Salvage of Long‐Term Central Venous Catheters During an Outbreak ofPseudomonas...
Transcript of Salvage of Long‐Term Central Venous Catheters During an Outbreak ofPseudomonas...

Salvage of Long‐Term Central Venous Catheters During an Outbreak of Pseudomonas putidaand Stenotrophomonas maltophilia Infections Associated With Contaminated Heparin Catheter‐Lock Solution • Author(s): M. Beatriz Souza Dias , MD, PhD; Alina Bernardes Habert , MD; Vera Borrasca , RN;Valeska Stempliuk , RN, PhD; Aina Ciolli , RN; M. Rita E. Araújo , MD; Silvia F. Costa , MD,PhD; Anna S. Levin , MD, PhDSource: Infection Control and Hospital Epidemiology, Vol. 29, No. 2 (February 2008), pp. 125-130Published by: The University of Chicago Press on behalf of The Society for Healthcare Epidemiologyof AmericaStable URL: http://www.jstor.org/stable/10.1086/526440 .
Accessed: 15/05/2014 02:43
Your use of the JSTOR archive indicates your acceptance of the Terms & Conditions of Use, available at .http://www.jstor.org/page/info/about/policies/terms.jsp
.JSTOR is a not-for-profit service that helps scholars, researchers, and students discover, use, and build upon a wide range ofcontent in a trusted digital archive. We use information technology and tools to increase productivity and facilitate new formsof scholarship. For more information about JSTOR, please contact [email protected].
.
The University of Chicago Press and The Society for Healthcare Epidemiology of America are collaboratingwith JSTOR to digitize, preserve and extend access to Infection Control and Hospital Epidemiology.
http://www.jstor.org
This content downloaded from 91.229.248.208 on Thu, 15 May 2014 02:43:47 AMAll use subject to JSTOR Terms and Conditions

infection control and hospital epidemiology february 2008, vol. 29, no. 2
o r i g i n a l a r t i c l e
Salvage of Long-Term Central Venous CathetersDuring an Outbreak of Pseudomonas putida and
Stenotrophomonas maltophilia Infections AssociatedWith Contaminated Heparin Catheter-Lock Solution
M. Beatriz Souza Dias, MD, PhD; Alina Bernardes Habert, MD; Vera Borrasca, RN; Valeska Stempliuk, RN, PhD;Aina Ciolli, RN; M. Rita E. Araujo, MD; Silvia F. Costa, MD, PhD; Anna S. Levin, MD, PhD
objective. To describe the management of patients with long-term central venous catheters (CVCs) during an outbreak of infectiondue to Pseudomonas putida and Stenotrophomonas maltophilia associated with contaminated heparin catheter-lock solution.
design. Descriptive study.
setting. Private, 250-bed tertiary-care hospital.
methods. In March 2003, we identified 2 febrile cancer patients with P. putida bacteremia. Over 2 days, 7 cases of bacteremia wereidentified; lots of syringes prefilled with heparin catheter-lock solution, supplied by a compounding pharmacy, were recalled and sampleswere cultured. More cases of bacteremia appeared during the following days, and any patient who had had a catheter lock infused withthe suspect solution was asked to provide blood samples for culture, even if the patient was asymptomatic. Isolates that were recoveredfrom culture were typed by pulsed-field gel electrophoresis. Antimicrobial salvage treatment of long-term CVCs was attempted.
results. A total of 154 patients had had their catheter lock infused with solution from the lots that were suspected of being contaminated.Only 48 of these patients had CVCs. By day 7 of the outbreak, 18 of these patients had become symptomatic. Twenty-six of the remaining30 asymptomatic patients then also provided blood samples for culture, 10 of whom developed fever shortly after samples were collected.Thirty-two patients were identified who had P. putida bacteremia; 9 also had infection due to S. maltophilia. Samples from 1 of the 3 lotsof prefilled syringes in use at the time of the outbreak also grew P. putida on culture. Molecular typing identified 3 different clones of P.putida from patients and heparin catheter-lock solution, and 1 clone of S. maltophilia. A total of 27 patients received antimicrobial therapyregimens, some of which included decontamination of the catheter lock with anti-infective lock solution. Of 27 patients, 19 (70%) retainedtheir long-term CVC during the 6-month follow-up period.
conclusions. To our knowledge, this is one of the largest prospective experiences in the management of bloodstream infection associatedwith long-term CVCs. The infections were caused by gram-negative bacilli and were managed without catheter removal, with a highresponse rate. We emphasize the risks of using intravenous formulations of medications supplied by compounding pharmacies that producelarge quantities of drugs.
Infect Control Hosp Epidemiol 2008; 29:125-130
From the Infection Control Department, Hospital Sırio Libanes (M.B.S.D., V.B., V.S., A.C., M.E.R.A., A.S.L.), and the Infection Control Department andLIM 54, Hospital das Clınicas (A.B.H., S.F.C.), and Department of Infectious Diseases (A.B.H., S.F.C.), University of Sao Paulo, Brazil.
Received July 26, 2007; accepted October 16, 2007; electronically published December 20, 2007.� 2007 by The Society for Healthcare Epidemiology of America. All rights reserved. 0899-823X/2008/2902-0005$15.00. DOI: 10.1086/526440
Recent medical advances have resulted in more patients withcomplex medical problems who require the use of centralvenous catheters (CVCs) for prolonged periods of time. Thesecatheters are used for the administration of intravenous fluids,medications, blood products, and parenteral nutrition; theyare also used to provide hemodialysis and to monitor thehemodynamic status of patients. Therefore the use of long-term CVCs—in particular, tunneled Broviac-Hickman–typecatheters and totally implantable venous access devices (ie,ports)—is very common.1,2
As a result, catheter-related infection has become a sig-nificant clinical problem. Infections associated with long-termCVCs almost always involve internal colonization of the cath-eter. This colonization can be derived from contaminationof the catheter hub by the skin microflora, which are generallygram-positive organisms, such as coagulase-negative staph-ylococci and Staphylococcus aureus. The catheter hub can alsobe contaminated by gram-positive or gram-negative organ-isms on healthcare professionals’ hands.3 Infusates can beanother source of contamination that may cause outbreaks
This content downloaded from 91.229.248.208 on Thu, 15 May 2014 02:43:47 AMAll use subject to JSTOR Terms and Conditions

126 infection control and hospital epidemiology february 2008, vol. 29, no. 2
of infection. In such cases, gram-negative organisms are themajor cause of catheter-related infection and bacteremia.4
Unusual pathogens, such as other Pseudomonas species andRalstonia pickettii, have been recovered during several out-breaks associated with contaminated heparin catheter-lockflush solutions.5-9
Currently, catheter-related infection is a major cause ofpremature catheter removal. Because long-term CVC place-ment is indispensable for certain patients and because re-placing the catheter requires another surgical procedure, atadditional cost, techniques to preserve these devices are animportant goal in catheter management.10,11 The aim of thisstudy was to describe the management of long-term CVCsin patients affected by an outbreak of infection due to P.putida and S. maltophilia that was associated with contami-nated heparin catheter-lock solution.
methods
Background of Outbreak
Hospital Sırio-Libanes is a private, 250-bed hospital in SaoPaulo, Brazil, that predominantly treats surgery and oncologypatients. The majority of cancer patients use a CVC to receivechemotherapy. This group includes both inpatients and out-patients, and catheter locks are provided when the CVC isused intermittently. When not in use, implanted cathetershad heparin catheter-lock solution infused once per month,and tunnelled catheters had the solution infused once perweek. The prefilled syringes used to infuse the solution wereused for only 1 patient and used only 1 time. The volumeof solution used varied from 2 to 5 mL, and any remainingvolume of solution was discarded with the syringe.
On March 14, 2003, the pediatric oncology physician no-tified the infection control unit that blood cultures orderedfor the investigation of fever in 2 patients both seemed toyield the same unusual bacterium. The next day, P. putidawas identified in blood samples from these and other patients.An outbreak of infection was suspected. A case patient wasdefined as any patient with a blood culture positive for P.putida. A list of the first 7 case patients was made, whichincluded data on age, underlying conditions, symptoms, thepresence of CVCs, and the site from which blood sampleswere collected (ie, through the catheter or from a peripheralvein). All of the patients had tumors and indwelling CVCs,and either were inpatients or were outpatients followed upat the oncology clinic. Therefore, the heparin catheter-locksolution was strongly suspected as the source of the outbreak.The 3 lots of prefilled syringes in use had been bought froma new supplier; they contained 5 mL of 100 U/mL heparinsolution.
Interventions
The first intervention was the prompt recall and quarantineof syringes containing heparin catheter-lock solution from allhospital units, followed by culture of solution samples in the
clinical microbiology laboratory. A list was made of all pa-tients who had a catheter lock infused with a syringe of hep-arin catheter-lock solution from March 11 (the date the indexpatient received heparin solution) through March 15 (the datethe hospital stopped using the solution that was suspected tobe contaminated).
The physicians in charge of the patients listed were notifiedof the problem and asked to contact their patients. The phy-sicians were also asked to evaluate patients for symptoms ofinfection and to instruct them to come to the oncology clinicif such symptoms developed. Six days after the beginning ofthe outbreak, all cancer outpatients who had a CVC wereasked to come to the hospital so that blood samples couldbe obtained through the catheter. For some patients, bloodsamples were also obtained from a peripheral vein.
The hospital pharmacy was inspected and the pharmacy’spractices with respect to storage, handling, and administra-tion of the syringes filled with heparin catheter-lock solutionwere evaluated. A visit was also made to the compoundingpharmacy that supplied the syringes.
Microbiologic Study
Blood culture and bacterial identification were performed byuse of automated methods (Bact Alert and Vitek; Bio-Merieux), and additional manual identification tests (ie,growth at 42�C, gelatin lyses, and H2S production) were per-formed. Antimicrobial susceptibility was tested by the diskdiffusion method and interpreted according to the criteria ofthe Clinical and Laboratory Standards Institute (formerly theNational Committee for Clinical Laboratory Standards).12
P. putida was isolated from 1 of the 3 lots of prefilledsyringes in use. Colonies with different morphologies recov-ered from samples taken from the same syringe or from thesame blood culture were identified separately. After the iden-tification, all strains were plated on MacConkey agar and thenstored in cow’s milk (10% wt/vol) at �70�C for furtheranalysis.
Molecular Typing
Random amplified polymorphic DNA-polymerase chain re-action (RAPD-PCR) and pulsed field gel electrophoresis(PFGE) were used to evaluate the relationships between theisolates recovered during the outbreak. DNA from P. putidawas extracted by alkaline lyses as described elsewhere.13
RAPD-PCR was performed as described by Renders et al.14
After electrophoresis in 1% agarose gels, the ethidium bro-mide–stained DNA fragments were photographed (Polaroid).Banding patterns were analyzed, and types were assigned onthe basis of single- or multiple-band differences.
PFGE was done for P. putida and S. maltophilia. Whole-cell DNA was digested with the macrorestriction enzyme SpeI,and the fragment-size patterns obtained by PFGE were de-termined by use of a contour-clamped homogeneous electric
This content downloaded from 91.229.248.208 on Thu, 15 May 2014 02:43:47 AMAll use subject to JSTOR Terms and Conditions

salvage of cvcs in an outbreak of cvc-associated infection 127
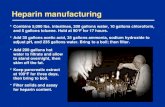
figure. Distribution of cases of bacteremia during the outbreak period. Case patients were those with a blood culture positive forPseudomonas putida and/or Stenotrophomonas maltophilia. BC, time blood samples were obtained for culture.
field DR-II apparatus (Bio-Rad Laboratories). Patterns wereanalyzed as recommended by Tenover et al.15
Clinical Treatment and CVC Management
Asymptomatic cancer outpatients with a CVC who werecalled in to provide blood samples for culture had their cath-eter locks decontaminated with an anti-infective solution con-taining amikacin (2 mg/mL) and heparin (100 U/mL), whichwas changed every 24 hours. Patients also received 0.5 g ofciprofloxacin orally, twice per day, until blood culture resultswere available (for a maximum of 5 days). If blood cultureresults were negative, antibiotic therapy was stopped.
It was decided that if any blood culture was positive forP. putida or if a patient presented clinical symptoms, the casewould be managed as recommended by the infection controlphysician: the patient would be treated with an antimicrobial(ie, cefepime, ceftazidime, meropenem, or ciprofloxacin) ad-ministered for 14 days through the catheter, and the catheterlock would be decontaminated with anti-infective solutioncontaining amikacin.
A new blood sample was collected from the catheter atleast 48 hours after the completion of treatment. Patients werefollowed up for 6 months. The catheter was removed only ifpositive culture results or symptoms persisted, or if the cath-eter was malfunctioning or no longer needed. During the 6-month follow-up period, blood cultures were performed onlyif clinically indicated.
results
Patient Management
During the period from March 11 to March 15, a total of154 patients had had their catheter lock infused with at least1 syringe of heparin catheter-lock solution from the 3 dif-ferent lots suspected of being contaminated. Only 48 of these
patients had CVCs. The other 106 patients had peripheralintravenous access devices or short-term devices that hadalready been removed and were asymptomatic at the time ofthe investigation; they did not present symptoms and had nopositive blood culture results during the outbreak period.They were subsequently lost to follow-up.
By day 7 of the outbreak, 18 patients with CVCs had be-come symptomatic: 5 inpatients and 13 outpatients. At thispoint, the 30 asymptomatic patients with CVCs were calledin to the hospital so that blood samples could be obtainedfor culture: 26 patients provided samples, 3 were in distanttowns, and 1 refused. Of these 26 outpatients, 10 developedfever shortly after blood samples were collected. This factsuggested that bacteremia developed after catheter manipu-lation, and these patients were also confirmed as case patients,for a total of 28 symptomatic cases. Four asymptomatic out-patients had catheter-obtained blood samples that grew P.putida on culture; they never developed signs of sepsis, despitekeeping their catheters. The distribution of cases over timeis shown in the Figure.
The age of the patients ranged from 2 to 92 years (median,54 years), and they were predominantly female (20 of 32[63%]). Most patients (24 of 32 [75%]) had solid tumors, 7(22%) of 32 had hematologic malignancies, and only 1 hadmyasthenia gravis. Four (13%) of the 32 patients had neu-trophil counts of less than 500 cells/mm3. No patients in-volved in the outbreak died.
Immediately after treatment, all control cultures were neg-ative for P. putida. During the 6-month follow-up period, nocases of P. putida bacteremia occurred among the patientsinvolved in the outbreak.
There were 5 patients who had peripheral blood samplesand catheter-obtained blood samples that grew P. putida onculture; 1 of these patients kept the CVC for the entire follow-up period. The 4 remaining patients had their catheters re-
This content downloaded from 91.229.248.208 on Thu, 15 May 2014 02:43:47 AMAll use subject to JSTOR Terms and Conditions

128 infection control and hospital epidemiology february 2008, vol. 29, no. 2
table Rate of Catheter Salvage During the 6 Months After an Outbreak ofInfection Due to Pseudomonas putida and Stenotrophomonas maltophilia
Catheter type Total
No. (%) of catheters
SalvagedRemoved because
of infectionRemoved forother reasons
CVC with implantedvenous access device 21 15 (71) 4 (19)a 2 (10)
Broviac-Hickman 6 4 (67) 1 (16) 1 (16)Total 27 19 (70) 5 (19)a 3 (11)
a One catheter removed after 3.5 months because of infection.
moved; 1 removal was performed because S. maltophilia bac-teremia developed 3.5 months after the outbreak.
No problems were found in the hospital with respect tothe storage, distribution, handling, or administration of theheparin catheter-lock solution. The compounding pharmacycould not provide control samples for microbiological testing.
Microbiologic Findings and Molecular Typing
Blood cultures were performed for 44 patients; of these pa-tients, 32 had catheter-obtained samples that were positivefor P. putida on culture. Five of these patients also had pe-ripheral blood samples that were positive for P. putida onculture. S. maltophilia was also recovered from culture for 9patients.
Both typing methods for P. putida showed the same results.There were 3 different genotypes identified (A, B, and C),and all were recovered from patients and from syringes ofheparin catheter-lock solution. Type A was found in all sy-ringes, whereas type B and type C were each found in 2syringes. One syringe contained all 3 types. A total of 3 pa-tients were simultaneously infected with 2 different strains ofP. putida.
S. maltophilia was not found in the heparin catheter-locksolution. Typing of 5 S. maltophilia isolates showed that allof them had the same PFGE pattern.
Catheter Management
Of the 32 case patients, 27 had long-term CVCs and 5 hadshort-term intravascular catheters. The short-term catheterswere promptly removed and no attempt at salvage was made.
Despite the recommendations made by the infection con-trol physician, treatment of the patients with long-term CVCsvaried widely. A total of 27 different regimens were used.Amikacin was the antibiotic most commonly used in anti-infective solution for the decontamination of catheter locks(used for 11 patients), although levofloxacin and cefepimewere also used. The antimicrobials administered intrave-nously were as follows: ciprofloxacin (9 patients), cefepime(8), carbapenems (7), levofloxacin (3), and ceftazidime (3).The only antibiotic administered orally was ciprofloxacin,which was given to 12 patients.
A total of 17 patients had their catheter lock decontami-
nated in association with receiving with 1 or more antimi-crobials parenterally or orally, and only 3 (18%) of these 17had their catheter removed. For 3 patients, the combinationof oral ciprofloxacin therapy and catheter-lock decontami-nation with anti-infective solution containing amikacin wassuccessful, but 2 of them were asymptomatic. A total of 10patients did not have their catheter lock decontaminated, and2 (20%) of these patients had their catheters removed. Oneasymptomatic patient was treated successfully with oral cip-rofloxacin for just 5 days, without removal of the Broviac-Hickman catheter.
A summary of outcomes according to type of catheter isshown in the Table. Of 27 patients with long-term CVCs, 19(70%) were successfully treated without removal of their cath-eters during the 6-month follow-up period.
discussion
Outbreaks of bloodstream infection caused by various agentslinked to contaminated infusions and medications have beenwell described. Contamination can occur during the manu-facturing process or it can be extrinsic, occurring, for ex-ample, during the manipulation of multidose vials. In theoutbreak at our institution, the contamination occurred dur-ing the manufacture of prefilled syringes containing heparincatheter-lock solution at a compounding pharmacy. Otheroutbreaks caused by drugs produced in compounding phar-macies have been described, such as Exophiala infection dueto contaminated injectable steroids16 and Pseudomonas flu-orescens infection due to contaminated heparin-saline flushsolution.9 The epidemiology of P. putida infection is poorlystudied, and potential sources are not well determined,though it has been reported to contaminate tap water17 andanti-fog solution.18
In Brazil, the compounding of a drug is allowed only ifthere is no commercially available equivalent that is adequatefor the special needs of a patient.19 The compounding of drugsfor third parties, which resell them to individual patients, andthe compounding of drugs in anticipation of receiving pre-scriptions are not considered legitimate practices. However,there are manufacturers that produce large quantities and actas wholesalers, although they consider themselves compound-ing pharmacies and thus are not subject to the strict gov-
This content downloaded from 91.229.248.208 on Thu, 15 May 2014 02:43:47 AMAll use subject to JSTOR Terms and Conditions

salvage of cvcs in an outbreak of cvc-associated infection 129
ernment regulations generally applicable to pharmaceuticalcompanies. In the case of the outbreak at our institution, thehospital purchased the syringes prefilled with heparin cath-eter-lock solution from a compounding pharmacy, as thisformulation of heparin is not commercially available. At pre-sent, regulations for compounding pharmacies are clear and,if followed, guarantee patient safety. It is their enforcementthat is essential at this point.
The outbreak described here involved 32 oncology patientswith P. putida bacteremia, of whom 9 were also infected withS. maltophilia. None of the samples of the heparin solutionimplicated in the outbreak grew S. maltophilia on culture,although PFGE typing showed that the 5 typed isolates wereidentical. There are 2 possible explanations for this: cross-transmission of the organism between patients, or a commonsource. It has been suggested that because this organism iswidely distributed in the environment, there may be greatgenetic diversity among isolates in a hospital.20 Cross-trans-mission, however, has been implicated in an outbreak of S.maltophilia infection in bone marrow transplant recipientsthat resulted from poor hand hygiene,21 as well as in an out-break involving neonates.22 On the other hand, there are anumber of reports suggesting that S. maltophilia can be trans-mitted by contaminated common sources, including tapwater,23,24 faucet aerators,25 ventilator temperature sensors,26
items in the hospital room environment,27 and medical equip-ment.28 In the outbreak at our institution, it seems probablethat the heparin solution that was found to be contaminatedwith P. putida may also have been contaminated with S. mal-tophilia that was not detected. To our knowledge, this typeof transmission has not been described before.
Treatment of catheter-related infections usually involvesremoval of the catheter. If the infection is caused by gram-negative bacilli, as were the infections in this outbreak, mostinvestigators recommend catheter removal because of thehigher risk of relapse and mortality, although there have beenno randomized trials to determine the optimal managementstrategy.29
In situations in which catheter removal is not possible,conservative treatment can be tried as is usually done in casesof infection due to coagulase-negative staphylococci.30 It hasbeen suggested that treatments that include decontaminationof the catheter lock with anti-infective solution are signifi-cantly more likely to result in catheter salvage. In vitro activityagainst gram-negative bacilli in biofilms has been demon-strated for amikacin, ceftazidime, cefepime, and ciprofloxacinin a model mimicking catheter-related infections.31
In our study, as soon as the outbreak was identified, theinfection control department made a recommendation totreat patients who were suspected of having infections, andthe recommended treatment included parenteral antibiotictherapy and decontamination of the catheter lock with anti-infective solution. However, as a result of choices made bytheir physicians, our patients received a wide range of dif-ferent treatments, which included oral antibiotic therapy, in-
travenous antibiotic therapy, and/or decontamination of thecatheter lock with anti-infective solution. Despite this vari-ation in treatment, the rate of catheter salvage from the timeof the outbreak to the end of the 6-month follow-up periodwas very high (70%) and did not differ on the basis of whetherthe patient had the catheter lock decontaminated. One pos-sible explanation for the success of most of the treatments,despite the conservative approach taken at our institution,may be the prompt recognition of the outbreak and the earlyadministration of antimicrobial therapy. Another possibilitymay be the low human pathogenicity of non-aeruginosa spe-cies of Pseudomonas such as P. putida. These organisms areprimarily plant pathogens and may not have virulence factors,such as the adherence proteins for human tissue that arepresent in P. aeruginosa.32
In summary, to our knowledge this is one of the largestprospective experiences in managing bloodstream infectionsassociated with long-term CVCs. The infections were causedby gram-negative bacilli and were managed without catheterremoval, with a high response rate. We also emphasize therisks of using intravenous formulations of medications pre-pared by compounding pharmacies that do not follow guide-lines and regulations and that produce and supply large quan-tities of drugs.
acknowledgments
Potential conflicts of interest. All authors report no conflicts of interest rel-evant to this article.
Address reprint requests to Anna S. Levin, MD, PhD, Rua Banibas, 618,Sao Paulo-SP 05460-010, Brazil ([email protected]).
references
1. Wade JC, Newman KA, Schimpff SC, et al. Two methods for improvedvenous access in acute leukemia patients. JAMA 1981; 246:140-144.
2. Rubenstein EB, Fender A, Rolston KVI, et al. Vascular access by physicianassistants: evaluation of an implantable peripheral port system in cancerpatients. J Clin Oncol 1995; 13:1513-1519.
3. Sotir MJ, Lewis C, Bisher EW, Ray SM, Soicie JM, Blumberg HM. Ep-idemiology of device-associated infections related to a long-term im-plantable vascular access device. Infect Control Hosp Epidemiol 1999; 20:187-191.
4. Prospero E, Barbadoro P, Savini S, Manso E, Annino I, D’Errico MM.Cluster of Pseudomonas aeruginosa catheter-related bloodstreams infec-tions traced to contaminated multidose heparinized saline solutions ina medical ward. Int J Hyg Environ Health 2006; 209:553-556.
5. Hsueh PR, Teng LJ, Pan HJ, et al. Outbreak of Pseudomonas fluorescensbacteremia among oncology patients. J Clin Microbiol 1998; 36:2914-2917.
6. Torii K, Noda Y, Miyazaki Y, Ohta M. An unusual outbreak of infusion-related bacteremia in a gastrointestinal disease ward. Jpn J Infect Dis2003; 56:177-178.
7. Kimura AC, Calvet H, Higa JI, et al. Outbreak of Ralstonia pickettiibacteremia in a neonatal intensive care unit. Pediatr Infect Dis J 2005;24:1099-1103.
8. Perz JF, Craig AS, Strattin CW, Bodner SJ, Phillips WE Jr, Schaffner W.Pseudomonas putida septicemia in a special care nursery due to contam-
This content downloaded from 91.229.248.208 on Thu, 15 May 2014 02:43:47 AMAll use subject to JSTOR Terms and Conditions

130 infection control and hospital epidemiology february 2008, vol. 29, no. 2
inated flush solutions prepared in a hospital pharmacy. J Clin Microbiol2005; 43:5316-5318.
9. Centers for Disease Control and Prevention. Pseudomonas bloodstreaminfections associated with a heparin/saline flush—Missouri, New York,Texas, and Michigan, 2004-2005. MMWR Morb Mortal Wkly Rep 2005;54:269-272.
10. Albo Lopez C, Lopez Rodriguez D, Constenla Camba MI, Jimenez BlancoA, Araujo LF, Garcia-Medina J. Infectious and non-infectious compli-cations of tunneled central catheters in hematologic patients [in Spanish].Sangre (Barc) 1999; 44:176-181.
11. Biffi R, de Braud F, Orsi F, et al. Totally implantable central venous accessports for long-term chemotherapy: a prospective study analyzing com-plications and cost of 333 devices with a minimum follow-up of 180days. Ann Oncol 1998; 9:767-773.
12. National Committee for Clinical Laboratory Standards (NCCLS). Ref-erence Standards for Antimicrobial Susceptibility Testing. Wayne, PA:NCCLS; 2002:M100-59.
13. Sambrook, J, Fritsch EF, Maniatis T. Molecular Cloning, a LaboratoryManual. 2nd ed. Cold Spring Harbor, NY: Cold Spring Harbor Labo-ratory Press; 1989.
14. Renders N, Romling Y, Verbrugh H, Van Belkum A. Comparative typingof Pseudomonas aeruginosa by random amplification of polymorphicDNA or pulsed-field gel electrophoresis of DNA macrorestriction frag-ments. J Clin Microbiol 1996; 34:3190-3195.
15. Tenover, F, Arbeit R, Goering R, et al. Interpreting chromosomal DNArestriction patterns produced by pulsed-field gel electrophoresis: criteriafor bacterial strain typing. J Clin Microbiol 1995; 33:2233-2239.
16. Centers for Disease Control and Prevention. Exophiala infection fromcontaminated injectable steroids prepared by a compounding phar-macy—United States, July–November 2002. MMWR Morb Mortal WklyRep 2002; 51:1109-1112.
17. Aumeran C, Paillard C, Robin F, et al. Pseudomonas aeruginosa andPseudomonas putida outbreak associated with contaminated water outletsin an oncohaematology paediatric unit. J Hosp Infect 2007; 65:47-53.
18. Romney M, Sherlock C, Stephens G, Clarke A. Pseudo-outbreak of Pseu-domonas putida in a hospital outpatient clinic originating from a con-taminated commercial anti-fog solution— Vancouver, British Columbia.Can Commun Dis Rep 2000; 26:183-184.
19. Agencia Nacional de Vigilancia Sanitaria (ANVISA). Resolucao da Di-retoria Colegiada- RDC no. 214, de 12 de Dezembro de 2006. Dispoesobre Boas Praticas de Manipulacao de Medicamentos para Uso Humanoem farmacias. Available at: http://e-legis.anvisa.gov.br/leisref/public/showAct.php?idp25128&wordp. Accessed May 24, 2007.
20. Valdezate S, Vindel A, Martin-Davila P, Del Saz BS, Baquero F, Canton
R. High genetic diversity among Stenotrophomonas maltophilia strainsdespite their originating at a single hospital. J Clin Microbiol 2004; 42:693-699.
21. Klausner JD, Zukerman C, Limaye AP, Corey L. Outbreak of Stenotro-phomonas maltophilia bacteremia among patients undergoing bone mar-row transplantation: association with faulty replacement of handwashingsoap. Infect Control Hosp Epidemiol 1999; 20:756-758.
22. Gulcan H, Kuzuku C, Durmaz R. Nosocomial Stenotrophomonas mal-tophilia cross-infection: three cases in newborns. Am J Infect Control2004; 32: 365-368.
23. Sakhnini E, Weissmann A, Oren I. Fulminant Stenotrophomonas mal-tophilia soft tissue infection in immunocompromised patients: an out-break transmitted via tap water. Am J Med Sci 2002; 323: 269-272.
24. Verweij PE, Meis JF, Christmann V, et al. Nosocomial outbreak of col-onization and infection with Stenotrophomonas maltophilia in preterminfants associated with contaminated tap water. Epidemiol Infect 1998;120:251-256.
25. Weber DJ, Rutala WA, Blanchet CN, Jordan M, Gergen MF. Faucetaerators: a source of patient colonization with Stenotrophomonas mal-tophilia. Am J Infect Control 1999; 27:59-63.
26. Rogues AM, Maugein J, Allery A, et al. Electronic ventilator temperaturesensors as a potential source of respiratory tract colonization with Sten-otrophomonas maltophilia. J Hosp Infect 2001; 49:289-292.
27. Labarca JA, Leber AL, Kern VL, et al. Outbreak of Stenotrophomonasmaltophilia bacteremia in allogenic bone marrow transplant patients: roleof severe neutropenia and mucositis. Clin Infect Dis 2000; 30:195-197.
28. Alfieri N, Ramotar K, Armstrong P, Spornitz ME, Ross G, Winnick J,Cook DR. Two consecutive outbreaks of Stenotrophomonas maltophilia(Xanthomonas maltophilia) in an intensive-care unit defined by restric-tion fragment-length polymorphism typing. Infect Control Hosp Epide-miol 1999; 20:553-556.
29. Hanna H, Afif C, Alakech B, et al. Central venous catheter-related bac-teremia due to gram-negative bacilli: significance of catheter removal inpreventing relapse. Infect Control Hosp Epidemiol 2004; 25:646-649.
30. Fatkenheuer G, Cornely O, Seifert H. Clinical management of catheter-related infections. Clin Microbiol Infect 2002; 8: 545-550.
31. Lee MY, Ko KS, Song JH, Peck KR. In vitro effectiveness of the antibioticlock technique (ALT) for the treatment of catheter-related infections byPseudomonas aeruginosa and Klebsiella pneumoniae. J Antimicrob Che-mother 2007; 60:782-787.
32. Ma Q, Zhai Y, Schneider JC, Ramseier TM, Saier MH. Protein secretionsystems of Pseudomonas aeruginosa and P. fluorescens. Biochim BiophysActa 2003; 1611: 223-233.
This content downloaded from 91.229.248.208 on Thu, 15 May 2014 02:43:47 AMAll use subject to JSTOR Terms and Conditions