Sepsis Clc
Transcript of Sepsis Clc
-
8/3/2019 Sepsis Clc
1/25
Stephanie Swanson RN, BSN
-
8/3/2019 Sepsis Clc
2/25
PhilosophyThrough staff education early signs of sepsis can be
identified and aggressive treatment implemented. Safeand effective management will improve patientsurvival rates.
(Pickard, 2006)
-
8/3/2019 Sepsis Clc
3/25
MissionTo educate floor staff on sepsis, systemic inflammatory
response syndrome (SIRS), multi-organ dysfunction(MODs). Providing them with the knowledge of theprocess, signs for early identification and treatmentplans.
-
8/3/2019 Sepsis Clc
4/25
Learning outcomes To have an understanding of the infective process as it
relates to sepsis
Understand SIRS as it relates to MODs
Identify early signs of sepsis
Identify the four indicators of patient advancement towardSIRS
Know when and how to initiate non-ICU sepsis protocol Know your role in the non-ICU sepsis protocol
Identify when patient may not be appropriate for non-ICUsetting
-
8/3/2019 Sepsis Clc
5/25
Course sequence Part one
What is sepsis
Understanding possible sources
Progression of sepsis, SIRS and MODS Sepsis + organ dysfunction
Sepsis + organ dysfunction + volume resistant hypotension
Mortality rate
Who goes septic? Patient presentation (whats my septic patient look
like?)
(Gunthrie-Chu,2009)
-
8/3/2019 Sepsis Clc
6/25
Course one description Microorganisms invade a body system and initiate
systemic inflammatory response (SIRS)
Gram- negative and gram positive aerobes, anaerobes,fungi, exogenous sources and endogenous sources.
SIRS wide spread inflammatory response to severeinfective process progresses to multiple organ systemdysfunction syndrome (MODS). (Urden, Stacey, Lough, 2010)
-
8/3/2019 Sepsis Clc
7/25
Course descripton Severe sepsis occurs in > 750,000 patients in the U.S.
annually
Leading cause of death in non-coronary critical careunits
Mortality rate of 38- 59 %(Urden, Stacey, Lough, 2010)
-
8/3/2019 Sepsis Clc
8/25
Course description I go, you go, we all go
every patient with a severe infection have potential tobecome septic.
Consider coexisting health conditions
Source of infection
Patient presentation
PNA and UTI are most commonly associated with sepsis(Urden, Stacey, Lough, 2010)
-
8/3/2019 Sepsis Clc
9/25
Course description Look at holistic picture
Dont get tunnel vision
Look for worsening trends Skin color, LOC, orientation
Changes in vital signs.
Remember not everyone is septic
Age does not predict sepsis anyone can go septic(Urden, Stacey, Lough, 2010)
-
8/3/2019 Sepsis Clc
10/25
Objectives part one RN will be able to provide early identification of
patients with potential of progression to sepsis
RN will report assessment finding to physician andrequest initiation of non-ICU sepsis protocol.
Identify SIRS score Severe sepsis vs. septic shock
-
8/3/2019 Sepsis Clc
11/25
Part two SIRS criteria
Vital signs
What to watch for Lab values
Blood cultures
Lactate
WBCs Neutrophils (Matthews & Harsh, 2010)
-
8/3/2019 Sepsis Clc
12/25
Part two The plan
Know when to act
Be prepared with what to expect
Understanding nursing action on sepsis protocol
(Matthews & Harsh, 2010)
-
8/3/2019 Sepsis Clc
13/25
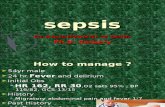
Course description Identify SIRS criteria rating of patient
Report patients with two of the following parametersto physician
Temp < 98.6 or > 100.4
Pulse > 90/min
Resp >20 or pCO2 < 32 WBC 12000 or bands > 10% neutrophils
(Matthews & Harsh 2010)
-
8/3/2019 Sepsis Clc
14/25
Course description RN monitoring of septic patients will increase
Strict Q2hr I & O report output of < 30ml/hr after
6hr.Vitals signs Q1hr x 4 hr, Q2hr x 2, Q4hr x 24
frequency may be increased based upon nursingjudgement
Give antibiotics as ordered Treat fever > 101F, hyperglycemia protocol, and DVT
prophylaxis. (Matthews & Harsh, 2010)
-
8/3/2019 Sepsis Clc
15/25
Objectives part two
The RN will identify and report patients with any 2 of
4 SIRS criteria to physician
RN will request non-ICU sepsis protocol and initiate
RN monitoring will increase
-
8/3/2019 Sepsis Clc
16/25
Part three Using the protocol outside the ICU
Treatment of hypotension with fluids.
When to know a higher level of care is required
Trends in vital signs to watch for
Urinary output Skin color (Matthews & Harsh 2010.)
-
8/3/2019 Sepsis Clc
17/25
Course description Please look at past medical history, pre- existing conditions
may require a more reserved fluid resuscitation efforts.
Give 500 mL of NS over 30 min, repeat x1 for systolic < 90
Notify physician if systolic BP < 90 or HR > 100 after 2boluses.
If unresponsive to initial fluid bolus be prepared to beginaggressive resuscitation with 500 mL bolus of NS Q 30 min
(parameters will be established by physician on volumes) Remember this is an intravascular depletion and volume
resuscitation can exceed 6L for the severely septic patient.(Matthews & Harsh 2010)
-
8/3/2019 Sepsis Clc
18/25
Course descriptionWorsening trend in vital signs
Temp > 103
Systolic blood pressure < 60 Heart rate > 140
Respiratory rate > 35
Urine output of < 30mL/hr
Increased O2 needs or decreasing O2 sats Mottled skin
Acute mental status changes (Matthews & Harsh 2010)
-
8/3/2019 Sepsis Clc
19/25
Course description Patient requires a higher level of care!
Unsuccessful volume resuscitation may requirepressors for vascular support.
End goal is adequate end organ tissue perfusion.(Urden, Stacy, Lough 2010)
-
8/3/2019 Sepsis Clc
20/25
Part three objectives The nurse will implement sepsis management bundle
Administer IV antibiotics as ordered
Begin fluid challenge
Increase monitoring by RN maintained.
-
8/3/2019 Sepsis Clc
21/25
Course one evaluation Evaluation of content will be assessed through written
exam. Exam will include multiple choice, fill in theblank.
Content will include definition of sepsis Risk factors
Identification of organisms responsible for sepsis
Identification of when to report
Case study
Score > 90% required for completion andadvancement to course 2
-
8/3/2019 Sepsis Clc
22/25
Course two EvaluationWritten exam that includes
SIRS criteria
Identification of at risk patient
Identification of expected nursing interventions
Exam will be multiple choice and fill in the blank
Case study
Score > 90% required for completion and advancementto course 2
-
8/3/2019 Sepsis Clc
23/25
Course three evaluation Each participant will receive 3 different case studies at
end of part 3 for completion in 1 hour.
Evaluation will require a written evaluation of 3separate case studies. Case studies will includeassessment of patient, lab interpretation, clinical
presentation of patient and individualized plan of carefor all 3 cases.
-
8/3/2019 Sepsis Clc
24/25
Instructor Evaluation Upon course completion please complete survey
received with case studies.
Survey will address:
Course content
Applicability in clinical setting
Instructor knowledge of content
Strengths and weakness of course content Strengths and weakness of instruction method
Suggestions.
-
8/3/2019 Sepsis Clc
25/25
ReferencesMatthews, J, & Harsh, H. (2010). Identifying your septic patient. Informally publishedmanuscript, Department of Nursing Educaton, Exempla Health system
Guthrie-Chu, C. (2009). Sepsis and septic shock.American Journal of Critical Care Nursing,16(2), 110-119.
Larson, E. (2007). Development and implementation of multi-disciplinary sepsis protocol.Critical Care Nurse,23(3), 43-54.
Urden, L., Stacy, K., & Lough, M. (2010). Critical care nursing diagnosis and management.St. Louis, Mo.: Mosby.