Reflux gastritis intact stomach · tween the normal and reflux gastritis groups, but significantly...
Transcript of Reflux gastritis intact stomach · tween the normal and reflux gastritis groups, but significantly...

J Clin Pathol 1990;43:303-306
Reflux gastritis in the intact stomach
GM Sobala, R F G King, A T R Axon, M F Dixon
AbstractGastric biopsy specimens from patientswho have undergone gastric surgery fre-quently exhibit foveolar hyperplasia,oedema, vasodilatation and congestion,and a paucity of inflammatory cells asconsequences of entero-gastric reflux.Similar, albeit generally milder, changeswere found in 47 of316 (15%) non-surgicalpatients undergoing endoscopy for dys-peptic symptoms. To relate these changesto bile reflux or other potential gastricirritants the total bile acid concentrationwas measured in samples of fasting gas-tric juice, and the use of a symptomquestionnaire ascertained the patients'cigarette consumption, use of non-steroidal anti-inflammatory drugs(NSAIDs), and alcohol intake. Whenpatients with reflux gastritis were com-pared with normal controls (n = 91),significant increases in associated pepticulceration and NSAID use were found inthe group with reflux, but no increases inbile acid concentrations. Indeed, only onepatient had evidence of duodenogastricreflux.
It is concluded that most cases of"reflux gastritis" in the intact stomachare not due to reflux of bile. Our findingsindicate an important pathogenic role forlong term NSAID use, in what might beusefully termed type C or "chemical"gastritis.
GastroenterologyUnit, The GeneralInfirmary, LeedsGM SobalaA T R AxonProfessorial SurgicalUnitR F G KingUniversityDepartment ofPathologyM F DixonCorrespondence to:Dr M F Dixon, Departmentof Pathology, University ofLeeds LS2 9JT.Accepted for publication16 November 1989
A distinctive histological picture has recentlybeen recognised in biopsy specimens takenfrom postoperative stomachs: it is character-ised by foveolar elongation, tortuosity andhypercellularity, together with oedema, vaso-dilatation, congestion and a paucity of inflam-matory cells in the lamina propria.1 It iscorrelated with objective measures of entero-gastric bile reflux, and has therefore beentermed "reflux gastritis". These histologicalfeatures, however, are not confined to thepostoperative stomach and we have previouslyseen similar changes in 35 of 205 non-surgicalpatients with non-ulcer dyspepsia.' This is a
substantial proportion, and is difficult toattribute to abnormal duodenogastric bilereflux alone. We have therefore hypothesisedthat this histological picture may, in fact, be a
non-specific response to a variety of gastricirritants, bile being just one.The aim of this study was to confirm the
prevalence of "reflux gastritis" in the intact
stomach, to examine its relation with gastro-duodenal pathology, and to determine whetherit is associated with high alcohol intake, useof non-steroidal anti-inflammatory agents(NSAIDs) or total bile acid concentrations infasting gastric juice as a measure of duodeno-gastric reflux. It was decided for two reasonsthat the chief analyses should be between thosepatients diagnosed as having reflux gastritisand those with normal antral histology. Firstly,because before reflux gastritis was recognisedas a separate entity, almost all such biopsyspecimens would have been reported as beingwithin normal limits; and secondly, we con-sidered that any possible effects of irritants onthe gastric mucosa would be masked by themore obvious sequelae of Helicobacter pylori(previously known as Campylobacter pylori')infection in those patients with type B chronicgastritis.'
Patients and methodsBiopsy specimens were obtained from patientsparticipating in a study investigating possibleassociations between dyspeptic symptoms andH pylori. Over 12 months two antral biopsyspecimens were taken from each of 316 patientsattending an endoscopy clinic with symptomsof dyspepsia. Patients with previous gastricsurgery were excluded. All patients were givena "symptom questionnaire" which includeddetailed questions about alcohol intake and useof NSAIDs. Alcohol consumption was re-corded in terms of units per week; use ofNSAIDs was recorded on a four point scale (0= none at all; 1 = several times a month; 2 =several times a week; 3 = daily).
MEASUREMENT OF TOTAL BILE ACIDIn 110 patients 5 ml offasting gastric juice wereaspirated into a clean container and then storedat - 20'C for analysis within three months.Total bile acid concentrations were thenmeasured using the previously describedsteroid dehydrogenase method.4 By thismethod a bile acid concentration of > 1 mmol/lis regarded as abnormal and indicative ofclinically important duodenogastric reflux.'The biopsy specimens were immediately
fixed in 100% formalin and routinely processed.Paraffin wax sections were cut at three levelsand stained by haematoxylin and eosin.Additional sections taken at level 2 were stainedwith the modified Giemsa technique for Hpylori. All sections were examined by the samepathologist (MFD) without knowledge ofotherpatient data. The presence of foveolar hyper-
303
on January 30, 2020 by guest. Protected by copyright.
http://jcp.bmj.com
/J C
lin Pathol: first published as 10.1136/jcp.43.4.303 on 1 A
pril 1990. Dow
nloaded from

Sobala, King, Axon, Dixon
Table 1 Demographic details, prevalence of ulcer disease, and H pylori infection byhistologicalgroup
Mean Ulcer PercentageHistology n age Range Male disease positive
Normal 91 38-8 (18-70) 539°0 3.30 3.3Chronic superficial
gastritis 97 43-7* (18-69) 58 80o 33°.t 928tChronic atrophic
gastritis 77 48 1t (19-74) 5844% 4555%t 94-8tReflux gastritis 47 37 0 (18-66) 68% 12-8%* 2-1Lymphocytic gastritis 4 41 0 (22-67) 75O0 25% 25
Group differs from controls: *= p < 0-05; t= p < 0-001.
Table 2 Prevalence ofpossible risk factors (gastric irritants) in patients with normalhistology and reflux gastritis
Percentage of Percentage ofpatients heavy High bile
Perecentage of taking drinkers acidHistology smokers NSAIDs (>30 units/week) (>I mmol/l)
Normal 40 8(n = 76) 66(n = 76) 7 9(n = 76) 0of27Reflux gastritis 432 (n = 37) 21-6 (n = 37) 16-2 (n = 37) 1 of 23
n.s. p < 005 p = 015 n.s.
plasia, lamina propria oedema, and vascularcongestion were scored on a scale of 0 (none) to3 (severe), and these were added to two scores(0 to 3) for paucity of acute and chronicinflammatory cells, respectively, to give a totalreflux score (minimum 0, maximum 15). Onthe basis of previous work, patients with refluxscores of 11 or more were considered to have"reflux gastritis".'Comparisons between groups were per-
formed with standard non-parametric ranktests for ordinal data, and Fisher's exact test fornominal data using the SAS statistics packageon a mainframe computer.6
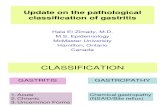
ResultsFive different patterns of antral histology wereide*tified: (i) normal; (ii) chronic superficialgastritis; (iii) chronic atrophic gastritis; (iv)reflux gastritis; and (v) lymphocytic gastritis.The demographic details of these five groups,together with the prevalence of ulcer diseaseand H pylori infection are shown in table 1.Patients with chronic gastritis or lymphocytic
gastritis were excluded from further analysis,leaving 47 with reflux gastritis and 91 withnormal histology.There were no significant differences in age
or sex distribution between patients withnormal histology and reflux gastritis, but sig-nificantly more patients with reflux gastritishad peptic ulcers (oesophageal, gastric, pyloricor duodenal) than did patients with normalhistology.
POSSIBLE GASTRIC IRRITANTSOf the 138 patients with either normal his-tology or reflux gastritis, 113 (81 9%) respon-ded to the questionnaire (table 2). Cigaretteconsumption did not differ significantly be-tween the normal and reflux gastritis groups,but significantly more patients in the groupwith reflux gastritis were taking NSAIDs. Fig1 shows changes of reflux gastritis in a patienttaking aspirin daily. There was a significantcorrelation between NSAID use and the totalreflux score, as well as with foveolar hyper-plasia and vascular congestion (table 3). Al-though there was a trend towards more patientsin the group with reflux gastritis being heavydrinkers, this did not reach significance. Fig 2shows the reflux gastritis in a patient consum-ing 40 units of alcohol a week. There were nodifferences in median gastric fasting total bilesalt concentrations between control and patienthistology in the 49 people in both groups inwhom it was measured. Only one patient inthese two groups had an abnormal bile acidconcentration and he also had reflux gastritis(fig 3).
DiscussionAlthough the histological features of refluxgastritis were originally described in post-operative stomachs in association with entero-gastric bile reflux, our results confirm that theyare often found in dyspeptic subjects withintact stomachs. The absence of an inflam-
Figure 1 (a) Antralbiopsy specimensfrom apatient taking aspirinregularly, showing mildfoveolar elongation andtortuosity; (b) higherpower view showingincreased cellularity of thefoveolae with nuclearenlargement, some nuclear"crowding" at the surface,and mild mucin depletion.
304
on January 30, 2020 by guest. Protected by copyright.
http://jcp.bmj.com
/J C
lin Pathol: first published as 10.1136/jcp.43.4.303 on 1 A
pril 1990. Dow
nloaded from

Reflux gastritis
Table 3 Correlation between histologicalfeatures andprevalence of ingestion ofNSAIDs
Spearmancorrelation
Histologicalfeature coefficient p Value
Foveolar hyperplasia 0-21 p = 003Lamina propria oedema 0 08 NSVascular congestion 0 20 p = 003Histological reflux score 0-24 p = 0-01
matory cell infiltrate in this condition hashampered its recognition by pathologists: mostsuch biopsy specimens would previously havebeen passed as normal. Our finding of a higherincidence of ulcer disease in the group withreflux gastritis compared with controls, how-ever, supports the notion that this is a separatepathological entity. The association withgastroduodenal ulcers suggests that there arecommon aetiological factors for both refluxgastritis and ulcer disease. Alternatively, somecases of antral reflux gastritis may be secondaryto duodenal ulcer disease if this has led topyloroduodenal scarring and facilitatedenterogastric bile reflux. Reflux gastritis maythen replace the original condition of antral Hpylori associated chronic gastritis generallypresent in patients with duodenal ulcers. Ourstudy again confirms the strong negative cor-relation between H pylori and the histologicalpicture of reflux gastritis.7The finding of an increased gastric bile acid
concentration in only one of 23 cases of refluxgastritis in intact stomachs contrasts with a rateof 11 out of 27 in mostly postoperative patientsin our previous study.' A single estimation offasting gastric juice bile acid concentration maynot be a specific measure of bile reflux in anyone patient, but it has been shown to give anaccurate representation of bile reflux in apopulation.8 This result therefore indicatesthat "reflux gastritis" is usually caused byagents other than bile in the non-surgicalstomach.Our search for other causative agents was
only partially successful. Nevertheless, we have
established a clear association between use ofNSAIDs and the presence of the histologicalpicture of "reflux gastritis". While the role ofNSAIDs in causing acute erosive gastritis andhaemorrhage in both experimental animals andman is well documented,9 there have been fewhistological studies on the effects of long termuse. Until recently their possible effects on thegastric mucosa have invariably been assessed interms ofan acute and chronic inflammatory cellresponse. It is now appreciated, however, thatchronic mucosal inflammation is widelyprevalent in the age group of patients who takeNSAIDs and that this is a consequence of Hpylori colonisation. In H pylori positive casesthe associated chronic gastritis dominates thehistological appearances and masks anydamage caused by NSAIDs. Thus it is notsurprising that a study from the era before Hpylori concluded that the presence and severityof chronic gastritis remained unaffected byfour weeks of treatment with NSAIDs.Y Evenrecent studies on patients taking NSAIDswhere H pylori has been sought have failed todistinguish changes induced by these drugsfrom H pylori-related inflammation byseparate consideration of biopsy specimensfrom H pylori positive and negative cases andcomparison with positive and negative controlsubjects not taking NSAIDs." 12 That there areepithelial changes brought about by NSAIDs,which are unrelated to H pylori and inflam-matory cell infiltration, is indicated by adetailed study on 13 patients with drug inducedgastric erosions,'3 and further support comesfrom a description of "gastric adaptation" tochronic aspirin ingestion in which it was foundthat surface epithelial regeneration and vas-cular congestion were more common aftertreatment.'4 Interestingly, this study alsoreported changes of atrophy associated withtreatment: in our patients those takingNSAIDs were also more likely to exhibitatrophy (Spearman rank correlation coefficientr = 029; p = 0002).
Figure 2 (a) Antralmucosa from 41 year oldman who drinks 40 units ofalcohol a week. There iselongation and distortionoffoveolae with mildoedema of the superficiallamina propria. (b)Higher power view ofanother biopsy specimenfrom this subject showsnuclear crowding in thefoveolae and glandularatrophy with laminapropria fibrosis.
:~~'^, :f~J~ .. >.t.ts'='t'
f~~~~~~~~~~~~~~j
'-;
305
,tF j ,
.1 "-, .-e .'k,
on January 30, 2020 by guest. Protected by copyright.
http://jcp.bmj.com
/J C
lin Pathol: first published as 10.1136/jcp.43.4.303 on 1 A
pril 1990. Dow
nloaded from

Sobala, King, Axon, Dixon
Figure 3 (a) Foveolarhyperplasia and distortionis evident in this antralbiopsy specimenfrom thepatient with confirmed bilereflux (gastric juice bileacids = 7 05 mmol/l).Although a basalaggregate of lymphocytes ispresent, highermagnification (b) showsveryfew inflammatorycells in the superficiallamina propria andconfirms foveolar andsurface hypercellularityand mucin depletion.
We were unable to identify with certaintyany other predisposing factors for reflux gas-
tritis, although there was a non-significanttrend towards an association with high alcoholintake. Again previous studies of gastritis inalcoholics have been confounded (with hind-sight) by the interplay with H pylori relatedgastritis. Nevertheless, some relevant observa-tions emerge from previous reports on thesubject. Williams comments that "inflarh-matory lesions were notably slight or entirelyabsent, even in some inveterate spirit drink-ers," and one of his cases showed widespreadhyperplasia of the surface epithelium.i5 On theother hand, Parl found a higher incidence ofchronic gastritis in alcoholic patients comparedwith controls, but also described, "formation ofvilli in the antrum with ... extensive epithelialregeneration even in the absence of acutemucosal damage"'.i6 This anecdotal evidencefor a pattern of response distinct from chronicgastritis is strengthened by a detailed his-tological study of alcoholic haemorrhagic gas-tritis in which scores for epithelial regenerationand mucosal oedema were significantly higherthan those in gastric biopsy specimens fromcontrol subjects.i7 Furthermore, damagecaused by alcohol induces mast cell degranula-tion and release of vasoactive mediators,i8 a
mechanism analagous to that implicated in bilereflux gastritis.'9 It has to be conceded,however, that even if alcohol was a factor thiswould leave about half of our cases of refluxgastritis unaccounted for.We conclude that the findings of foveolar
hyperplasia, capillary dilatation and conges-tion, and lamina propria oedema with no in-crease in chronic inflammatory cells comprise a
distinct histological entity. This has previouslybeen termed reflux gastritis but would prob-ably now be better categorised under a lessrestrictive term. In keeping with our previousclassification into type A (autoimmune) andtype B (bacteria-associated) gastritis,3 we
would advocate type C "chemical" gastritis forthis category as it seems to be a consequence of
%"1 A,4*.
I '4~~~~~~~~
/ t 8'.. #.4' ° -,o.'r'
'V\;4: ; <'t S * <N j
,- R ^-v > -,,,r.-
'C..~~~~~~~~~~~~~~.
gastric irritation by bile constituents, NSAIDs,or other, as yet unidentified, agents.
1 Dixon MF, O'Connor HJ, Axon ATR, King RFJG,Johnston D. Reflux gastritis: distinct histopathologicalentity? J Clin Pathol 1986;39:524-30.
2 Wyatt JI, Dixon MF. Chronic gastritis-a pathogeneticapproach. JPathol 1988;154:113-24.
3 Goodwin CS, Armstrong JA, Chilvers T, et al. Transfer ofCampylobacter pylori and Campylobacter mustelae toHelicobacter gen. nov. as Helicobacter pylori comb. nov.and Helicobacter mustelae comb. nov. respectively.International Journal of Systematic Bacteriology 1989;39:397-405.
4 Dewar EP, King RFGJ, Johnston D. Bile acid and lyso-lecithin concentrations in the stomach of patients withgastric ulcer: before operation and after treatment byhighly selective vagotomy, Billroth I partial gastrectomyand truncal vagotomy and pyloroplasty. Br J Surg 1983;70:401-5.
5 Rhodes J, Barnardo DE, Phillips SF, Rovelstad PA,Hofmann AF. Increased reflux of bile into the stomach inpatients with gastric ulcer. Gastroenterology 1969;57:241-52.
6 SAS user's guide: statistics. Version 5 edition. Cary, NorthCarolina: SAS Institute Inc, 1985.
7 O'Connor HJ, Wyatt JI, Dixon MF, Axon ATR. Campy-lobacter like organisms and reflux gastritis. J Clin Pathol1986;39:531-4.
8 Houghton PWJ, Mortensen NJMcC, Thomas WEG,Cooper MJ, Morgan AP, Burton P. Intragastric bile acidsand histological changes in gastric mucosa. Br J Surg1986;73:354-6.
9 Rainsford KD. An analysis of the gastro-intestinal side-effects on non-steroidal anti-inflammatory drugs, withparticular reference to comparative studies in man andlaboratory species. Rheumatol Int 1982;2:1-10.
10 McIntyre RLE, Irani MS, Piris J. Histological study of theeffects of three anti-inflammatory preparations on thegastric mucosa. J Clin Pathol 1981;34:836-42.
11 Doube A, Morris A. Nonsteroidal anti-inflammatory drug-induced dyspepsia-is Campylobacter pyloridis impli-cated? Br J Rheumatol 1988;27:110-2.
12 Upadhyay R, Howatson A, McKinlay A, Danesh BJZ,Sturrock RD, Russell RI. Campylobacter pyloriassociated gastritis in patients with rheumatoid arthritistaking nonsteroidal anti-inflammatory drugs. Br JRheumatol 1988;27:113-6.
13 Laipe L, Marin-Sorensen M, Weinstein WM. The histologyof gastric erosions in patients taking non-steroidal anti-inflammatory drugs (NSAIDs): a prospective study.Gastroenterology 1988;94:A247.
14 Graham DY, Smith JL, Spjut HJ, Torres E. Gastricadaptation: studies in humans during continuous aspirinadministration. Gastroenterology 1988;95:327-33.
15 Wynn Williams A. Effects of alcohol on gastric mucosa. BrMed J 1956;i:256-9.
16 Parl FF, Lev R, Thomas E, Pitchumoni CS. Histologic andmorphometric study of chronic gastritis in alcoholicpatients. Hum Pathol 1979;10:45-56.
17 Laine L, Weinstein WM. Histology of alcoholic hemorr-hagic "gastritis": a prospective evaluation. Gastro-enterology 1988;94:1254-62.
18 Oates PJ, Hakkinen JP. Studies on the mechanism ofethanol-induced gastric damage in rats. Gastroenterology1988;94: 10-21.
19 Rees W, Rhodes J. Bile reflux in gastro-oesophageal disease.Clin Gastroenterol 1977;6:179-200.
306
on January 30, 2020 by guest. Protected by copyright.
http://jcp.bmj.com
/J C
lin Pathol: first published as 10.1136/jcp.43.4.303 on 1 A
pril 1990. Dow
nloaded from