SAH for Neurology Residents
-
Upload
dhaval-shukla -
Category
Health & Medicine
-
view
644 -
download
5
description
Transcript of SAH for Neurology Residents

ANEURYSMAL SUBARACHNOID HEMORRHAGE
Dhaval Shukla
Associate Professor
Dept of Neurosurgery,NIMHANS

SAH Etiology- Non Traumatic
• Aneurysmal Rupture : 80-85%• Non aneurysmal perimesencephalic haemorrhage :
10%• Arteriovenous Malformation/ Fistula• Intracranial vessel dissection• Venous Sinus thrombosis• Vasculitis• Coagulopathy• Drug abuse/ Cocaine use• Hypertensive crisis

Aneurysm• Focal outpouching from the arterialwall

Epidemiology
• Prevalence of aneurysm 1-6%• Multiple aneurysm in 20 – 30%• Only about 20% of them rupture during a
lifetime– 10/1 lakh population / year (average)– India – 3-4 (hospital based studies)– High in Finland and Japan (15-30)– Low in France, China

Risk factors for aneurysm formation
• Incidence increases with age – Peak at 50-60 years– Very rare in children
• Female gender (1.2 – 1.6 times more common)
• Hypertension
• Smoking• Genetic factors
– Connective tissue disorders (Marfan, Ehler Danlos Syndrome)– Polycystic Kidney Disease– Familial occurrence (7 to 20%)

Natural History
• 10-12% die before receiving medical attention
• 40-50 % of hospitalized pts.die within 1 month
• Only 1/3rd of survivors have “good results”.


Clinical features
• Sudden severe headache (Thunderclap)– 1 in 8 to 10 pts with sudden severe headache have SAH
• Nausea, vomiting• Meningismus• Altered consciousness / coma• Focal neurological deficit• Seizures (10-25%)• Prodromal symptoms – sentinel bleeds (50%)• Ocular haemorrhages

Pitfalls in clinical diagnosis

HUNT AND HESS SCALE.
I - Asymptomatic or with mild headache
II-Moderate or severe headache, nuchal rigidity
III-Confusion, drowsiness, or mild focal deficit (discounting third nerve palsy)
IV-Stupor or hemiparesis, early decerebrate rigidity
V-Deep coma, extensor posturing

WFNS Grading
Grade GCS Clinical examination
1 15 No motor deficit
2 13-14 No motor deficit
3 13-14 Motor deficit
4 7-12 With or without motor deficit
5 3-6 With or without motor deficit


Diagnostic studies
SAH– CT scan– Lumbar Puncture
Intracranial aneurysm– DSA– CTA
– MRA

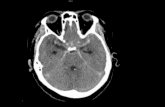
CT scan
• CT scan head-positive in up to
- 95-100% in 12-24 hours
- 80% in 3 days
- 70% in 5 days
- 50% at1 week
- 30% at 2 weeks
MRI is not sensitive in acute bleed


Fisher’s Grade
2
4

Modified Fisher’s Grade

CT
• Intraventricular Hemorrhage (IVH)
• Hydrocephalus
• Intracerebral hematoma (ICH)
• Brain edema
• Infarction caused by vasospasm

Hydrocephalus IVH and ICH

Pitfalls in CT diagnosis

Lumbar puncture (LP)
• Positive in
o 100% in 12 hrs to 2 weeks
o >70% after 3 weeks
o 40% after 4 weeks

Supernatant xanthochromia

Pitfalls in LP diagnosis

Importance of correct diagnosis !
• A disease of high morbidity and mortality
• Good grade patients are usually misdiagnosed
• Misdiagnosis ranges 25-50%


DSA
• Digital Subtraction Angiography (DSA)
“gold standard”
• Mortality -<0.1%
• Total neurological morbidity - 1%
• Permanent neurological morbidity -0.5%.

DSA

DSA

3D Rotational angiogram

CT Angiogram (CTA)
Demonstrate aneurysms as small as 2 to 3
mm
• Useful for surgical planning
• A screening tool in populations at high risk
• Sensitivity 95 – 97%

Magnetic Resonance Angiography-
Takes ½ to 1 hour
Detects aneurysms >3 to 5 mm
MRI detects thrombosed aneurysms
Screening modality

Angiogram-negative SAH• 15 to 20%
– 65 % are prepontine or perimesencephalic
• Causes– Vasospasm– Hypoperfusion– Poor angiographic technique – Thrombosis
• Repeat angiography– Undetected aneurysms found in an additional 2–5% of cases
at 2–4 weeks

Perimesencephalic bleed
• Venous hemorrhage• Younger• Non-hypertensive• Better grade • More in males• Prognosis good• Re-bleeding is rare• Delayed ischemic deficit
very few

Initial Management
• Absolute bed rest with 30degrees head elevation
• Analgesia- short-acting and reversible agent
– Pain is associated with a transient elevation in blood pressure and
increased risk of rebleeding
• Sedation with a short-acting benzodiazepine such as
midazolam
– Use with caution to avoid distorting subsequent neurologic
evaluation

Initial Management• Hourly neurochecks
• Strict input and output monitoring
• Monitoring BP, oxygen saturation
• Comatose patients – Intubation and ventilation
• Seizure prophylaxis- Phenytoin
• Stool softeners
• Nimodipine (60mg q4h for 21 days)

INVESTIGATIONS
• Hemoglobin, serum electrolytes, glucose, and arterial gases
• ECG
• Renal and liver function tests
• Chest radiography

Specific problems in aneurysmal SAH
• Rebleeding
• Vasospasm
• Hydrocephalus
• Hyponatremia
• Seizures
• Pulmonary complications
• Cardiac complications

Rebleed
• Most disastrous and disabling
• Mortality rates-70 to 90 %
• Prevention of rebleed is early intervention

Rebleed
• First 24 hrs- 4-6 %
• 1-2 % per day for 2 weeks ( cumulative 20%)
• 30% rebleed by 30 days
• 50% rebleed by 6 months
• There after 3% per year

Vasospasm
• Delayed ischemic neurlogic deficit-
• Onset on the 3rd day
• Peak 6_8 days
• Resolves by 3 weeks

Vasospasm
• Clinical Features
- delayed deterioration
- focal neurlogic deficits
- confusion, irritability
- fever
- raised ESR, total WBC count

Vasospasm management

Hydrocephalus• Acute hydrocephalus occurs in 15% to 87%
– With IVH - 35 to 65 %– managed by external ventricular drainage (EVD)
• Chronic shunt-dependent hydrocephalus occurs in 8.9% to 48%– Chronic hydrocepalus in 50% of pts with Ac. HCP– Treated with ventricular shunt placement


Seizures• Early 6% to 18%
• Delayed seizures 3% to 7%
• Risk factors– MCA aneurysm– Thickness of SAH– ICH– Rebleeding– Infarction– Poor neurological grade– History of hypertension
• Prophylactic anticonvulsants in the immediate posthemorrhagic period
• Routine long-term use of anticonvulsants is not recommended

Medical Complicationsof SAH

Cardiac Complications
• Hypertension treated requiring IV medication (27%)
• Hypotension requiring pressors (18%)
• Life-threatening arrhythmia (8%)
• Myocardial ischemia (6%)
• Successful resuscitation from cardiac arrest (4%)
• Troponin I elevation (20%-68%)– Regional wall motion
abnormalities (26%)
ECG Changes
• ST segment alterations (15%–67%)
• T-wave changes (12%–92%)
• Prominent U waves (4%–52%)
• QT prolongation (11%–66%)
• Conduction abnormalities (7.5%)
• Sinus bradycardia (16%)
• Sinus tachycardia (8.5%)

Neurogenic stunned myocardium
• Most severe form of cardiac injury
• Transient lactic acidosis
• Cardiogenic shock
• Pulmonary edema
• Widespread T-wave inversions
• Prolonged QT interval
• Reversible left ventricular wall motion abnormalities

Hyponatremia • 10% to 30%• Associated with onset of vasospasm• Cerebral salt wasting• Risk factors
– Poor clinical grade
– ACOMA aneurysm
– Hydrocephalus,
• Treatment– Aggressive volume resuscitation
– 3% saline
– Fludrocortisones

Pulmonary complications
• Chest Infection
• Neurogenic pulmonary edema

Definitive treatment• Microsurgical Clipping OR Endovascular coiling
should be performed as early as feasible in the majority of patients to reduce the rate of rebleeding
• Complete obliteration of the aneurysm should be achieved whenever possible
• Determination of aneurysm treatment, as judged by both neurosurgeons and endovascular specialists, should be a multidisciplinary decision based on characteristics of the patient and the aneurysm

Coiling

DACA Aneurysm Coiling


Coiling or Clipping
• For patients with ruptured aneurysms
judged to be technically amenable to both
endovascular coiling and neurosurgical
clipping, endovascular coiling should be
considered

Clipping preferred• Patients presenting with large ICH and MCA aneurysm • Aneurysm characteristics
– Wide neck– Blebs– Geometrically complex with incorporation of branch artery– Partially thrombosed – Giant
• Inability to navigate delivery system• Patients preference

Coiling preferred
• In elderly
• In poor-grade
• Aneurysms of basilar artery

Conclusion
• SAH is a NEUROSURGICAL EMERGENCY
• High index of suspicion is required
• Immediate investigation with a CT scan +/-LP should be done.
• Securing aneurysm early results in better outcome

Outcome
• Age
• WFNS grade
• Fisher grade
• Size of aneurysm
• Severity of vasospasm