Relationship of growth and psychoneurologic status of 2-year-old children of birthweight 500–999 g
-
Upload
geoffrey-ford -
Category
Documents
-
view
215 -
download
2
Transcript of Relationship of growth and psychoneurologic status of 2-year-old children of birthweight 500–999 g
Early Human Development, 13 (1986) 329-337 Elsevier
329
EHD 00746
Relationship of growth and psychoneurologic status of 2-year-old children of birthweight 500-999 g
Geoffrey Ford, Anne Rickards, William H. Kitchen, Margaret M. Ryan and Jean V. Lissenden
Department of Obstetrics and Gynaecology, University of Melbourne, and The Royal Women’s Hospital, Melbourne, Australia
Accepted for publication 22 December 1985
Summary
There were 257 liveborn infants of birthweight 500-999 g born in one tertiary centre in the 5 l/4 years commencing January 1977; 86 (33.5%) survived to 2 years of age, corrected for prematurity and 83/86 (96.5%) were fully assessed. The prevalence of cerebral palsy was lo/83 (12%) and 17/83 (20%) had a major impairment. The distribution of weights and heights for 2-year-old boys and girls was significantly lower than for the standard population, as was the head cir- cumference distribution for boys; the distribution of the Mental Developmental Index (Bayley Scales) was not related to the head circumference or body weight at two years or to head-circumference/bodyweight or height ratios. At birth measure- ments of weight, length and head circumference were under the 3rd percentile for 13/86 (15%), 9/86 (10.5%) and 9/86 (10.5%) respectively. By 2 years of age, weight, length and head circumference were under the 3rd percentile in 23/83 (27.7%) 26/83 (31.3%) and 4/83 (4.8%) respectively. 12 children who were SGA at birth were fully assessed at 2 years; the group of 6, who continued with poor postnatal weight gains (under the 3rd percentile) had the highest rate of major impairment but included were the only extremely SGA twins and the only two major malformations in the study. We found no association of other health problems or unfavourable social factors with poor postnatal growth or impaired outcome.
infant; extremely low birthweight; fetal growth retardation; neurobehavioural out- come
Address for correspondence: Dr. W.H. Kitchen, The Royal Women’s Hospital, 132 Grattan Street, Carlton 3053, Australia.
0378-3782/86/$03.50 0 1986 Elsevier Science Publishers B.V. (Biomedical Division)
330
We use the term ‘extremely low birthweight (ELBW) infant’ to denote babies of birthweight under 1000 g. Since the introduction of neonatal intensive care, survival of these infants has improved considerably [12,15] but despite the technological advances, poor growth, health problems and major impairments continue to be reported in follow-up studies [9,10,16]. Many of these infants are born between 24 and 28 weeks gestation and frequently they gain weight poorly in hospital and continue it at home. In addition, some ELBW infants have already experienced poor prenatal growth. Any deleterious effect of suboptimal growth during this critical perinatal period of brain growth in humans is largely inferred from reference to animal studies [5]; although there is some concern for the long-term outcome of all ELBW infants there is particular apprehension for those who have grown poorly during this critical period.
From a cohort of ELBW children enrolled in a prospective longitudinal study, we sought answers to the following questions:
(a) what was the prevalence among 2-year-old ELBW children, of major sensorineural impairment, health problems and poor postnatal growth?
(b) What perinatal and intervening social, health and growth variables were associated with major impairments at 2 years of age?
(c) Were ELBW infants with coexisting intrauterine growth retardation specially disadvantaged at two years with respect to growth, health problems or major impairments?
Patients and Methods
The study cohort comprised 257 liveborn ELBW infants; 86 (33.5%) survived to the age of 2 years. All infants were delivered in a tertiary perinatal centre, The Royal Women’s Hospital, Melbourne, Australia in the 5 l/4 years, commencing January 1977; we report the outcome of 83/86 (96.5%) of the survivors who were fully assessed at the age of 2 years, corrected for their premature delivery. Their mean birthweight was 860 g (S.D. 99, range 565-990 g) and the mean gestational age was 27.5 weeks (S.D. 2.2, range 24-32 weeks). 52 (62.7%) mothers had been booked for delivery in the hospital and 31 (37.3%) had been transferred to this tertiary centre because of pregnancy complications. All mothers were Caucasian but 22 (26.5%) were recent immigrants whose first language was not English; 11 (13.3%) of family breadwinners belonged to professional groups, 45 (54.2%) were skilled or semi-skilled workers and 27 (32.5%) were either unskilled workers or the families were receiving social security benefits.
Infants were weighed to the nearest 5 g on electronic scales on admission to the intensive care unit and the crown-heel length and occipito-frontal head cir- cumference were measured on the first day of life. Details of clinical care of the infants have already been reported [8]. If fresh, unmodified breast milk from the infant’s own mother was available it was given untreated by nasogastric tube; otherwise an isocaloric humanized formula was utilized; the aim was to achieve by the 7th day an intake of 100-110 kcal/kg/day. Enteral feeding was frequently
331
inadequate necessitating supplementation or complete replacement by parenteral alimentation; for the latter, peripheral veins were used and in the absence of significant jaundice or thrombocytopenia, the intravenous nutrient solutions in- cluded a lipid preparation. Gestational age assessments were based on evidence from an early ultrasonic examination of the crown-rump length [22] and/or menstrual history if reliable; although gestation was assessed clinically [I], this estimate was used in data analysis only if the obstetric data were unavailable or there was a discrepancy of at least three weeks from the obstetrical assessment.
Percentile points for the anthropometric measurements of each infant at birth were obtained from composite intrauterine growth charts derived from recent hospital births in Melbourne [lo]; source data for these charts indicated that sex differences for the birthweight from 24 to 32 weeks gestation were both inconsistent and small so separate charts for male and female infants were unnecessary. Infants with birthweights under the 3rd percentile were designated as small-for-gestational age (SGA). Major impairment comprised children with one or more of the follow- ing: cerebral palsy, Mental Development Index (MDI) under 69, severe bilateral sensorineural deafness, bilateral blindness.
The children were seen close to 2 years from their expected date of delivery by the psychologist; the assessment included the Bayley Scales of Infant Development; the results of the MD1 are reported in this study. The pediatrician performed a standardized neurodevelopmental assessment, and recorded the child’s standing height, naked weight and the maximum occipito-frontal head circumference mea- sured with a plastic tape measure. Weights were recorded to the nearest 0.1 kg and measurements of length to the nearest 0.1 cm. Most children had previously had audiological screening tests and had been examined by an audiologist; further assessments were offered to all children. The sex-specific anthropometric data derived from an Australian metropolitan population in 1971-72 were used as the standard population to determine the percentile points for each ELBW infant at two years corrected age [13]. The children with body weights under the 3rd percentile were considered to have poor postnatal growth.
Data were analysed by computer, using Statistical Package for Social Sciences programmes [21]. Differences in proportion were compared using corrected x2 tests, differences in distribution were compared using two-tailed t-tests for normally distributed data or otherwise Mann-Whitney U-tests and linear regression analyses were used to compare the relationships of the growth measurements with the MDI. Differences were regarded as statistically significant if P-value for the appropriate test was less than 0.05.
Results
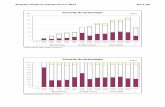
The mean 4 2 S.D. at 2 years of age for weight, height and occipitofrontal head circumference for 2-year-old males and females are contrasted with the standard population. Both sexes were significantly smaller in weight and height (all z-values 4.2, all P-values < 0.003). A significantly smaller mean head circumference was found only in males (z = 4.2, P = 0.003) (Fig. 1).
332
Weight - kg Height - cm
18-
16 -
14 -
12
10 C I 8
Male Female
95r
90- 85;j 11 80
75 -
70 Male Female
Head circumference - cm
ELBW children
I
Standard
population
Fig. 1. Mean and 1 S.D. of weight, height and head circumference of extremely low birthweight children at 2 years corrected age compared with a standard population.
TABLE I
Outcome in relation to categories of poor growth at birth and/or at 2 years
Group: 1 2 3 4 Total
SGA 2-year weight < 3rd percentile
Yes Yes
Yes No
No Yes
No No
n
Cerebral palsy n (5%) Quadriplegia, severe
motor disability Hemiplegia, mild
motor disability Diplegia, mild motor
disability
I 5 16 55 83
0 (0) l(20) 2 (13) 7 (13) 10 (12) 0 0 2 1 3
0 1 0 3 4
0 0 0 3 3
Sensorineural deafness 0 0 1 1 2
Bilateral blindness 0 0 2 0 2
Mental developmental Index mean 82.3 97.0 * 89.7 89.7 ** 89.5 (S.D.) (21.6) (6.2) (17.3) (15.8) (16.6) MD1 < 69 n (W) 2 (28.6%) 0 3 (18.8%) 5 (9.5%) 9 (10.8%)
Major impairment n (%) 2 (29) l(20) 3 (19) ll(20) 17 (20)
* MD1 for Groups 1 and 2 combined 88.4 (S.D. 18.1). ** MD1 for Groups 3 and 4 combined 89.7 (S.D. 16.5).
333
In Table I, children are classified into one of four groups according to their intrauterine and subsequent postnatal growth pattern: Group 1 SGA infants with poor postnatal weight gains (under the 3rd percentile) Group 2 SGA infants showing some catch-up in weight (above the 3rd percentile). Group 3 Non-SGA infants with poor postnatal weight gains. Group 4 Non-SGA infants with weight above the 3rd percentile at 2 years.
Twelve children at birth were SGA and poor weight gains persisted in 7 children at 2 years; of the 71 children who were not SGA, 16 demonstrated poor weight gains at 2 years; altogether 23/83 (27.7%) of the 2-year-old children had poor weight gains (Table I). The pattern for height at 2 years was similar, 26/83 (31.3%) being under the 3rd percentile but in contrast only 4/83 (4.8%) children had an occipitofrontal head circumference under the 3rd percentile.
For the whole study group, the prevalence of cerebral palsy was 12% and 17 children (20%) had a major impairment (Table I). No statistically significant differences were found in the prevalence of major impairments in the 12 children who were SGA compared with the 71 who were not SGA (Table I). Group 1, the seven SGA children with poor postnatal weight gains tended to have the worst outcome; included were the only two children in the study with major malforma- tions (craniosynostosis, Fallot’s tetralogy) and the only twins with extreme in- trauterine growth retardation with birthweights of 540 g (-3.7 S.D.) and 850 g (- 3.0 SD.) at 32 weeks gestation. The remaining 3 SGA children with poor postnatal weight gains were free of impairments and with MDIs of 95, 109 and 110. One of the 5 children in Group 2 - SGA children with catch-up growth - had an MD1 of 93 and spastic hemiplegia but another four children were free of impair- ments and the MD1 scores were 102, 102, 100 and 88.
In Table II, some perinatal, social and health characteristics of the 23 2-year-old children with poor postnatal growth are contrasted with the other 60 children. Birthweights of the two groups were almost identical but the children with poor postnatal growth were significantly more mature, duration of supplemental oxygen was shorter, and they tended to have more hospital readmissions and more days in hospital (P = 0.055 and P = 0.07, respectively).
In a linear regression analysis the absolute values of the occipito-frontal head circumference were not significantly associated with MD1 scores (r = 0.03, NS). To test the hypothesis that preferential head growth was significantly related to MDI, we performed linear regression analyses of the ratios of head circumference/body weight (r = - 0.08) and the head circumference/height (r = -0.05) with the MDI. These correlations are not statistically significant.
There were 17 multiple births in the study; the prevalence of major impairments was 24.5% (19.7% for singletons) and the mean MD1 was 86.9 (S.D., 14.9) compared with 90.2 (17.0) for singletons. The prevalence of impairments in the 47 girls was 19.1% (22.2% for boys). The mean MD1 for girls was 90.3 (S.D. 6.3) compared with 88.6 (S.D. 17.2) for the boys. None of these differences is statistically significant.
Data on three children not assessed close to the age of 2 years are excluded from the preceding results because no MD1 results .were available. None were SGA at birth and when last seen at 12, 18 and 36 months respectively all were growing
334
TABLE II
Perinatal, social and health variables in relation to poor growth at 2 years
All children Weight at 2 years (n =83) < 3rd centile z 3rd centile
(n = 23) (n=60)
Maternal height (cm) mean S.D.
Birthweight (g) mean SD.
Gestational age (weeks) mean S.D.
IPPV n (W)
IPPV 2 10 days n (‘76)
Oxygen 30 days n (56) 54 (65.1) 12 (52.2) 42 (70.0)
Illnesses after primary hospitalization
2 1 wheezing episode n (%)
Surgical operations n (W)
Hospital re-admissions Total hospital days n
Total hospital admissions n
Total children admitted n (W)
Major impairment n (%)
MD1 mean S.D.
160.5 161.0 160.5 8.1 9.1 7.1
860 847 866 99 114 92
27.5 28.5 27.1 2.2 2.4 2.1
65 (78.3) 18 (78.3) 47 (78.3)
30 (36.1) 5 (21.7) 25 (41.7)
31 (37.4)
20
536
60
28 (33.7)
17 (20.5) 89.5 16.6
9 (39.1)
7
342
31
10 (43.5)
5 (21.7) 87.4 18.4
22 (36.7)
13
194
29
18 (30.0)
12 (20.0) 90.4 15.9
Significance
NS
NS
t = 2.53 P = 0.013
NS
z =1.2 * NS
z = 2.05 * P = 0.04
z = 0.42 * NS z = 0.6 * NS
L =1.8 * P = 0.07 NS r=1.9* P = 0.055 NS x2 = 0.8 * NS NS t = 0.8 NS
* Mann-Whitney U-test. NS, not significant.
satisfactorily. The latter child had severe sensorineural deafness, whereas the others had no sensorineural handicap or apparent developmental delay. The children probably would be classified with Group 4 - non-SGA infants with weight above 3rd percentile at 2 years. Their inclusion would not appreciably alter our study results or conclusions.
335
Discussion
As a group, the ELBW children in our study tended to gain weight poorly in hospital and at the age of 2 years the distribution for weight and height were significantly lower than for the standard population. The only growth measurement that was not significantly reduced at 2 years was the head circumference of girls. Ross et al. [13] also noted preferential head growth in girls although their sample comprised appropriate weight for gestation infants of birthweight under 1501 g.
SGA infants were more likely to show poor postnatal weight gains but otherwise this group was not disadvantaged at two years. Although the sample size was small, the seven SGA infants who also gained weight poorly postnatally (and did comprise of two with major malformations and two extremely SGA twins) was possibly the subgroup at highest risk for impairments. We speculate that prenatal factors rather than inadequate postnatal nutrition underlies both the continued poor growth and impaired outcome in some of these children.
Prolonged or recurrent hospitalization, frequent wheezing episodes or caretaking problems were not clearly associated with poor growth at 2 years of age although other studies report this association [20]. Small maternal stature likewise appeared an unlikely cause for poor postnatal growth of so many children, for the mothers of SGA infants were not significantly shorter than the mothers of children who grew satisfactorily; the mean heights of mothers of SGA and non-SGA infants were almost exactly on the 50th percentile (162 cm) [13] (Table II).
Head growth, as indicated by occipito-frontal head circumference was less affected at two years than the other growth dimensions, particularly in the girls. Preferential brain growth cannot necessarily be inferred from apparently satisfac- tory head circumference values. The maximum occipito-frontal head circumference at 2 years does not necessarily reflect brain growth; with the dolicocephalic skull of a typical ex-premature infant, head circumference is greater for the same brain volume compared with a head which is approximately spherical [2]. No child in the study had a ventriculoperitoneal shunt for hydrocephalus. Because ultrasonic ex- amination of the cerebral ventricular system was not performed routinely on all ELBW infants, mild arrested hydrocephalus therefore cannot be definitely excluded in children born before June 1980. An unexpected finding in our study was the lack of correlation of MD1 with either the absolute head circumference or the ratio of head circumference/body weight at 2 years; this is contrary to the findings of Ross et al. [23], Gross et al. [8] and Lipper et al. [19]. In the latter reports infants weighed less than 1501 g at birth rather than 1000 g in our series; possibly the distortion of the shape of the head in the smaller infants was more pronounced than in the larger babies.
We used Australian standards for assessment of intrauterine and postnatal growth. Intrauterine growth dimensions were derived from hospital births in Melbourne occurring in 1973-1979 [17] and as the standard for postnatal growth we used sex-specific data from metropolitan children born in Sydney in 1971 and 1972. Because of the difficulties inherent in the assessment of gestational age in ELBW we relied preferentially on obstetrical data rather than clinical assessments of the
336
infant. The scoring system of Dubowitz and Dubowitz [7] and the modification of Ballard et al. [l] have not been validated for infants of extreme prematurity.
Our growth findings are consistent with other recent reports. Hirata et al. [ll] noted that of 18 survivors of birthweight 501-750 g, the mean height and weight were near the 5th percentile until 3 years but additional ‘catch up’ occurred between 4 and 6 years; Britton et al. [4] found that for outborn survivors of birthweight less than 801 g, 57% were below the 3rd percentile for weight, 37% for length and 17% for head circumference at 18 months post-term.
Growth is more favourable if the sample comprises only AGA infants of birthweight under 1501 g [23,26], or neurologically normal children [27]. Detailed comparison of growth data between studies is not possible because of differences in population samples, particularly in relation to the upper limit of birthweight and the exclusion of SGA and neurologically abnormal children [3,6,18,24,28].
Hack et al. [9] reported the outcome at 8 months post term of 192 infants who weighed less than 1500 g at birth; poor weight gains (weight under the 3rd percentile) was present in 46% of SGA infants at term but only 28% at 8 months. For SGA infants, poor weight gains were noted in 92% of infants at term and 50% at 8 months of age. In a more recent report, 22% of the cohort still had poor weight gain at 33 months corrected age [lo]. Whether catch-up growth will occur in children in our study is uncertain; however, in our earlier cohort study of infants weighing 1500 g or less at birth, substantial catch-up occurred between 2 and 8 years, the percentage of children with weights under the 10th percentile decreasing progressively from 17.6% at 3 years to 9.2% at 6 years and to 7.6% at 8 years of age
]I41. Prolonged or recurrent hospitalization, frequent wheezing episodes or caretaking
problems were not clearly associated with growth failure at two years of age although other studies report this association [20].
One may speculate that the present preoccupation with energy balance, the nutritional requirements [25] for the baby and emotional needs of the infant and family is directing attention away from other possible areas for intervention, The poor growth of the infants in our own and other studies indicates the need for basic research to identify what growth or other factors we are currently not providing for a patient that is essentially a fetus, not a neonate [29].
Acknowledgements
This study was supported in part by the National Health and Medical Research Council, Australia, and the 3AW Community Service Trust.
References
1 Ballard, J.L., Kazmaier, K. and Driver, M. (1977): A simplified assessment of gestational age. Pediatr. Res., 11, 374.
2 Baum, J.D. and Searle, D. (1971): Head shape and size of preterm low birthweight infants. Dev. Med. Child Neural., 13, 576-578.
337
3 Bennett, F.C., Robinson, N.M. and Sells, C.J. (1983): Growth and development of infants weighing less than 800 grams at birth. Pediatrics, 71, 319-323.
4 Britton, S.B., Fitzhardinge, P.M. and Ashby, S. (1981): Is intensive care justified for infants weighing less than 801 gm at birth? J. Pediatr., 99, 937-943.
5 Dobbing, J. and Sands, J. (1973): Quantitative growth and development of the human brain. Arch. Dis. Child., 48, 757-767.
6 Driscoll, J.M., Jr., Driscoll, Y.T. and Steir, M.E. et al. (1982): Mortality and morbidity in infants less than 1001 grams birth weight. Pediatrics, 69, 21-26.
7 Dubowitz, L.M.S. and Dubowitz, V. (1977): Gestational age of the newborn. Addison-Wesley, MA, pp. 45.
8 Gross, S.J., Oehler, J.M. and Eckerman, C.O., (1980): Head growth and developmental outcome in very low birth-weight infants. Pediatrics, 71, 70-75.
9 Hack, M., Merkatz, I.R. and Gordon, D. et al. (1982): The prognostic significance of postnatal growth in very low-birth weight infants. Am. J. Obstet. Gynecol., 143, 693-699.
10 Hack, M., Rivers, A. and Fanaroff, A.A. (1983): The very low birthweight infant: The broader spectrum of morbidity during infancy and early childhood. J. Dev. Behav. Pediatr., 4, 243-249.
11 Hirata, T., Epcar, J.T. and Walsh, A. et al. (1983): Survival and outcome of infants 500 to 750 grams: A six year experience. J. Pediatr., 102, 741-748.
12 Hoskins, E.M., Elliot, E. and Shennan, A.T. et al. (1983): Outcome of very low-birth weight infants born in a perinatal center. Am. J. Obstet. Gynecol., 145, 135-140.
13 Jones, D.L. and Hemphill, W. (1974): Weight height and other physical characteristics of New South Wales Children. Part II. Children under five years of age. Government Printer, New South Wales, Australia.
14 Kitchen, W.H., McDougall, A.B. and Naylor, F.D. (1980): A longitudinal study of very low birthweight infants: III Distance growth at eight years of age. Dev. Med. Child Neurol. 22, 163-171.
15 Kitchen, W.H., Ryan, M.M. and Rickards, A. et al. (1980): A longitudinal study of very low birthweight infants. IV: An overview of performance at eight years of age. Dev. Med. Child Neurol., 22, 172-188.
16 Kitchen, W.H., Yu. V.Y.H., Lissenden, J.V. and Bajuk, B. (1982): Collaborative study of very-low- birthweight infants: Techniques of perinatal care and mortality. Lancet, 2, 1454-1457.
17 Kitchen, W.H., Robinson, H.P. and Dickinson, A.J. (1983): Revised intrauterine growth curves for an Australian hospital population. Aust. Paediatr. J., 19, 157-161.
18 Kumar, P., Anday, E.K. and Sacks, L.M. et al. (1980): Follow-up studies of very low birth weight infants (1,250 grams or less) born and treated within a perinatal center. Pediatrics, 66, 438-444.
19 Lipper, E., Lee, K.-S., Gartner, L.M. and Grellong, B. (1981): Determinants of neurobehavioural outcome in low-birth-weight infants. Pediatrics, 67, 502-505.
20 Manser, J. (1984): Growth in the high-risk infant. Clin. Perinatol., 11, 19-40. 21 Nie, N.H., Hull, C.H., Jenkins, J.G., Steinbrenner, K. and Bent, D.H. (1970): Statistical Package for
Social Sciences, 2nd edn. McGraw-Hill, New York. 22 Robinson, H. (1973): Sonar measurement of fetal crown-rump length as a means of assessing
maturity in the first trimester of pregnancy. Br. Med. J., 4, 28-31. 23 Ross, G., Krauss, A.N. and Auld, P.A. (1983): Growth achievement in low-birth-weight premature
infants: Relationship to neurobehavioural outcome at one year. J. Pediatr., 103, 105-108. 24 Saigal, S., Rosenbaum, P., Stoskopf, B. and Milner, R. (1982): Follow-up of infants 501 to 1500 gm
birthweight delivered to residents of a geographically defined region with perinatal intensive care facilities. J. Pediatr., 100, 606-613.
25 Stern, L. (1982): Early postnatal growth of low birthweight infants: what is optimal? Acta. Paediatr. Stand. (Suppl.), 296, 6-13.
26 Tudehope, D.I., Burns, Y. and Callaghan, M. et al. (1983): The relationship between intrauterine and postnatal growth on subsequent psychomotor development of very low birthweight (VLBW) infants. Aust. Paediatr. J., 19, 3-8.
27 Kimble, K.J., Araigno, R.L., Stevenson, D.K. and Sunshine, P. (1982): Growth to age 3 years among very low-birth-weight sequelae-free survivors of modern neonatal intensive care. J. Pediatr., 100, 622-624.
28 Vohr, B., Oh, W. and Rosenfield, A.G. et al. (1979): The preterm small-for-gestational age infant: A two-year follow-up study. Am. J. Obstet. Gynecol., 133, 425-431.
29 Warshaw, J.B. (1979): The growth retarded fetus. Clin. Perinatol., 6, 353-363.