Aalborg Media Lab 16-Jul-15 OOP Analysis and Design Lecture 16.
SEPSISmyharnetthealth.org/wp-content/uploads/2018/05/...Oct'15 Nov'15 Dec'15 Jan'16 Feb'16 Mar'16...
Transcript of SEPSISmyharnetthealth.org/wp-content/uploads/2018/05/...Oct'15 Nov'15 Dec'15 Jan'16 Feb'16 Mar'16...

SEPSIS PHYSICIAN
EDUCATION
2017

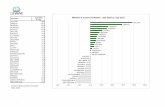
Oct'15 Nov'15 Dec'15 Jan'16 Feb'16 Mar'16 Apr'16 May'16 Jun'16 Jul'16 Aug'16 Sept'16 Oct'16 Nov'16
% Compliance 42.8 0.3 0 21.4 6.7 22.2 36.4 23.1 53.3 40 42.9 27.3 46.2 42.9
50th percentile 31.7 31.7 31.7 37.5 37.5 37.5 41.2 41.2 41.2 36.7 36.7 36.7 36.7 36.7
0
10
20
30
40
50
60
70
80
90
100
PER
CEN
T C
OM
PLI
AN
CE
SEPSIS COMPLIANCE
% Compliance
50th percentile
Linear (% Compliance)

SEPSIS 3rd and 4th QTR 2016
Sampled Cases Data Algorithm End Value (Reasons for Failures)
Severe Sepsis Fail Septic Shock Fail
Initial Sepsis
Population
Cases Sampled (Cat B, D, E, X)
Excluded Cases
(Cat B)
Sepsis Passed (Cat E)
Sepsis Failed
(Cat D)
Antibiotic Admin
Initial Lactate Level
Blood Cultures
Repeat Lactate Level
Crystalloid Fluids
Vasopressor Admin
6 Hour Counter
Persistent Hypo
tension Other *
Incomplete Cases
(Cat X)
3rd Quarter 2016
Jul 24 24 9 6 9 1 3 0 0 3 0 1 1 0 0
Aug 22 22 8 6 8 1 2 2 0 2 0 1 0 0 0
Sep 22 22 11 3 8 0 0 3 2 3 0 0 0 0 0
Qtr. Total 68 68 28 15 25 2 5 5 2 8 0 2 1 0 0
4th Quarter 2016
Oct 22 22 9 6 7 0 2 0 2 2 1 0 0 0 0
Nov 26 26 7 6 8 1 1 0 3 1 0 0 2 0 5
Dec 30 30 9 8 12 0 1 2 3 4 1 0 1 0 1
Qtr. Total 78 78 25 20 27 1 4 2 8 7 2 0 3 0 6
Total for Selected Period
146 146 53 35 52 3 9 7 10 15 2 2 4 0 6

Where Are We Failing?
• Not starting the antibiotic timely or choosing the wrong
antibiotic or combination of antibiotics.
• Blood Cultures not ordered or obtained after the antibiotic is
administered.
• Not using the Sepsis order set**
– Not identifying septic patient
– Fluid bolus not appropriate amount for body weight
(<30ml/kg)
– Initial Lactate Level not ordered or not ordered in the 6
hours before or 3 hours after severe sepsis presentation
window.
– Repeat Lactate Level if > 2 not repeated or not repeated
within the 6 hour window of severe sepsis presentation.
– Wrong Lactate Acid ordered and it does not automatically
reflex if > 2.
Please use Sepsis Order Sets………
4

SEPSIS This measure can and usually begins in the ED. However, the patient
may develop severe sepsis/septic shock as a inpatient or experience
more than one episode of severe sepsis/septic shock but we will
abstract the first episode.
All patients 18 years and older with an ICD 10 code of Sepsis will fall
into the measure. If criteria/documentation for severe sepsis/septic
shock are met it will stay in the measure for abstraction.
If the patient is to receive “comfort care” please dictate this in the
progress notes. If dictated prior to or within 3 hours of presentation of
severe sepsis and prior to or within 6 hours of septic shock it will
remove the patient from the measure.
The next slide will review the criteria for “severe sepsis” and “septic
shock”. Severe Sepsis components/criteria must be met within 6 hours
of each other. The date and time in which the last criteria for severe
sepsis is met (includes physician dictation of source of infection) is the
date and time that is used for presentation. This is the date and time
that the timed components of the measure must meet, 6 hours prior to
and 3 hours following severe sepsis presentation.
5

SEVERE SEPSIS CRITERIA Documented source or suspected source of clinical infection (except viral and
fungal infections) by a physician/APN/PA. Documentation of signs and
symptoms is not acceptable for a suspected infection.
AND
2 or more SIRS criteria
• Temp > 38.3˚C (100.9) or < 36˚C (98.6)
• Heart Rate > 90min
• Respiratory Rate > 20min
• WBC > 12,000 or < 4,000 or 10% Bands
AND
Organ Dysfunction (any one) (Except if documented normal for patient, from
acute condition that is not infection, from chronic conditions or medications.)
• Systolic BP < 90, or mean arterial pressure <65, or a decrease in SBP by
40mmHg from baseline with physician/APN/PA documentation that the decrease
is related to infection, severe sepsis or septic shock and not other causes.
• Acute Respiratory Failure evidenced by a new need for invasive or non-invasive
ventilation. ET/Tracheostomy Tube, BIPAP or CPAP.
• Creatinine > 2.0, or urine output < 0.5ml/kg/hour for 2 hours
• Total Bilirubin > 2 mg/dl
• Platelet count < 100,000
• INR > 1.5 or PTT > 60 sec
• Lactate > 2 mmol/l
6

SEPTIC SHOCK CRITERIA
There must be documentation of Severe Sepsis present.
AND
Hypotension persists in the hour after the conclusion of the
30ml/kg crystalloid fluid administration: As evidence by 2 or
more consecutive BP readings:
Systolic BP < 90, OR
Mean Arterial Pressure < 65 OR
Decrease in SBP by > 40 mmHg from the last recorded
SBP considered normal for given patient WITH
physician/APN/PA documentation that the decrease
is related to infection, severe sepsis or septic shock and
not other causes.
OR
Tissue hypo-perfusion is present as evidenced by:
-Initial Lactate level is = or > 4mmol/l
Physician/APN/PA documentation/dictation of Septic Shock. 7

8
The date and time in which the last criterion was met within 6 hours of
each other to establish the presence of severe sepsis will be the “start”
date and time.
If criteria for severe sepsis is not met but there is physician dictation
of Severe Sepsis then that dictation time will be the date and time of
Severe Sepsis present.
If criteria for severe sepsis are met after physician/APN/PA
documentation of septic shock, the date and time of documentation of
Septic Shock will be used as presentation time.
If criteria for severe sepsis are not documented and there is not
physician/APN/PA documentation of severe sepsis, but there is
physician/APN/PA documentation of septic shock, the earliest time
septic shock was documented will be the sepsis presentation time.
If the clinical criteria was met or there is physician/APN/PA
documentation of severe sepsis but within 6 hours there is additional
physician/APN/PA documentation indicating that the patient does not
have severe sepsis then disregard the previous documentation/criteria.

9
Should occur within 3 hours of presentation of Severe Sepsis:
Assess measurement of lactate (6 hours prior to until 3 hours after).
Obtain Blood Cultures (48 hours prior to until 3 hours after).
Unless there is a documented delay as to why the blood cultures were not
obtained timely. Surgical patients receiving prophylactic antibiotic prior to
severe sepsis/septic shock presentation, patient was treated for another type of
infection prior to severe sepsis/septic shock presentation, lab unavailable to draw
cultures within 45 mins or longer)
Administer Broad Spectrum Antibiotics: Correct single dose or combination
doses of approved antibiotics. (Administered 24 hours prior to or within 3 hours
after presentation date and time.)
Make sure the first ordered antibiotic is administered promptly. If not
administered prior to presentation time, the first antibiotic has to be started
within 3 hours of presentation time. If a combination of IV antibiotics are
prescribed they must also be given within 3 hours of presentation time. Please
refer to the next two slides for recommended antibiotic monotherapy and/or
combinations of antibiotic therapy.

Antibiotic Monotherapy Table
10
ertapenem ceftriaxone ampicillin/sulbactam
Invanz® Rocephin® Unasyn
meropenem ceftaroline fosamil piperacillin/tazobactam
Merrem® Teflaro® Zosyn®
cefotaxime levofloxacin
Claforan® Levaquin®
ceftazidime amoxicillin/clavulanate
Fortaz® Augmentin®

Combination Antibiotic Table (Choose one from each column)
11
Column A Column B
aminoglycoside (gentamicin or tobramycin)
cephalosporin (1st & 2nd Gen) OR
OR clindamycin IV OR
aztreonam daptomycin OR
OR glycopeptide (vancomycin) OR
ciprofloxacin linezolid OR
macrolide OR
penicillin

12
Should occur within 6 hours of presentation of Severe Sepsis:
Repeat lactate measurement if >2
Please use the Sepsis Order Set .
Will automatically re-order lactate level if >2.
Fluid Resuscitation (30ml/kg) (0.9% Normal Saline or Lactated Ringers given
for hypotension or lactate level >= 4). Total volume infused must be at least
30ml/kg which should be specified in the physician order. (Within 3 hours of
Septic Shock Presentation)
The Sepsis Order Set will calculate this for you.
If hypotension is still present after completion of at least 30ml/kg fluid boluses
as evidence by documentation of 2 or more consecutive SBP readings < 90,
Mean arterial pressure < 65, or a decrease in SBP by > 40 mmHg from the last
previously recorded SBP and physician/APN/PA documentation that is it from
infection, severe sepsis or septic shock not other causes, in the hour following
the conclusion of the boluses or initial lactate >=4.
Add:
Vasopressor administration, Reassessment of Volume Status, Tissue Reprofusio
Vasopressors (IV or Intraosseous): Norepinephrine (Levophed), Epinephrine
(Adrenalin), Phenylephrine (Neosynephrine), (Vazculep), Dopamine (Inotropin),
Vasopressin (Pitressin)
If Vasopressors needed (hypotension persists) should be received within 6 hours
of Septic Shock presentation.

13
Repeat volume status and tissue perfusion assessment (for chart abstraction the
dictation must be in the time window beginning at the fluid administration date/time
and ending 6 hours after presentation of septic shock date and time to pass the
measure) consisting of either:
A focused exam by the MD/PA/APN including date and time dictated, including:
Vital Signs Assessment (temp, pulse, resp, BP)
AND Cardiopulmonary Exam-notes must include both heart and lung assessment.
AND Capillary Refill Evaluation (capillary refill, nail bed refill, etc.)
AND Peripheral Pulse Evaluation (radial, brachial, dorsalis pedis, femoral, etc.)
AND Skin Examination (reference to color, flushed, mottled, pale, etc.)
New for Jan 1, 2017 discharges:
Documentation indicating Physician/APN/PA has performed, or attested to
performing a physical examination, perfusion (re-perfusion) assessment, or sepsis
(severe sepsis or septic shock) focused exam is acceptable.
Documentation indicating Physician/APN/PA has reviewed, performed, or attested to
reviewing or performing a Vital Sign Assessment, Cardiopulmonary Exam, Capillary
Refill Exam, Peripheral Pulse Evaluation, and a Skin Examination is acceptable.
(Without documentation of the specific components.)

OR Any 2 of the following with date and time dictated:
CVP measurement (CVP or RAP right atrial pressure must be documented that
reading was obtained by a central venous catheter.) Measurements from a PICC
line are acceptable.
Central venous oxygen measurement (Sv02 or Scv02 obtained by central
venous catheter.)
Bedside cardiovascular ultrasound (actual performance of test). May be
performed in a location other than the bedside such as imaging department or
ultrasound department.
Passive leg raise or Fluid Challenge (noted to be positive or negative). With the
patient in a semi-recumbent position both legs are raised to a 45 degree angle
and v/s response is evaluated.
A Fluid Challenge is the rapid infusion of crystalloid fluid volumes between
500 mls to 1000 mls over 15-20 mins and is done to assess the responsiveness
to fluids. (Starts at the completion of the crystalloid fluid administration and
stops 6 hours after the presentation of septic shock date and time.
14

References
• The Specification Manual for National Hospital
Inpatient Quality Measures. (2017)Version 5.2
(for discharges 1/01/2017-12-31-2017)
Retrieved from: http://www.qualitynet.org.
15

QUESTIONS?
Please contact one of the Quality Improvement
Specialists:
Deborah Priebe ext. 5286
Pam Wise ext. 5288
16