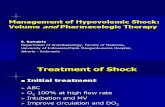
Treatment priorities
Throughout every phase of trauma care,the priorities of airway, breathing, and circu-lation are paramount. Problems encounteredin these areas must be addressed rapidly andsequentially. Sources of bleeding are contin-ually assessed, Hemodynamic monitoring isperformed on a continuous basis and changesreported to the trauma-attending physician.'"
FLUID RESUSCITATION
In the ICU, fluid resuscitation is carriedout in a more controlled fashion than in theacute posttraumatic situation. During initial

Hypovolemic Shock
resuscitation attempts, IV access is obtainedthrough the use of at least 2 large bore (14-16)gauge or larger catheters. Femoral cordis linesare commonly used in our institution whenthere are no contraindications for using thissite. The small ports on the pulmonary arteryand triple-lumen catheters are typically inade-quate for rapid fluid resuscitation and shouldbe used only after other large bore cathetersare in place,
INITIAL FLUID MANAGEMENT
The goal of fluid administration in thetrauma patient is to replace volume in or-der to support cardiovascular function by in-creasing cardiac preload and to maintain ade-quate peripheral oxygen delivery,'' Rapid fluidresuscitation is considered the cornerstoneof therapy by some for the initial manage-ment of hypovolemic shock, However, therehas been controversy over the years regard-ing the aggressive administration of TV flu-ids to hypotensive patients with penetratingtorso wounds. Research studies from the early1990s suggest that IV fluids should be de-layed until the time of definitive operativeintervention, '^' "
In young patients, volume infusion is typi-cally infused at the maximum rate allowed bythe equipment and the size of the cannulatedvein until a response is appreciated. In olderpatients or those with comorbid conditionssuch as cardiac disease, fluid resuscitation istitrated to response to avoid complications as-sociated with hypervolemia,'°
Attempting to reach normotension by thetransfusion of resuscitation fluids is not nec-essarily the goal. Much time can be lost chas-ing vital signs with fluid resuscitation when,in some injuries, early definitive operative in-tervention to stop blood loss is required,
CYSTALLOIDS VERSUS COLLOIDS
Parenteral solutions for the IV resuscitationof hypovolemic shock are classified as crys-talloid or colloid, depending on molecular
weight. Controversy exists regarding the ap-propriate choice of resuscitation fluid for thetrauma victim with mild to moderate hem-orrhage. The focus of this controversy cen-ters primarily on the effect each fluid typehas on the lungs. Proponents of colloid ther-apy argue that maintenance ofthe plasma col-loid oncotic pressure (PCOP) is necessary tominimize interstitial edema, particularly Ln thelungs. The concern is that massive crystalloidresuscitation creates an oncotic pressure gra-dient encouraging movement of fluid fromthe intravascular space into the pulmonaryinterstitium. Colloid supporters further pro-pose that since colloids remain primarily inthe intravascular space, they are more effec-tive volume expanders, and also are less likelyto cause peripheral edema than crystalloids.However, little support is found in the litera-ture to support superior efficacy of one solu-tion over the other.^'^
CRYSTALLOIDS
Crystalloid solutions are generally safe andeffective for resuscitation of patients in hypo-volemic shock. Isotonie human plasma solu-tions, with sodium as the principal osmoticactive particle, are used for resuscitation.They can be administered rapidly through pe-ripheral veins due to their low viscosity. Iso-tonie fluids have the same osmolality as bodyfluids; therefore, there are no osmotic forcesdirecting fluids into, or out of, intracellularcompartments. During resuscitation, isotoniecrystalloids are administered approximately3 to 4 times the assessed vascular deficit toaccount for the distribution between the in-travascular and extravascular spaces. Crystal-loids partition themselves in a manner simi-lar to the body's extracellular w ater content;75% extravascular and 25% intravascular Themajority of complications associated withthe use of crystalloid solutions are eitherbecause of undertreatment or because ofovertreatment.' '"'' '
The use of one specific crystalloid over an-other is largely a matter of institutional or

10 CRITICAL CARE NURSING QUARTERLY/JANUARY-MARCH 2005
provider preference. Normal saline is the onlycrystalloid that can be mixed with blood andblood products. Patients resuscitated withlarge amounts of normal saline are at riskfor developing hyperchloremic metabolic aci-dosis because its chloride concentration ishigher than that of plasma. Lactated Ringer'ssolution has the advantage of a more physio-logic electrolyte composition.
Hypertonic saline solutions are crystalloidsthat contain sodium in amounts higher thanphysiologic concentrations. They expand theextracellular space, by creating an osmoticeffect that displaces water from the intra-cellular compartments. Hypertonic saline de-creases wound and peripheral edema. Thereis some research to suggest, however, that hy-pertonic saline resuscitation may contributeto increased bleeding. ''*'"'
Most sources agree that the best way tomanage hypovolemic shock in trauma pa-tients is the judicious use of w armed TV fluidsand blood products. Many trauma centers ini-tially infuse 2 to 3 L of lactated ringers or nor-mal saline and then consider blood products ifthe patient remains symptomatic. While crys-talloids are infusing, the blood bank has timeto type and cross-match the patient for trans-fusion of type-specific blood.'°"
COLLOIDS
Colloids are solutions that have a higher-molecular-weight species and create an os-motic effect. Colloids remain in the in-travascular space for longer periods thando crystalloids. Smaller quantities are re-quired to restore circulating blood volume.Colloids attract fluid from the extravascu-lar to the intravascular space because oftheir oncotic pressure. Examples are albumin,hetastarch, dextrans, modified fluid gelatin,and urea bridge gelatin. They are expen-sive to use and complications have been re-ported Ln their use. Albumin has been im-plicated in decreased pulmonary function,depressed myocardial function, decreasedserum calcium concentration, and coagula-tion abnormalities.'" Hetastarch may cause
decreased platelet count and prolongation ofthe partial thromboplastin time. Several com-plications have been associated with the useof dextran, to include renal failure, anaphy-laxis, and bleeding. Gelatins are associatedwith anaphylactoid reactions. They also maycause depression of serum fibronectin. Be-cause ofthe high cost and complication rates,there appears to be no clear advantage to us-ing colloid solutions,'*'"'
Blood products and component therapy
Neither crystalloid or colloid solutions in-crease oxygen-carrying capacity. Administra-tion of large amounts of fluids can also provedetrimental by diluting hemoglobin levels andcontributing to fluid volume overload.''
Blood products are currently the most read-ily available fluids to increase oxygen-carryingcapacity and cardiac preload. However, trans-fusions carry the risk of various blood-bornepathogens and transfusion reactions. Thereis considerable debate regarding indicationsfor transfusion. Patients with hemorrhage ofup to approximately 20% of their total bloodvolume can be safely volume replaced withcrystalloids in a ratio of 3 mL of crystalloidper milliliter of estimated blood loss. Dur-ing the infusion of crystalloids, the bloodbank has time to perform a type and cross-match, so that, if needed, type-specific bloodis available for transfusion. Most agree thatpatients with 20% to 40% loss of circulatingblood volume, or those demonstrating evi-dence of hemodynamic instability, and thosewith blood gas evidence of shock, despite ag-gressive fluid resuscitation, may benefit fromblood transfusions, '
BLOOD TYPES AND Rh ISSUES
The decision to transfuse should be basedon the assessment of ongoing blood loss, thepatient's ability to compensate, and the avail-ability of cross-matched blood products. Ad-ditional considerations are given to the pa-tient's age and presence of comorbidities,^Ultimately, type-specific blood products are

Hypovolemic Shock 11
preferred, but w hen a patient arrives in ap-parent shock or extremis, the universal donortype O, Rh negative, is transfused using a rapidinfusor/warmer device.
Rh-negative blood may be in short sup-ply; therefore, some hospitals have poli-cies in place that allow Rh-positive GroupO, packed red blood cells (PRBCs) to betransfused in men, and women older thanchildbearing age. The rationale behind thispractice is that naturally occurring anti-Rhbodies do not exist, therefore there is no ad-vantage to the use of Rh-negative blood. How-ever, there is some concern that Rh-negativepatients may have been sensitized from preg-nancy or previous transfusions and could de-velop a delayed hemolytic transfusion reac-tion from Rh-positive blood use. This is a rareoccurrence; therefore, O-Rh-positive PRBCsare considered the first choice for emergencytransfusions, with consideration for the use ofO-Rh-negative PRBCs for females with child-bearing potential.^ Some sources recommendthat the number of transfusions of type O belimited to 4 units, after which type-specificblood should be available in most institutionsreceiving trauma patients. However, whennecessary, type O blood may be continueduntil the patient stabilizes or type specific is
that can be used in conjunction with bloodproduct transfusion, Lactated Ringer's solu-tion w ill cause precipitation of blood w ithin
Type-specific blood is ABO and Rh compat-ible and is available within less than 15 min-utes in most institutions. Type-specific bloodhas been shown to be safe and effective dur-ing emergency resuscitations.18
MASSIVE TRANSEUSION
Trauma practitioners are frequently facedwith situations that require decision makingto weigh the risks and benefits of massivetransfusions. When the decision is made toproceed, there are technological considera-tions that affect infusion rates. Large borecatheters, as well as high-volume IV tubing, al-low for the fastest blood administration. Pres-sure bags and/or mechanical rapid transfusiondevices further increase flow rates. Remem-ber that normal saline is the only fluid additive
BLOOD COMPONENT THERAPIES
At this writing, component therapy remainsthe current standard for blood transfusion.It refers to the utilization of the compo-nents of whole blood to include RBCs, freshfrozen plasma (FFP), platelets, and cryopre-cipitate. One unit of whole blood contains200 mL of red blood cells and 250 mL ofplasma, which contains coagulation factors.Component therapy has several advantagesover whole blood, and evidence suggests thatthe PRBCs and component therapy are aseffective as whole-blood transfusion withoutthe disadvantages. PRBCs and componentsare more readily available and are less expen-sive and easier to store than whole blood. Vol-ume expansion can be accomplished w ith acombination of crystalloids and PRBCs, An-other advantage of component therapy overwhole blood is that infusions can be tailoredspecifically to the needs of the individual pa-tient. Furthermore, PRBCs increase oxygen-carrying capacity more efficiently than wholeblood. The disadvantage of whole blood isthat platelets are not w ell preserved, and clot-ting factors decrease rapidly at blood storagetemperatures. For these reasons, PRBC infu-sion with component therapies are consid-ered the methods of choice for increasing redblood cell mass and oxygen-carrying capacityin hemorrhagic shock,
COMPUCATIONS OF TRANSFUSIONS
Blood-borne pathogens
Improved screening has significantlydecreased the incidence of blood-bornepathogens or transfusion-transmitted diseases(TTDs),- However, they still contribute tothe incidence of late death from transfusion.Increased awareness and concerns relatedto TTDs, especially HIV infection, have

12 CRITICAL CARE NURSING QUARTERLY/JANUARY-MARCH 2005
prompted caution and reconsideration ofblood transfusion indications. Hepatitis B isthe most common infectious complication.Before testing for hepatitis C, non-A non-Bhepatitis was the most frequent infectiouscomplication,'^
Transfusion reactions
Transfusion reactions are categorized intohemolytic and nonhemolytic types. Majorhemolytic transfusion reactions occur as a re-sult of the interaction of antibodies in theplasma of the recipient with antigens presentin the red cells of the donor. It is importantto stress that the majority of hemolytic reac-tions are due to clerical error in the identifi-cation of blood samples or in the administra-tion of properly cross-matched blood to thewrong patient. During high-stress situationsof massive transfusion administration, metic-ulous attention must be paid to the processessurrounding blood banking and blood prod-uct administration to avoid this preventablecomplication,'^
Nonhemolytic transfusion reactions aremore common and related to reactions toleukocytes or proteins in the donor blood.These may be mitigated by premedicationwith antipyretics and antihistamines. Typi-cal reactions may be mild, consisting of rashor nuld bronchoconstriction. More rare aresevere responses such as subglottic edema,severe bronchoconstriction, and anaphylaxiswith cardiovascular collapse,'^
Platelet and coagulation factors
Along with the previously mentioned con-cerns for blood-borne pathogens and trans-fusion reactions, there are several othercomplications related to blood product trans-fusions, with higher complications rates asso-ciated with massive transfusion therapy, oftenconsidered 10 U or more. Massive transfusionof blood products and concurrent infusion oflarge volumes of crystalloid cause certainhematologic and physiologic consequences.
Not only do coagulation factors and plateletnumbers and function diminish during RBC
storage, the massive blood and fluid admin-istration further dilutes the number of cir-culating platelets. This dilutional thrombocy-topenia causes clotting abnormalities. It isimportant to assure that there is appropri-ate and timely administration of platelets andFFP to prevent this complication. Treatmentshould be based on clinical evidence of im-paired hemostasis, by following prothrombintime, partial thromboplastin time, and plateletcount. While circulating platelet counts of20,000 per mm^ or fewer may be adequatein nonbleeding patients, platelet transfusionis appropriate for patients with evidence ofongoing microvascular bleeding with levels of100,000 per mm' (see references 4 and 19),
Massive transfusion therapy can contributeto significant electrolyte and acid-base distur-bances. Among these are hypocalcemia, hy-perkalemia, and hypokalemia, Hypocalcemiaoccurs during massive transfusion, becauseeach unit of PRBCs contains citrate, whichbinds to ionized calcium in the blood. Largecitrate doses may be toxic and can precipi-tate hypocalcemia. Clinical signs of hypocal-cemia include prolongation of the QT seg-ments on ECG, skeletal muscle tremors, andperioral tingling. Calcium levels should beclosely monitored during massive transfu-sion therapy. Citrate also may contributeto hypomagnesemia. Because of this re-lationship, treatment of hypocalcemia andhypomagnesemia includes concomitant useof calcium chloride and magnesium chlo-ride in massive transfusion, based on mea-sured serum levels; empiric treatment is not
Banked blood contains significantly ele-vated potassium levels because of cell lysisthat occurs during the collection and stor-age of blood, Hyperkalemia, however, is rareduring massive transfusion, because packedcells quickly reestablish their ionic pump-ing mechanism and potassium is rapidly ab-sorbed. In actuality, hypokalemia occurs morefrequently secondary to transient metabolicalkalosis occurring during massive transfu-sion, which causes potassium to move intothe ^ ' ^

Hypovolem ic Shock 13
Acid-base disorders are commonly associ-ated with large volume transfusions. Eventhough banked blood is acidic because of itscitrate content, metabolic acidosis is not typi-cally a result ofthe transfusions, but is relatedto underlying hypovolemic shock. Treatmentshould concentrate on improving tissue per-fusion and oxygenation as well as an ongoingsearch for underlying sources of hemorrhage.Sodium bicarbonate administration is not rec-ommended and has several detrimental sideeffects. In rare circumstances, a trauma pa-tient may have metabolic acidosis due to acause other than hypovolemia, such as comor-bid factors to include diabetic ketoacidosis,carbon monoxide (CO) poisoning, drug, ortoxic ingestion,^
HYPOTHERMIA
Hypothermia is a serious consequenceof massive blood product transfusion. Pro-gressive core hypothermia with persistentmetaboUc acidosis is the precursor of se-vere and ongoing coagulopathy states,^ Thereare complex pathophysiologic interactionsat play that contribute to impaired coagula-tion. Mikhail refers to the physiologic lim-its of the body in response to hypovolemicshock as "the trauma triad of death"; hy-pothermia, acidosis, and coagulopathy' Hy-pothermia has been strongly implicated inthe development of acidosis and is frequentlydemonstrated as a consequence of severe in-jury and routinely prescribed resuscitationefforts,'"^ Studies suggest that as many as twothirds of all trauma patients arrive at emer-gency departments with hypothermia, regard-less of geographic locale,' *' Many trauma pa-tients develop hypothermia at some pointin their treatment and this is poorly toler-ated. Hypothermia occurs in trauma patientswith minimal cold stress secondary to in-adequate tissue oxygenation and perfusion,preventing the body from generating enoughheat to maintain normothermia,^' Predispos-ing factors are age, injury severity, impairedthermogenesis, elevated serum alcohol lev-els, fluid resuscitation, blood product trans-
fusions, and exposure of body cavities duringsurgery.'
Gentilello classifies hypothermia in traumapatients into 3 risk categories based on corebody temperature. Mild hypothermia (34°C-36°C) accelerates oxygen consumption inan at-risk patient population. Moderate hy-pothermia (32°C-34°C) further slows physio-logic functions. Severe hypothermia (<32°C)is considered a life-threatening emergency.^'
There are a number of adverse clinical ef-fects related to hypothermia. These are car-diac dysrhythmias, reduction in cardiac out-put, increasing systemic vascular resistance,increased lactic acid production, and coagu-lopathic bleeding. Hypothermia has a deleteri-ous effect on the oxyhemoglobin dissociationcurve, shifting it to the left, w hich impairsoxygen delivery and worsens the shock
Many research studies have directly linkedthe presence of hypothermia in trauma pa-tients with high mortality rates.'^"^' The pri-mary goal is to identify those patients at riskand to intervene in this cycle of hypothermia,acidosis, and coagulopathy' Core tempera-ture should be monitored continuously. At ourinstitution we use a foley catheter with a ther-mal measuring device that provides contin-uous core temperature measurement. Effortsto prevent hypothermia should be employedsuch as using a high-volume fluid warmer dur-ing massive transfusion therapy.
Based on these findings, the surgical ap-proach to the care of the severely injuredtrauma patient has changed over time. Earlyon, the goal of trauma surgeons was to pro-vide definitive operative intervention by per-forming a traditional exploratory laparotomy,where all injuries were identified and re-paired. Patients would spend long periodsof time in the operating room, receiving flu-ids, blood products, and with open peri-toneum, resulting in core thermal tempera-ture loss. Predictable evaporative heat losswith an open peritoneum, despite state-of-the-art resuscitation procedures, is 4,6°C perhour, ^ Patients w ould leave the operatingroom cold and coagulopathic. Currently the

14 CRITICAL CARE NURSING QUARTERLY/JANLIARY-MARCH 2005
goal in trauma operative resuscitation is toperform "damage control" or staged laparo-tomy. This initial procedure is abbreviatedand intended to control hemorrhage and con-tamination, pack the abdomen, perform tem-porary closure of the abdominal wall, andmove the patient quickly to the ICU for fur-ther stabilization and rewarming procedures.Stopping or abbreviating the initial procedureallows the trauma team to correct coagu-lopathy, maximize oxygen delivery, and re-verse acidosis and hypothermia. Followingstabilization in the ICU, the patient can re-turn to the operating room for a more con-trolled completion ofthe surgical procedure,^Again, the goal is to prevent the triad of hy-pothermia, acidosis, and coagulopathy, be-cause of the high mortality associated withthis syndrome,' As we compress the timeframes through which we move our patientstow ard definitive operative intervention, itis imperative that critical care nurses un-derstand their role in intervening in thispathogenesis.
Rewarming techniques
The selection of rewarming techniques isbased on how severely hypothermia is affect-ing the patient. Stable patients who are mildlyhypothermic, and without life-threatening in-juries, are typically treated with passive exter-nal rewarming techniques. Passive rewarmingtechniques involve removing wet clothing, in-creasing ambient room temperature, decreas-ing airflow^ and insulating the patient, and al-lowing his or her metabolic heat to increasebody temperature.
Active external rewarming techniques in-clude warm fluid circulating, convection air,"space blankets," and radiant heat lamps.Head covering is important, as 50% of radi-ant heat loss occurs from the scalp. Thesestrategies are typically more effective in pre-venting hypothermia than in treating it. Itshould not be the sole source of rewarmingfor patients exhibiting an adverse response tohypothermia, as results are not immediatelyeffective.
Active core rewarming techniques includethe administration of warmed humidified air,heated body cavity lavage to include peri-toneum and pleura, and warmed IV fluidinfusion and blood transfusions. Patients re-quiring large boluses of fluid for resuscita-tion as well as blood products can receive asubstantial amount of heat through warm IVfluids,
Extracorporeal circulatory rewarming tech-niques, such as cardiopulmonary bypass,venovenous, or arteriovenous, are the most ef-ficient rew^arming methods. However, they re-quire large bore vessel cannulation, especiallytrained technician and dedication to the duty.Therefore, these procedures are typically re-stricted to a few tertiary centers.^'
Coagulopathy
Coagulopathy, or hypocoagulability aftermajor trauma, is common in severely injuredpatients and recognized as a major causeof early death. There are many contribut-ing factors, and the pathophysiologic rela-tionships are complex. Little progress hasbeen made in correcting this phenomenononce it develops. Virtually all normal physi-ologic clotting mechanisms are severely de-ranged in the cold, acidotic, bleeding traumapatient. The clotting cascade, governed bya series of temperature sensitive reactions,is inhibited during episodes of hypothermia.Clotting abnormalities are exacerbated whencore body temperature falls below 34°C,Platelet function is also affected by lo w bodytemperatures.
Treatment for hypovolemia includes infu-sion of cystalloids and blood products, Coag-ulopathy becomes clinically important duringmassive transfusion therapy. Coagulation fac-tors are rapidly depleted. During shock, hep-atic function is impaired, impacting the abilityofthe liver to rapidly mobilize additional coag-ulation factors. Prothrombin time and partialthromboplastin time should be carefully mon-itored. Transfusion of FFP and platelets shouldbe administered on the basis of the results ofcoagulation profiles."*

Hypovolemic Shock 15
BLOOD SUBSTITUTES
Despite advances in detecting TTDs, con-cerns StiU remain regarding the risk oftransmitting hepatitis and human immun-odeficiency virus (HIV) during transfusiontherapy. There are reports of PRBC countshortages every year, and storage of red bloodcells has finite limitations. As a result, thereis a great deal of interest in the developmentof blood substitutes as an alternative choicein the treatment of hypovolemic shock. Un-like blood, hemoglobin substitutes requireno cross-match, have a long shelf life, andreportedly carry no risk of blood-borne vi-ral pathogens. Additionally, since they havea lower viscosity than blood, flow throughsmall capillaries may be enhanced, which po-tentiates peripheral oxygen delivery,'*'' ' Pre-clinical studies showed hemoglobin substi-tutes to be as effective as blood and moreeffective than standard colloid or crystalloidsolutions for resuscitation from hemorrhagicand septic shock. The hope was to providean immediate on-site replacement for trau-matic blood loss, prevent tissue ischemia andorgan failure, and provide effective hemo-dynamic support for septic-shock-inducedhypotension. '•• '*
Recent research supports the concept thatpostinjury multiple organ failure is relatedto inflammatory response. Biologic media-tors present in stored blood have been im-plicated in early postinjury hyperinflamma-tory syndrome and multiple organ failurethrough priming of circulating neutrophils.Some newer hemoglobin-based substitutesare free of priming agents and may pro-vide an alternative to transfusing PRBCs inthe early postinjury phase, • '*' ^ Human-polymerized hemoglobin (PoIyHeme®) is auniversally compatible, pathogen-free, read-ily available, oxygen-carrying blood substitutebeing developed for use in case of urgentblood loss. Recent study shows that this com-pound increases survival in patients with life-threatening red blood cell levels by maintain-ing hemoglobin levels in the absence of redcell transfusion,'^' The Food and Drug Admin-
istration has approved transfusion of up to10 consecutive units of polytteme for acutebleeding. Stage 3 clinical trials are currentlyin process in several trauma centers,
SHOCK SEQUELAE
Systemic inflammatory responsesyndrome
Systemic inflammatory response syndrome(SIRS) describes the pathophysiologic re-sponse to a cascade of events precipitatedby shock. Usually after trauma, a controlledinflammatory response occurs, which is de-signed to heal wounds and w ard off infection.However, continuous stimulation or severe in-fection may result in a sustained inflammation(SIRS), The result is an imbalance of cellularoxygen supply and demand, which results inoxygen extraction deficit. This inflammatoryresponse may occur without any source ofbacterial infection.^
Overwhelming SIRS occurs with persistentstimulation disrupting anaerobic cellular cy-cles. Disruption in the process of cellularmetabolism promotes a cascade of events in-cluding promotion of adhesion of molecules,catecholamines, chemotaxis, and a coagula-tion cascade. There is an accompanying de-crease in vascular resistance resulting in pro-found increased cardiac index, designed topromote oxygen delivery and cellular oxy-gen uptake. This hypermetabolic demand,coupled with acute deficit in oxygen ex-traction and metabolic failure, is precur-sors of multiple organ dysfunction syndrome
MODS
Historically, infection has been consideredthe cause of SIRS and MODS. Typical sourcesof infection are IV catheters placed in the pre-hospital environment or emergency depart-ment. Also implicated are urethral cathetersand endotracheal tubes. Decreased gastricacid allows for increased numbers of bac-teria to survive and multiply, theoretically,allowing translocation of bacteria in the

16 CRITICAL CARE NURSING QUARTERLY^ANUARY-MARCH 2005
distal bowel, theoretically resulting in highpneumonia rates, ^
Studies show that approximately 60% oftrauma patients will have clinical signs ofsepsis without an apparent bacterial source.Sepsis, and the ensuing multiple organ fail-ure, remains a leading cause of death inthe surgical ICU, despite significant advancesmade regarding the management of traumavictims. ^ Sepsis is characterized by increasedoxygen consumption, and increased car-diac index w ith decreased vascular resis-tance. These are indicators of the hyperdy-namic cardiovascular state associated withsepsis,'
The process of an uncontrolled inflamma-tory response with a progression to MODSis recognized as a defect in cellular signal-ing. Recall the previous discussion of trimodaldeath patterns following major traumatic in-jury. Late deaths may occur 5 to 4 weeks af-ter the initial shock episode. Inadequate earlyresuscitation has been implicated in the cas-cade of acidosis, hypothermia, and coagu-lopathy. This triad leads to multisystem or-gan failure and death. Lee and others describethe initial response to shock and develop-ment of SIRS, followed by progressive organfailure. This continuum is initiated and per-petuated by inflammation and inflammatorymediators.^^
These topics are complex, requiring in-depth discussion and, as such, are beyond thescope of this overview article, How ever, it isimportant for the critical care nurse to ex-plore ongoing research regarding cytokines,complement activation, and lipid mediators.Studies are currently adding to the body ofknowledge regarding inflammatory responseand multisystem organ failure after hypov-olemic shock.
As compensatory mechanisms continue tofail, tissue ischemia results from hypoperfu-sion as blood flow is shunted away from tis-sues with high metabolic demands, eitherfrom microvascular injury or from inflamma-tory response. Organ system failures com-monly seen are pulmonary, hepatic, and renalfailure. When 3 or more systems are affected.
the mortality rate climbs as high as 80% to
End points of resuscitation
At what point does one determine that re-suscitation is complete? Many researchers usethe same clinical, physiologic, or laboratorystudies to identify subtle hypoperfusion andto determine when adequate or normal perfu-sion resumes following resuscitation. Typicalend points are blood pressure, heart rate, andurine output,'"^ However, recent studies sug-gest tissue hypoperfusion can persist despitenormal vital signs. Cardiac and pulmonaryfunction can be monitored fairly accurately inthe ICU with current technology. By contrast,tissue perfusion, which represents circulatoryfunction ofthe peripheral tissues, is measuredindirectly by a variety of subjective symptoms,such as vital signs, pulse rate and quality, skintemperature, color, and moistness as well asmental status. These assessments are routinelyused to infer circulatory status and tissue per-fusion, but they are not direct quantitativemeasurements of tissue perfusion, ^ The chal-lenge is to identify those patients at risk forhypoperfusion; it may be present despite nor-mal cardiac indices, '* Other modes of assess-ment, to include gastric tonometry, transcu-taneous oxygen, and CO2 measurements, arecurrently being utilized as early warning signsof tissue hypoxia and hemodynamic shock incritically ill patients.'"
If we go back and review the defmitionof shock as the consequence of insufficienttissue perfusion, resulting in inadequate cel-lular oxygenation, what parameters do w echoose to measure cellular oxygenation andtissue perfusion? In patients with inadequatetissue perfusion, oxygen delivery is insuffi-cient for the generation of adenosine triphos-phate. Without adenosine triphosphate, thebody cannot sustain normal cellular func-tion. Anaerobic metabolism and tissue aci-dosis are results, CO2 levels increase in thesplanchnic or gut circulation. Successful re-suscitation from shock is measured by a lim-itation of oxygen debt and tissue acidosis

Hypovolemic Shock 17
with the return of aerobicClinicians rely upon both global and organ-specific parameters to measure end productsof inotropic metabolism to determine if com-plete resuscitation has been achieved. Basi-cally, global indexes measure overall degree ofhypoperfusion, based on a number of readilyavailable data sets. Some of these include thefollowing.
Oxygen delivery index
Oxygen delivery index (DO2D (normalvalue 500-600 mL/min/m^) is determined byCO (carbon monoxide), hemoglobin satura-tion, and the ability of the lungs to load oxy-gen onto the hemoglobin molecule. In severehemorrhagic shock, there is a decrease in cir-culating hemoglobin, which influences thiscomponent of oxygen delivery.
Cardiac output is affected by several clinicalconditions related to trauma, to include acutemyocardial infarction, hypovolemia, septicshock, neurogenic shock, cardiac contusion,and pericardial tamponade.
Pulmonary function relative to oxygendelivery is affected by the presence ofpneumothorax, hemothorax, flail chest, pul-monary contusion, loss of effective airway, in-adequate mechanical ventilation, and othersequelae of trauma, to include pneumonia,atelectasis, excessive secretions, and patientpositioning. In a severely injured patient, itis common to exhibit abnormal DO2I val-ues based on any, or all, of these clinicalfactors.
The oxygen consumption index value(normal value, 125 mL/min/m^) may mea-sure 4 or 5 times the norm in a criticallyinjured patient. Some causes of increasedVO2I include pain, agitation, posturing,fever, increased w ork of breathing, andtachycardia.
Mixed venous oxygen saturation
Continuous mixed venous oxygen satura-tion (SVO2) monitoring reflects how muchoxygen was consumed by the tissues. Patients
requiring aggressive resuscitation will demon-strate abnormally low values because of ei-ther inadequate oxygen delivery or excessiveoxygen demand by the tissues. Normal val-ues for SVO2 are between 65% and 80%; whenvalues fall below 50%, anaerobic metabolismis present, A low VO2 tells us that the pa-tient is underresuscitated, or still in shock, butit is nonspecific as to the cause. This tech-nology requires invasive monitoring via a PAcatheter, which is associated with significantmorbidity to include improper catheter place-ment, pneumothorax, infection, and equip-ment malfunction, ^
Arteriovenous carbon dioxide gradient
The gradient between arterial and mixedvenous PACO2 levels reflects the degree andduration of hypoperfusion and is an excel-lent barometer of the degree of hypovolemicshock. Normally, CO2 is cleared Ln the pul-monary circulation, but in profound shockthere is a decrease in cardiac output and poorpulmonary blood flow, resulting in an accu-mulation of PACO2 in the tissues, A gap greaterthan 11 mm Hg suggests severe compromise.While arteriovenous carbon dioxide gradient(AVPACO2) provides a general assessment re-garding the effectiveness of resuscitation ef-forts, it does not provide specific organicinformation, '
There have been recent technological ad-vances that may provide more informa-tion regarding organ-specific or regionalresuscitation effectiveness. These are tonom-etry, capnometry, and near-infrared spec-troscopy. We will discuss their use in mea-suring specific intracellular tissue response toresuscitation.
Gastric tonometryGastric tonometry assesses gastric mucosal
pH as a marker of the adequacy of resusci-tation, evaluating perfusion at the splanch-nic bed. The GI tract is very sensitive toany decrease in circulating volume and maysignificantly compromise gut perfusion. This

18 CRITICAL CARE NURSING QUARTERLY/JANUARY-MARCH 2005
technique involves the use of a nasogastrictube with a saline-filled, gas-permeable sili-cone balloon at the tip to measure CO2 emit-ted from the gastric cells, PACO2 is then con-verted to a pH value. A pH value less than 7,35suggests anaerobic metabolism, a potentiallynegative predictor of adequate splanchnicperfusion, raising the patient's risk for MODSand sepsis. Studies however are not conclu-sive, yet there are indications that gastrictonometry warrants consideration as a use-ful assessment tool in measuring gastric tissueperfusion.^^
Subiinguai capnometry
Recent research involving both animal andhuman subjects suggests that measurement ofthe proximal GI tract using sublingual PACO2strongly correlates with decreases in distal gutblood flow and increases in lactic acid dur-ing shock states. Since it is a relatively simple,noninvasive procedure, it has potential as anearly triage resuscitation tool,' ' A microelec-trode CO2 probe is placed under the tongue,providing continuous information regardingtissue perfusion ofthe proximal GI tract. Con-tinued research is necessary, but early indica-tors are promising.
Near-infrared spectroscopyNear-infrared spectroscopy is another tech-
nology on the horizon that may show promiseas a guide to end points of resuscitation.Minimally invasive, it measures intracellularoxygen levels, quantifies intracellular func-tion, and identifies other conditions thatmay affect intracellular metabolism,^^ It as-sesses the absorption of infrared light by satu-rated hemoglobin molecules and cytochrome-a,a^. It works by passing light waves viaprobes through muscle tissue. The devicedisplays levels of saturated hemoglobin andcytochrome-a,a3 to alert providers to organ-specific hypoxia or to indicate successfulresuscitation efforts through the reappear-ance of reflected red light. It holds promise
in predicting patients at risk for multisys-tem organ failure early in the course ofresuscitation.
Both global parameter management suchas SVO2, lactate, and base deficit are helpfulin determining decompensation or improve-ment in resuscitation states. Care providersshould not be lulled into a false senseof security, when vital signs and basichemodynamic parameters fall within nor-mal limits during resuscitation. New tech-nologies measuring regional tissue perfusionmay be an adjunct tool in this assessmentprocess.29
SUMMARY
Shock is a complex physiologic state, re-sulting in extreme dysfunction of cellular bio-chemistry, resulting inadequate tissue perfu-sion, and cellular death, Hypovolemic shockis most commonly seen in major trauma pa-tients, although the major trauma victim is ad-ditionally at risk for cardiogenic, obstructive,and distributive shock. Differential diagnosescan be complex.
Resuscitation from shock is restorationof adequate tissue perfusion. Early identi-fication and aggressive treatment is neces-sary to prevent or mitigate the effects ofshock states, SIRS and MODS, Current ther-apies are not without controversy. Ongoingresearch is aimed at further understand-ing the complex biochemical and physi-ologic responses to shock, to guide fur-ther development of appropriate treatmentmethodologies.
The critical care nurse remains a key mem-ber of the trauma team as resuscitation mea-sures are continued into the critical care en-vironment. It is imperative that the criticalcare nurse understand the trauma patient'scomplex physiologic response to injury, befamiliar with methods to monitor for keyindicators of shock states, and respond asa team member to provide timely and ag-gressive treatment to achieve positive patientoutcomes.

REFERENCES
Hypovolemic Shock 19
1, Mower-Wade D, Bartley M, Chiari-Allwein J.Shock: do you know how to respond? Nursing.2000;30(10):34-40,
2, Stern SA, Bobek EM, Resuscitation: managementof shock. In: Ferrera PC, Colucciello SA, Marx JA,et al,, eds. Trauma Management: An EmergencyMedicine Approach. St Louis: Mosby; 2001:75-102,
3, Bell RM, Krontz BE. Initial assessment. In: Mattox KL,Feliciano DV, Moore EE, eds, Traunia. 4th ed. NewYork: McGraw-HiU; 2000,
4, Scalea TM, Boswell SA. Initial management of trau-matic shock. In: McQuillen K, Von KA, Rueden KT,Nartsock RL, Flynn MB, Whalen E, eds. TraumaNursing: From Resuscitation Through Rehabilita-tion. 3rd ed. Philadelphia: WB Saunders; 2002:201-221,
5, Mikhail J, The trauma triad of death. AACN Clin Is-sues. 1999;10(l):85-94.
6, Cairns CB. Rude unhinging of the machinery of life:metabolic approaches to hemorrhagic shock. CurrOpin CritCare. 2OOl;7(6):437-443,
7, Muliins RJ. Management of shock. In: Mattox KL,Feliciano DV, Moore EE, eds. Trauma, 4th ed. NewYork: McGraw-Hill; 2000:195-229.
8, Advanced Trauma Ufe Support Course for Doc-tors {Instructor Course Manual). Shock. 6th ed.Chicago: American College of Surgeons; 1997.
9, Vary TV, McLean B, Von Reuden KT. Shock andmultiple organ dysfunction syndrome. In: McQuillenK, Von KA, Rueden KT, Nartsock RL, Flynn MB,Wlialen E. eds. Trauma Nursing: From Resuscita-tion Through Rehabilitation. 3rd ed. Philadelphia:WB Saunders; 2002:173-200.
10. Bongard FS. Shock and resuscitation. In: BongardFS, Sue DS, eds. Current Critical Care Diagnosisand Treatment. 2nd ed. New York: Lange MedicalBooks/McGraw-Hill; 242-267; 2002.
11. Cohen S. Shock. In: Cohen S, ed. Trauma NursingSecrets. PhUadelphia: Hanley and Belfus; 2003:109-114,
12. Davis JW, Shackford SR, Holbrook TL. Base deficitas a sensitive indicator of compensated shock intissue oxygen utilization. Surg Gyencol Obstet.1991;173:473-476.
13. Husein FA, Martin MJ, MuUinex PS, Steele SR, ElliotDC. Serum lactate and base deficit as predictors ofmortality and morbidity. Am f Surg 2003;185(5):484-491,
14. Kaplan LJ, Me Partland K, Santora TA, Trooskin SZ.Start with a subjective assessment of skin tempera-ture to identify hypoperfusion in intensive care unitpatients./ Trauma. 2001;50(4):620-628.
15. Bickell WH, Wall MJ, Pepe PE, et al. Immediate ver-sus delayed fluid resuscitation for hypotensive pa-tients with penetrating torso injuries. A' FnglJ Med.1994;331:1105-1109,
16. Trunkey DD. Prehospital fluid resuscitation. In:Trunkey DD, Lewis FR Jr, eds. Current Therapy ofTrauma. 4th ed. Chicago: Mosby; 1999:129-130.
17. Schierhout G, Roberts I, Alderson P, Bunn F, Colloidsversus crystalloids for fluid resuscitation in criticallyill patients, Cochran Database SystRev. 1999;3.
18. Moore EE, Mattox KL, Feliciano DV Transfusion,autotransfusion, and blood substitutes. In: MooreEE, Mattox KL, Feliciano DV, eds. Trauma Manual.New York: McGraw-Hill; 2003:84-90,
19. Rotundo MF, Reilly PM. Bleeding and coagulationcomplications. In: Mattox KL, Feliciano Dy MooreEE, eds. Trauma. 4th ed. New York, McGraw-Hill;2000:1267-1285.
20. Luna GK, Maier Ry Pavlin EG, Anardi D, Copass MK,Oreskovich MR. Incidence and effect of hypother-mia in seriously injured patients, / Trauma. 1987;27:1014-1018,
21. Gentilello L. Hypothermia in trauma. In: Trunkey DD,Lewis FR, eds. Current Therapy of Trauma. 4th ed.Baltimore: Mosby; 1999:325-328,
22. BurchJM, DentonJR, Noble RD. Physiologic rationalefor abbreviated laparotomy. Surg Clin North Am.1997;77:779-782.
23. Gould SA, Moore EE, Hoyt DB, et al. The first ran-domized trial of human polymerized hemoglobin asa blood substitute in acute trauma and emergentsurgery.yy4;M Coll Surg. 2OO2;445-455.
24. Johnson JL, Moore EE, Offner PJ, et al. Resuscita-tion with a blood substitute abrogates pathologicpostinjury neutrophil cytotoxic function./ Trauma.2001;50(3):449-456.
25. Biffl WL, Moore EE, Haenel JB. Hemoglobin solutionsfor trauma resuscitation. In: Trunkey DD, Lewis FR,eds. Current Therapy of Trauma. 4th ed. Baltimore:Mosby; 1999:329-333.
26. Wilson RF, Tyburski JG, Janning SW. Sepsis in trauma.In: Wilson RF, ed. Handbook of Trauma: Pitfalls andPearls. Philadelphia: Lippincott, Williams & Wilkins;1999:596-625.
27. Jarrar D, Chaudry IH, Wang P Organ dysfunc-tion following hemorrhage and sepsis: mecha-nisms and therapeutic approaches. Int f Mol Med.1999;4(6):575-583.
28. Lee CC, Marill KA, Carter WA, Crupi RS. A currentconcept of trauma-induced multiorgan failure. AnnFmergMed. 2001;38(2):170-176.
29. Schulman C. End points of resuscitation: choosingthe right parameters to monitor. Dimens Crit CareNurs. 2OO2;21(1):2-I4.
30. Tatevossian R, Wo C, Velhamos G, Demetriades D,Shoemaker W, Transcutaneous oxygen in CO2 asearly warning of tissue hypoxia and bemodynamicshock and critically ill emergency patients, Crit CareMed. 2000;28(7):2248-2253,
31. Mikhail J, Massive transfusion in trauma: process andoutcomes,/ Trauma Nurs. 2OO4;l l(2):55-60.