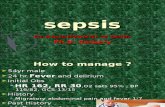
SEPTICEMIA, SEPSIS, SEPTIC SHOCK SEPTICEMIA, SEPSIS, SEPTIC SHOCK.
Sepsis markers
-
Upload
dr-mohamed-maged-kharabish -
Category
Health & Medicine
-
view
183 -
download
0
Transcript of Sepsis markers
Introduction
• Sepsis can occur suddenly and deteriorate rapidly
• Timely diagnosis of sepsis is the key of success
Sepsis markers
• Diagnostic– Useful for identifying or ruling out sepsis– Identifying patients who may benefit from
specific therapies
• Assessing the response to therapy
• Prognostic
Ideal sepsis markers
• High sensitivity (increase pathologically in the presence of disease)
• High specificity (does not increase in the absence of disease)
• Related to the disease burden and extent• Changes in accordance with the clinical
evolution• Anticipates clinical changes before it
happens
Ideal sepsis markers
• Adds independent information about the risk or prognosis
• Reproducible
• Easy and cheap
What do we have now?
• WCC
• Lactate– Tissue perfusion variables
• Biomarkers– C-reactive protein (CRP)– Procalcitonin (PCT)– Cytokines– New markers
What do we have now?
• Large numbers of markers– Cytokines– Receptors biomarkers– Coagulation biomarkers– Biomarkers related to vascular endothelial
damage– Markers related to organ dysfunction– Acute phase protein biomarkers– others
Lactate production
Critical illness leading to increased tissue oxygen extraction
Oxygen delivery Oxygen consumption
Oxygen debt
Global tissue hypoxia
Anaerobic metabolism
Lactate production
Lactate
• Raised in severe sepsis and septic shock– Hypoperfusion (secondary to anaerobic
metabolism)
– Cellular metabolic failure
– Decrease clearance by the liver
Prognostic and predict mortality
• It can be used as …– Monitoring response of septic patients to resuscitation
– Stratification and prognosis
• Serial lactate level monitoring is recommended– High lactate clearance:
• less required vasopressors therapy, greater improvements in APACHE II scores and decreased mortality rates
Lactate clearance
• In patients with septic shock– Survivors vs non-survivors
• Initial lactate level did not differ much
•Survivors had a significant decrease in lactate levels and less “lactate clearance time”
Lactate clearance
• Lactate clearance– The percentage lactate decrease over the
initial 6 hr ED evaluation and treatment period
CRP
• Acute phase protein
• Synthesized in liver
• IL-6 (and IL-1 and TNFα) stimulate synthesis
• Binds bacterial polysaccharide/ chromatin– Activates the classical complement pathway– Increase the immune inflammatory response
• Esp. in bacteria infection (vs viral)
CRP
• Level of CRP begins within 4-6hrs after stimulus
• Doubles every 8hrs
• Peaks at 36-50 hrs
• Half-life 19hrs
CRP
• A sensitive marker of inflammation and tissue damage
• Other conditions result in raised in CRP– Rheumatological disease
• SLE• Systemic sclerosis• Dermatomyositis• Sjogren’s disease
– Inflammatory bowel disease– Haematological disease
• E.g. leukaemia– Graft-versus-host disease
Procalcitonin
• A peptide precursor of calcitonin• Produced by
– parafollicular cells of the thyroid – neuroendocrine cells of the lung and the
intestine (extrathyroidal)
• It raises in a response to a proinflammatory stimulus– Esp of bacterial origin (mainly from the cells of
lung and the intestine)
PCT- characteristics
• Short half-life (~24hrs) independent of renal function
• Easy to measure in serum and plasma (stable in vivo and in vitro)
• Plasma concentration ~ <0.05-1000ng/ml
• In systemic inflammation or in infection– Persists as long as inflammatory process
continues
• Mechanical trauma– Increase within 2-4hrs– Peak in 1st or 2nd day then diminish
Procalcitonin (PCT)• Reference values (except newborn)
– Significantly lower in leukopenic patients
< 0.05ng/ml Healthy individuals
< 0.5ng/ml Probability of sepsis is low, local infection possible
0.5-2ng/ml Grey zone, recheck 6-12hrs later
>2ng/ml Probability of sepsis is high
• Antibiotics were started/ stopped based on a predefined cut-off ranges of PCT value
• Primary end point– 28 and 60 days mortality– No. of days without antibiotics
• PCT is also associated with other conditions– VAP– Severe acute pancreatitis– Acute exacerbation of COPD
Nonbacterial infection: Viruses, Fungi, Parasites
• PCT tend to be low in viral infection– However, in systemic viral infection, PCT value can
as high as 16 ng/ml
• A low serum PCT cannot be used to exclude bacterial from viral infections but that a combination of PCT, CRP, white blood cell count, and clinical illness scoring might be more useful
Nonbacterial infection: Viruses, Fungi, Parasites
• In patients with fungal infections, results have been variable
• Infection with the malaria parasite often leads to very high levels of serum, as high as 662 ng/mL
Sepsis and PCT: The Pediatric Experience
• Variable in sensitivity and specificity• Some authors recommended against the use of
PCT in routine diagnosis of bacterial sepsis in neonates, because of more complicated PCT measurement and its expense in comparison with CRP.
Different features of CRP and PCT
• CRP levels may not further increase during more severe stages of sepsis.
• PCT rises in proportion to the severity of sepsis and reaches its highest levels in septic shock.
Therefore, the diagnostic capacity of PCT is Therefore, the diagnostic capacity of PCT is superior to that of CRP due to the close superior to that of CRP due to the close correlation between PCT levels and the correlation between PCT levels and the
severity of sepsis and outcome.severity of sepsis and outcome.
Therefore, the diagnostic capacity of PCT is Therefore, the diagnostic capacity of PCT is superior to that of CRP due to the close superior to that of CRP due to the close correlation between PCT levels and the correlation between PCT levels and the
severity of sepsis and outcome.severity of sepsis and outcome.
Different features of CRP and PCT
• PCT reacted more quickly than CRP
• PCT concentrations had their maximum levels prior to those of CRP
Allows anticipation of a diagnosis of sepsis 24-48 hours
before the CRP level would
Allows anticipation of a diagnosis of sepsis 24-48 hours
before the CRP level would
Different features of CRP and PCT
• CRP concentrations were high already during the less severe stages of organ dysfunction and systemic inflammation– values were not much further increased during the
more severe stages of disease.
• PCT levels correlates with the stages of disease (especially increased in patients with organ dysfunction, severe sepsis or septic shock.)
CRP less useful in distinguishing evolution of sepsis in severe sepsis and septic shock
CRP less useful in distinguishing evolution of sepsis in severe sepsis and septic shock
Different features of CRP and PCT
• PCT concentrations more rapidly declined as compared with CRP
CRP remained high even in the late stage of disease
CRP remained high even in the late stage of disease
Prognosis
• PCT levels were significantly associated with – admission to a special care unit– duration of intravenous antibiotic use– total duration of antibiotic treatment– length of hospital stay, whereas CRP was
related only to the latter two variables.
• These data suggest that PCT may be a valuable addition to currently used markers of infection for diagnosis of infection and prognosis in patients with fever at the AED
New sepsis markers
• Soluble CD14 subtype (Generic name- Presepsin)
• Heparin-Binding protein
• Others
Quick turn around time- for emergency and intensive
care use
Quick turn around time- for emergency and intensive
care use
Heparin-binding protein
• An early marker of circulatory failure in sepsis
• Release from activated neutrophils
– A potent inducer of vascular leakage
– Resulted in extravasation of plasma and WBC to the focus of infection
• TNF-a– The initiating factor in the activation of host
response and subsequent cytokine release during infection
– Concentration increase 24 times after LPS challenge during in vivo experimental endotoxemia
• Short half-life of 17 min– Short-term concentration in response to
bacterial challenge
However, the diagnostic utility of TNF is insufficient for distinguishing infectious
inflammationWhy?
• Interleukin-6– Increased concentrations correlating to infection
– Activation time: very short
– Half-life time ~ 1hr
– Sensitive early diagnosis of neonatal sepsis– Adult values
• Sepsis 300-2700ng/L• SIRS 100ng/L
– Usefulness in adult diagnosis has not well established.