Selective dopamine-1 receptor agonist augments regional myocardial blood flow: Comparison of...
Transcript of Selective dopamine-1 receptor agonist augments regional myocardial blood flow: Comparison of...

Selective dopamine-1 receptor agonist augments regional myocardial blood flow: Comparison of fenoldopam and dopamine
A new class of vasodilators exhibiting selective dopamine-1 receptor agonist activity is being introduced into clinical practice. Inasmuch as various vasodilators either augment or decrease myocardial blood flow (“coronary steal”) depending on their pharmacologic action, the goal of this study was to assess the effects of fenoldopam (selective dopamine-1 receptor agonist) and dopamine (nonselective dopamine-1 receptor agonist) on regional myocardial blood flow in the presence of coronary occlusion. Accordingly, in 16 dogs anesthetized with pentobarbital, the left anterior descending coronary artery was occluded. Cardiovascular and renal hemodynamic effects were measured before and after intravenous infusion of renal equipotent doses of either fenoldopam (n = 9, 0.1 pglkglmin) or dopamine (n = 7, 1 rglkglmin). Both fenoldopam and dopamine caused a significant and comparable increase in renal blood flow. Fenoldopam but not dopamine significantly decreased the calculated peripheral vascular resistance and subsequently increased cardiac output. Dopamine had no effect on regional myocardial blood flow. In contrast, fenoldopam augmented transmural myocardial blood flow in normal (from 114 + 10 to 188 f 27 ml1100 gmlmin, p < 0.02) and ischemic border myocardium (from 45 ? 5 to 68 ? 11 ml/100 gm/min, p < 0.03 and p < 0.02 vs dopamine). There was a significant increase in blood flow to both the endocardial and epicardial layers of normal and ischemic border myocardium. These changes were accompanied by a significant reduction in coronary vascular resistance in the normal myocardium. In addition, with fenoldopam increments in myocardial blood flow in normal and ischemic border myocardium showed a significant correlation with changes in renal blood flow (I = 0.76, p < 0.01 and r = 0.60, p < 0.01, respectively). No such correlation was observed after dopamine. In conclusion, low-dose infusion of selective (fenoldopam) and nonselective (dopamine) dopamine-1 receptor agonists resulted in comparable increases in renal blood flow but divergent effects on regional myocardial perfusion. Fenoldopam but not dopamine resulted in improved perfusion in normal and ischemic border myocardium. It is postulated that these findings may have important clinical implications in the treatment of patients with heart failure, renal dysfunction, and concomitant ischemic heart disease. (AM HEART J 1992;124:418.)
Yi Shi, MD, Andrew Zalewski, MD, Barry Bravette, MD, Andrew R. Maroko, and
Peter R. Maroko, MD Philadelphia, Pa
Regional myocardial blood flow is influenced by complex interactions among anatomic, neural, me- chanical, and metabolic fact0rs.l Evidence exists that various vasodilators may exert either beneficial or detrimental effects on redistribution of collateral flow in the presence of myocardial ischemia.” The discovery of postsynaptic dopamine-1 (DA,) recep-
From the Division of Cardiology, Department of Medicine, Jefferson Med- ical College.
Supported in part by a grant from SmithKline Beecham Pharmaceuticals.
Received for publication Oct. 28, 1991; accepted Feb. 17, 1992.
Reprint requests: Andrew Zalewski, MD, Suite 5611 Gibbon Building, Thomas Jefferson University, 111 S. 11th St.. Philadelphia, PA 19107.
411l38102
tors, which regulate vascular tone in many vascular beds,j raises questions regarding their effect on col- lateral flow in the ischemic myocardium. Dopamine, which in higher doses activates not only DA1 recep- tors but also N- and P-adrenoceptors, causes vaso- constriction4 and an increase in myocardial oxygen consumption,5 which is detrimental in myocardial ischemia. In contrast fenoldopam, a novel selective DA1 agonist, is devoid of 01- and fl-adrenoceptor ac- tivity.6 These properties of fenoldopam explain its potential for clinical applications in the treatment of patients with hypertension71 8 or congestive heart failure.g+10 Accordingly the present study was de- signed to determine the effect of fenoldopam and dopamine on regional myocardial blood flow after coronary artery occlusion. Fenoldopam and dopa-
418

Volume 124
Number 2 Comparison of fenoldopam with dopamine 419
Table I. Reproducibility of regional blood flow measurements (N = 8)
After CA0
15 min 30 min P
Myocardial blood flow Normal zone Ischemic border zone Center ischemic zone
Renal blood flow
125.60 t 13.73 129.60 f 12.69 NS 33.79 + 6.96 31.75 + 4.47 NS
9.16 f 2.18 9.49 + 1.61 NS 563.88 + 62.70 528.56 + 45.63 NS
CAO. Coronary artery occlusion; NS, not significant.
mine were administered intravenously at equipotent doses resulting in similar renal vasodilation.
METHODS Experimental preparation. Sixteen dogs were anesthe-
tized with sodium pentobarbital(30 mg/kg intravenously), endotracheal tubes were placed, and the lungs were venti- lated with room air by means of a volume respirator (Har- vard Apparatus Inc., South Natick, Mass.). Systemic arte- rial pressure (Statham P23 dB pressure transducer, Viggo- Spectramed Inc., Critical Care Div., Oxnard, Calif.) and ECG lead aVF were recorded continuously throughout the experiments. A thoracotomy was performed through the fifth intercostal space, and the heart was suspended in a pericardial cradle. The left anterior descending coronary artery was isolated, and a 2-O silk suture was placed around it. All experiments conformed to the “Position of the American Heart Association on Research Animal Use,” adopted November 11,1984 by the American Heart Asso- ciation.
Protocol. After completion of the surgical procedures, the left anterior descending coronary artery was occluded. Thirty minutes later, when all animals were hemodynam- ically stable, colored nonradioactive microspheres (10 mil- lion, 15 :t 0.45 grn, E-Z Trac, Los Angeles, Calif.) were in- jected into the left atrium. A reference blood sample was withdrawn from the femoral artery at the rate of 10.5 ml/ min, beginning 15 seconds before injection of microspheres and continuing for a total of 90 seconds. The animals were then randomly assigned to receive a l&minute intravenous infusion of either dopamine (n = 7,1 pg/kg/min) or fenold- opam (n = 9,0.1 pg/kg/min). The doses of both drugs were selected on the basis of findings in a previous report indi- cating their equipotent effect on renal blood flow.ll After a 15-minute infusion of dopamine or fenoldopam, a differ- ent color of nonradioactive microspheres was injected into the left atrium with simultaneous withdrawal of a reference blood sample as described previously. The color of the mi- crospheres before and after treatment was selected ran- domly for each animal. Four colors (blue, yellow, red, and green) were used in this study. No changes in arterial pres- sure and heart rate were seen as a result of microsphere in- jections. Afterward, Brilliant Green dye (Sigma Diagnos- tics, St. Louis, MO.) was injected into the left atrium to delineate the area of ischemic myocardium in vivo. Then the dogs were killed by intravenous injection of potassium
chloride. The hearts were excised, and the left ventricle was frozen at -70” C and cut into 3 mm thick slices from the apex to the site of occlusion. Multiple transmural biopsy samples were obtained from each dog. Based on the distri- bution of Brilliant Green dye, samples were obtained from the normal zone, the ischemic border zone, and the center ischemic myocardium. Special attention was paid to ob- taining only ischemic tissue (approximately 1 cm wide) ad- jacent to the normal zone in the ischemic border biopsy specimens. Each sample was then divided into endocardial and epicardial layers (at least 2 gm each). In addition, multiple samples of renal tissues were obtained for blood flow analysis.
Regional blood flow measurements. The reference blood samples and myocardial and renal tissue specimens were processed as described in detail by Hale et a1.12 The process of tissue and blood digestion was carried out with reagent solutions supplied by the manufacturer. The final dilution volume was calculated by drawing up the mixture into the tip of a variable-volume automatic pipette. The total number of microspheres of each color in individual samples was calculated after microspheres were counted in at least 16 chambers with a Fuchs-Rosenthal hemocytom- eter (Hansser Scientific Partnership, Horsham, Pa.); a modification of the formula described by Hale et a1.12 was used. Then regional myocardial and renal blood flow and cardiac output were computed as described by Utley et a1.13 for radioactive microspheres. Transmural regional myo- cardial blood flow for each biopsy specimen was calculated as a weighted mean of the corresponding blood flow in the endocardial and epicardial layers. Results regarding myo- cardial and renal blood flow were expressed as milliliters per 100 grams per minute (ml/100 gm/min). In addition, coronary vascular resistance (dynes x set x cm-5/gm) was - calculated by means of the following formula: (AP x 80)/ RMBF, where AP (mm Hg) was mean arterial pressure and RMBF (L/gm/min) was regional myocardial blood flow in the normal myocardium. Peripheral vascular resistance (dynes x set x cm-“) was calculated as (AP x 8O)/CO, where CO was cardiac output (L/min).
To assess the reproducibility of blood flow measure- ments, repeated injections of colored microspheres were carried out 15 minutes and 30 minutes after coronary ar- tery occlusion in eight dogs. As shown in Table I, nonra- dioactive microspheres yielded excellent reproducibility of myocardial and renal blood flow measurements.

420 Shi et al.
250 Normal Zone lschemic Border Zone
1
August 1992
American Heart Journal
lschemic Zone
pco 02
ml/lOOg/min . p<o 02
r --I
PC0 03
NS
m && DOPAMINE FENOLDOPAM DOPAMINE FENOLDOPAM OOPAMINE FENOLDOPAM
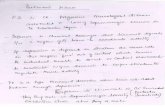
Fig. 1. Transmural blood flow in normal zone, ischemic border zone, and center ischemic myocardium af- ter dopamine and fenoldopam. Fenoldopam (0.1 pg/kg/min) produced significant increase in transmural myocardial blood flow in normal and ischemic border myocardium, whereas dopamine (1 pg/kg/min) had no effect.
Table II. Hemodynamic data
HR (beatslmin) AP (mm Hg) CO (Llmin) PVR (dynes X set x cme5)
Treatment Before After Before After Before After Before After
Dopamine 123 t 11 125 k 10 95 + 5 91 i 4 3.9 2 0.4 3.7 + 0.5 2,025 _t 147 2,097 t 173
Fenoldopam 140 * 7 138 f 7 98 k 3 92 -t 3 3.2 k 0.5 4.8 + 0.7* 2,637 2 282 1,746 + 214t
HR, Heart rate; AP, mean arterial pressure; CO, cardiac output; PVR, peripheral vascular resistance.
*p < 0.05 versus before and versus dopamine tp < 0.02 versus before. $p < 0.01 versus before.
Statistical analysis. Data were expressed as mean + SEM. Comparisons within and between groups were carried out with Student’s paired and unpaired t tests, respec- tively.
RESULTS
Baseline heart rate, mean arterial pressure, cardiac output, and calculated peripheral vascular resistance were similar 30 minutes after coronary occlusion in dogs randomly assigned to receive either dopamine or fenoldopam. Furthermore, regional myocardial blood flow in the normal zone, the ischemic border zone, and the center ischemic myocardium did not differ between the two groups before initiation of either treatment. Hence both groups were comparable be- fore dopamine or fenoldopam infusion.
Hemodynamics (Table II). Heart rate did not change significantly after either dopamine or fenoldopam infusion. Dopamine did not affect mean arterial pressure, whereas fenoldopam caused a small but significant decrease from 98 r+ 3 mm Hg to 92 f 3 mm Hg (p < 0.01). Cardiac output did not change after dopamine, whereas fenoldopam produced a
significant increase in cardiac output from 3.2 + 0.5 L/min to 4.8 + 0.7 L/min (p < 0.05), an increase of 50%. The calculated peripheral vascular resistance was not affected significantly by dopamine infusion, whereas fenoldopam resulted in a significant de- crease from 2637 + 282 dynes X set x crne5 to 1746 + 214 dynes X set X cme5 (p < 0.02), a decrease of 34%.
Regional myocardial blood flow. Transmural blood flow in the normal zone, the ischemic border zone, and the center ischemic myocardium did not change significantly after dopamine infusion (Fig. 1). In contrast, fenoldopam caused a significant increase in transmural blood flow in normal and ischemic border myocardium. It increased from 114.14 + 9.89 ml/100 gm/min to 188.28 + 26.84 ml/100 gm/min (p < 0.02) and from 44.71 f 4.94 ml/100 gm/min to 67.54 t 10.85 ml/100 gmlmin (p < 0.03 and p < 0.02 vs dopamine), respectively. Transmural blood flow in the center ischemic zone was 16.26 I 3.02 ml/100 gmlmin before and 16.74 k 3.43 ml/100 gmlmin af- ter fenoldopam infusion (not significant). The distri- bution of regional myocardial blood tlow in the

Volume 124
Number 2 Comparison of fenoldopam with dopamine 421
Table III. The effects of dopamine and fenoldopam on the distribution of regional myocardial blood flow
Before
Dopamine
After Before
Fenoldopam
After
Normal zone
Ischemic blxder zcme
Center ischemic zcme
Endo 142.00 t 16.92 131.15 + 15.82 107.75 f 11.82 173.72 k 26.46* Epi 128.48 T 15.63 130.68 t 16.45 120.95 i 9.46 202.89 t 29.04-T Endo 33.03 +- 4.96 24.77 + 3.92 36.76 -t 5.48 55.23 + lO.l$$ Epi 43.89 f 6.30 35.84 f 6.53 52.91 If- 4.91 79.92 + 12.07$§
Endo 8.69 k 1.86 8.12 i 2.72 11.63 k 3.60 9.13 -t 2.11 Epi 19.80 -+ 7.39 19.21 + 8.27 20.90 k 3.29 24.57 + 5.75
Endo. Endocardial flow (ml/lOOgm/min); Epi, epicardial flow (ml/lOOgm/min) *p < O.OZ:I versus before. tp < 0.01 versus before. $p < 0.05 veraus before. §p < 0.0% versus dopamine.
endocardial and epicardial layers is shown in Table III. Fenoldopam infusion resulted in a significant in- crease in the endocardial and epicardial samples from the normal myocardium and the ischemic bor- der zone, whereas dopamine had no effect. The cal- culated coronary vascular resistance in the normal myocardium did not change significantly after dopamine infusion. In contrast, fenoldopam caused a significant reduction in the calculated coronary vas- cular resistance from 7.27 ? 0.61 X lo6 dynes X
set X cm-5/gm to 4.65 t 0.72 X lo6 dynes X set X
cmP5/gm (p < 0.001). Renal blood flow. Renal blood flow increased signif-
icantly from 592 -t 29 ml/100 gm/min to 734 -+ 66 ml/100 gm/min after dopamine infusion (p < 0.05). A similar significant increase in renal blood flow from 482 +- 57 ml/100 gm/min to 803 +- 137 ml/lOOgm/ min was observed after fenoldopam (p < 0.05 and NS vs dopamine). Thus dopamine and fenoldopam infu- sions resulted in comparable enhancement in renal perfusion. There was a significant linear correlation between increments in renal and myocardial blood flow in normal (y = 26.12 L 0.15x, r = 0.76, p < 0.01) and ischemic border myocardium (y = 4.56 -t 0.06x, r = 0.80, p < 0.01) in the group treated with fenold- opam (Fig. 2). In contrast, no such correlation was observed in the group treated with dopamine (r = 0.30 and r = 0.16, p = NS for both normal and ischemic border myocardium, respectively).
DISCUSSION
The major findings of this study were (1) low-dose infusion of fenoldopam but not dopamine produced a significant increase in regional myocardial blood flow in normal and ischemic border myocardium, and (2) a linear correlation existed between increases in
myocardial blood flow in either normal or ischemic border zones and the increase in renal blood tlow in the group treated with fenoldopam.
Cardiovascular effects of dopamine and fenoldopam. Cardiovascular and renal effects of dopamine infu- sion at 1 pg/kg/min as observed in this study are con- sistent with those in previous reportsus l4 Although significant renal vasodilation was observed, no in- crease in regional myocardial blood flow was noted in the present study. This is likely related to differences in DA1 receptor density in coronary and renal circu- lation. Furthermore, even a low dose of dopamine (i.e., 1 pg/kg/min) is associated with ol-adrenoceptor agonist activity, which reduces the vasodilating effect of the drug.” Therefore coronary vasodilation after dopamine has been noted in vitro15 and in vivoi6 only after a-adrenoceptor blockade. This effect of dopa- mine has been attenuated with a specific DA1 recep- tor antagonist,16 which indicates the presence of these receptors in coronary circulation. An increase in coronary blood flow in vivo has also been observed after higher doses of dopamine, resulting in P-adreno- ceptor activation and an increase in myocardial oxy- gen consumption.5
In contrast, fenoldopam administration resulted in arteriolar vasodilation as indicated by a decrease in arterial pressure and an increase in cardiac output and renal blood flow, which is consistent with the previously described DA1 agonist activity of this compound.“-s As expected fenoldopam and dopa- mine produced comparable increases in renal blood flow but interestingly had divergent effects on re- gional myocardial blood flow.
The mere fact that the drug is a vasodilator does not predict redistribution of collateral flow in the is- chemic myocardium. For example, minoxidil,17 ni-

422 Shi et al. August 1992
American Heart Journal
300
1 Fenoldopam l
y = 26.12 +0.15x, r = 0.76, p<O.Ol .
-I . 200
AMBFN ,oo
0 $?Y
l ,8 0 0
-1OO~.,.(.,.,.,.~
-200 600 1000
100
60 , . , , I l
60
-200 0 200 400 600 600 1000
Fig. 2. Relationship between increases in transmural my- ocardial blood flow in either normal (upper panel) or ischemic border (lower panel) myocardium and changes in renal blood flow. Closed circles denote values after fenold- opam; open circles denote values after dopamine. Strong correlation exists between changes in transmural myocar- dial blood flow and renal flow after fenoldopam, whereas no correlation is seen after dopamine. A A&U’, Change in my- ocardial blood flow; A RBF, change in renal blood flow; N, normal myocardium; IB, ischemic border myocardium.
troprusside,2 adenosine,18 and dipyridamolelg, 2o cause “coronary steal” by diverting myocardial flow from the ischemic myocardium. These unfavorable changes in myocardial perfusion are paralleled by worsening of myocardial ischemia as evidenced by an increase in ST segment elevation with some of the previously mentioned agents.2, I7 In contrast, nitro- glycerin has an opposite effect increasing collateral flow to the ischemic myocardium.2 Findings in the present study demonstrated that fenoldopam in- creased myocardial blood flow to the normal myo- cardium and to the ischemic border zone. The direct vasodilating effect of fenoldopam on coronary arteri- oles in the ischemic border myocardium seems un- likely, inasmuch as these vessels are already dilated by metabolically related stimuli. More likely alter- ations in the vascular tone of the large conductance
and small resistance vessels in the normal zone were responsible for observed changes. It is postulated that dilation of the small resistance vessels produced the decrease in coronary vascular resistance and im- proved myocardial blood flow in the nonischemic myocardium. The increase in myocardial perfusion in the ischemic border zone was likely related to dilation of the large conductance vessels, which allowed for increased perfusion via collateral channels. The ob- served increase in cardiac output cannot solely ac- count for the changes in myocardial perfusion. As demonstrated by Braunwald et al.,“l an increase in cardiac output has minimal effect on coronary blood flow as opposed to changes in arterial pressure. Thus an increase in coronary blood flow to normal and is- chemic border myocardium after fenoldopam oc- curred despite a significant reduction in arterial pressure, no change in heart rate, and the known lack of an inotropic effect of fenoldopam.6,” Therefore changes in coronary blood flow as a result of an increase in myocardial oxygen consumption should be excluded. An alternative explanation might in- clude a decrease in the left ventricular filling pressure after fenoldopam. This mechanism is doubtful, how- ever, because fenoldopam at a dose of 0.1 pg/kg/min exhibited no effect on pulmonary wedge pressure even in the presence of heart failure.‘s A strong lin- ear correlation between the increases in myocardial flow and renal blood flow after fenoldopam implies that the increases in myocardial perfusion were me- diated through the same mechanism, that is, activa- tion of DA1 receptors in these two vascular beds.
Limitations of the study. This study has some limi- tations. Cardiac contractility, which might affect cardiac output and myocardial blood flow, was not measured. It is unlikely, however, that it played an important role, inasmuch as neither fenoldopam nor dopamine at the doses used in this study demon- strated any effect on cardiac contractility.“, l1 The admixture of normal myocardium to the ischemic border samples could be responsible for some of the increase in myocardial blood flow. We attempted to minimize this artifact by separating the perfused and nonreperfused myocardium by injecting dye and slicing the heart into 3 mm thick slices before obtaining myocardial samples. Therefore we believe that such contamination is insignificant.
Myocardial blood flow was measured by means of nonradioactive colored microspheres. This technique obviates t,he problem of disposal of radioactive ma- terial. Hale et al. l2 demonstrated a close correlation between myocardial blood flow measurements ob- tained with radioactive and nonradioactive micro- spheres. The present study also demonstrated excel-

Volume 124
Number 2 Comparison of fenoldopam with dopamine 423
lent reproducibility of repeated flow measurements with the use of nonradioactive microspheres (Table I). Although colored microspheres generally yield higher values than radioactive microspheres, this be- comes significant only with markedly increased blood flow beyond values observed in this study. The observed effects of DA1 agonist activity on regional myocardial blood flow and hemodynamics have been demonstrated in dogs anesthetized with pentobar- bital. Species differences and differences in the mag- nitude of the response in the awake state cannot be excluded.s2
Clinical applications. The therapeutic role of DA1 agonist activity with fenoldopam has already been tested in patients with congestive heart failuregT10 and hypertension. 7, 8 The present study focused on the effect of fenoldopam on myocardial and renal perfusion at infusion rates resulting in only minor changes in systemic blood pressure. It is postulated that in conditions where dopamine is administered to improve renal function, fenoldopam might be pref- erable because it improved cardiac performance and coronary blood flow (in normal and ischemic border myocardium). Hence findings in this study suggest a therapeutic role for DA1 receptor agonists in patients with renal dysfunction and concomitant ischemic heart disease, particularly during times of adverse conditions, for example, noncardiac and cardiac sur- gery or invasive procedures that are otherwise asso- ciat,ed with higher morbidity. The results of this study, however, should not be extrapolated to higher doses of fenoldopam producing a greater decrease in systemic blood pressure and a reduction in coronary perfusion pressure.
In conclusion, the DA1 receptor agonist fenold- opam increased myocardial blood flow in normal and ischemic border myocardium. These changes were closely correlated with increases in renal perfusion. It is postulated that these properties of fenoldopam may have important therapeutic implications in pa- tients uith renal dysfunction and concomitant is- chemic heart disease.
tom in the central nervous system? Commun Psychopharma- co1 1979;3:447-56.
4. Nayler WG, McInnes I, Stone J, Carson V, Lowe TE. Effect of dopamine on coronary vascular resistance and myocardial function. Cardiovasc Res 1971;5:161-8.
5. Brooks HL, Stein PD, Matson JL, Hyland JW. Dopamine-in- duced alterations in coronary hemodvnamics in dam. Circ Res cI 1978;12:120-6.
6. Hahn RA, Wardell Jr JR, Sarau HM, Ridley PT. Character- ization of the peripheral and central effects of SK&F 82526. a novel dopamine receptor agonist. J Pharmacol Exp Ther 1982;223:305-13.
7. Murphy MB, Murphy MD, McCoy CE, et al. Augmentation of renal blood flow and sodium excretion in hypertensive patients during blood pressure reduction by intravenous administra- tion of the dopaminei agonist fenoldopam. Circulation 1987; 76:1312-8.
8. Elliott WJ, Weber RR, Nelson KS, et al. Renal and hemody- namic effects of intravenous fenoldopam versus nitroprusside in severe hypertension. Circulation 1990;81:970-7.
9. Young JB, Leon CA, Pratt CM, Suarez JM, Aronoff RD, Rob- erts R. Hemodynamic effects of an oral dopamine receptor ag- onist (fenoldopaml in patients with congestive heart failure. J Am Co11 Cardiol 1985;6:792-6.
10. Young JB, Leon CA, Pratt CM, Kingry C, Taylor AA, Roberts R. Intravenous fenoldopam in heart failure: comparing the hemodynamic effects of dopaminei receptor agonism with ni- troprusside. AM HEART J 1988;115:378-84.
11. Lass NA, Glock D, Goldberg LI. Cardiovascular and renal he- modynamic effects of intravenous infusions of the selective DAi agonist, fenoldopam, used alone or in combination with dopamine and dobutamine. Circulation 1988;78:1310-15.
12. Hale SL, Alker KJ, Kloner RA. Evaluation of nonradioactive, colored microspheres for measurement of regional myocardial blood flow in dogs. Circulation 1988;78:428-34.
13. Utley J, Carlson E, Hoffman JIE, Martinez HM, Buckburg CD. Total and regional myocardial blood flow measurements with 25r(, 15~, 9w. and filtered 1-10~ diameter microsoheres and antipyrine in dogs and sheep. &rc Res 1974:34:391-405.
14. Boughi S, Horton R, Antonipillai I, Manoogian C, Ehrlich L, ?Jadler d. Comparison of donamine and fenoldonam effects on renal blood flow and prostacyclin excretion in normal and es- sential hypertensive subjects. J Clin Endocrinol Metab 1989;69:1116-21.
15. Toda N, Goldberg LI. Effects of dopamine on canine coronary arteries. Cardiovasc Res 1975;9:384-9.
16. Kopia GA, Valocik RE. Demonstration of specific dopamine-1 receptor-mediated coronary vasodilation in the anesthetized dog. J Pharmacol Exp Ther 1989;248:215-21.
17. Radvanv P, Davies MA, Muller JE, Maroko PR. Effects of minoxidil on coronary collateral flow and acute myocardial injury following experimental coronary artery occlusion. Car- diovasc Res 1978;12:120-6.
18. Schnaar RI, Sparks HV. Response of large and small coronary arteries to nitroglycerin, NaNOz and adenosine. Am J Physiol 1972:223:223-8.
We thank Ms. Laraine Bartlett for preparation of the manu- script.
19. Fam’WM, McGregor M. Effect of nitroglycerin and dipyrida- mole on regional coronary resistance. Circ Res 1968;22:649-59.
20. Tomoike H, Ootsubo H, Sakai K, Kikuchi Y, Nahamura M.
REFERENCES
1. Braunwald E. Heart disease. Philadelphia: WB Saunders, 1988:1193-1203.
2. Chiarieilo M. Gold HK. Leinbach RC. Davis MA, Maroko PR.
Continuous measurement of coronary artery diameter in situ. Am J Physiol 1981;240:H73-9.
21. Braunwald E, Sarnoff SJ, Case RB, Stainsby WN, Welch Jr GH. Hemodynamic determinants of coronary flow: effect of chances in aortic uressure and cardiac outnut on the relation-
Comparison between the effects of nitroprusside and nitro- ship between myocardial oxygen consumption and coronary glycerm on ischemic injury during acute myocardial infarc- flow. Am J Physiol 1958;192:157-63. tion. Circulation 1976;54:766-73. 22. Bishop SP, White FC, Bloor CM. Regional myocardial blood
3. Goldberg LI, Kohli JD. Peripheral pre- and post-synaptic flow during acute myocardial infarction in the conscious dog. dopamine receptors: are they different from dopamine recep- Circ Res 1976:38:429-38.